Tear Osmolarity in the Diagnosis of Systemic Dehydration and Dry Eye Disease
Abstract
1. Introduction
2. Terminology
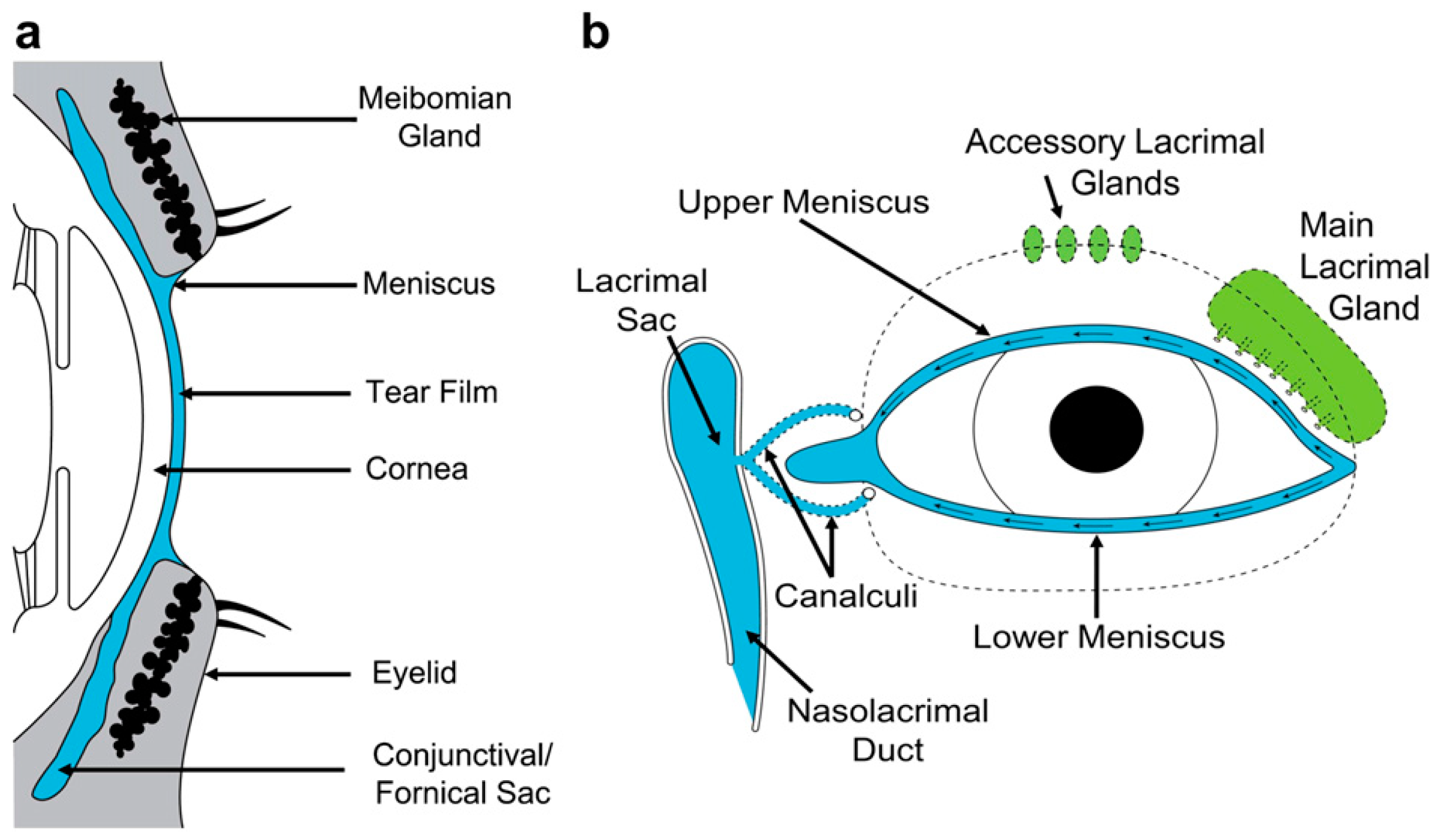
3. The Tears
3.1. Introduction
3.2. The Lacrimal Secretion
3.3. Tear Mixing and Distribution
3.4. Tear Osmolarity
3.5. Tear Osmolarity in Normal Eyes, in Open Eye Conditions
3.6. Tear Osmolarity in Dry Eye Disease
3.7. The Impact of Environment and Behaviour on Tear Osmolarity
3.8. The Effect of Tear Flow-Rate on Tear Osmolarity
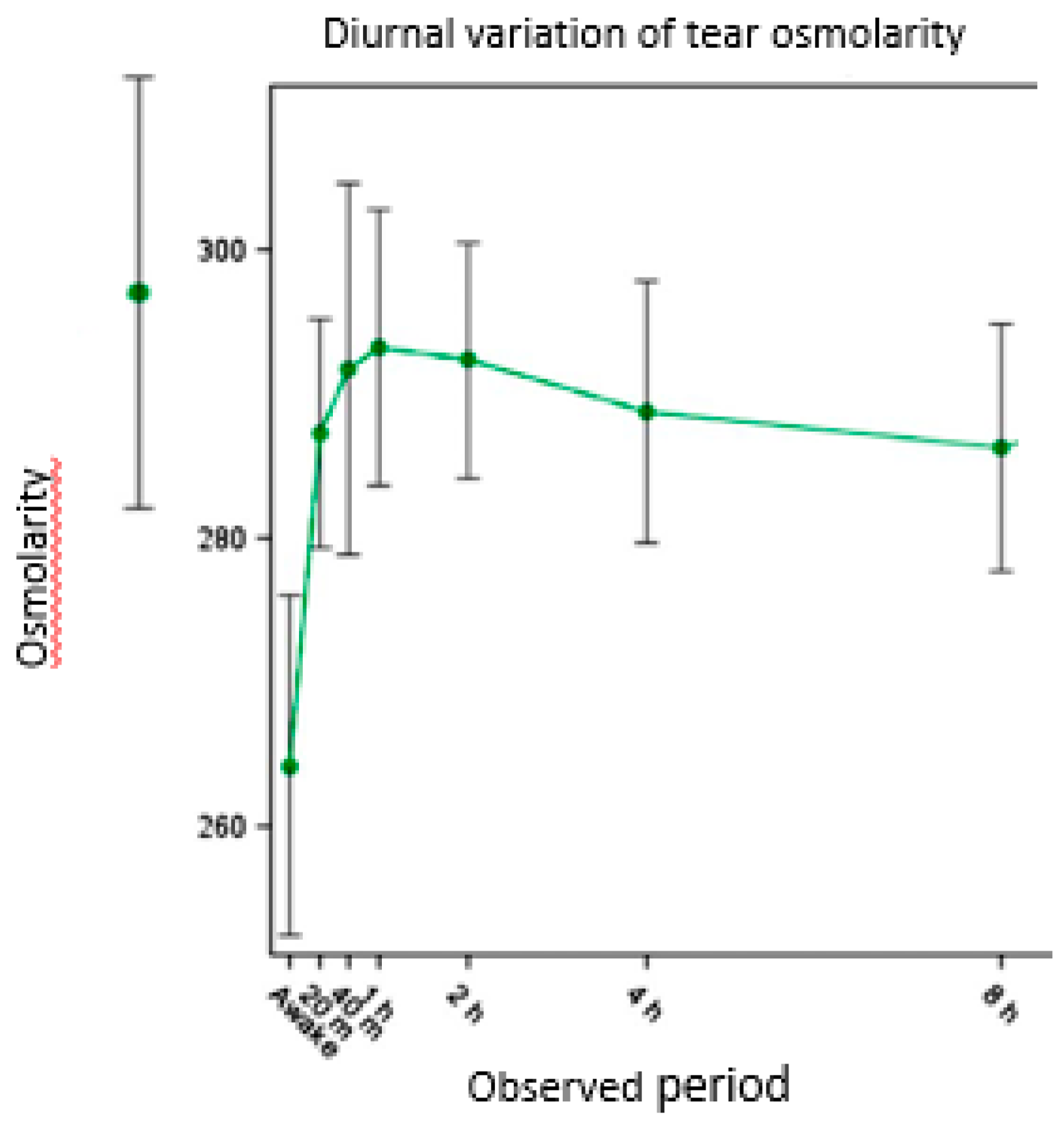
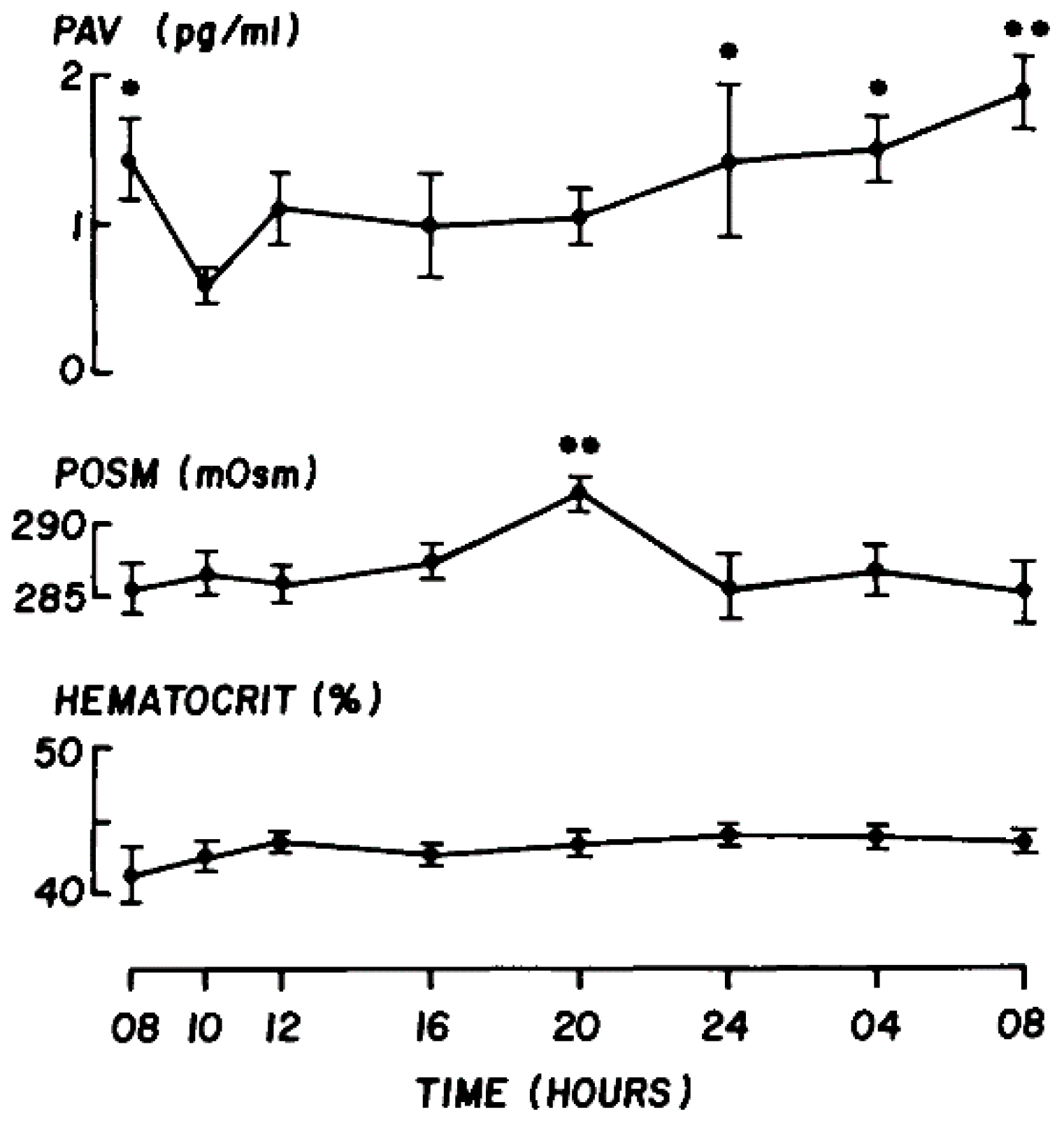
3.9. The diurnal Variation of Tear Osmolarity
4. Body Hydration and Dehydration
4.1. Introduction
4.2. Diagnosis of Systemic Dehydration
4.3. Body Hydration and Tear Osmolarity
5. The Concept of Basal Tear Osmolarity
5.1. Introduction
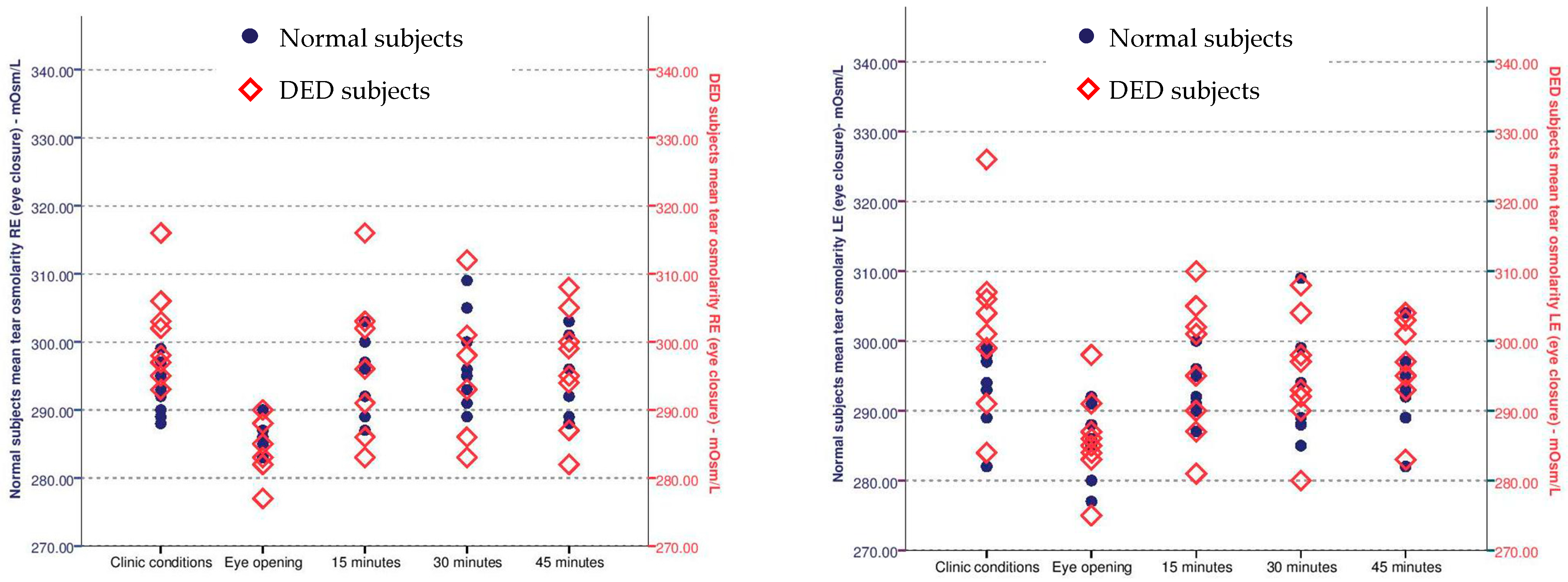
5.2. Measurement of Tear Osmolarity after Eye Closure
5.3. Estimating the Necessary Period of Eye Closure to Achieve the BTO
5.4. Measurement of Tear Osmolarity at High Ambient Humidity, in Open-Eye Conditions
5.5. Measuring Basal Tear Osmolarity after eye Closure or Exposure to High Ambient Humidity
6. Inter-Eye Differences in Tear Osmolarity
7. Eye Closure Studies
8. High Humidity Studies
9. Discussion
9.1. Introduction
9.2. Exposure to High Ambient Humidity
9.3. Eye Closure Studies
9.4. Predicted Utility of the BTO in Estimating Systemic Hydration
9.5. Tear Osmolarity at the Ocular Surface during Sleep
9.6. Systemic Dehydration Dry Eye (SDDE)—A New Class of Dry Eye Disease
9.7. A further Implication of the BTO—Apossible Correction Factor for Tear Biomarkers
10. Using Basal Tear Osmolarity as a Screening Test for Systemic Dehydration
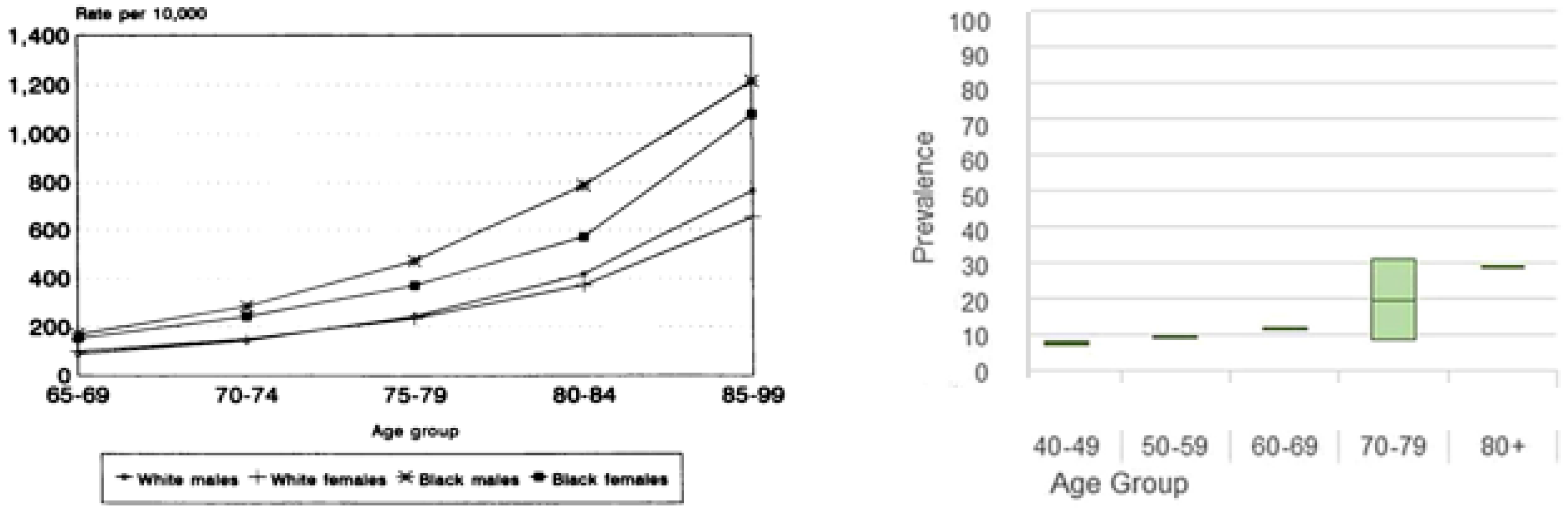
10.1. In the Elderly
- A first requirement is to validate the concept of the BTO by showing that eye closure for 45 min does indeed achieve a basal tOsm level, close in osmolarity to an individual’s own pOsm and that this finding is highly repeatable in the individual. This requires contemporary measurements of pOsm and tOsm after 45 min of eye closure in participants with healthy eyes and a normal lacrimal function and in patients with DED (ADDE and EDE) showing a broad range of tear hyperosmolarities.
- High humidity CEC studies, at an RH 80–90%, are needed in patients showing a broad range of tear hyperosmolarity, mapping the time taken to bring down the tOsm to BTO level. These data could be used to design a shortened eye closure test acceptable for routine use in elderly patients. This would need to be trialed in eye closure studies.
- The shortened BTO test could then be trialed in a residential care-home setting, comparing BTO values with pOsm values on multiple occasions, to establish its credentials as a screening test for body-water deprivation. It would be important to measure pOsm directly, from blood samples and to estimate it from selected formulae.
10.2. In Other Groups
11. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nose, H.; Mack, G.W.; Shi, X.R.; Nadel, E.R. Role of Osmolality and Plasma Volume during Rehydration in Humans. J. Appl. Physiol. 1988, 65, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Cheuvront, S.N.; Ely, B.R.; Kenefick, R.W.; Sawka, M.N. Biological Variation and Diagnostic Accuracy of Dehydration Assessment Markers. Am. J. Clin. Nutr. 2010, 92, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Hooper, L.; Bunn, D.K.; Downing, A.; Jimoh, F.O.; Groves, J.; Free, C.; Cowap, V.; Potter, J.F.; Hunter, P.R.; Shepstone, L. Which Frail Older People Are Dehydrated? The UK DRIE Study. J. Gerontol. Ser. Biomed. Sci. Med. Sci. 2016, 71, 1341–1347. [Google Scholar] [CrossRef] [PubMed]
- Lacey, J.; Corbett, J.; Forni, L.; Hooper, L.; Hughes, F.; Minto, G.; Moss, C.; Price, S.; Whyte, G.; Woodcock, T. A Multidisciplinary Consensus on Dehydration: Definitions, Diagnostic Methods and Clinical Implications. Ann. Med. 2019, 51, 232–251. [Google Scholar] [CrossRef]
- Warren, J.L.; Bacon, W.E.; Harris, T.; McBean, A.M.; Foley, D.; Phillips, C. The Burden and Outcomes Associated with Dehydration among US Elderly, 1991. Am. J. Public Health 1994, 84, 1265–1269. [Google Scholar] [CrossRef]
- Siervo, M.; Bunn, D.; Prado, C.M.; Hooper, L. Accuracy of Prediction Equations for Serum Osmolarity in Frail Older People with and without Diabetes. Am. J. Clin. Nutr. 2014, 100, 867–876. [Google Scholar] [CrossRef] [PubMed]
- Reid, J. Speech by Rt Hon John Reid MP, Secretary of State for Health, 11 March 2004: Managing New Realities: Integrating the Care Landscape. Webarchive Natl. Gov UK 2004. Available online: www.dh.gov.uk/en/MediaCentre/Speeches/Speecheslist/DH_4076406 (accessed on 1 December 2020).
- El-Sharkawy, A.M.; Sahota, O.; Maughan, R.J.; Lobo, D.N. The Pathophysiology of Fluid and Electrolyte Balance in the Older Adult Surgical Patient. Clin. Nutr. 2014, 33, 6–13. [Google Scholar] [CrossRef]
- Stookey, J.D. High Prevalence of Plasma Hypertonicity among Community-Dwelling Older Adults: Results from NHANES III. J. Am. Diet. Assoc. 2005, 105, 1231–1239. [Google Scholar] [CrossRef]
- Matz, R. Dehydration in Older Adults. JAMA 1996, 275, 911–912. [Google Scholar] [CrossRef]
- Willshire, C. Tear Dynamics: Tear Osmolarity and Reflex Features of the Lacrimal Functional Unit. Doctoral Dissertation, Anglia Ruskin University, Cambridge, UK, 2017. [Google Scholar]
- Willshire, C.; Bron, A.J.; Gaffney, E.A.; Pearce, E.I. Basal Tear Osmolarity as a Metric to Estimate Body Hydration and Dry Eye Severity. Prog. Retin. Eye Res. 2018, 64, 56–64. [Google Scholar] [CrossRef]
- Willshire, C.; Buckley, R.J.; Bron, A.J. Estimating Basal Tear Osmolarity in Normal and Dry Eye Subjects. Contact Lens Anterior Eye 2018, 41, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, B.D.; Whitmer, D.; Nichols, K.K.; Tomlinson, A.; Foulks, G.N.; Geerling, G.; Pepose, J.S.; Kosheleff, V.; Porreco, A.; Lemp, M.A. An Objective Approach to Dry Eye Disease Severity. Investig. Ophthalmol. Vis. Sci. 2010, 51, 6125–6130. [Google Scholar] [CrossRef] [PubMed]
- Farris, R.L.; Stuchell, R.N.; Mandel, I.D. Tear Osmolarity Variation in the Dry Eye. Trans. Am. Ophthalmol. Soc. 1986, 84, 250–268. [Google Scholar]
- Hooper, L.; Abdelhamid, A.; Ali, A.; Bunn, D.K.; Jennings, A.; John, W.G.; Kerry, S.; Lindner, G.; Pfortmueller, C.A.; Sjöstrand, F. Diagnostic Accuracy of Calculated Serum Osmolarity to Predict Dehydration in Older People: Adding Value to Pathology Laboratory Reports. BMJ Open 2015, 5, e008846. [Google Scholar] [CrossRef] [PubMed]
- Halperin, M.L.; Goldstein, M.B.; Stark, J. Fluid, Electrolyte and Acid-Base Physiology: A Problem-Based Approach. Crit. Care Nurs. Q. 1994, 17, 88–89. [Google Scholar] [CrossRef]
- Gaffney, E.A.; Tiffany, J.M.; Yokoi, N.; Bron, A.J. Warren. Prog. Retin. Eye Res. 2010, 29, 59–78. [Google Scholar] [CrossRef]
- Tomlinson, A.; Khanal, S. Assessment of Tear Film Dynamics: Quantification Approach. Ocul. Surf. 2005, 3, 81–95. [Google Scholar] [CrossRef]
- MacDonald, E.A.; Maurice, D.M. The Kinetics of Tear Fluid under the Lower Lid. Exp. Eye Res. 1991, 53, 421–425. [Google Scholar] [CrossRef]
- Yokoi, N.; Bron, A.J.; Georgiev, G.A. The Precorneal Tear Film as a Fluid Shell: The Effect of Blinking and Saccades on Tear Film Distribution and Dynamics. Ocul. Surf. 2014, 12, 252–266. [Google Scholar] [CrossRef]
- Mircheff, A.K. Lacrimal Fluid and Electrolyte Secretion: A Review. Curr. Eye Res. 1989, 8, 607–617. [Google Scholar] [CrossRef]
- Turpie, B.; Yoshimura, T.; Gulati, A.; Rios, J.D.; Dartt, D.A.; Masli, S. Sjögren’s Syndrome-like Ocular Surface Disease in Thrombospondin-1 Deficient Mice. Am. J. Pathol. 2009, 175, 1136–1147. [Google Scholar] [CrossRef] [PubMed]
- Dartt, D.A. Dysfunctional Neural Regulation of Lacrimal Gland Secretion and Its Role in the Pathogenesis of Dry Eye Syndromes. Ocul. Surf. 2004, 2, 76–91. [Google Scholar] [CrossRef]
- Dartt, D.A. Neural Regulation of Lacrimal Gland Secretory Processes: Relevance in Dry Eye Diseases. Prog. Retin. Eye Res. 2009, 28, 155–177. [Google Scholar] [CrossRef]
- Hodges, R.R.; Dartt, D.A. Signaling Pathways of Purinergic Receptors and Their Interactions with Cholinergic and Adrenergic Pathways in the Lacrimal Gland. J. Ocul.pharmacol. Ther. 2016, 32, 490–497. [Google Scholar] [CrossRef]
- Stevenson, W.; Pugazhendhi, S.; Wang, M. Is the Main Lacrimal Gland Indispensable? Contributions of the Corneal and Conjunctival Epithelia. Surv. Ophthalmol. 2016, 61, 616–627. [Google Scholar] [CrossRef]
- Taiara, C.; Smith, B. Palpebral Dacryoadenectomy. Am. J. Ophthalmol. 1973, 75, 461–465. [Google Scholar] [CrossRef]
- Scherz, W.; Dohlman, C.H. Is the Lacrimal Gland Dispensable? Keratoconjunctivitis Sicca after Lacrimal Gland Removal. Arch. Ophthalmol. 1975, 93, 281. [Google Scholar] [CrossRef] [PubMed]
- Hornblass, A.; Guberina, C.; Herschorn, B.J. Palpebral Dacryoadenectomy for Epiphora. Ophthal.plast. Reconstr. Surg. 1988, 4, 227–230. [Google Scholar] [CrossRef] [PubMed]
- Rose, G.E.; Wright, J.E. Pleomorphic Adenoma of the Lacrimal Gland. Br. J. Ophthalmol. 1992, 76, 395–400. [Google Scholar] [CrossRef]
- Shiue, M.H.; Kulkarni, A.A.; Gukasyan, H.J.; Swisher, J.B.; Kim, K.-J.; Lee, V.H. Pharmacological Modulation of Fluid Secretion in the Pigmented Rabbit Conjunctiva. Life Sci. 2000, 66, PL105–PL111. [Google Scholar] [CrossRef]
- Dartt, D.A. Regulation of Mucin and Fluid Secretion by Conjunctival Epithelial Cells. Prog. Retin. Eye Res. 2002, 21, 555–576. [Google Scholar] [CrossRef]
- Li, Y.; Kuang, K.; Yerxa, B.; Wen, Q.; Rosskothen, H.; Fischbarg, J. Rabbit Conjunctival Epithelium Transports Fluid, and P2Y22 Receptor Agonists Stimulate Cl− and Fluid Secretion. Am. J. Physiol.-Cellphysiol. 2001, 281, C595–C602. [Google Scholar] [CrossRef]
- Klyce, S.D.; Crosson, C.E. Transport Processes across the Rabbit Corneal Epithelium: A Review. Curr. Eye Res. 1985, 4, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Cerretani, C.F.; Radke, C.J. Tear Dynamics in Healthy and Dry Eyes. Curr. Eye Res. 2014, 39, 580–595. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.; Baum, J. Basic Tear Flow. Does It Exist? Ophthalmology 1980, 87, 920–930. [Google Scholar] [CrossRef]
- Murube, J. Basal, Reflex, and Psycho-Emotional Tears. Ocul. Surf. 2009, 7, 60–66. [Google Scholar] [CrossRef]
- Nelson, J.D.; Wright, J.C. Tear Film Osmolality Determination: An Evaluation of Potential Errors in Measurement. Curr. Eye Res. 1986, 5, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.T. The Lacrimal Secretory System and Its Treatment. Am. J. Ophthalmol. 1966, 62, 47–60. [Google Scholar] [CrossRef]
- Seifert, P.; Spitznas, M. Vasoactive Intestinal Polypeptide (VIP) Innervation of the Human Eyelid Glands. Exp. Eye Res. 1999, 68, 685–692. [Google Scholar] [CrossRef]
- Cross, D.A.; Krupin, T. Implications of the Effects of General Anesthesia on Basal Tear Production. Anesth. Analg. 1977, 56, 35–37. [Google Scholar] [CrossRef]
- Gilbard, J.P.; Cohen, G.R.; Baum, J. Decreased Tear Osmolarity and Absence of the Inferior Marginal Tear Strip after Sleep. Cornea 1992, 11, 231–233. [Google Scholar] [CrossRef]
- Allansmith, M.R.; Kajiyama, G.; Abelson, M.B.; Simon, M.A. Plasma Cell Content of Main and Accessory Lacrimal Glands and Conjunctiva. Am. J. Ophthalmol. 1976, 82, 819–826. [Google Scholar] [CrossRef]
- Dartt, D.A.; Moller, M.; Poulsen, J.H. Lacrimal Gland Electrolyte and Water Secretion in the Rabbit: Localization and Role of (Na+ + K+)-Activated ATPase. J. Physiol. 1981, 321, 557–569. [Google Scholar] [CrossRef] [PubMed]
- Ubels, J.L.; Williams, K.K.; Bernal, D.L.; Edelhauser, H.F. Evaluation of Effects of a Physiologic Artificial Tear on the Corneal Epithelial Barrier: Electrical Resistance and Carboxyfluorescein Permeability. In Lacrimal Gland, Tear Film, and Dry Eye Syndromes; Springer: Berlin/Heidelberg, Germany, 1994; pp. 441–452. [Google Scholar]
- Katona, M.; Vizvári, E.; Németh, L.; Facskó, A.; Venglovecz, V.; Rakonczay, Z.; Hegyi, P.; Tóth-Molnár, E. Experimental Evidence of Fluid Secretion of Rabbit Lacrimal Gland Duct Epithelium. Investig. Ophthalmol. Vis. Sci. 2014, 55, 4360–4367. [Google Scholar] [CrossRef][Green Version]
- Calonge, M.; Pinto-Fraga, J.; González-García, M.J.; Enríquez-de-Salamanca, A.; López-de la Rosa, A.; Fernández, I.; López-Miguel, A. Effects of the External Environment on Dry Eye Disease. Int. Ophthalmol. Clin. 2017, 57, 23–40. [Google Scholar] [CrossRef] [PubMed]
- Anon. Workplace Health Committee; OHS Information Sheet No. 5; The Working Environment Part1-Thermal Comfort (Revised); Centre for Workplace Health and Improvement: Belfast, Ireland, 1998. [Google Scholar]
- Terry, J.E.; Hill, R.M. Human Tear Osmotic Pressure: Diurnal Variations and the Closed Eye. Arch. Ophthalmol. 1978, 96, 120–122. [Google Scholar] [CrossRef] [PubMed]
- Gilbard, J.P.; Farris, R.L.; Santamaria, J. Osmolarity of Tear Microvolumes in Keratoconjunctivitis Sicca. Arch. Ophthalmol. 1978, 96, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, W.J.; Hill, R.M. Human Tears: Osmotic Characteristics. Investig. Ophthalmol. Vis. Sci. 1983, 24, 1624–1626. [Google Scholar]
- White, K.M.; Benjamin, W.J.; Hill, R.M. Human Basic Tear Fluid Osmolality. Acta Ophthalmol. 1993, 71, 530–538. [Google Scholar] [CrossRef] [PubMed]
- Pensyl, C.D.; Benjamin, W.J. Vapor Pressure Osmometry: Minimum Sample Microvolumes. Acta Ophthalmol. Scand. 1999, 77, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Gilbard, J.P. Tear Film Osmolarity and Keratoconjunctivitis Sicca. Eye Contact Lens 1985, 11, 243–250. [Google Scholar]
- Gilbard, J.P.; Farris, R.L. Tear Osmolarity and Ocular Surface Disease in Keratoconjunctivitis Sicca. Arch. Ophthalmol. 1979, 97, 1642–1646. [Google Scholar] [CrossRef]
- Farris, R.L. Tear Osmolarity—A New Gold Standard? In Lacrimal Gland, Tear Film, and Dry Eye Syndromes; Springer: Berlin/Heidelberg, Germany, 1994; pp. 495–503. [Google Scholar]
- Versura, P.; Profazio, V.; Campos, E.C. Performance of Tear Osmolarity Compared to Previous Diagnostic Tests for Dry Eye Diseases. Curr. Eye Res. 2010, 35, 553–564. [Google Scholar] [CrossRef]
- Tomlinson, A.; McCann, L.C.; Pearce, E.I. Comparison of Human Tear Film Osmolarity Measured by Electrical Impedance and Freezing Point Depression Techniques. Cornea 2010, 29, 1036–1041. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, M.; Massingale, M.L.; Ye, F.; Godbold, J.; Elfassy, T.; Vallabhajosyula, M.; Asbell, P.A. Tear Osmolarity as a Biomarker for Dry Eye Disease Severity. Investig. Ophthalmol. Vis. Sci. 2010, 51, 4557–4561. [Google Scholar] [CrossRef] [PubMed]
- Versura, P.; Campos, E.C. TearLab® Osmolarity System for Diagnosing Dry Eye. Expert Rev. Mol. Diagn. 2013, 13, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Rocha, G.; Gulliver, E.; Borovik, A.; Chan, C.C. Randomized, Masked, in Vitro Comparison of Three Commercially Available Tear Film Osmometers. Clin. Ophthalmol. Auckl. NZ 2017, 11, 243. [Google Scholar] [CrossRef] [PubMed]
- Khajuria, A.; Krahn, J. Osmolality Revisited—Deriving and Validating the Best Formula for Calculated Osmolality. Clin. Biochem. 2005, 38, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Sen, D.K.; Sarin, G.S. Tear Glucose Levels in Normal People and in Diabetic Patients. Br. J. Ophthalmol. 1980, 64, 693–695. [Google Scholar] [CrossRef]
- Aragona, P.; Giuffrida, S.; Di Stefano, G.; Ferreri, F.; Di Benedetto, A.; Bucolo, C.; Cro, M. Ocular surface changes in type 1 diabetic patients. In Lacrimal Gland, Tear Film, and Dry Eye Syndromes 3; Springer: Berlin/Heidelberg, Germany, 2002; pp. 667–672. [Google Scholar]
- Tomlinson, A.; Khanal, S.; Ramaesh, K.; Diaper, C.; McFadyen, A. Tear Film Osmolarity: Determination of a Referent for Dry Eye Diagnosis. Investig. Ophthalmol. Vis. Sci. 2006, 47, 4309–4315. [Google Scholar] [CrossRef]
- Eldridge, D.; Sullivan, B.; Berg, M.; Lemp, M.; Durrie, D. Longitudinal Variability of Tear Film Osmolarity in Normal and Dry Eye Patients. Investig. Ophtalmol. Vis. Sci. 2010, 51, 3379. [Google Scholar]
- Li, M.; Du, C.; Zhu, D.; Shen, M.; Cui, L.; Wang, J. Daytime Variations of Tear Osmolarity and Tear Meniscus Volume. Eye Contact Lens 2012, 38, 282–287. [Google Scholar] [CrossRef]
- Niimi, J.; Tan, B.; Chang, J.; Zhou, Y.; Ghanekar, A.; Wong, M.; Lee, A.; Lin, M.C. Diurnal Pattern of Tear Osmolarity and Its Relationship to Corneal Thickness and Deswelling. Cornea 2013, 32, 1305–1310. [Google Scholar] [CrossRef]
- Jacobi, C.; Jacobi, A.; Kruse, F.E.; Cursiefen, C. Tear Film Osmolarity Measurements in Dry Eye Disease Using Electrical Impedance Technology. Cornea 2011, 30, 1289–1292. [Google Scholar] [CrossRef]
- Keech, A.; Senchyna, M.; Jones, L. Impact of Time between Collection and Collection Method on Human Tear Fluid Osmolarity. Curr. Eye Res. 2013, 38, 428–436. [Google Scholar] [CrossRef]
- Nolfi, J.; Caffery, B. Randomized Comparison of in Vivo Performance of Two Point-of-Care Tear Film Osmometers. Clin. Ophthalmol. Auckl. NZ 2017, 11, 945. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Peng, C.-C.; Cerretani, C.; Braun, R.J.; Radke, C. Evaporation-Driven Instability of the Precorneal Tear Film. Adv. Colloid Interface Sci. 2014, 206, 250–264. [Google Scholar] [CrossRef] [PubMed]
- Georgiev, G.A.; Yokoi, N.; Ivanova, S.; Tonchev, V.; Nencheva, Y.; Krastev, R. Surface Relaxations as a Tool to Distinguish the Dynamic Interfacial Properties of Films Formed by Normal and Diseased Meibomian Lipids. Soft Matter 2014, 10, 5579–5588. [Google Scholar] [CrossRef] [PubMed]
- Chao, W.; Belmonte, C.; del Castillo, J.M.B.; Bron, A.J.; Dua, H.S.; Nichols, K.K.; Novack, G.D.; Schrader, S.; Willcox, M.D.; Wolffsohn, J.S. Report of the Inaugural Meeting of the TFOS i 2= Initiating Innovation Series: Targeting the Unmet Need for Dry Eye Treatment. Ocul. Surf. 2016, 14, 264–316. [Google Scholar] [CrossRef]
- Bron, A.J.; Yokoi, N.; Gaffney, E.; Tiffany, J.M. Predicted Phenotypes of Dry Eye: Proposed Consequences of Its Natural History. Ocul. Surf. 2009, 7, 78–92. [Google Scholar] [CrossRef]
- Baudouin, C. The Vicious Circle in Dry Eye Syndrome: A Mechanistic Approach. J. FRANCAIS Ophtalmol. 2007, 30, 239–246. [Google Scholar] [CrossRef]
- Baudouin, C.; Irkeç, M.; Messmer, E.M.; Benítez-del-Castillo, J.M.; Bonini, S.; Figueiredo, F.C.; Geerling, G.; Labetoulle, M.; Lemp, M.; Rolando, M. Clinical Impact of Inflammation in Dry Eye Disease: Proceedings of the ODISSEY Group Meeting. Acta Ophthalmol. (Copenh.) 2018, 96, 111–119. [Google Scholar] [CrossRef]
- Bron, A.J.; de Paiva, C.S.; Chauhan, S.K.; Bonini, S.; Gabison, E.E.; Jain, S.; Knop, E.; Markoulli, M.; Ogawa, Y.; Perez, V. Tfos Dews II Pathophysiology Report. Ocul. Surf. 2017, 15, 438–510. [Google Scholar]
- Craig, J.P.; Nelson, J.D.; Azar, D.T.; Belmonte, C.; Bron, A.J.; Chauhan, S.K.; de Paiva, C.S.; Gomes, J.A.; Hammitt, K.M.; Jones, L. TFOS DEWS II Report Executive Summary. Ocul. Surf. 2017, 15, 802–812. [Google Scholar] [CrossRef]
- Higuchi, A.; Kawakita, T.; Tsubota, K. IL-6 Induction in Desiccated Corneal Epithelium in Vitro and in Vivo. Mol. Vis. 2011, 17, 2400. [Google Scholar]
- Li, D.-Q.; Chen, Z.; Song, X.J.; Luo, L.; Pflugfelder, S.C. Stimulation of Matrix Metalloproteinases by Hyperosmolarity via a JNK Pathway in Human Corneal Epithelial Cells. Investig. Ophthalmol. Vis. Sci. 2004, 45, 4302–4311. [Google Scholar] [CrossRef] [PubMed]
- Kam, W.; Sullivan, D.A.; Sullivan, B.D.; Venkiteshwar, M. Does Hyperosmolarity Induce an Irreversible Process Leading to Human Corneal Epithelial Cell Death? Investig. Ophthalmol. Vis. Sci. 2016, 57, 6181. [Google Scholar]
- Lemp, M.A.; Bron, A.J.; Baudouin, C.; del Castillo, J.M.B.; Geffen, D.; Tauber, J.; Foulks, G.N.; Pepose, J.S.; Sullivan, B.D. Tear Osmolarity in the Diagnosis and Management of Dry Eye Disease. Am. J. Ophthalmol. 2011, 151, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Arita, R.; Chalmers, R.; Djalilian, A.; Dogru, M.; Dumbleton, K.; Gupta, P.K.; Karpecki, P.; Lazreg, S.; Pult, H. TFOS DEWS II Diagnostic Methodology Report. Ocul. Surf. 2017, 15, 539–574. [Google Scholar] [CrossRef] [PubMed]
- Korb, D.R. Survey of Preferred Tests for Diagnosis of the Tear Film and Dry Eye. Cornea 2000, 19, 483–486. [Google Scholar] [CrossRef]
- Madden, L.C.; Tomlinson, A.; Simmons, P.A. Effect of Humidity Variations in a Controlled Environment Chamber on Tear Evaporation After Dry Eye Therapy. Eye Contact Lens 2013, 39, 169–174. [Google Scholar] [CrossRef]
- Lee, S.-C.; Poon, C.-S.; Li, X.-D.; Luk, F. Indoor Air Quality Investigation on Commercial Aircraft. Indoor Air 1999, 9, 180–187. [Google Scholar] [CrossRef]
- Abusharha, A.A.; Pearce, E.I. The Effect of Low Humidity on the Human Tear Film. Cornea 2013, 32, 429–434. [Google Scholar] [CrossRef]
- Tsubota, K.; Nakamori, K. Effects of Ocular Surface Area and Blink Rate on Tear Dynamics. Arch. Ophthalmol. 1995, 113, 155–158. [Google Scholar] [CrossRef]
- Tsubota, K. Tear Dynamics and Dry Eye. Prog. Retin. Eye Res. 1998, 17, 565–596. [Google Scholar] [CrossRef]
- Mishima, S.; Maurice, D. The Effect of Normal Evaporation on the Eye. Exp. Eye Res. 1961, 1, 46–52. [Google Scholar] [CrossRef]
- Mishima, S. Some Physiological Aspects of the Precorneal Tear Film. Arch. Ophthalmol. 1965, 73, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Krogh, A.; Lund, C.; Pedersen-Bjergaard, K. The Osmotic Concentration of Human Lacrymal Fluid. Actaphysiol. 1945, 10, 88–90. [Google Scholar] [CrossRef]
- Hind, H.W.; Goyan, F.M. The Hydrogen Ion Concentration and Osmotic Properties of Lacrimal Fluid. J. Am.pharm. Assoc. Sci. Ed 1949, 38, 477–479. [Google Scholar] [CrossRef]
- Thaysen, J.H.; Thorn, N.A. Excretion of Urea, Sodium, Potassium and Chloride in Human Tears. Am. J. Physiol. 1954, 178, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, H.; Hosokawa, K. Studies on the Mechanism of Salt and Water Secretion from the Lacrimal Gland. Jpn. J. Physiol. 1963, 13, 303–318. [Google Scholar] [CrossRef] [PubMed]
- Rismondo, V.; Osgood, T.B.; Leering, P.; Hattenhauer, M.G.; Ubels, J.L.; Edelhauser, H.F. Electrolyte Composition of Lacrimal Gland Fluid and Tears of Normal and Vitamin A-Deficient Rabbits. Eye Contact Lens 1989, 15, 222–229. [Google Scholar]
- Ubels, J.L.; Harkema, J.R. The Rabbit Lacrimal Gland in Vitamin A Deficiency. Investig. Ophthalmol. Vis. Sci. 1994, 35, 1249–1253. [Google Scholar]
- Ubels, J.L.; Hoffman, H.M.; Srikanth, S.; Resau, J.H.; Webb, C.P. Gene Expression in Rat Lacrimal Gland Duct Cells Collected Using Laser Capture Microdissection: Evidence for K+ Secretion by Duct Cells. Investig. Ophthalmol. Vis. Sci. 2006, 47, 1876–1885. [Google Scholar] [CrossRef]
- Botelho, S.Y.; Martinez, E.V. Electrolytes in Lacrimal Gland Fluid and in Tears at Various Flow Rates in the Rabbit. Am. J. Physiol.-Leg. Content 1973, 225, 606–609. [Google Scholar] [CrossRef][Green Version]
- Gilbard, J.P.; Dartt, D.A. Changes in Rabbit Lacrimal Gland Fluid Osmolarity with Flow Rate. Investig. Ophthalmol. Vis. Sci. 1982, 23, 804–806. [Google Scholar]
- Danziger, J.; Zeidel, M.L. Osmotic Homeostasis. Clin. J. Am. Soc. Nephrol. 2015, 10, 852–862. [Google Scholar] [CrossRef]
- Rikkert, M.O.; Hoefnagels, W.H.L.; Deurenberg, P. Age-Related Changes in Body Fluid Compartments and the Assessment of Dehydration in Old Age. Hydration Aging 1998, 13–32, urn:nbn:nl:ui:32-43434. [Google Scholar]
- Bossingham, M.J.; Carnell, N.S.; Campbell, W.W. Water Balance, Hydration Status, and Fat-Free Mass Hydration in Younger and Older Adults. Am. J. Clin. Nutr. 2005, 81, 1342–1350. [Google Scholar] [CrossRef]
- Cheuvront, S.N.; Kenefick, R.W. Dehydration: Physiology, Assessment, and Performance Effects. Compr.physiol. 2011, 4, 257–285. [Google Scholar]
- Baron, S.; Courbebaisse, M.; Lepicard, E.M.; Friedlander, G. Assessment of Hydration Status in a Large Population. Br. J. Nutr. 2015, 113, 147–158. [Google Scholar] [CrossRef]
- Ciura, S.; Bourque, C.W. Transient Receptor Potential Vanilloid 1 Is Required for Intrinsic Osmoreception in Organum Vasculosum Lamina Terminalis Neurons and for Normal Thirst Responses to Systemic Hyperosmolality. J. Neurosci. 2006, 26, 9069–9075. [Google Scholar] [CrossRef]
- Leng, G.; Mason, W.T.; Dyer, R.G. The Supraoptic Nucleus as an Osmoreceptor. Neuroendocrinology 1982, 34, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Liedtke, W.; Choe, Y.; Martí-Renom, M.A.; Bell, A.M.; Denis, C.S.; Hudspeth, A.J.; Friedman, J.M.; Heller, S. Vanilloid Receptor–Related Osmotically Activated Channel (VR-OAC), a Candidate Vertebrate Osmoreceptor. Cell 2000, 103, 525–535. [Google Scholar] [CrossRef]
- Bourque, C.W. Central Mechanisms of Osmosensation and Systemic Osmoregulation. Nat. Rev. Neurosci. 2008, 9, 519–531. [Google Scholar] [CrossRef]
- Cheuvront, S.N.; Kenefick, R.W.; Charkoudian, N.; Sawka, M.N. Physiologic Basis for Understanding Quantitative Dehydration Assessment. Am. J. Clin. Nutr. 2013, 97, 455–462. [Google Scholar] [CrossRef]
- Egan, G.; Silk, T.; Zamarripa, F.; Williams, J.; Federico, P.; Cunnington, R.; Carabott, L.; Blair-West, J.; Shade, R.; McKinley, M. Neural Correlates of the Emergence of Consciousness of Thirst. Proc. Natl. Acad. Sci. USA 2003, 100, 15241–15246. [Google Scholar] [CrossRef]
- Denton, D.; Shade, R.; Zamarippa, F.; Egan, G.; Blair-West, J.; McKinley, M.; Fox, P. Correlation of Regional Cerebral Blood Flow and Change of Plasma Sodium Concentration during Genesis and Satiation of Thirst. Proc. Natl. Acad. Sci. USA 1999, 96, 2532–2537. [Google Scholar] [CrossRef]
- Thomas, D.R.; Cote, T.R.; Lawhorne, L.; Levenson, S.A.; Rubenstein, L.Z.; Smith, D.A.; Stefanacci, R.G.; Tangalos, E.G.; Morley, J.E.; Council, D. Understanding Clinical Dehydration and Its Treatment. J. Am. Med. Dir. Assoc. 2008, 9, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Zerbe, R.L.; Miller, J.Z.; Robertson, G.L. The Reproducibility and Heritability of Individual Differences in Osmoregulatory Function in Normal Human Subjects. J. Lab. Clin. Med. 1991, 117, 51. [Google Scholar]
- Armstrong, L.E. Assessing Hydration Status: The Elusive Gold Standard. J. Am. Coll. Nutr. 2007, 26, 575S–584S. [Google Scholar] [CrossRef] [PubMed]
- Maughan, R.J. Hydration, Morbidity, and Mortality in Vulnerable Populations. Nutr. Rev. 2012, 70, S152–S155. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Barber, J.; Campbell, E.S. Economic Burden of Dehydration among Hospitalized Elderly Patients. Am. J. Health Syst.pharm. 2004, 61, 2534–2540. [Google Scholar] [CrossRef] [PubMed]
- Manz, F.; Wentz, A. The Importance of Good Hydration for the Prevention of Chronic Diseases. Nutr. Rev. 2005, 63, S2–S5. [Google Scholar] [CrossRef]
- Oei, E.; Paudel, K.; Visser, A.; Finney, H.; Fan, S.L. Is Overhydration in Peritoneal Dialysis Patients Associated with Cardiac Mortality That Might Be Reversible? World J. Nephrol. 2016, 5, 448. [Google Scholar] [CrossRef]
- Rikkert, M.G.O.; Deurenberg, P.; Jansen, R.W.; van’t Hof, M.A.; Hoefnagels, W.H. Validation of Multi-frequency Bioelectrical Impedance Analysis in Detecting Changes in Fluid Balance of Geriatric Patients. J. Am. Geriatr. Soc. 1997, 45, 1345–1351. [Google Scholar] [CrossRef]
- Martin, A.D.; Daniel, M.Z.; Drinkwater, D.T.; Clarys, J.P. Adipose Tissue Density, Estimated Adipose Lipid Fraction and Whole Body Adiposity in Male Cadavers. Int. J. Obes. Relat. Metab. Disord. 1994, 18, 79–83. [Google Scholar] [CrossRef]
- Morgan, A.L.; Sinning, W.E.; Weldy, D.L. Age Effects on Body Fluid Distribution during Exercise in the Heat. Aviat. Space Environ. Med. 2002, 73, 750–757. [Google Scholar] [PubMed]
- Gaspar, P.M. Water Intake of Nursing Home Residents. J. Gerontol. Nurs. 1999, 25, 23–29. [Google Scholar] [CrossRef]
- Rolls, B.J.; Phillips, P.A. Aging and Disturbances of Thirst and Fluid Balance. Nutr. Rev. 1990, 48, 137–144. [Google Scholar] [CrossRef]
- De Castro, J.M. de Age-Related Changes in Natural Spontaneous Fluid Ingestion and Thirst in Humans. J. Gerontol. 1992, 47, P321–P330. [Google Scholar] [CrossRef] [PubMed]
- Lindeman, R.D.; Tobin, J.; Shock, N.W. Longitudinal Studies on the Rate of Decline in Renal Function with Age. J. Am. Geriatr. Soc. 1985, 33, 278–285. [Google Scholar] [CrossRef]
- Zizza, C.A.; Ellison, K.J.; Wernette, C.M. Total Water Intakes of Community-Living Middle-Old and Oldest-Old Adults. J. Gerontol. Ser. Biomed. Sci. Med. Sci. 2009, 64, 481–486. [Google Scholar] [CrossRef]
- He, S.; Craig, B.A.; Xu, H.; Covinsky, K.E.; Stallard, E.; Thomas, J., III; Hass, Z.; Sands, L.P. Unmet Need for ADL Assistance Is Associated with Mortality among Older Adults with Mild Disability. J. Gerontol. Ser. Biomed. Sci. Med. Sci. 2015, 70, 1128–1132. [Google Scholar] [CrossRef]
- Davies, I.; O’Neill, P.A.; MClean, K.A.; Cantania, J.; Bennett, D. Age-Associated Alterations in Thirst and Arginine Vasopressin in Response to a Water or Sodium Load. Age Ageing 1995, 24, 151–159. [Google Scholar] [CrossRef]
- Morley, J. Water, Water Everywhere and Not a Drop to Drink. J. Gerontol. A. Biol. Sci. Med. Sci. 2000, 55, M359–M360. [Google Scholar] [CrossRef] [PubMed]
- Sands, J.M. Urine Concentrating and Diluting Ability during Aging. J. Gerontol. Ser. Biomed. Sci. Med. Sci. 2012, 67, 1352–1357. [Google Scholar] [CrossRef]
- Mentes, J. Oral Hydration in Older Adults: Greater Awareness Is Needed in Preventing, Recognizing, and Treating Dehydration. AJN Am. J. Nurs. 2006, 106, 40–49. [Google Scholar] [CrossRef]
- Wolff, A.; Stuckler, D.; McKee, M. Are Patients Admitted to Hospitals from Care Homes Dehydrated? A Retrospective Analysis of Hypernatraemia and in-Hospital Mortality. J. R. Soc. Med. 2015, 108, 259–265. [Google Scholar] [CrossRef]
- Hydration for Health Initiative, April 2012. Hydration in the Aging: A Review of Current Knowledge. Available online: www.h4hinitiative.com/tools (accessed on 1 October 2017).
- Leibovitz, A.; Baumoehl, Y.; Lubart, E.; Yaina, A.; Platinovitz, N.; Segal, R. Dehydration among Long-Term Care Elderly Patients with Oropharyngeal Dysphagia. Gerontology 2007, 53, 179–183. [Google Scholar] [CrossRef]
- Hooper, L.; Abdelhamid, A.; Attreed, N.J.; Campbell, W.W.; Channell, A.M.; Chassagne, P.; Culp, K.R.; Fletcher, S.J.; Fortes, M.B.; Fuller, N. Clinical Symptoms, Signs and Tests for Identification of Impending and Current Water-loss Dehydration in Older People. Cochrane Libr. 2015. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US). DRI, Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate; National Academy Press: New York, NY, USA, 2005; ISBN 0-309-09170-5. [Google Scholar]
- Botelho, S.Y.; Martinez, E.V.; Pholpramool, C.; Prooyen, H.; van Janssen, J.T.; De Palau, A. Modification of Stimulated Lacrimal Gland Flow by Sympathetic Nerve Impulses in Rabbit. Am. J. Physiol. Leg. Content 1976, 230, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Fortes, M.B.; Diment, B.C.; Di Felice, U.; Gunn, A.E.; Kendall, J.L.; Esmaeelpour, M.; Walsh, N.P. Tear Fluid Osmolarity as a Potential Marker of Hydration Status. Med. Sci. Sports Exerc. 2011, 43, 1590–1597. [Google Scholar] [CrossRef] [PubMed]
- Walsh, N.P.; Fortes, M.B.; Esmaeelpour, M. Influence of Modest Changes in Whole-Body Hydration on Tear Fluid Osmolarity: Important Considerations for Dry Eye Disease Detection. Cornea 2011, 30, 1517. [Google Scholar] [CrossRef]
- Walsh, N.P.; Fortes, M.B.; Raymond-Barker, P.; Bishop, C.; Owen, J.; Tye, E.; Esmaeelpour, M.; Purslow, C.; Elghenzai, S. Is Whole-Body Hydration an Important Consideration in Dry Eye? Investig. Ophthalmol. Vis. Sci. 2012, 53, 6622–6627. [Google Scholar] [CrossRef]
- Uchino, M.; Dogru, M.; Yagi, Y.; Goto, E.; Tomita, M.; Kon, T.; Saiki, M.; Matsumoto, Y.; Uchino, Y.; Yokoi, N. The Features of Dry Eye Disease in a Japanese Elderly Population. Optom. Vis. Sci. 2006, 83, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Moss, S.E.; Klein, R.; Klein, B.E. Long-Term Incidence of Dry Eye in an Older Population. Optom. Vis. Sci. 2008, 85, 668–674. [Google Scholar] [CrossRef]
- Guo, B.; Lu, P.; Chen, X.; Zhang, W.; Chen, R. Prevalence of Dry Eye Disease in Mongolians at High Altitude in China: The Henan Eye Study. Ophthalmic Epidemiol. 2010, 17, 234–241. [Google Scholar] [CrossRef]
- Lemp, M.A. Advances in Understanding and Managing Dry Eye Disease. Am. J. Ophthalmol. 2008, 146, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Yokoi, N.; Komuro, A.; Nishida, K.; Kinoshita, S. Effectiveness of Hyaluronan on Corneal Epithelial Barrier Function in Dry Eye. Br. J. Ophthalmol. 1997, 81, 533–536. [Google Scholar] [CrossRef]
- Zhu, H.; Chauhan, A. A Mathematical Model for Tear Drainage through the Canaliculi. Curr. Eye Res. 2005, 30, 621–630. [Google Scholar] [CrossRef]
- Stern, M.E.; Gao, J.; Schwalb, T.A.; Ngo, M.; Tieu, D.D.; Chan, C.-C.; Reis, B.L.; Whitcup, S.M.; Thompson, D.; Smith, J.A. Conjunctival T-Cell Subpopulations in Sjogren’s and Non-Sjogren’s Patients with Dry Eye. Investig. Ophthalmol. Vis. Sci. 2002, 43, 2609–2614. [Google Scholar]
- Tomlinson, A.; Madden, L.; Pearce, I. Influence of Modest Changes in Whole-Body Hydration on Tear Fluid Osmolarity: Important Considerations for Dry Eye Disease Detection Reply. Cornea 2011, 30, 1517–1518. [Google Scholar] [CrossRef]
- Stapleton, F.; Alves, M.; Bunya, V.Y.; Jalbert, I.; Lekhanont, K.; Malet, F.; Na, K.-S.; Schaumberg, D.; Uchino, M.; Vehof, J. Tfos Dews Ii Epidemiology Report. Ocul. Surf. 2017, 15, 334–365. [Google Scholar] [CrossRef] [PubMed]
- Bron, A.J.; Evans, V.E.; Smith, J.A. Grading of Corneal and Conjunctival Staining in the Context of Other Dry Eye Tests. Cornea 2003, 22, 640–650. [Google Scholar] [CrossRef]
- Schiffman, R.M.; Christianson, M.D.; Jacobsen, G.; Hirsch, J.D.; Reis, B.L. Reliability and Validity of the Ocular Surface Disease Index. Arch. Ophthalmol. 2000, 118, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Charlton, J.F.; Schwab, I.R.; Stuchell, R. Tear Hyperosmolarity in Renal Dialysis Patients Asymptomatic for Dry Eye. Cornea 1996, 15, 335–339. [Google Scholar] [CrossRef]
- Baudouin, C.; Messmer, E.M.; Aragona, P.; Geerling, G.; Akova, Y.A.; Benítez-del-Castillo, J.; Boboridis, K.G.; Merayo-Lloves, J.; Rolando, M.; Labetoulle, M. Revisiting the Vicious Circle of Dry Eye Disease: A Focus on the Pathophysiology of Meibomian Gland Dysfunction. Br. J. Ophthalmol. 2016, 100, 300–306. [Google Scholar] [CrossRef]
- Gilbard, J.P.; Carter, J.B.; Sang, D.N.; Refojo, M.F.; Hanninen, L.A.; Kenyon, K.R. Morphologic Effect of Hyperosmolarity on Rabbit Corneal Epithelium. Ophthalmology 1984, 91, 1205–1212. [Google Scholar] [CrossRef]
- Kang, J.; Fulop, G.; Friedman, A.H. Tear Urea Nitrogen and Creatinine Levels in Renal Patients. Acta Ophthalmol. 1988, 66, 407–412. [Google Scholar] [CrossRef]
- Van Haeringen, N.J.; Glasius, E. Collection Method Dependant Concentrations of Some Metabolites in Human Tear Fluid, with Special Reference to Glucose in Hyperglycaemic Conditions. Albrecht Von Graefes Arch. Für Klin. Exp. Ophthalmol. 1977, 202, 1–7. [Google Scholar] [CrossRef]
- Balík, J. The Lacrimal Fluid in Keratoconjunctivitis Sicca*: A Quantitative and Qualitative Investigation. Am. J. Ophthalmol. 1952, 35, 773–782. [Google Scholar] [CrossRef]
- Bhave, G.; Neilson, E.G. Body Fluid Dynamics: Back to the Future. J. Am. Soc. Nephrol. 2011, 22, 2166–2181. [Google Scholar] [CrossRef]
- Sack, R.A.; Beaton, A.; Sathe, S.; Morris, C.; Willcox, M.; Bogart, B. Towards a Closed Eye Model of the Pre-Ocular Tear Layer. Prog. Retin. Eye Res. 2000, 19, 649–668. [Google Scholar] [CrossRef]
- Farris, R.L.; Stuchell, R.N.; Mandel, I.D. Basal and Reflex Human Tear Analysis: I. Physical Measurements: Osmolarity, Basal Volumes, and Reflex Flow Rate. Ophthalmology 1981, 88, 852–857. [Google Scholar] [CrossRef]
- Ogasawara, K.; Tsuru, T.; Mitsubayashi, K.; Karube, I. Electrical Conductivity of Tear Fluid in Healthy Persons and Keratoconjunctivitis Sicca Patients Measured by a Flexible Conductimetric Sensor. Graefes Arch. Clin. Exp. Ophthalmol. 1996, 234, 542–546. [Google Scholar] [CrossRef]
- Iester, M.; Orsoni, G.J.; Gamba, G.; Taffara, M.; Mangiafico, P.; Giuffrida, S.; Rolando, M. Improvement of the Ocular Surface Using Hypotonic 0.4% Hyaluronic Acid Drops in Keratoconjunctivitis Sicca. Eye 2000, 14, 892–898. [Google Scholar] [CrossRef]
- George, C.P.; Messerli, F.H.; Genest, J.; Nowaczynski, W.; Boucher, R.; Kuchel, O.; Rojo-Ortega, M. Diurnal Variation of Plasma Vasopressin in Man. J. Clin. Endocrinol. Metab. 1975, 41, 332–338. [Google Scholar] [CrossRef]
- Armstrong, L.E. Hydration Assessment Techniques. Nutr. Rev. 2005, 63, S40–S54. [Google Scholar] [CrossRef]
- Sollanek, K.J.; Kenefick, R.W.; Walsh, N.P.; Fortes, M.B.; Esmaeelpour, M.; Cheuvront, S.N. Assessment of Thermal Dehydration Using the Human Eye: What Is the Potential? J. Therm. Biol. 2012, 37, 111–117. [Google Scholar] [CrossRef]
- Holland, J.J.; Ray, M.; Irwin, C.; Skinner, T.L.; Leveritt, M.; Desbrow, B. Tear Osmolarity Is Sensitive to Exercise-Induced Fluid Loss but Is Not Associated with Common Hydration Measures in a Field Setting. J. Sports Sci. 2018, 36, 1220–1227. [Google Scholar] [CrossRef]
- Ungaro, C.T.; Reimel, A.J.; Nuccio, R.P.; Barnes, K.A.; Pahnke, M.D.; Baker, L.B. Non-Invasive Estimation of Hydration Status Changes through Tear Fluid Osmolarity during Exercise and Post-Exercise Rehydration. Eur. J. Appl. Physiol. 2015, 115, 1165–1175. [Google Scholar] [CrossRef]
- Bryce, J.; Boschi-Pinto, C.; Shibuya, K.; Black, R.E.; WHO Child Health Epidemiology Reference Group. WHO Estimates of the Causes of Death in Children. Lancet 2005, 365, 1147–1152. [Google Scholar] [CrossRef]
| Author | Method | n | Tear Osmolarity |
|---|---|---|---|
| Tomlinson et al., 2006 [66] | Meta-analysis: DFP and VP measurements. 1978–2005 | 815 | 302.0 ± 9.7 mOsm/L |
| Eldridge et al., 2010 [67] | TearLab® | 30 | 301.8 ± 10.5 mOsms/L |
| Li et al., 2012 [68] | TearLab® | 10 | 298.0 ± 14.2 mOsms/L |
| Niimi et al., 2013 [69] | TearLab® | 38 | 297 ± 15 mOsms/L |
| Jacobi et al., 2011 [70] | TearLab® | 133 | 301 mOsmol/L (range 298–304 mOsmol/L) |
| Sullivan et al., 2010 [14] | Tear Lab® | 75 | 302.2 ± 8.3 |
| Keech et al., 2013 [71] | Tear Lab® | 10 15 | 304.0 ± 8.4 mOsm/L 301.2 ± 7.2 mOsm/L |
| Nolfi et al., 2017 [72] | Tear Lab® | 20 | 295.4 ± 8.6 mOsm/L |
| Tear Osmolarity tOsm | Basal Tear Osmolarity BTO | Plasma Osmolarity pOsm | Clinical Status |
|---|---|---|---|
| T1 | T1 | P1 | No DED; normal hydration |
| Up | T1 | P1 | ADDE or EDE; normal hydration |
| T1 | Up | Up | Preclinical dehydration; tOsm not yet in the DED range |
| Up | Up | Up | Current clinical dehydration; SDDE Local dry eye tests may indicate there is coincident ADDE and EDE. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bron, A.J.; Willshire, C. Tear Osmolarity in the Diagnosis of Systemic Dehydration and Dry Eye Disease. Diagnostics 2021, 11, 387. https://doi.org/10.3390/diagnostics11030387
Bron AJ, Willshire C. Tear Osmolarity in the Diagnosis of Systemic Dehydration and Dry Eye Disease. Diagnostics. 2021; 11(3):387. https://doi.org/10.3390/diagnostics11030387
Chicago/Turabian StyleBron, Anthony J., and Catherine Willshire. 2021. "Tear Osmolarity in the Diagnosis of Systemic Dehydration and Dry Eye Disease" Diagnostics 11, no. 3: 387. https://doi.org/10.3390/diagnostics11030387
APA StyleBron, A. J., & Willshire, C. (2021). Tear Osmolarity in the Diagnosis of Systemic Dehydration and Dry Eye Disease. Diagnostics, 11(3), 387. https://doi.org/10.3390/diagnostics11030387






