Clinical Observation of Allergic Conjunctival Diseases with Portable and Recordable Slit-Lamp Device
Abstract
:1. Introduction
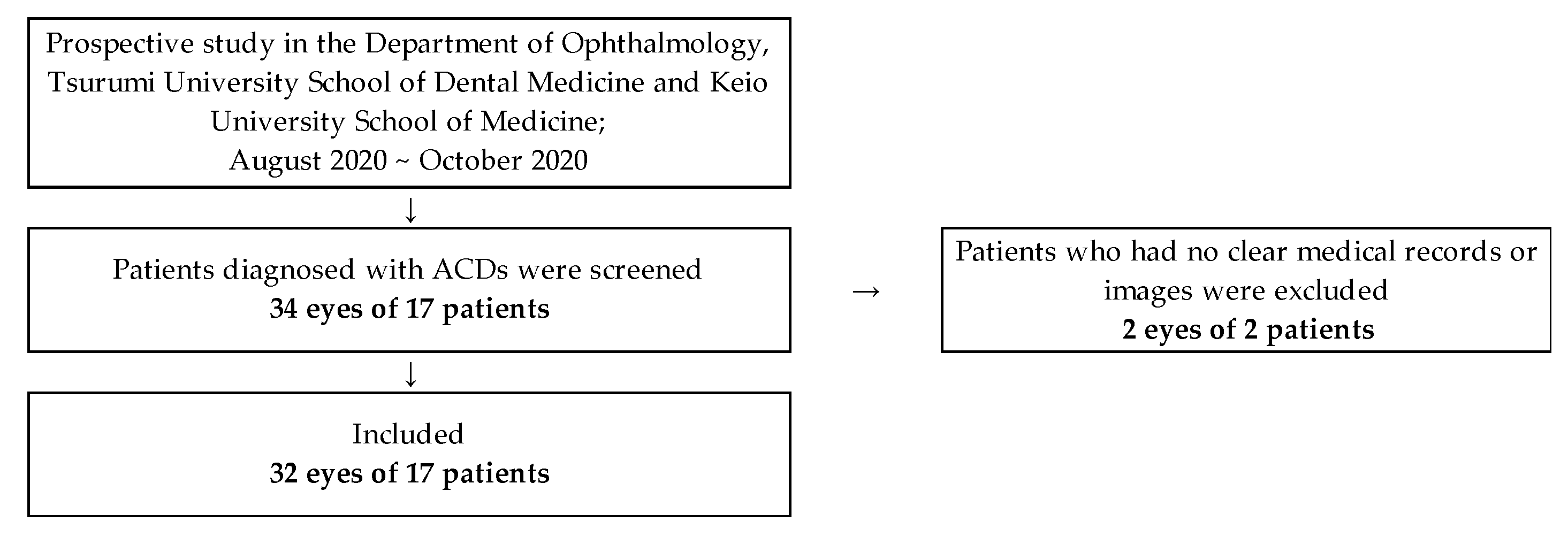
2. Materials and Methods
2.1. Ethics Approval
2.2. Study Design
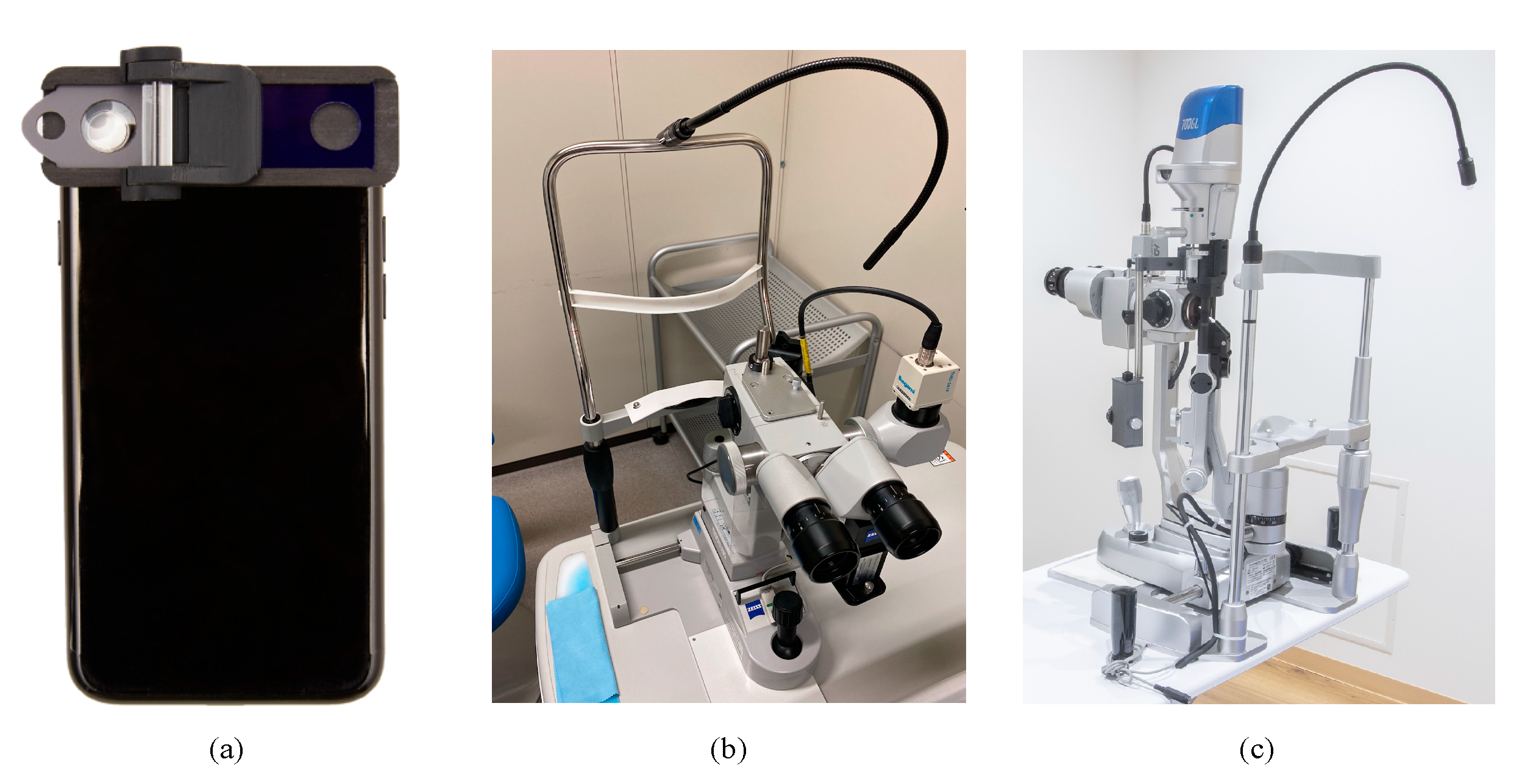
2.3. Conventional Non-Portable Slit-Lamp Microscope and SEC Examination
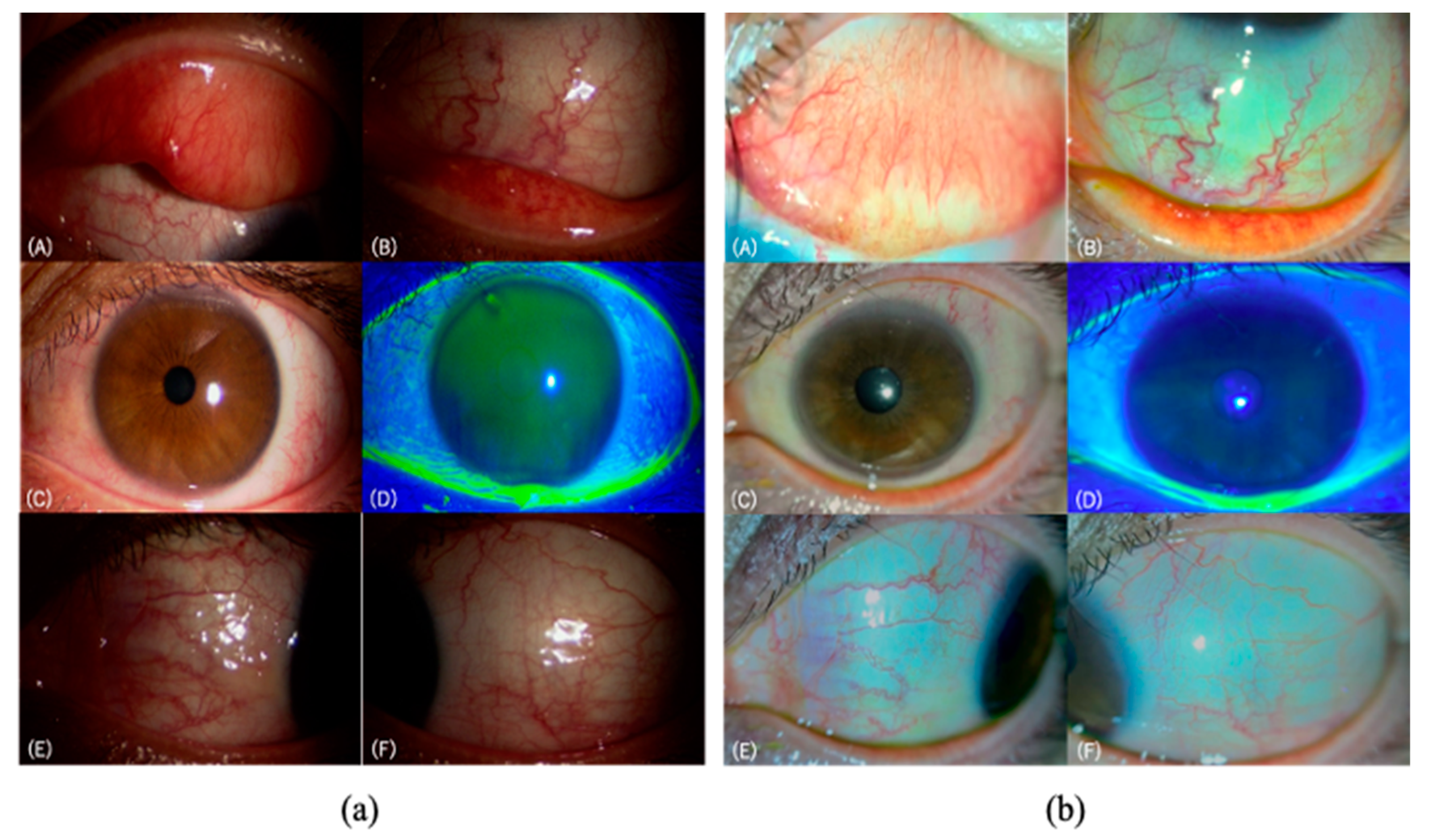
2.4. Evaluation of Allergic Conjunctival Diseases by the Conventional Slit-Lamp Microscope and the SEC
2.5. Statistical and Data Analysis
3. Results
3.1. Demographics of the Subjects
3.2. Correlation of ACD Grading Evaluation by the Two Devices
3.3. Reproducibility of the ACD Grading Evaluated by the Two Devices
4. Discussion
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Okuda, M. Epidemiology of Japanese cedar pollinosis throughout Japan. Ann. Allergy Asthma Immunol. 2003, 91, 288–296. [Google Scholar] [CrossRef]
- Okubo, K.; Kurono, Y.; Fujieda, S.; Ogino, S.; Uchio, E.; Odajima, H.; Takenaka, H.; Baba, K. Japanese Society of A: Japanese guideline for allergic rhinitis. Allergol. Int. 2011, 60, 171–189. [Google Scholar] [CrossRef] [Green Version]
- Miyazaki, D.; Takamura, E.; Uchio, E.; Ebihara, N.; Ohno, S.; Ohashi, Y.; Okamoto, S.; Satake, Y.; Shoji, J.; Namba, K.; et al. Japanese guidelines for allergic conjunctival diseases 2020. Allergol. Int. 2020, 69, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, A.; Motterle, L.; Bortolotti, M. Allergy and the eye. Clin. Exp. Immunol. 2008, 153, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Fujishima, H.; Okada, N.; Matsumoto, K.; Fukagawa, K.; Igarashi, A.; Matsuda, A.; Ono, J.; Ohta, S.; Mukai, H.; Yoshikawa, M.; et al. The usefulness of measuring tear periostin for the diagnosis and management of ocular allergic diseases. J. Allergy Clin. Immunol. 2016, 138, 459–467. [Google Scholar] [CrossRef] [Green Version]
- Ibrahim, O.M.A.; Dogru, M.; Kaido, M.; Kojima, T.; Fujishima, H.; Tsubota, K. Functional Visual Acuity Assessment of Severe Atopic Keratoconjunctivitis. Cornea 2014, 33, S13–S18. [Google Scholar] [CrossRef]
- Sy, H.; Bielory, L. Atopic keratoconjunctivitis. Allergy Asthma Proc. 2013, 34, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Fukushima, A.; Ohashi, Y.; Ebihara, N.; Uchio, E.; Okamoto, S.; Kumagai, N.; Shoji, J.; Takamura, E.; Nakagawa, Y.; Namba, K.; et al. Therapeutic effects of 0.1% tacrolimus eye drops for refractory allergic ocular diseases with proliferative lesion or corneal involvement. Br. J. Ophthalmol. 2014, 98, 1023–1027. [Google Scholar] [CrossRef]
- Yucel, O.E.; Ulus, N.D. Efficacy and safety of topical cyclosporine A 0.05% in vernal keratoconjunctivitis. Singapore Med. J. 2016, 57, 507–510. [Google Scholar] [CrossRef] [Green Version]
- Kumar, S. Vernal keratoconjunctivitis: A major review. Acta Ophthalmol. 2009, 87, 133–147. [Google Scholar] [CrossRef] [PubMed]
- Vichyanond, P.; Pacharn, P.; Pleyer, U.; Leonardi, A. Vernal keratoconjunctivitis: A severe allergic eye disease with remodeling changes. Pediatr. Allergy Immunol. 2014, 25, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Yazu, H.; Fukagawa, K.; Shimizu, E.; Sato, Y.; Fujishima, H. Long-term outcomes of 0.1% tacrolimus eye drops in eyes with severe allergic conjunctival diseases. Allergy Asthma Clin. Immunol. 2021, 17, 1–9. [Google Scholar] [CrossRef]
- Zhong, X.; Liu, H.; Pu, A.; Xia, X.; Zhou, X. M cells are involved in pathogenesis of human contact lens-associated giant papillary conjunctivitis. Arch. Immunol. Exp. 2007, 55, 173–177. [Google Scholar] [CrossRef] [Green Version]
- Donshik, P.C.; Ehlers, W.H.; Ballow, M. Giant Papillary Conjunctivitis. Immunol. Allergy Clin. N. Am. 2008, 28, 83–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zepeda Ortega, B.; Rosas Vargas, M.A.; Ito Tsuchiya, F.M.; del Rio Navarro, B.E.; Sienra Monge, J.J. Allergic conjunctivitis in children. Rev. Alerg. Mexico 2007, 54, 41–53. [Google Scholar]
- Fujishima, H.; Fukagawa, K.; Takano, Y.; Okamoto, S.; Nakagawa, Y.; Uchio, E.; Yokoi, N.; Fukushima, A.; Takamura, E. The Early Efficacy of Topical Levocabastine in Patients with Allergic Conjunctivitis. Allergol. Int. 2006, 55, 301–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Sullivan, E.P.; Malhotra, R.; Migdal, C. Prescription of eye drops. Postgrad. Med. J. 2001, 77, 654–655. [Google Scholar] [CrossRef] [PubMed]
- Al Hanaineh, A.T.; Hassanein, D.H.; Abdelbaky, S.H.; El Zawahry, O.M. Steroid-induced ocular hypertension in the pediatric age group. Eur. J. Ophthalmol. 2018, 28, 372–377. [Google Scholar] [CrossRef]
- Maier, P.; Lapp, T.; Reinhard, T. Ocular involvement in atopic dermatitis: Clinical aspects and therapy. Ophthalmologe 2017, 114, 514–524. [Google Scholar] [CrossRef] [PubMed]
- Kolbe, L.; Kligman, A.M.; Schreiner, V.; Stoudemayer, T. Corticosteroid-induced atrophy and barrier impairment measured by non-invasive methods in human skin. Ski. Res. Technol. 2001, 7, 73–77. [Google Scholar] [CrossRef]
- Shimizu, E.; Ogawa, Y.; Yazu, H.; Aketa, N.; Yang, F.; Yamane, M.; Sato, Y.; Kawakami, Y.; Tsubota, K. Smart Eye Camera: An innovative technique to evaluate tear film breakup time in a murine dry eye disease model. PLoS ONE 2019, 14, e0215130. [Google Scholar] [CrossRef]
- Yazu, H.; Shimizu, E.; Okuyama, S.; Katahira, T.; Aketa, N.; Yokoiwa, R.; Sato, Y.; Ogawa, Y.; Fujishima, H. Evaluation of Nuclear Cataract with Smartphone-Attachable Slit-Lamp Device. Diagnostics 2020, 10, 576. [Google Scholar] [CrossRef]
- Shimizu, E.; Yazu, H.; Aketa, N.; Yokoiwa, R.; Sato, S.; Yajima, J.; Katayama, T.; Sato, R.; Tanji, M.; Sato, Y.; et al. A Study Validating the Estimation of Anterior Chamber Depth and A Study Validating the Estimation of Anterior Chamber Depth and Iridocorneal Angle with Portable and Non-Portable Slit-Lamp Microscopy. Sensors 2021, 21, 1436. [Google Scholar] [CrossRef]
- Yazu, H.; Shimizu, E.; Aketa, N.; Dogru, M.; Okada, N.; Fukagawa, K.; Fujishima, H. The efficacy of 0.1% tacrolimus ophthalmic suspension in the treatment of severe atopic keratoconjunctivitis. Ann. Allergy Asthma Immunol. 2019, 122, 387–392. [Google Scholar] [CrossRef]
- Takamura, E.; Uchio, E.; Ebihara, N.; Ohno, S.; Ohashi, Y.; Okamoto, S.; Kumagai, N.; Satake, Y.; Shoji, J.; Nakagawa, Y.; et al. Japanese guidelines for allergic conjunctival diseases 2017. Allergol. Int. 2017, 66, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Gloor, B.R. Hans Goldmann (1899–1991). Eur. J. Ophthalmol. 2010, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.Z.; Tan, C.W. Smartphone Imaging in Ophthalmology: A Comparison with Traditional Methods on the Reproducibility and Usability for Anterior Segment Imaging. Ann. Acad. Med. Singap. 2016, 45, 6–11. [Google Scholar] [PubMed]
- Dubbs, S.B.; Blosser, K.M.; Richardson, A.C. A smartphone, a slit lamp, and an ophthalmology consult. Clin. Case Rep. 2019, 7, 2004–2005. [Google Scholar] [CrossRef] [Green Version]
- Mohammadpour, M.; Mohammadpour, L.; Hassanzad, M. Smartphone Assisted Slit Lamp Free Anterior Segment Imaging: A novel technique in teleophthalmology. Contact Lens Anterior Eye 2016, 39, 80–81. [Google Scholar] [CrossRef]
- Miyazaki, D.; Fukagawa, K.; Fukushima, A.; Fujishima, H.; Uchio, E.; Ebihara, N.; Shoji, J.; Takamura, E.; Namba, K.; Ohashi, Y.; et al. Air pollution significantly associated with severe ocular allergic inflammatory diseases. Sci. Rep. 2019, 9, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mimura, T.; Ichinose, T.; Yamagami, S.; Fujishima, H.; Kamei, Y.; Goto, M.; Takada, S.; Matsubara, M. Airborne particulate matter (PM2.5) and the prevalence of allergic conjunctivitis in Japan. Sci. Total Environ. 2014, 487, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, E.; Yazu, H.; Aketa, N.; Yokoiwa, R.; Sato, S.; Katayama, T.; Hanyuda, A.; Sato, Y.; Ogawa, Y.; Tsubota, K. Smart Eye Camera: A validation study for evaluating the tear film breakup time in human subjects. Transl. Vis. Sci. Technol. 2021, in press. [Google Scholar]
| Cases | 17 | |
|---|---|---|
| Male/Female | 12/5 | |
| Age (y) | 21.5 ± 14.8 | |
| Eyes | 34 | |
| Perennial Allergic Conjunctivitis (PAC) | 4 | |
| Seasonal Allergic Conjunctivitis (SAC) | 18 | |
| Giant Papillary Conjunctivitis (GPC) | 2 | |
| Atopic Keratoconjunctivitis (AKC) | 5 | |
| Vernal Keratoconjunctivitis (VKC) | 3 | |
| Unclear or Lack of Images | 2 | |
| Average Scores (point) | ||
| RE (Conventional/SEC) | 3.3 ± 2.4/3.2 ± 2.1 | 0.33 * |
| LE (Conventional/SEC) | 3.4 ± 2.4/4.3 ± 3.1 | 0.34 * |
| BE (Conventional/SEC) | 6.6 ± 4.8/7.5 ± 3.6 | 0.43 * |
| Eye | Palpebral Conjunctiva | Bulbar Conjunctiva | Limbus | Cornea | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sign | Hyperemia | Swelling | Follicle | Papillae | Giant Papillae | Hyperemia | Chemosis | Swelling | Trantas | Epithelial Disorder | ||
| RE | n | 17 | ||||||||||
| κ | 0.78 | 0.88 | 0.87 | 0.88 | - | 1.00 | 1.00 | - | - | 0.63 | 0.73 | |
| 95% CI | 0.70–0.85 | 0.83–0.94 | 0.80–0.93 | 0.83–0.94 | - | - | - | - | - | 0.46–0.81 | 0.67–0.78 | |
| LE | n | 17 | ||||||||||
| κ | 0.78 | 0.50 | 0.87 | 0.87 | - | 0.81 | 1.00 | - | - | 0.73 | 0.45 | |
| 95% CI | 0.71–0.85 | 0.41–0.59 | 0.81–0.93 | 0.72–0.86 | - | 0.75–0.87 | - | - | - | 0.65–0.82 | 0.39–0.51 | |
| BE | n | 34 | ||||||||||
| κ | 0.78 | 0.87 | 0.75 | 0.83 | - | 0.89 | 1.00 | - | - | 0.72 | 0.63 | |
| 95% CI | 0.75–0.82 | 0.83–0.91 | 0.71–0.79 | 0.80–0.87 | - | 0.86–0.91 | - | - | - | 0.66–0.77 | 0.60–0.66 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yazu, H.; Shimizu, E.; Sato, S.; Aketa, N.; Katayama, T.; Yokoiwa, R.; Sato, Y.; Fukagawa, K.; Ogawa, Y.; Tsubota, K.; et al. Clinical Observation of Allergic Conjunctival Diseases with Portable and Recordable Slit-Lamp Device. Diagnostics 2021, 11, 535. https://doi.org/10.3390/diagnostics11030535
Yazu H, Shimizu E, Sato S, Aketa N, Katayama T, Yokoiwa R, Sato Y, Fukagawa K, Ogawa Y, Tsubota K, et al. Clinical Observation of Allergic Conjunctival Diseases with Portable and Recordable Slit-Lamp Device. Diagnostics. 2021; 11(3):535. https://doi.org/10.3390/diagnostics11030535
Chicago/Turabian StyleYazu, Hiroyuki, Eisuke Shimizu, Shinri Sato, Naohiko Aketa, Taiichiro Katayama, Ryota Yokoiwa, Yasunori Sato, Kazumi Fukagawa, Yoko Ogawa, Kazuo Tsubota, and et al. 2021. "Clinical Observation of Allergic Conjunctival Diseases with Portable and Recordable Slit-Lamp Device" Diagnostics 11, no. 3: 535. https://doi.org/10.3390/diagnostics11030535








