Sex Difference in the Risk of Dementia in Patients with Atrial Fibrillation
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Population
2.3. Study Outcome
2.4. Covariates
2.5. Ascertainment of AF and CHA2DS2-VASc Scoring
2.6. Statistical Analysis
2.7. Patient and Public Involvement
3. Results
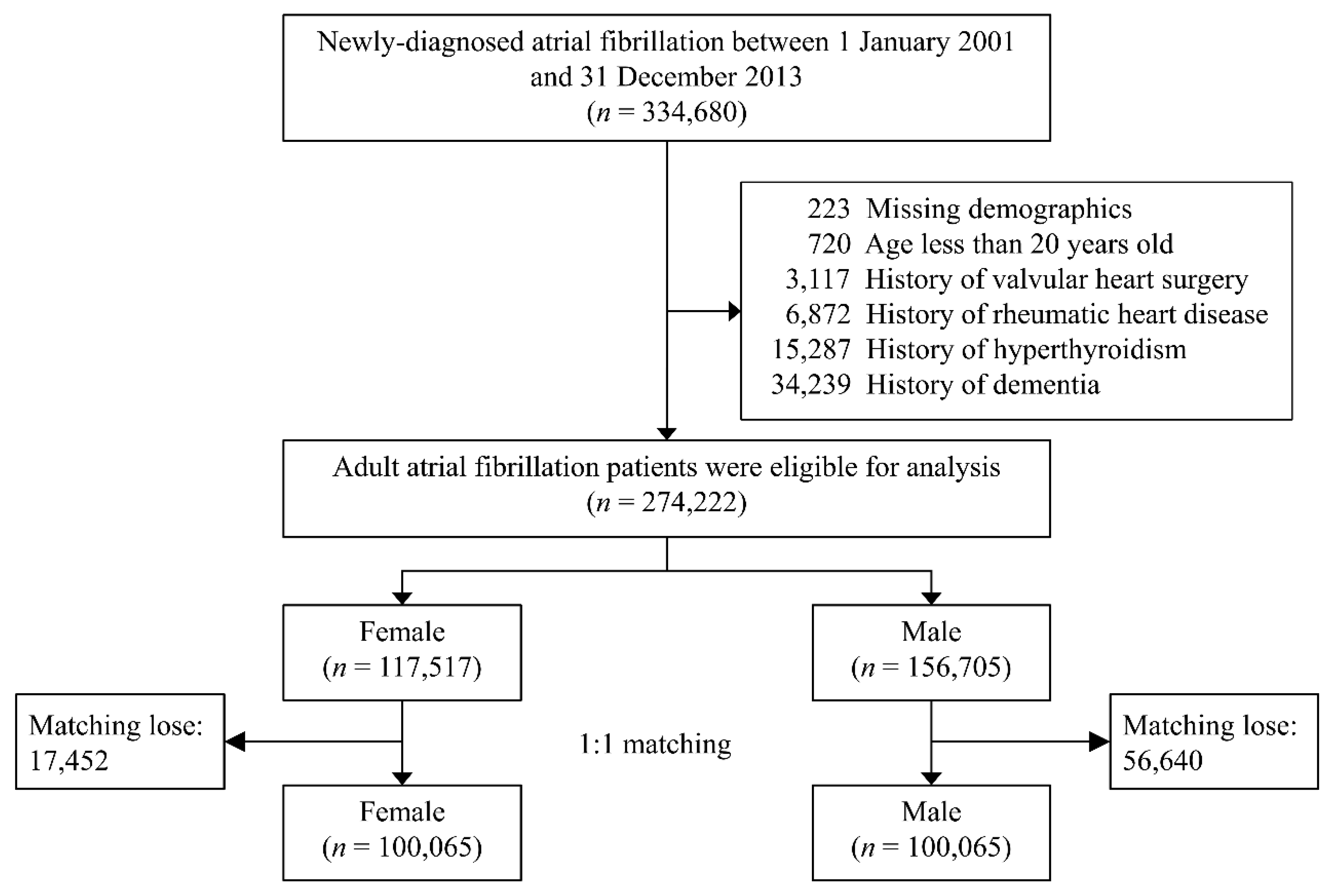
3.1. Study Population
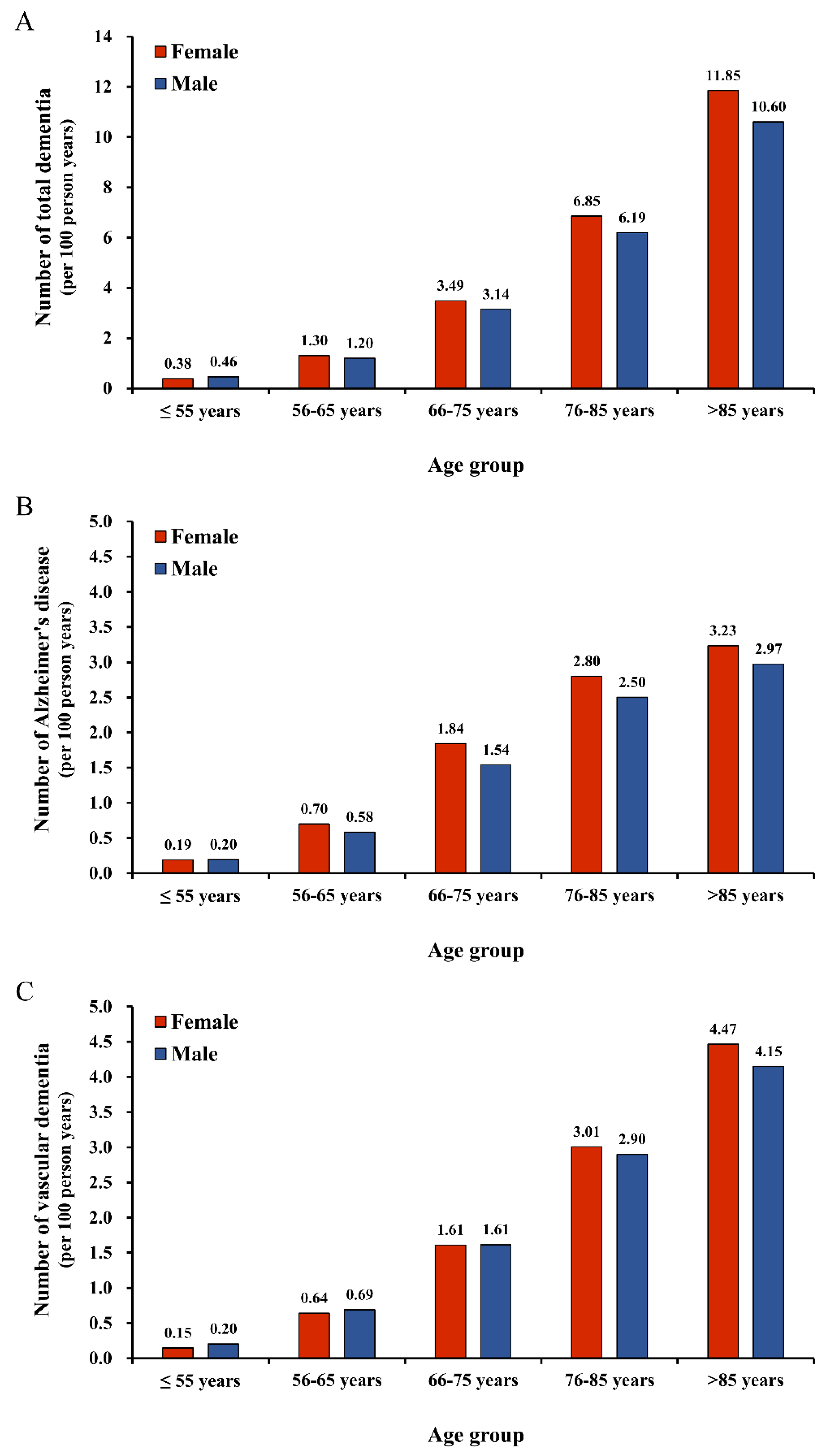
3.2. Dementia Risk Between Sexes Through Age-Stratified Analysis Before PSM
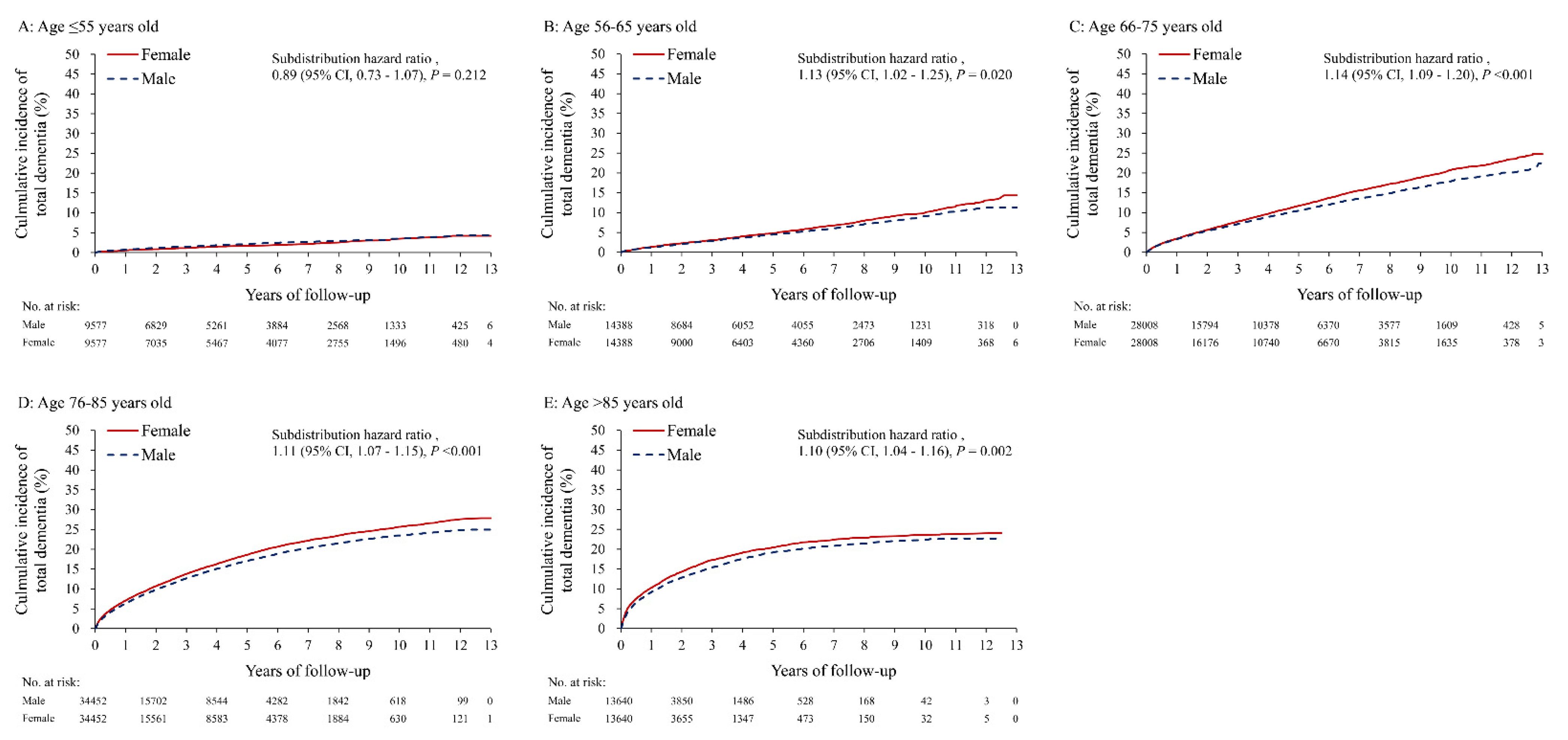
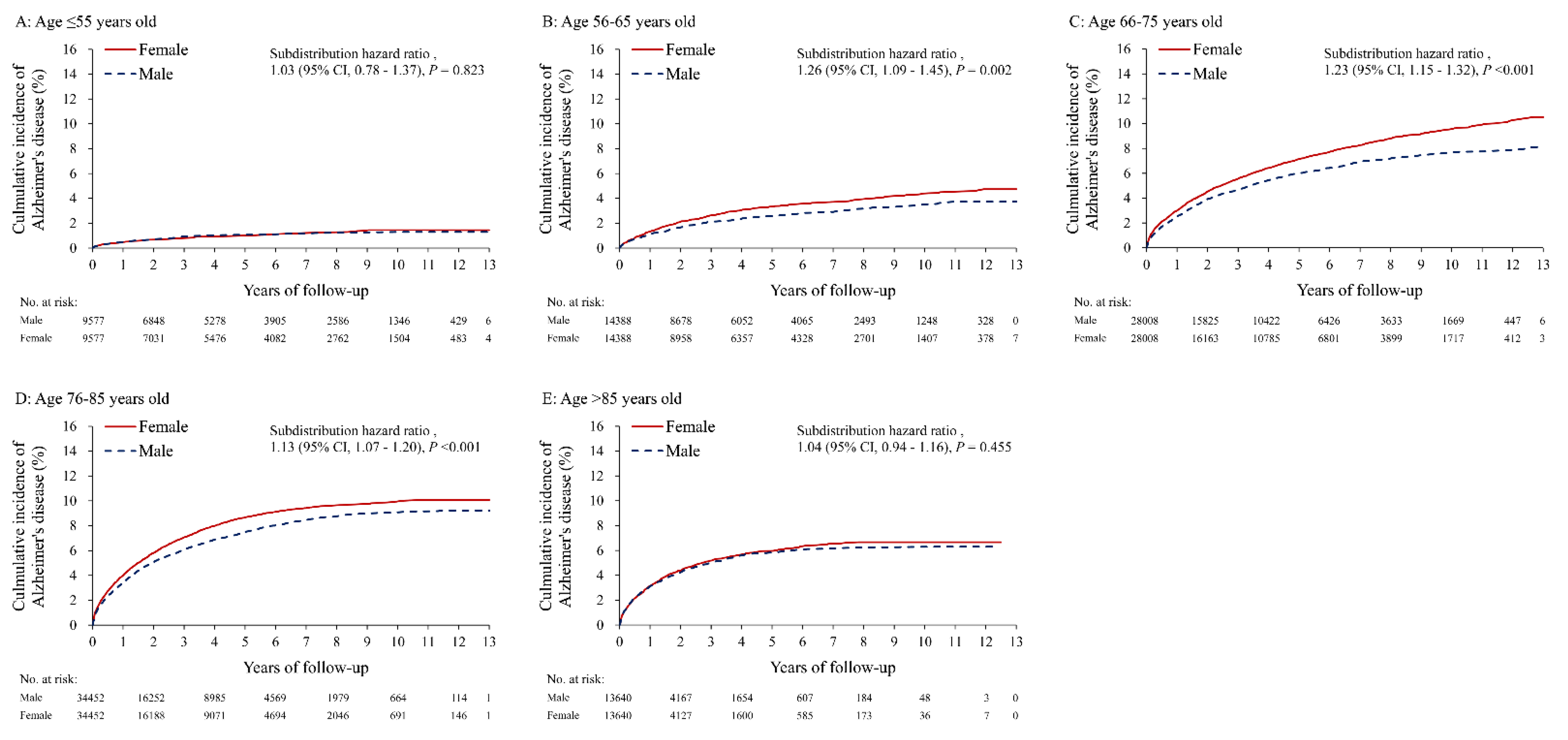
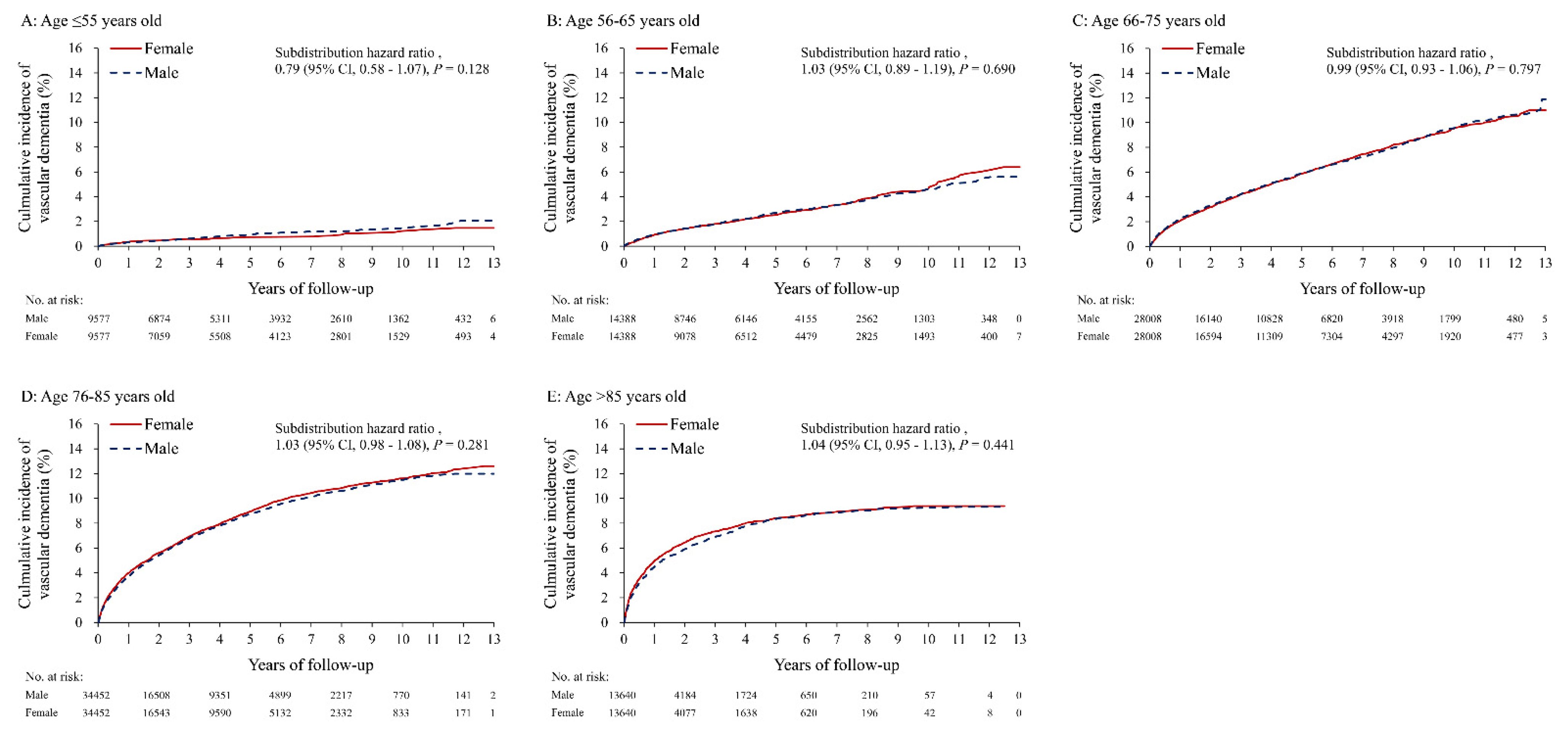
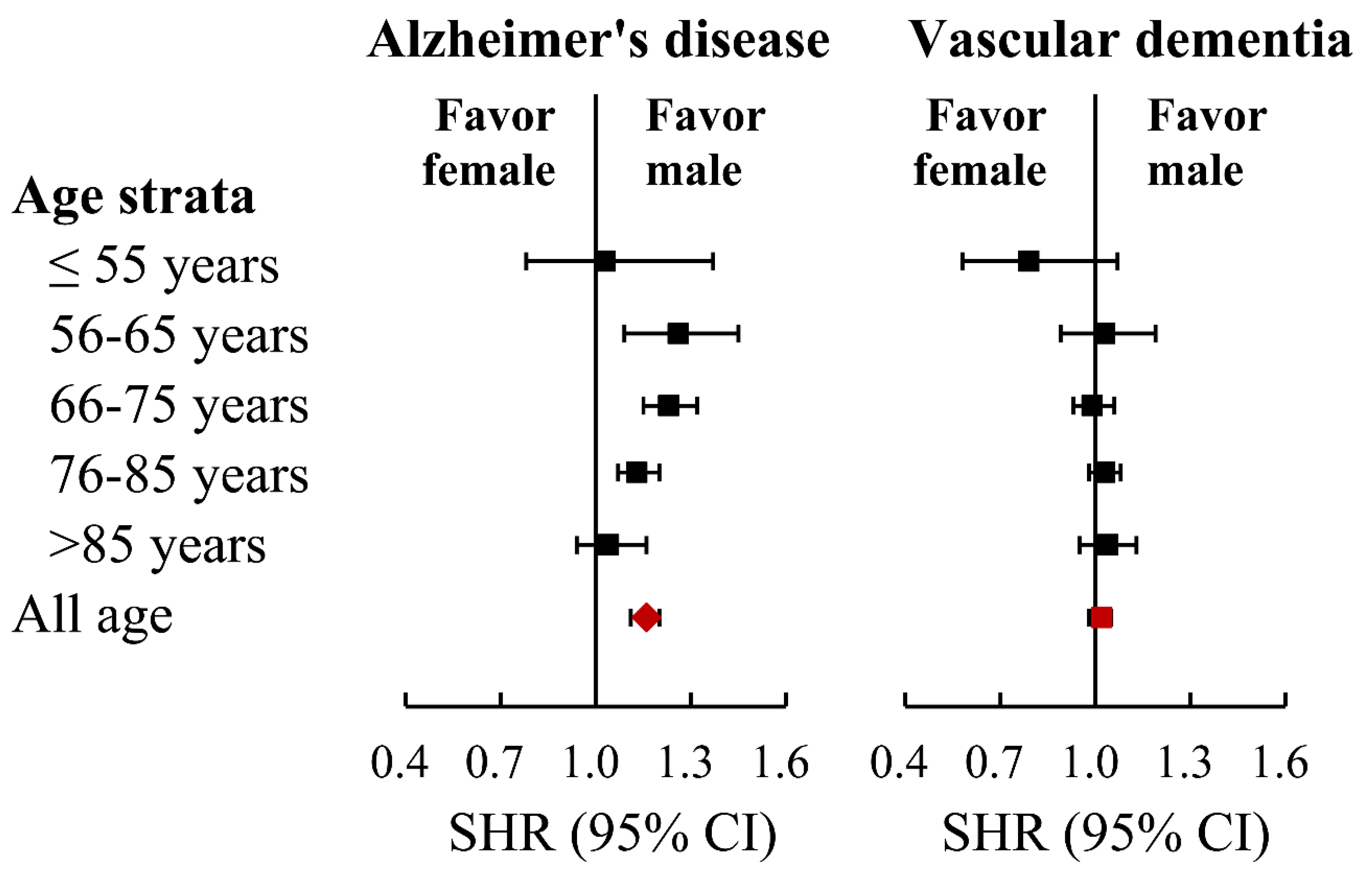
3.3. Risk of Developing Dementia between Sexes through Age-Stratified Analysis after PSM
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, L.Y.; Norby, F.L.; Gottesman, R.F.; Mosley, T.H.; Soliman, E.Z.; Agarwal, S.K.; Loehr, L.R.; Folsom, A.R.; Coresh, J.; Alonso, A. Association of Atrial Fibrillation with Cognitive Decline and Dementia Over 20 Years: The ARIC-NCS (Atherosclerosis Risk in Communities Neurocognitive Study). J. Am. Heart Assoc. 2018, 7, e007301. [Google Scholar] [CrossRef]
- Dublin, S.; Anderson, M.L.; Haneuse, S.J.; Heckbert, S.R.; Crane, P.K.; Breitner, J.C.; McCormick, W.; Bowen, J.D.; Teri, L.; McCurry, S.M.; et al. Atrial fibrillation and risk of dementia: A prospective cohort study. J. Am. Geriatr. Soc. 2011, 59, 1369–1375. [Google Scholar] [CrossRef]
- Santangeli, P.; Di Biase, L.; Bai, R.; Mohanty, S.; Pump, A.; Cereceda Brantes, M.; Horton, R.; Burkhardt, J.D.; Lakkireddy, D.; Reddy, Y.M.; et al. Atrial fibrillation and the risk of incident dementia: A meta-analysis. Heart Rhythm 2012, 9, 1761–17686. [Google Scholar] [CrossRef]
- Staerk, L.; Sherer, J.A.; Ko, D.; Benjamin, E.J.; Helm, R.H. Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes. Circ. Res. 2017, 120, 1501–1517. [Google Scholar] [CrossRef]
- Emdin, C.A.; Wong, C.X.; Hsiao, A.J.; Altman, D.G.; Peters, S.A.; Woodward, M.; Odutayo, A.A. Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: Systematic review and meta-analysis of cohort studies. BMJ 2016, 532, h7013. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, A.J.; Overvad, T.F.; Lip, G.Y.; Lane, D.A. Is female sex a risk factor for stroke and thromboembolism in patients with atrial fibrillation? A systematic review and meta-analysis. QJM 2014, 107, 955–967. [Google Scholar] [CrossRef] [PubMed]
- Niewada, M.; Kobayashi, A.; Sandercock, P.A.; Kaminski, B.; Czlonkowska, A. Influence of gender on baseline features and clinical outcomes among 17,370 patients with confirmed ischaemic stroke in the international stroke trial. Neuroepidemiology 2005, 24, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Rosamond, W.; Flegal, K.; Friday, G.; Furie, K.; Go, A.; Greenlund, K.; Haase, N.; Ho, M.; Howard, V.; Kissela, B.; et al. Heart disease and stroke statistics—2007 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2007, 115, e69–e171. [Google Scholar] [CrossRef]
- Renoux, C.; Coulombe, J.; Suissa, S. Revisiting sex differences in outcomes in non-valvular atrial fibrillation: A population-based cohort study. Eur. Heart J. 2017, 38, 1473–1479. [Google Scholar] [CrossRef] [PubMed]
- Wu, V.C.; Wu, M.; Aboyans, V.; Chang, S.H.; Chen, S.W.; Chen, M.C.; Wang, C.L.; Hsieh, I.C.; Chu, P.H.; Lin, Y.S. Female sex as a risk factor for ischaemic stroke varies with age in patients with atrial fibrillation. Heart 2020, 106, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Tatemichi, T.K.; Paik, M.; Bagiella, E.; Desmond, D.W.; Stern, Y.; Sano, M.; Hauser, W.A.; Mayeux, R. Risk of dementia after stroke in a hospitalized cohort: Results of a longitudinal study. Neurology 1994, 44, 1885–1891. [Google Scholar] [CrossRef]
- Pohjasvaara, T.; Erkinjuntti, T.; Vataja, R.; Kaste, M. Dementia three months after stroke: Baseline frequency and effect of different definitions of dementia in the Helsinki Stroke Aging Memory Study (SAM) cohort. Stroke 1997, 28, 785–792. [Google Scholar] [CrossRef]
- Desmond, D.W.; Moroney, J.T.; Sano, M.; Stern, Y. Incidence of dementia after ischemic stroke: Results of a longitudinal study. Stroke 2002, 33, 2254–2260. [Google Scholar] [CrossRef]
- Alzheimer’s Association. Alzheimer’s disease facts and figures. Alzheimer Dement. 2017, 13, 325–373. [Google Scholar]
- Beam, C.R.; Kaneshiro, C.; Jang, J.Y.; Reynolds, C.A.; Pedersen, N.L.; Gatz, M. Differences Between Women and Men in Incidence Rates of Dementia and Alzheimer’s Disease. J. Alzheimers Dis. 2018, 64, 1077–1083. [Google Scholar] [CrossRef] [PubMed]
- Plassman, B.L.; Langa, K.M.; Fisher, G.G.; Heeringa, S.G.; Weir, D.R.; Ofstedal, M.B.; Burke, J.R.; Hurd, M.D.; Potter, G.G.; Rodgers, W.L.; et al. Prevalence of dementia in the United States: The aging, demographics, and memory study. Neuroepidemiology 2007, 29, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Edland, S.D.; Rocca, W.A.; Petersen, R.C.; Cha, R.H.; Kokmen, E. Dementia and Alzheimer disease incidence rates do not vary by sex in Rochester, Minn. Arch. Neurol. 2002, 59, 1589–1593. [Google Scholar] [CrossRef] [PubMed]
- Fratiglioni, L.; Viitanen, M.; von Strauss, E.; Tontodonati, V.; Herlitz, A.; Winblad, B. Very old women at highest risk of dementia and Alzheimer’s disease: Incidence data from the Kungsholmen Project, Stockholm. Neurology 1997, 48, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Letenneur, L.; Gilleron, V.; Commenges, D.; Helmer, C.; Orgogozo, J.M.; Dartigues, J.F. Are sex and educational level independent predictors of dementia and Alzheimer’s disease? Incidence data from the PAQUID project. J. Neurol. Neurosurg. Psychiatry 1999, 66, 177–183. [Google Scholar] [CrossRef]
- Matthews, F.E.; Stephan, B.C.; Robinson, L.; Jagger, C.; Barnes, L.E.; Arthur, A.; Brayne, C.; Cognitive, F.; Ageing Studies, C. A two decade dementia incidence comparison from the Cognitive Function and Ageing Studies I and II. Nat. Commun. 2016, 7, 11398. [Google Scholar] [CrossRef]
- Hsieh, C.Y.; Chen, C.H.; Li, C.Y.; Lai, M.L. Validating the diagnosis of acute ischemic stroke in a National Health Insurance claims database. J. Formos. Med. Assoc. 2015, 114, 254–259. [Google Scholar] [CrossRef]
- Chen, C.W.; Lin, C.C.; Chen, K.B.; Kuo, Y.C.; Li, C.Y.; Chung, C.J. Increased risk of dementia in people with previous exposure to general anesthesia: A nationwide population-based case-control study. Alzheimer Dement. 2014, 10, 196–204. [Google Scholar] [CrossRef]
- Zhang, B.; Wang, H.E.; Bai, Y.M.; Tsai, S.J.; Su, T.P.; Chen, T.J.; Wang, Y.P.; Chen, M.H. Inflammatory bowel disease is associated with higher dementia risk: A nationwide longitudinal study. Gut 2021, 70, 85–91. [Google Scholar] [CrossRef]
- Cheng, C.L.; Lee, C.H.; Chen, P.S.; Li, Y.H.; Lin, S.J.; Yang, Y.H. Validation of acute myocardial infarction cases in the national health insurance research database in taiwan. J. Epidemiol. 2014, 24, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Lai, M.S.; Syu, C.Y.; Chang, S.C.; Tseng, F.Y. Accuracy of diabetes diagnosis in health insurance claims data in Taiwan. J. Formos. Med. Assoc. 2005, 104, 157–163. [Google Scholar] [PubMed]
- Chang, C.H.; Lee, Y.C.; Tsai, C.T.; Chang, S.N.; Chung, Y.H.; Lin, M.S.; Lin, J.W.; Lai, M.S. Continuation of statin therapy and a decreased risk of atrial fibrillation/flutter in patients with and without chronic kidney disease. Atherosclerosis 2014, 232, 224–230. [Google Scholar] [CrossRef]
- Lin, L.J.; Cheng, M.H.; Lee, C.H.; Wung, D.C.; Cheng, C.L.; Kao Yang, Y.H. Compliance with antithrombotic prescribing guidelines for patients with atrial fibrillation—A nationwide descriptive study in Taiwan. Clin. Ther. 2008, 30, 1726–1736. [Google Scholar] [CrossRef] [PubMed]
- Miyasaka, Y.; Barnes, M.E.; Petersen, R.C.; Cha, S.S.; Bailey, K.R.; Gersh, B.J.; Casaclang-Verzosa, G.; Abhayaratna, W.P.; Seward, J.B.; Iwasaka, T.; et al. Risk of dementia in stroke-free patients diagnosed with atrial fibrillation: Data from a community-based cohort. Eur. Heart J. 2007, 28, 1962–1967. [Google Scholar] [CrossRef]
- Rocca, W.A. Time, Sex, Gender, History, and Dementia. Alzheimer Dis. Assoc. Disord. 2017, 31, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Mielke, M.M.; Vemuri, P.; Rocca, W.A. Clinical epidemiology of Alzheimer’s disease: Assessing sex and gender differences. Clin. Epidemiol. 2014, 6, 37–48. [Google Scholar] [CrossRef]
- Goette, A.; Rocken, C. Atrial amyloidosis and atrial fibrillation: A gender-dependent “arrhythmogenic substrate”? Eur. Heart J. 2004, 25, 1185–1186. [Google Scholar] [CrossRef] [PubMed]
- Leone, O.; Boriani, G.; Chiappini, B.; Pacini, D.; Cenacchi, G.; Martin Suarez, S.; Rapezzi, C.; Bacchi Reggiani, M.L.; Marinelli, G. Amyloid deposition as a cause of atrial remodelling in persistent valvular atrial fibrillation. Eur. Heart J. 2004, 25, 1237–1241. [Google Scholar] [CrossRef] [PubMed]
- Golive, A.; May, H.T.; Bair, T.L.; Jacobs, V.; Crandall, B.G.; Cutler, M.J.; Day, J.D.; Mallender, C.; Osborn, J.S.; Weiss, J.P.; et al. The Impact of gender on atrial fibrillation incidence and progression to dementia. Am. J. Cardiol. 2018, 122, 1489–1495. [Google Scholar] [CrossRef] [PubMed]
- Joundi, R.A.; Cipriano, L.E.; Sposato, L.A.; Saposnik, G. Stroke Outcomes Research Working, G. Ischemic stroke risk in patients with atrial fibrillation and CHA2DS2-VASc score of 1: Systematic Review and Meta-Analysis. Stroke 2016, 47, 1364–1367. [Google Scholar] [CrossRef]
- Pistoia, F.; Sacco, S.; Tiseo, C.; Degan, D.; Ornello, R.; Carolei, A. The epidemiology of atrial fibrillation and stroke. Cardiol. Clin. 2016, 34, 255–268. [Google Scholar] [CrossRef]
- Wandell, P.; Carlsson, A.C.; Sundquist, J.; Sundquist, K. The association between relevant comorbidities and dementia in patients with atrial fibrillation. Geroscience 2018, 40, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Bushnell, C.; McCullough, L.D.; Awad, I.A.; Chireau, M.V.; Fedder, W.N.; Furie, K.L.; Howard, V.J.; Lichtman, J.H.; Lisabeth, L.D.; Pina, I.L.; et al. Guidelines for the prevention of stroke in women: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014, 45, 1545–1588. [Google Scholar] [CrossRef]
- LaCroix, A.Z.; Guralnik, J.M.; Curb, J.D.; Wallace, R.B.; Ostfeld, A.M.; Hennekens, C.H. Chest pain and coronary heart disease mortality among older men and women in three communities. Circulation 1990, 81, 437–446. [Google Scholar] [CrossRef] [PubMed]
| Disease | ICD-9 CM Disease Code |
|---|---|
| Study Cohorts | |
| Atrial fibrillation (AF) | 427.31 |
| Excluding Diseases | |
| Rheumatic heart disease | 394.0, 394.1, 394.2, 395, 398.9 |
| Hyperthyroidism | 242 and any anti-thyroid drugs |
| Main outcome | |
| Dementia | 290.x, 294.x, 331.0 |
| Alzheimer disease | 331.0 |
| Vascular dementia | 290.4x with PET/SPECT |
| Comorbidities | |
| Hypertension | 401, 402, 403, 404, 405 and any anti-hypertension drugs |
| Diabetes mellitus | 250 and any oral hypoglycemic drugs or insulin |
| Ischemic heart disease | 410.x~414.x |
| Dyslipidemia | 272 and any lipid-lowing agents |
| Gout | 274.x |
| Chronic obstructive pulmonary disease | 491.x, 492.x, 496.x |
| Peripheral arterial disease (PAD) | 093.0, 437.3, 440.x, 441.x, 443.x, 444.0x, 444.22, 444.8x, 447.1, 447.8x, 447.9x, 557.1, 557.9, V43.4 |
| Chronic kidney disease | 580.x~589.x, 403.x~404.x, 016.0, 095.4, 236.9 250.4, 274.1, 442.1, 447.3, 440.1, 572.4, 642.1, 646.2, 753.1, 283.11, 403.01, 404.02, 446.21 |
| Dialysis | 585 |
| Abnormal liver function | 070, 456.0~456.2, 570, 571, 572.2~572.8, 573, V42.7 |
| Traumatic brain injury | 800.x~804.x, 850.x~854.x |
| Alcohol abuse | V113, 291.x, 305.0x, 357.5, 425.5, 303.x, 571.0, 571.1, 571.2, 571.3, 980.0 |
| Systemic thromboembolism | 415.1x, 444.22, 444.81, 444.21, 362.30, 362.34, 444.89, 557.0, 444.9x |
| Ischemic stroke | 433.x~437.x |
| Myocardial infarction | 410.x, 412.x |
| Stroke | 430.x~437.x |
| Heart failure | 428.x |
| Depression | 296.2x, 296.3x |
| Bipolar | 296.x |
| Before Matching | After Matching | ||||||
|---|---|---|---|---|---|---|---|
| Variables | Total (n = 274,222) | Female (n = 117,517) | Male (n = 156,705) | STD | Female (n = 100,065) | Male (n = 100,065) | STD |
| Age (years) | 71.8 ± 13.2 | 73.8 ± 12.4 | 70.2 ± 13.5 | 0.28 | 72.5 ± 12.5 | 72.5 ± 12.5 | 0.00 |
| Age group | |||||||
| ≤55 years | 31,738 (11.6) | 9641 (8.2) | 22,097 (14.1) | −0.19 | 9577 (9.6) | 9577 (9.6) | 0.00 |
| 56–65 years | 41,497 (15.1) | 14,788 (12.6) | 26,709 (17.0) | −0.13 | 14,388 (14.4) | 14,388 (14.4) | 0.00 |
| 66–75 years | 72,265 (26.4) | 30,993 (26.4) | 41,272 (26.3) | 0.00 | 28,008 (28.0) | 28,008 (28.0) | 0.00 |
| 76–85 years | 91,424 (33.3) | 41,927 (35.7) | 49,497 (31.6) | 0.09 | 34,452 (34.4) | 34,452 (34.4) | 0.00 |
| >85 years | 37,298 (13.6) | 20,168 (17.2) | 17,130 (10.9) | 0.18 | 13,640 (13.6) | 13,640 (13.6) | 0.00 |
| Monthly income, USD | |||||||
| ≤600 | 166,993 (60.9) | 72,897 (62.0) | 94,096 (60.0) | 0.04 | 63,393 (63.4) | 63,480 (63.4) | 0.00 |
| 601–800 | 86,118 (31.4) | 39,507 (33.6) | 46,611 (29.7) | 0.08 | 31,566 (31.5) | 31,480 (31.5) | 0.00 |
| >800 | 21,111 (7.7) | 5113 (4.4) | 15,998 (10.2) | −0.23 | 5106 (5.1) | 5105 (5.1) | 0.00 |
| Urbanization level | |||||||
| Low | 39,115 (14.3) | 18,071 (15.4) | 21,044 (13.4) | 0.06 | 14,249 (14.2) | 14,304 (14.3) | 0.00 |
| Moderate | 89,523 (32.6) | 38,516 (32.8) | 51,007 (32.5) | 0.00 | 32,521 (32.5) | 32,532 (32.5) | 0.00 |
| High | 80,059 (29.2) | 33,046 (28.1) | 47,013 (30.0) | −0.04 | 29,279 (29.3) | 29,196 (29.2) | 0.00 |
| Very high | 65,525 (23.9) | 27,884 (23.7) | 37,641 (24.0) | −0.01 | 24,016 (24.0) | 24,033 (24.0) | 0.00 |
| Comorbidities | |||||||
| Hypertension | 173,413 (63.2) | 79,158 (67.4) | 94,255 (60.1) | 0.15 | 64,159 (64.1) | 64,092 (64.1) | 0.00 |
| Diabetes mellitus | 69,355 (25.3) | 33,120 (28.2) | 36,235 (23.1) | 0.12 | 25,859 (25.8) | 25,817 (25.8) | 0.00 |
| Ischemic heart disease | 101,722 (37.1) | 42,706 (36.3) | 59,016 (37.7) | −0.03 | 36,186 (36.2) | 36,202 (36.2) | 0.00 |
| Dyslipidemia | 49,457 (18.0) | 22,705 (19.3) | 26,752 (17.1) | 0.06 | 17,867 (17.9) | 17,710 (17.7) | 0.00 |
| Gout | 28,848 (10.5) | 7359 (6.3) | 21,489 (13.7) | −0.25 | 7253 (7.2) | 7236 (7.2) | 0.00 |
| COPD | 51,732 (18.9) | 15,261 (13.0) | 36,471 (23.3) | −0.27 | 15,048 (15.0) | 14,909 (14.9) | 0.00 |
| Peripheral arterial disease | 13,311 (4.9) | 5689 (4.8) | 7622 (4.9) | 0.00 | 4810 (4.8) | 4790 (4.8) | 0.00 |
| Renal function status | |||||||
| Non-CKD | 235,735 (86.0) | 101,229 (86.1) | 134,506 (85.8) | 0.01 | 86,351 (86.3) | 86,316 (86.3) | 0.00 |
| CKD without dialysis | 30,624 (11.2) | 12,141 (10.3) | 18,483 (11.8) | −0.05 | 10,640 (10.6) | 10,745 (10.7) | 0.00 |
| CKD with dialysis | 7863 (2.9) | 4147 (3.5) | 3716 (2.4) | 0.07 | 3074 (3.1) | 3004 (3.0) | 0.00 |
| Abnormal liver function | 30,337 (11.1) | 11,303 (9.6) | 19,034 (12.1) | −0.08 | 10,107 (10.1) | 10,079 (10.1) | 0.00 |
| Traumatic brain injury | 5531 (2.0) | 2111 (1.8) | 3420 (2.2) | −0.03 | 1920 (1.9) | 1934 (1.9) | 0.00 |
| Alcohol abuse | 2767 (1.0) | 223 (0.2) | 2544 (1.6) | −0.15 | 223 (0.2) | 233 (0.2) | 0.00 |
| History of events | |||||||
| Systemic thromboembolism (excluding ischemic stroke) | 4708 (1.7) | 2093 (1.8) | 2615 (1.7) | 0.01 | 1694 (1.7) | 1656 (1.7) | 0.00 |
| Myocardial infarction | 11,916 (4.3) | 3796 (3.2) | 8120 (5.2) | −0.10 | 3559 (3.6) | 3555 (3.6) | 0.00 |
| Stroke | 37,376 (13.6) | 16,501 (14.0) | 20,875 (13.3) | 0.02 | 13,639 (13.6) | 13,613 (13.6) | 0.00 |
| Heart failure | 34,697 (12.7) | 16,456 (14.0) | 18,241 (11.6) | 0.07 | 12,207 (12.2) | 12,164 (12.2) | 0.00 |
| History of psychosis | |||||||
| Depression | 1896 (0.7) | 1010 (0.9) | 886 (0.6) | 0.03 | 708 (0.7) | 670 (0.7) | 0.00 |
| Bipolar | 2889 (1.1) | 1483 (1.3) | 1406 (0.9) | 0.04 | 1081 (1.1) | 1022 (1.0) | 0.01 |
| Medications | |||||||
| Anticoagulant | 62,373 (22.7) | 26,406 (22.5) | 35,967 (23.0) | −0.01 | 22,955 (22.9) | 23,032 (23.0) | 0.00 |
| Antiplatelet | 94,571 (34.5) | 38,573 (32.8) | 55,998 (35.7) | −0.06 | 33,646 (33.6) | 33,692 (33.7) | 0.00 |
| ACEi/ARB | 113,312 (41.3) | 50,462 (42.9) | 62,850 (40.1) | 0.06 | 41,141 (41.1) | 41,008 (41.0) | 0.00 |
| Dihydropyridine CCB | 68,488 (25.0) | 32,585 (27.7) | 35,903 (22.9) | 0.11 | 25,692 (25.7) | 25,564 (25.5) | 0.00 |
| Non-dihydropyridine CCB | 46,929 (17.1) | 21,102 (18.0) | 25,827 (16.5) | 0.04 | 17,314 (17.3) | 17,198 (17.2) | 0.00 |
| ß-blockers | 93,261 (34.0) | 42,680 (36.3) | 50,581 (32.3) | 0.09 | 34,887 (34.9) | 34,622 (34.6) | 0.01 |
| Statins | 32,312 (11.8) | 14,409 (12.3) | 17,903 (11.4) | 0.03 | 11,696 (11.7) | 11,547 (11.5) | 0.00 |
| DPP4 inhibitors | 5604 (2.0) | 2560 (2.2) | 3044 (1.9) | 0.02 | 2053 (2.1) | 2093 (2.1) | 0.00 |
| Biguanides | 26,651 (9.7) | 12,758 (10.9) | 13,893 (8.9) | 0.07 | 10,094 (10.1) | 10,014 (10.0) | 0.00 |
| Sulfonylurea | 29,146 (10.6) | 13,916 (11.8) | 15,230 (9.7) | 0.07 | 10,967 (11.0) | 10,971 (11.0) | 0.00 |
| Thiazolidinedione | 3769 (1.4) | 1808 (1.5) | 1961 (1.3) | 0.02 | 1488 (1.5) | 1454 (1.5) | 0.00 |
| Insulin | 8563 (3.1) | 4471 (3.8) | 4092 (2.6) | 0.07 | 3237 (3.2) | 3160 (3.2) | 0.00 |
| CHA2DS2-VASc score * | 3.3 ± 1.9 | 4.1 ± 1.7 | 2.8 ± 1.7 | 0.79 | 4.0 ± 1.7 | 2.9 ± 1.7 | 0.58 |
| CHA2DS2-VASc score group * | |||||||
| 0 | 16,156 (5.9) | 0 (0.0) | 16,156 (10.3) | −0.48 | 0 (0.0) | 8718 (8.7) | −0.44 |
| 1 | 31,510 (11.5) | 9137 (7.8) | 22,373 (14.3) | −0.21 | 9064 (9.1) | 11,465 (11.5) | −0.08 |
| 2 | 44,829 (16.3) | 11,474 (9.8) | 33,355 (21.3) | −0.32 | 11,324 (11.3) | 20,077 (20.1) | −0.24 |
| 3 | 56,571 (20.6) | 21,578 (18.4) | 34,993 (22.3) | −0.10 | 19,981 (20.0) | 24,109 (24.1) | −0.10 |
| 4 | 54,259 (19.8) | 28,785 (24.5) | 25,474 (16.3) | 0.21 | 23,928 (23.9) | 18,193 (18.2) | 0.14 |
| 5 | 36,594 (13.3) | 22,812 (19.4) | 13,782 (8.8) | 0.31 | 17,865 (17.9) | 9863 (9.9) | 0.23 |
| 6 | 20,074 (7.3) | 12,976 (11.0) | 7098 (4.5) | 0.24 | 9880 (9.9) | 5082 (5.1) | 0.18 |
| 7–9 | 14,229 (5.2) | 10,755 (9.2) | 3474 (2.2) | 0.30 | 8023 (8.0) | 2558 (2.6) | 0.25 |
| Follow-up years * | 3.4 ± 3.3 | 3.5 ± 3.3 | 3.4 ± 3.3 | 0.02 | 3.5 ± 3.4 | 3.4 ± 3.3 | 0.03 |
| Propensity score | 0.429 ± 0.159 | 0.488 ± 0.145 | 0.384 ± 0.155 | 0.69 | 0.457 ± 0.132 | 0.456 ± 0.132 | 0.01 |
| Type of Dementia/Age | Female (n = 100,065) | Male (n = 100,065) | Female vs. Male | |||||
|---|---|---|---|---|---|---|---|---|
| Patient | Event (%) | ID (95% CI) | Patient | Event (%) | ID (95% CI) | SHR (95% CI) | p-Value | |
| Any dementia | ||||||||
| ≤55 years | 9577 | 198 (2.1) | 0.39 (0.33–0.44) | 9577 | 223 (2.3) | 0.45 (0.39–0.51) | 0.89 (0.73–1.07) | 0.212 |
| 56–65 years | 14,388 | 780 (5.4) | 1.28 (1.19–1.37) | 14,388 | 696 (4.8) | 1.20 (1.11–1.29) | 1.13 (1.02–1.25) | 0.020 |
| 66–75 years | 28,008 | 3478 (12.4) | 3.40 (3.29–3.52) | 28,008 | 3087 (11.0) | 3.10 (2.99–3.21) | 1.14 (1.09–1.20) | <0.001 |
| 76–85 years | 34,452 | 6022 (17.5) | 6.78 (6.61–6.95) | 34,452 | 5500 (16.0) | 6.18 (6.02–6.34) | 1.11 (1.07–1.15) | <0.001 |
| >85 years | 13,640 | 2389 (17.5) | 11.94 (11.46–12.42) | 13,640 | 2211 (16.2) | 10.40 (9.97–10.83) | 1.10 (1.04–1.16) | 0.002 |
| Total | 100,065 | 12,867 (12.9) | 3.98 (3.91–4.05) | 100,065 | 11,717 (11.7) | 3.70 (3.63–3.77) | 1.11 (1.08–1.14) | <0.001 |
| Alzheimer’s disease | ||||||||
| ≤55 years | 9577 | 98 (1.0) | 0.19 (0.15–0.23) | 9577 | 95 (1.0) | 0.19 (0.15–0.23) | 1.03 (0.78–1.37) | 0.823 |
| 56–65 years | 14,388 | 415 (2.9) | 0.69 (0.62–0.75) | 14,388 | 333 (2.3) | 0.58 (0.51–0.64) | 1.26 (1.09–1.45) | 0.002 |
| 66–75 years | 28,008 | 1856 (6.6) | 1.80 (1.72–1.89) | 28,008 | 1521 (5.4) | 1.52 (1.44–1.60) | 1.23 (1.15–1.32) | <0.001 |
| 76–85 years | 34,452 | 2593 (7.5) | 2.80 (2.70–2.91) | 34,452 | 2309 (6.7) | 2.50 (2.40–2.60) | 1.13 (1.07–1.20) | <0.001 |
| >85 years | 13,640 | 693 (5.1) | 3.13 (2.89–3.36) | 13,640 | 667 (4.9) | 2.93 (2.71–3.15) | 1.04 (0.94–1.16) | 0.455 |
| Total | 100,065 | 5655 (5.7) | 1.72 (1.67–1.76) | 100,065 | 4925 (4.9) | 1.53 (1.48–1.57) | 1.16 (1.11–1.20) | <0.001 |
| Vascular dementia | ||||||||
| ≤55 years | 9577 | 76 (0.8) | 0.15 (0.11–0.18) | 9577 | 96 (1.0) | 0.19 (0.15–0.23) | 0.79 (0.58–1.07) | 0.128 |
| 56–65 years | 14,388 | 391 (2.7) | 0.63 (0.57–0.69) | 14,388 | 381 (2.7) | 0.65 (0.58–0.71) | 1.03 (0.89–1.19) | 0.690 |
| 66–75 years | 28,008 | 1674 (6.0) | 1.56 (1.48–1.63) | 28,008 | 1691 (6.0) | 1.64 (1.56–1.72) | 0.99 (0.93–1.06) | 0.797 |
| 76–85 years | 34,452 | 2854 (8.3) | 2.97 (2.86–3.08) | 34,452 | 2785 (8.1) | 2.93 (2.82–3.04) | 1.03 (0.98–1.08) | 0.281 |
| >85 years | 13,640 | 988 (7.2) | 4.45 (4.17–4.73) | 13,640 | 960 (7.0) | 4.16 (3.90–4.43) | 1.04 (0.95–1.13) | 0.441 |
| Total | 100,065 | 5983 (6.0) | 1.76 (1.72–1.81) | 100,065 | 5913 (5.9) | 1.79 (1.75–1.84) | 1.02 (0.98–1.05) | 0.429 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-L.; Chen, J.; Wang, H.-T.; Chang, Y.-T.; Chong, S.-Z.; Hsueh, S.; Chung, C.-M.; Lin, Y.-S. Sex Difference in the Risk of Dementia in Patients with Atrial Fibrillation. Diagnostics 2021, 11, 760. https://doi.org/10.3390/diagnostics11050760
Chen Y-L, Chen J, Wang H-T, Chang Y-T, Chong S-Z, Hsueh S, Chung C-M, Lin Y-S. Sex Difference in the Risk of Dementia in Patients with Atrial Fibrillation. Diagnostics. 2021; 11(5):760. https://doi.org/10.3390/diagnostics11050760
Chicago/Turabian StyleChen, Yung-Lung, Joseph Chen, Hui-Ting Wang, Ya-Ting Chang, Shaur-Zheng Chong, Shukai Hsueh, Chang-Ming Chung, and Yu-Sheng Lin. 2021. "Sex Difference in the Risk of Dementia in Patients with Atrial Fibrillation" Diagnostics 11, no. 5: 760. https://doi.org/10.3390/diagnostics11050760
APA StyleChen, Y.-L., Chen, J., Wang, H.-T., Chang, Y.-T., Chong, S.-Z., Hsueh, S., Chung, C.-M., & Lin, Y.-S. (2021). Sex Difference in the Risk of Dementia in Patients with Atrial Fibrillation. Diagnostics, 11(5), 760. https://doi.org/10.3390/diagnostics11050760






