Clinical Outcomes between P1 and P0 Lesions for Obscure Gastrointestinal Bleeding with Negative Computed Tomography and Capsule Endoscopy
Abstract
1. Introduction
2. Methods
2.1. Study Design and Patients
2.2. Capsule Endoscopy and Abdominal CT Procedures
2.3. Statistical Analysis
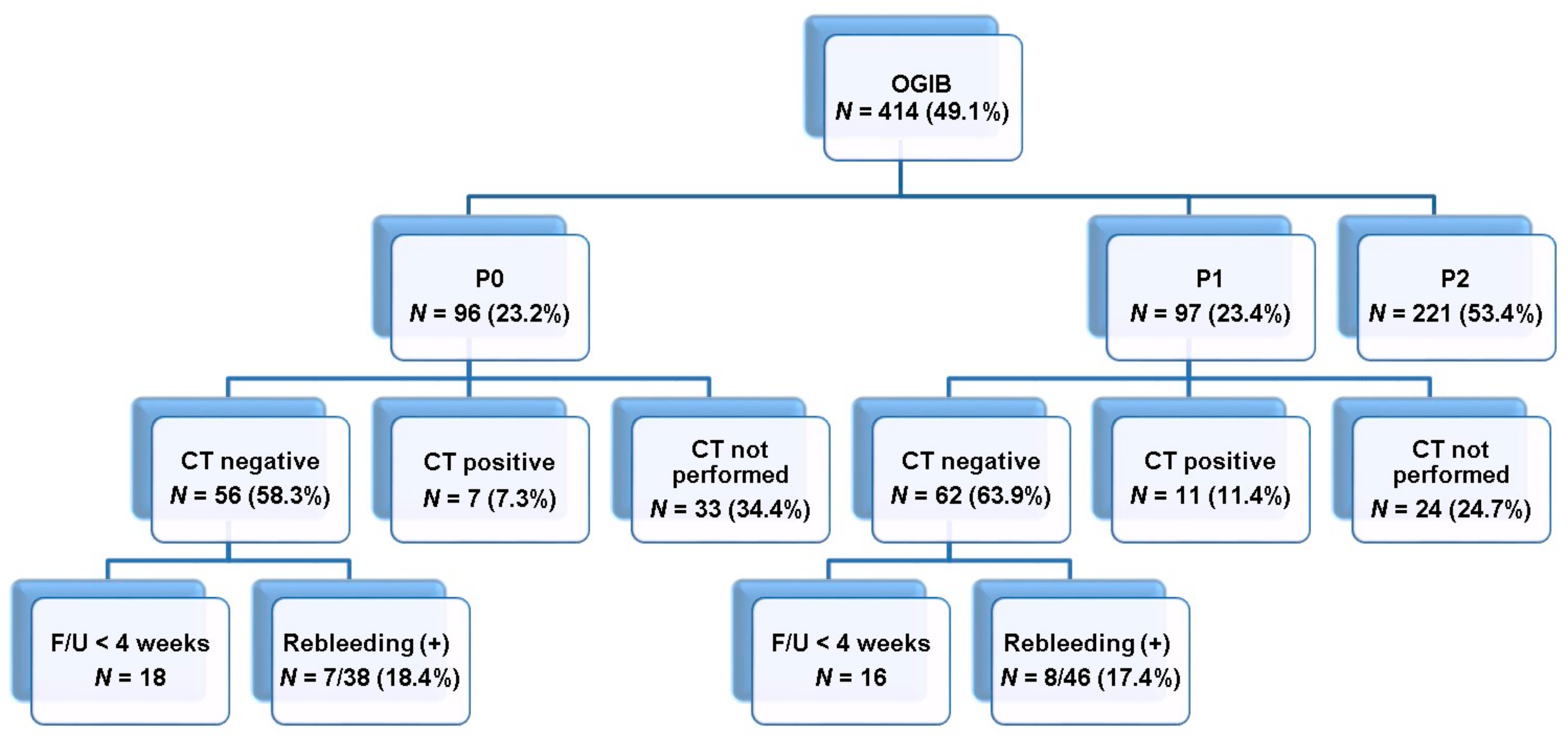
3. Results
3.1. Baseline Characteristics
3.2. Capsule Endoscopy-Related Data
3.3. Rebleeding Analysis
3.4. Rebleeding Risk Factors Analysis
3.5. Clinical Outcome and Treatment of Rebleeding Patients
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gerson, L.B.; Fidler, J.L.; Cave, D.R.; Leighton, J.A. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am. J. Gastroenterol. 2015, 110, 1265–1287. [Google Scholar] [CrossRef]
- Song, H.J.; Shim, K.-N. Current status and future perspectives of capsule endoscopy. Intest. Res. 2016, 14, 21–29. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shim, K.N.; Jeon, S.R.; Jang, H.J.; Kim, J.; Lim, Y.J.; Kim, K.O.; Song, H.J.; Lee, H.S.; Park, J.J.; Kim, J.H. Quality Indicators for Small Bowel Capsule Endoscopy. Clin. Endosc. 2017, 50, 148–160. [Google Scholar] [CrossRef] [PubMed]
- Shim, K.-N.; Moon, J.S.; Chang, N.K.; Hyuk, J.; Kim, J.H.; Min, B.H.; Jeon, S.R.; Kim, J.-O.; Choi, M.-G. Korean Gut Image Study Group Guideline for Capsule Endoscopy: Obscure Gastrointestinal Bleeding. Clin. Endosc. 2013, 46, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Pennazio, M.; Spada, C.; Eliakim, R.; Keuchel, M.; May, A.; Mulder, C.J.; Rondonotti, E.; Adler, S.N.; Albert, J.; Baltes, P.; et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2015, 47, 352–386. [Google Scholar] [CrossRef] [PubMed]
- Jeon, S.R. Use of small bowel capsule endoscopy in clinical practice: How has it performed? Korean J. Intern. Med. Jul. 2020, 35, 854–856. [Google Scholar] [CrossRef]
- Kim, S.H.; Lim, Y.J.; Park, J.S.; Shim, K.-N.; Yang, D.-H.; Chun, J.; Kim, J.S.; Lee, H.S.; Chun, H.J. Research Group for Capsule Endoscopy/Small Bowel Endoscopy Changes in performance of small bowel capsule endoscopy based on nationwide data from a Korean Capsule Endoscopy Registry. Korean J. Intern. Med. 2020, 35, 889–896. [Google Scholar] [CrossRef]
- Yamamoto, H.; Ogata, H.; Matsumoto, T.; Ohmiya, N.; Ohtsuka, K.; Watanabe, K.; Yano, T.; Matsui, T.; Higuchi, K.; Nakamura, T.; et al. Clinical Practice Guideline for Enteroscopy. Dig. Endosc. 2017, 29, 519–546. [Google Scholar] [CrossRef]
- Park, J.J.; Cheon, J.H.; Kim, H.M.; Park, H.S.; Moon, C.M.; Lee, J.H.; Hong, S.P.; Kim, T.I.; Kim, W.H. Negative capsule endoscopy without subsequent enteroscopy does not predict lower long-term rebleeding rates in patients with obscure GI bleeding. Gastrointest. Endosc. 2010, 71, 990–997. [Google Scholar] [CrossRef]
- Min, Y.; Jeon, S.W.; Jeen, Y.; Im, J.; Cheung, D.; Choi, M.-G.; Kim, J.-O.; Lee, K.; Ye, B.; Shim, K.-N.; et al. Long-term outcome of capsule endoscopy in obscure gastrointestinal bleeding: A nationwide analysis. Endoscopy 2013, 46, 59–65. [Google Scholar] [CrossRef]
- Riccioni, M.E.; Urgesi, R.; Cianci, R.; Rizzo, G.; D’Angelo, L.; Marmo, R.; Costamagna, G. Negative capsule endoscopy in patients with obscure gastrointestinal bleeding reliable: Recurrence of bleeding on long-term follow-up. World J. Gastroenterol. 2013, 19, 4520–4525. [Google Scholar] [CrossRef]
- Matsumura, T.; Arai, M.; Saito, K.; Okimoto, K.; Saito, M.; Minemura, S.; Oyamada, A.; Maruoka, D.; Nakagawa, T.; Watabe, H.; et al. Predictive factor of re-bleeding after negative capsule endoscopy for obscure gastrointestinal bleeding: Over 1-year follow-up study. Dig. Endosc. 2014, 26, 650–658. [Google Scholar] [CrossRef]
- Magalhães-Costa, P.; Bispo, M.; Santos, S.; Couto, G.; Matos, L.; Chagas, C. Re-bleeding events in patients with obscure gastrointestinal bleeding after negative capsule endoscopy. World J. Gastrointest. Endosc. 2015, 7, 403–410. [Google Scholar] [CrossRef]
- Niikura, R.; Yamada, A.; Nagata, N.; Kobayashi, Y.; Okamoto, M.; Mitsuno, Y.; Ogura, K.; Yoshida, S.; Shimbo, T.; Hirata, Y.; et al. New predictive model of rebleeding during follow-up of patents with obscure gastrointestinal bleeding: A multicenter cohort study. J. Gastroenterol. Hepatol. 2016, 31, 752–760. [Google Scholar] [CrossRef]
- Tan, W.; Ge, Z.Z.; Gao, Y.J.; Li, X.B.; Dai, J.; Fu, S.W.; Zhang, Y.; Xue, H.B.; Zhao, Y.J. Long-term outcome in patients with obscure gastrointestinal bleeding after capsule endoscopy. J. Dig. Dis. 2014, 16, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Yung, D.E.; Koulaouzidis, A.; Avni, T.; Kopylov, U.; Giannakou, A.; Rondonotti, E.; Pennazio, M.; Eliakim, R.; Toth, E.; Plevris, J.N. Clinical outcomes of negative small-bowel capsule endoscopy for small-bowel bleeding: A systematic review and meta-analysis. Gastrointest. Endosc. 2017, 85, 305–317.e2. [Google Scholar] [CrossRef] [PubMed]
- Harada, A.; Torisu, T.; Okamoto, Y.; Hirano, A.; Umeno, J.; Moriyama, T.; Washio, E.; Fuyuno, Y.; Fujioka, S.; Kitazono, T.; et al. Predictive Factors for Rebleeding after Negative Capsule Endoscopy among Patients with Overt Obscure Gastrointestinal Bleeding. Digestion 2019, 101, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Pasha, S.F.; Hara, A.K.; Leighton, J.A. Diagnostic evaluation and management of obscure gastrointestinal bleeding: A changing paradigm. Gastroenterol. Hepatol. 2009, 5, 839–850. [Google Scholar]
- Macdonald, J.; Porter, V.; McNamara, D. Negative capsule endoscopy in patients with obscure GI bleeding predicts low rebleeding rates. Gastrointest. Endosc. 2008, 68, 1122–1127. [Google Scholar] [CrossRef]
- Lapalus, M.-G.; Ben Soussan, E.; Saurin, J.-C.; Favre, O.; D’Halluin, P.N.; Coumaros, D.; Gaudric, M.; Fumex, F.; Antonietti, M.; Gaudin, J.-L.; et al. Capsule endoscopy and bowel preparation with oral sodium phosphate: A prospective randomized controlled trial. Gastrointest. Endosc. 2008, 67, 1091–1096. [Google Scholar] [CrossRef]
- Rosa, B.J.; Barbosa, M.; Magalhaes, J.; Rebelo, A.; Moreira, M.J.; Cotter, J. Oral purgative and simethicone before small bowel capsule endoscopy. World J. Gastrointest. Endosc. 2013, 5, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Saurin, J.-C.; Delvaux, M.; Gaudin, J.-L.; Fassler, I.; Villarejo, J.; Vahedi, K.; Bitoun, A.; Canard, J.-M.; Souquet, J.C.; Ponchon, T.; et al. Diagnostic Value of Endoscopic Capsule in Patients with Obscure Digestive Bleeding: Blinded Comparison with Video Push-Enteroscopy. Endoscopy 2003, 35, 576–584. [Google Scholar] [CrossRef] [PubMed]
- ASGE Standards of Practice Committee; Gurudu, S.R.; Bruining, D.H.; Acosta, R.D.; Eloubeidi, M.A.; Faulx, A.L.; Khashab, M.A.; Kothari, S.; Lightdale, J.R.; Muthusamy, V.R.; et al. The role of endoscopy in the management of suspected small-bowel bleeding. Gastrointest Endosc. 2017, 85, 22–31. [Google Scholar]
- Hilmi, I.; Kobayashi, T. Capsule endoscopy in inflammatory bowel disease: When and how. Intest. Res. 2020, 18, 265–274. [Google Scholar] [CrossRef]
- Jeon, S.R.; Jin-Oh, K.; Gun, K.H.; Hee, L.T.; Jun-Hyung, C.; Ju, P.E.; Seop, L.D.; Jung, K.W.; Min, K.B.; Young, C.J.; et al. Is there a difference between capsule endoscopy and computed tomography as a first-line study in obscure gastrointestinal bleeding? Turk. J. Gastroenterol. 2014, 25, 257–263. [Google Scholar] [CrossRef]
- Westerhof, J.; Weersma, R.K.; Koornstra, J.J. Risk factors for incomplete small-bowel capsule endoscopy. Gastrointest. Endosc. 2009, 69, 74–80. [Google Scholar] [CrossRef]
- Boal Carvalho, P.; Magalhães, J.; Dias De Castro, F.; Monteiro, S.; Rosa, B.; Moreira, M.J.; Cotter, J. Suspected blood indicator in capsule endoscopy: A valuable tool for gastrointestinal bleeding diagnosis. Arq. Gastroenterol. 2017, 54, 16–20. [Google Scholar] [CrossRef][Green Version]
- Curdia Goncalves, T.; Barbosa, M.; Rosa, B.; Moreira, M.J.; Cotter, J. Uncovering the uncertainty: Risk factors and clinical relevance of P1 lesions on small bowel capsule endoscopy of anemic patients. World J. Gastroenterol. 2016, 22, 8568–8575. [Google Scholar] [CrossRef]
- Kim, J.-B.; Ye, B.D.; Song, Y.; Yang, D.-H.; Jung, K.W.; Kim, K.-J.; Byeon, J.-S.; Myung, S.-J.; Yang, S.-K.; Kim, J.-H. Frequency of rebleeding events in obscure gastrointestinal bleeding with negative capsule endoscopy. J. Gastroenterol. Hepatol. 2013, 28, 834–840. [Google Scholar] [CrossRef]
- Park, J.; Jeon, S.R.; Kim, J.-O.; Kim, H.G.; Lee, T.H.; Cho, J.-H.; Ko, B.M.; Lee, J.S. Rebleeding rate and risk factors in nonsteroidal anti-inflammatory drug-induced enteropathy. J. Dig. Dis. 2018, 19, 279–287. [Google Scholar] [CrossRef]

| Variable | N = 84 |
|---|---|
| Age, years | 57.9 ± 19.9 |
| Old age (>65 years) | 30 (35.7) |
| Male gender | 49 (58.3) |
| Type of first bleeding | |
| Overt | 67 (79.8) |
| Occult | 17 (20.2) |
| CCI | 1.14 ± 1.68 |
| DM | 9 (10.7) |
| CVD | 35 (41.7) |
| LC | 5 (6.0) |
| ESRD | 4 (4.8) |
| CVA | 3 (3.6) |
| Medication at the first bleeding | |
| NSAIDs use | 12 (14.3) |
| Aspirin use | 10 (11.9) |
| Clopidogrel/cilostazol use | 3 (3.6)/1 (1.2) |
| DOAC use | 2 (2.4) |
| Warfarin use | 2 (2.4) |
| Lowest Hb level at the first bleeding (g/dL) | 8.6 ± 2.6 |
| pRBC transfusion, pints | 1.1 ± 1.9 |
| Follow-up duration, months | 35.9 ± 40.2 |
| Variable | N = 84 |
|---|---|
| Type of CE | |
| PillCam (SB1) | 8 (9.5) |
| PillCam (SB2) | 31 (36.9) |
| PillCam (SB3) | 34 (40.5) |
| MiroCam | 11 (13.1) |
| Acceptable quality of images, n (%) | 64 (76.2) |
| Arrival at cecum, n (%) | 72 (85.7) |
| Transit time, mean, min | 277.84 ± 208.31 |
| Results of CE | |
| P1 | 46 (54.8) |
| Red spot(s) or small isolated angioectasia | 22 (47.8) |
| Small isolated erosion | 18 (39.1) |
| Red spot(s) or small isolated angioectasia + small isolated erosion | 6 (13.0) |
| P0 | 38 (45.2) |
| Variable | P0 (N = 38) | P1 (N = 46) | p-value |
|---|---|---|---|
| Age, years | 56.8 ± 23.2 | 58.8 ± 17.1 | 0.665 |
| Old age (>65 years) | 14 (36.8) | 16 (34.8) | >0.999 |
| Male gender | 20 (52.6) | 29 (63.0) | 0.379 |
| Type of first bleeding | |||
| Overt | 29 (76.3) | 38 (82.6) | 0.588 |
| Occult | 9 (23.7) | 8 (17.4) | |
| CCI | 0.89 ± 1.33 | 1.34 ± 1.91 | 0.206 |
| DM | 6 (15.8) | 3 (6.5) | 0.288 |
| CVD | 16 (42.1) | 19 (41.3) | >0.999 |
| LC | 2 (5.3) | 3 (6.5) | >0.999 |
| ESRD | 0 | 4 (8.7) | 0.123 |
| CVA | 1 (2.6) | 2 (4.3) | >0.999 |
| Medication at the first bleeding | 9 (23.7) | 14 (30.4) | 0.624 |
| NSAIDs use | 5 (13.2) | 7 (15.2) | >0.999 |
| Aspirin use | 1 (2.6) | 9 (19.6) | 0.020 |
| Clopidogrel/cilostazol use | 0 | 4 (8.7) | 0.123 |
| DOAC use | 2 (5.3) | 0 | 0.202 |
| Warfarin use | 1 (2.6) | 1 (2.2) | >0.999 |
| Lowest Hb level at the first bleeding | 8.7 ± 3.0 | 8.5 ± 2.3 | 0.694 |
| pRBC transfusion, pints | 0.9 ± 1.5 | 1.3 ± 2.3 | 0.413 |
| Rebleeding | 7 (18.4) | 8 (17.4) | >0.999 |
| Time interval between the first episode and rebleeding | 11.4 ± 7.6 | 42.3 ± 42.0 | 0.078 |
| Follow-up duration, months | 36.2 ± 39.8 | 35.6 ± 41.1 | 0.942 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| P0 group | ||||
| Old age >65 years | 11.244 (1.349–93.699) | 0.025 | ||
| Aspirin use | 31.937 (1.995–511.293) | 0.014 | ||
| Initial Hb <8 g/dL | 6.707 (0.800–56.216) | 0.079 | ||
| Reuse of bleeding-related drugs | 6.655 (1.078–41.091) | 0.041 | ||
| P1 group | ||||
| CCI | 1.775 (1.239–2.542) | 0.002 | 2.019 (1.158–3.519) | 0.013 |
| LC | 6.058 (1.095–33.525) | 0.039 | ||
| Initial Hb <8 g/dL | 12.121 (1.483–99.082) | 0.020 | 15.085 (1.182–192.514) | 0.037 |
| pRBC transfusion (>2 pints) | 6.215 (0.992–38.937) | 0.051 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, Y.K.; Park, H.; Moon, J.R.; Jeon, S.R.; Kim, H.G.; Lee, T.H.; Park, J.; Kim, J.-O.; Lee, J.S.; Goong, H.J.; et al. Clinical Outcomes between P1 and P0 Lesions for Obscure Gastrointestinal Bleeding with Negative Computed Tomography and Capsule Endoscopy. Diagnostics 2021, 11, 657. https://doi.org/10.3390/diagnostics11040657
Cho YK, Park H, Moon JR, Jeon SR, Kim HG, Lee TH, Park J, Kim J-O, Lee JS, Goong HJ, et al. Clinical Outcomes between P1 and P0 Lesions for Obscure Gastrointestinal Bleeding with Negative Computed Tomography and Capsule Endoscopy. Diagnostics. 2021; 11(4):657. https://doi.org/10.3390/diagnostics11040657
Chicago/Turabian StyleCho, Young Kyu, Heesu Park, Jung Rock Moon, Seong Ran Jeon, Hyun Gun Kim, Tae Hee Lee, Junseok Park, Jin-Oh Kim, Joon Seong Lee, Hyeon Jeong Goong, and et al. 2021. "Clinical Outcomes between P1 and P0 Lesions for Obscure Gastrointestinal Bleeding with Negative Computed Tomography and Capsule Endoscopy" Diagnostics 11, no. 4: 657. https://doi.org/10.3390/diagnostics11040657
APA StyleCho, Y. K., Park, H., Moon, J. R., Jeon, S. R., Kim, H. G., Lee, T. H., Park, J., Kim, J.-O., Lee, J. S., Goong, H. J., Ko, B. M., & Park, S. (2021). Clinical Outcomes between P1 and P0 Lesions for Obscure Gastrointestinal Bleeding with Negative Computed Tomography and Capsule Endoscopy. Diagnostics, 11(4), 657. https://doi.org/10.3390/diagnostics11040657







