Frequency and Significance of Pathologic Pulmonary Findings in Postmortem Examinations—A Single Center Experience before COVID-19
Abstract
1. Introduction
2. Materials and Methods
2.1. Postmortem Diagnostic Procedure
2.2. Patients
2.3. Data Recording
2.4. Statistics
3. Results
3.1. Patient Characteristics and Causes of Death
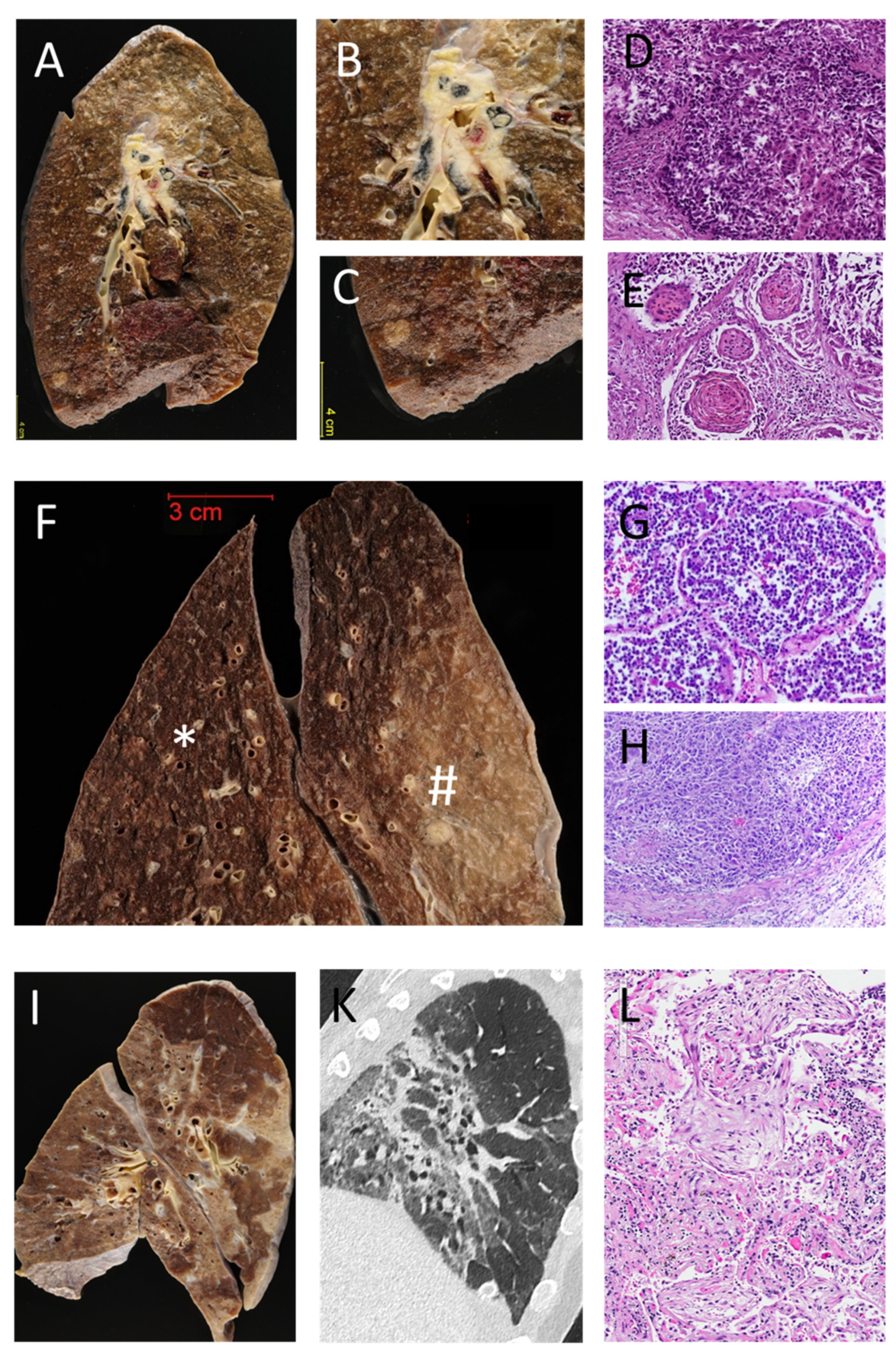
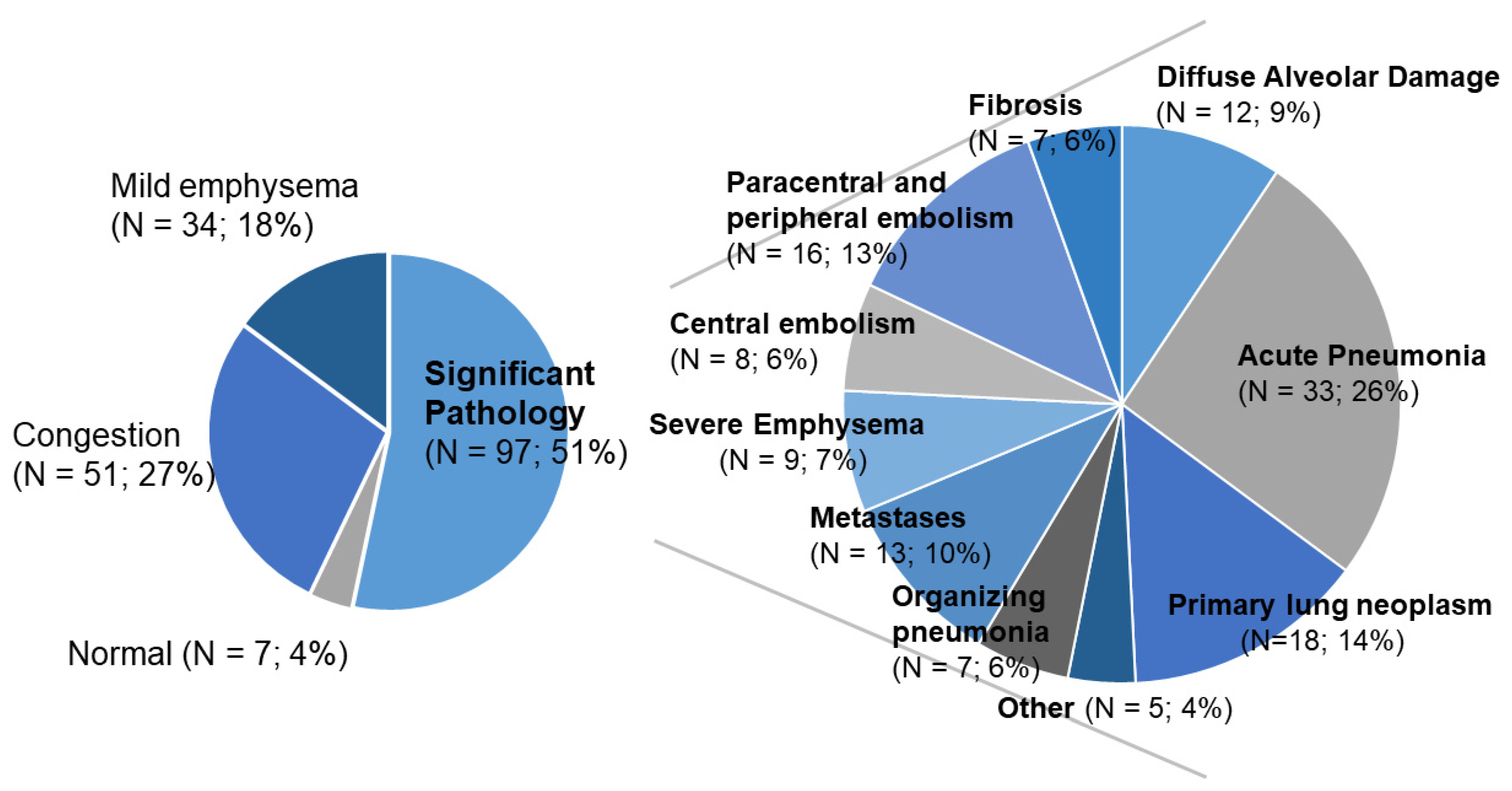
3.2. Pathological Pulmonary Findings
3.3. Correlation with Demographic Data and Clinical Findings
3.4. Comparison between Clinical Diagnoses and Postmortem Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Menter, T.; Haslbauer, J.D.; Nienhold, R.; Savic, S.; Hopfer, H.; Deigendesch, N.; Frank, S.; Turek, D.; Willi, N.; Pargger, H.; et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction. Histopathology 2020, 77, 198–209. [Google Scholar] [CrossRef] [PubMed]
- Tzankov, A.; Jonigk, D. Unlocking the lockdown of science and demystifying COVID-19: How autopsies contribute to our understanding of a deadly pandemic. Virchows Arch. 2020, 477, 331–333. [Google Scholar] [CrossRef] [PubMed]
- Borczuk, A.C.; Salvatore, S.P.; Seshan, S.V.; Patel, S.S.; Bussel, J.B.; Mostyka, M.; Elsoukkary, S.; He, B.; DEL Vecchio, C.; Fortarezza, F.; et al. COVID-19 pulmonary pathology: A multi-institutional autopsy cohort from Italy and New York City. Mod. Pathol. 2020, 33, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, F.; Pezzuto, F.; Fortarezza, F.; Hofman, P.; Kern, I.; Panizo, A.; Von Der Thüsen, J.; Timofeev, S.; Gorkiewicz, G.; Lunardi, F. Pulmonary pathology and COVID-19: Lessons from autopsy. The experience of European Pulmonary Pathologists. Virchows Arch. 2020, 477, 359–372. [Google Scholar] [CrossRef]
- Gulsvik, A.K.; Henriksen, A.H.; Svendsen, E.; Humerfelt, S.; Gulsvik, A. Validity of the European short list of respiratory diseases: A 40-year autopsy study. Eur. Respir. J. 2014, 45, 953–961. [Google Scholar] [CrossRef]
- Akindipe, O.A.; Fernandez-Bussy, S.; Staples, E.D.; Baz, M.A. Discrepancies between clinical and autopsy diagnoses in lung transplant recipients. Clin. Transplant. 2009, 24, 610–614. [Google Scholar] [CrossRef]
- Perkins, G.D.; McAuley, D.F.; Davies, S.; Gao, F. Discrepancies between clinical and postmortem diagnoses in critically ill patients: An observational study. Crit. Care 2003, 7, R129–R132. [Google Scholar] [CrossRef]
- Roosen, J.; Frans, E.; Wilmer, A.; Knockaert, D.C.; Bobbaers, H. Comparison of Premortem Clinical Diagnoses in Critically Ill Patients and Subsequent Autopsy Findings. Mayo Clin. Proc. 2000, 75, 562–567. [Google Scholar] [CrossRef]
- Roulson, J.; Benbow, E.W.; Hasleton, P.S. Discrepancies between clinical and autopsy diagnosis and the value of post mortem histology; a meta-analysis and review. Histopathology 2005, 47, 551–559. [Google Scholar] [CrossRef]
- Schwanda-Burger, S.; Moch, H.; Muntwyler, J.; Salomon, F. Diagnostic errors in the new millennium: A follow-up autopsy study. Mod. Pathol. 2012, 25, 777–783. [Google Scholar] [CrossRef]
- Sonderegger-Lseli, K.; Burger, S.; Muntwyler, J.; Salomon, F. Diagnostic errors in three medical eras: A necropsy study. Lancet 2000, 355, 2027–2031. [Google Scholar] [CrossRef]
- Winters, B.; Custer, J.; Jr, S.M.G.; Colantuoni, E.; Kapoor, S.G.; Lee, H.; Goode, V.; Robinson, K.; Nakhasi, A.; Pronovost, P.; et al. Diagnostic errors in the intensive care unit: A systematic review of autopsy studies. BMJ Qual. Saf. 2012, 21, 894–902. [Google Scholar] [CrossRef] [PubMed]
- Maris, C.; Martin, B.; Creteur, J.; Remmelink, M.; Piagnerelli, M.; Salmon, I.; Vincent, J.L.; Demetter, P. Comparison of clinical and post-mortem findings in intensive care unit patients. Virchows Arch. 2007, 450, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://pubmed.ncbi.nlm.nih.gov/?term=case+report+%2B+pulmonary+pathology+%2B+autopsy&sort=date&size=50&show_snippets=off. (accessed on 17 May 2021).
- Langer, R.; Tröhler, A.; Schnüriger, B.; Trippel, M.; Blank, A.; Banz, Y.; Candinas, D.; Perren, A.; Lugli, A. Implementation of modern tools in autopsy practice—The way towards contemporary postmortal diagnostics. Virchows Arch. 2018, 474, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Connolly, A.J.; Finkbeiner, W.E.; Ursell, P.C.; Davis, R.L. Autopsy Pathology: A Manual and Atlas; Elsevier BV: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Rusu, S.; Lavis, P.; Salgado, V.D.; Van Craynest, M.-P.; Creteur, J.; Salmon, I.; Brasseur, A.; Remmelink, M. Comparison of antemortem clinical diagnosis and post-mortem findings in intensive care unit patients. Virchows Arch. 2021, 1–8. [Google Scholar] [CrossRef]
- Friberg, N.; Ljungberg, O.; Berglund, E.; Berglund, D.; Ljungberg, R.; Alafuzoff, I.; Englund, E. Cause of death and significant disease found at autopsy. Virchows Arch. 2019, 475, 781–788. [Google Scholar] [CrossRef]
- Nagai, A.; Yamawaki, I.; Thurlbeck, W.M.; Takizawa, T. Assessment of Lung Parenchymal Destruction by Using Routine Histologic Tissue Sections. Am. Rev. Respir. Dis. 1989, 139, 313–319. [Google Scholar] [CrossRef]
- Khare, P.; Gupta, R.; Ahuja, M.; Khare, N.; Agarwal, S.; Bansal, D. Prevalence of Lung Lesions at Autopsy: A Histopathological Study. J. Clin. Diagn. Res. 2017, 11, EC13–EC16. [Google Scholar] [CrossRef]
- Ro, A.; Kageyama, N.; Tanifuji, T.; Sakuma, M. Autopsy-proven untreated previous pulmonary thromboembolism: Frequency and distribution in the pulmonary artery and correlation with patients’ clinical characteristics. J. Thromb. Haemost. 2011, 9, 922–927. [Google Scholar] [CrossRef]
- Daniels, C.E.; Yi, E.S.; Ryu, J.H. Autopsy findings in 42 consecutive patients with idiopathic pulmonary fibrosis. Eur. Respir. J. 2008, 32, 170–174. [Google Scholar] [CrossRef]
- Oda, K.; Ishimoto, H.; Yamada, S.; Kushima, H.; Ishii, H.; Imanaga, T.; Harada, T.; Ishimatsu, Y.; Matsumoto, N.; Naito, K.; et al. Autopsy analyses in acute exacerbation of idiopathic pulmonary fibrosis. Respir. Res. 2014, 15, 1–9. [Google Scholar] [CrossRef]
- Urer, H.N.; Ersoy, G.; Yılmazbayhan, E.D. Diffuse Alveolar Damage of the Lungs in Forensic Autopsies: Assessment of Histopathological Stages and Causes of Death. Sci. World J. 2012, 2012, 1–6. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Thille, A.W.; Peñuelas, O.; Lorente, J.A.; Fernández-Segoviano, P.; Rodriguez, J.-M.; Aramburu, J.-A.; Panizo, J.; Esteban, A.; Frutos-Vivar, F. Predictors of diffuse alveolar damage in patients with acute respiratory distress syndrome: A retrospective analysis of clinical autopsies. Crit. Care 2017, 21, 254. [Google Scholar] [CrossRef]
- Lee, H.E.; Yi, E.S.; Rabatin, J.T.; Bohman, J.K.; Roden, A.C. Histopathologic Findings in Lungs of Patients Treated With Extracorporeal Membrane Oxygenation. Chest 2018, 153, 825–833. [Google Scholar] [CrossRef]
- Manser, R.L.; Dodd, M.; Byrnes, G.; Irving, L.B.; Campbell, D.A. Incidental lung cancers identified at coronial autopsy: Implications for overdiagnosis of lung cancer by screening. Respir. Med. 2005, 99, 501–507. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jaccard, C.M.; Plüss, E.; Doulberis, M.; Tippel, M.; Banz, Y. Ungewöhnliche Ursache eines Kapillarlecksyndroms. Swiss Med. Forum 2018, 18, 517–519. [Google Scholar]
- Nichols, L.; Saunders, R.; Knollmann, F.D. Causes of Death of Patients With Lung Cancer. Arch. Pathol. Lab. Med. 2012, 136, 1552–1557. [Google Scholar] [CrossRef] [PubMed]
- Ussavarungsi, K.; Yi, E.S.; Maleszewski, J.J.; Kurtin, P.J.; Dasari, S.; Theis, J.D.; Dispenzieri, A.; Ryu, J.H. Clinical relevance of pulmonary amyloidosis: An analysis of 76 autopsy-derived cases. Eur. Respir. J. 2017, 49, 1602313. [Google Scholar] [CrossRef] [PubMed]
- Goldman, L.; Sayson, R.; Robbins, S.; Cohn, L.H.; Bettmann, M.; Weisberg, M. The Value of the Autopsy in Three Medical Eras. N. Engl. J. Med. 1983, 308, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Pastores, S.M.; Dulu, A.; Voigt, L.; Raoof, N.; Alicea, M.; Halpern, N.A. Premortem clinical diagnoses and postmortem autopsy findings: Discrepancies in critically ill cancer patients. Crit. Care 2007, 11, R48. [Google Scholar] [CrossRef]
- Graber, M.L.; Franklin, N.; Gordon, R. Diagnostic Error in Internal Medicine. Arch. Intern. Med. 2005, 165, 1493–1499. [Google Scholar] [CrossRef]
- Burton, J.L.; Underwood, J. Clinical, educational, and epidemiological value of autopsy. Lancet 2007, 369, 1471–1480. [Google Scholar] [CrossRef]
- Thurnheer, R.; Hoess, C.; Doenecke, C.; Moll, C.; Muntwyler, J.; Krause, M. Diagnostic performance in a primary referral hospital assessed by autopsy: Evolution over a ten-year period. Eur. J. Intern. Med. 2009, 20, 784–787. [Google Scholar] [CrossRef]
- Twigg, S.J.; McCrirrick, A.; Sanderson, P.M. A comparison of post mortem findings with post hoc estimated clinical diagnoses of patients who die in a United Kingdom intensive care unit. Intensive Care Med. 2001, 27, 706–710. [Google Scholar] [CrossRef] [PubMed]
- Murken, D.R.; Ding, M.; Branstetter, B.F.; Nichols, L. Autopsy as a Quality Control Measure for Radiology, and Vice Versa. Am. J. Roentgenol. 2012, 199, 394–401. [Google Scholar] [CrossRef] [PubMed]
- O’Grady, G. Death of the teaching autopsy. BMJ 2003, 327, 802–803. [Google Scholar] [CrossRef]
- Tweel, J.G.V.D.; Wittekind, C. The medical autopsy as quality assurance tool in clinical medicine: Dreams and realities. Virchows Arch. 2015, 468, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Lax, S.F.; Skok, K.; Zechner, P.; Kessler, H.H.; Kaufmann, N.; Koelblinger, C.; Vander, K.; Bargfrieder, U.; Trauner, M. Pulmonary Arterial Thrombosis in COVID-19 With Fatal Outcome. Ann. Intern. Med. 2020, 173, 350–361. [Google Scholar] [CrossRef] [PubMed]
- Nienhold, R.; Ciani, Y.; Koelzer, V.H.; Tzankov, A.; Haslbauer, J.D.; Menter, T.; Schwab, N.; Henkel, M.; Frank, A.; Zsikla, V.; et al. Two distinct immunopathological profiles in autopsy lungs of COVID-19. Nat. Commun. 2020, 11, 1–13. [Google Scholar] [CrossRef]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Eckermann, M.; Frohn, J.; Reichardt, M.; Osterhoff, M.; Sprung, M.; Westermeier, F.; Tzankov, A.; Kühnel, M.; Jonigk, D.; Salditt, T. 3d virtual pathohistology of lung tissue from COVID-19 patients based on phase contrast x-ray tomography. eLife 2020, 9, 9. [Google Scholar] [CrossRef] [PubMed]
| Cause of Death | N | % |
|---|---|---|
| Cardiopulmonal failure | 54 | 29 |
| (predominant respiratory component) | (18) | (10) |
| Myocardial infarction | 21 | 11 |
| Neoplasm | 27 | 14 |
| Pneumonia | 20 | 11 |
| Sepsis or peritonitis | 12 | 6 |
| Gastrointestinal hemorrhage | 11 | 6 |
| Aortic rupture | 11 | 6 |
| Pulmonary embolism | 10 | 5 |
| Cerebral/cerebrovascular | 7 | 4 |
| Hepatic failure | 6 | 3 |
| Intestinal ischemia | 2 | 1 |
| Others | 8 | 4 |
| Total | 189 | 100 |
| Diagnosis | Congruent (Complete Agreement/Confirmation of A Suspected Clinical Finding) | Specific Postmortem Finding of An Unclear Clinical Finding | Discrepant (No Confirmation of A Suspected Specific Finding/New Specific Finding at Autopsy) |
|---|---|---|---|
| acute pneumonia | 16 | 3 | 10 |
| metastases | 4 | 0 | 5 |
| paracentral and peripheral embolism | 2 | 0 | 4 |
| primary pulmonary neoplasm | 15 | 1 | 1 |
| congestion | 42 | 3 | 6 |
| normal | 7 | 0 | 0 |
| organizing pneumonia | 2 | 0 | 1 |
| DAD | 9 | 1 | 2 |
| severe emphysema | 3 | 3 | 1 |
| central embolism | 5 | 0 | 2 |
| mild emphysema | 21 | 5 | 8 |
| fibrosis | 4 | 0 | 0 |
| other | 2 | 0 | 1 |
| total | 132 | 16 | 41 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berezowska, S.; Schmid, A.; Losmanová, T.; Trippel, M.; Blank, A.; Banz, Y.; Jakob, S.M.; Langer, R. Frequency and Significance of Pathologic Pulmonary Findings in Postmortem Examinations—A Single Center Experience before COVID-19. Diagnostics 2021, 11, 894. https://doi.org/10.3390/diagnostics11050894
Berezowska S, Schmid A, Losmanová T, Trippel M, Blank A, Banz Y, Jakob SM, Langer R. Frequency and Significance of Pathologic Pulmonary Findings in Postmortem Examinations—A Single Center Experience before COVID-19. Diagnostics. 2021; 11(5):894. https://doi.org/10.3390/diagnostics11050894
Chicago/Turabian StyleBerezowska, Sabina, Andreas Schmid, Tereza Losmanová, Mafalda Trippel, Annika Blank, Yara Banz, Stephan M. Jakob, and Rupert Langer. 2021. "Frequency and Significance of Pathologic Pulmonary Findings in Postmortem Examinations—A Single Center Experience before COVID-19" Diagnostics 11, no. 5: 894. https://doi.org/10.3390/diagnostics11050894
APA StyleBerezowska, S., Schmid, A., Losmanová, T., Trippel, M., Blank, A., Banz, Y., Jakob, S. M., & Langer, R. (2021). Frequency and Significance of Pathologic Pulmonary Findings in Postmortem Examinations—A Single Center Experience before COVID-19. Diagnostics, 11(5), 894. https://doi.org/10.3390/diagnostics11050894







