Selective Surface Electrostimulation of the Denervated Zygomaticus Muscle
Abstract
1. Introduction
2. Methods
2.1. Study Characteristics
2.2. Study Timeline
2.3. Study Aims
2.4. Population
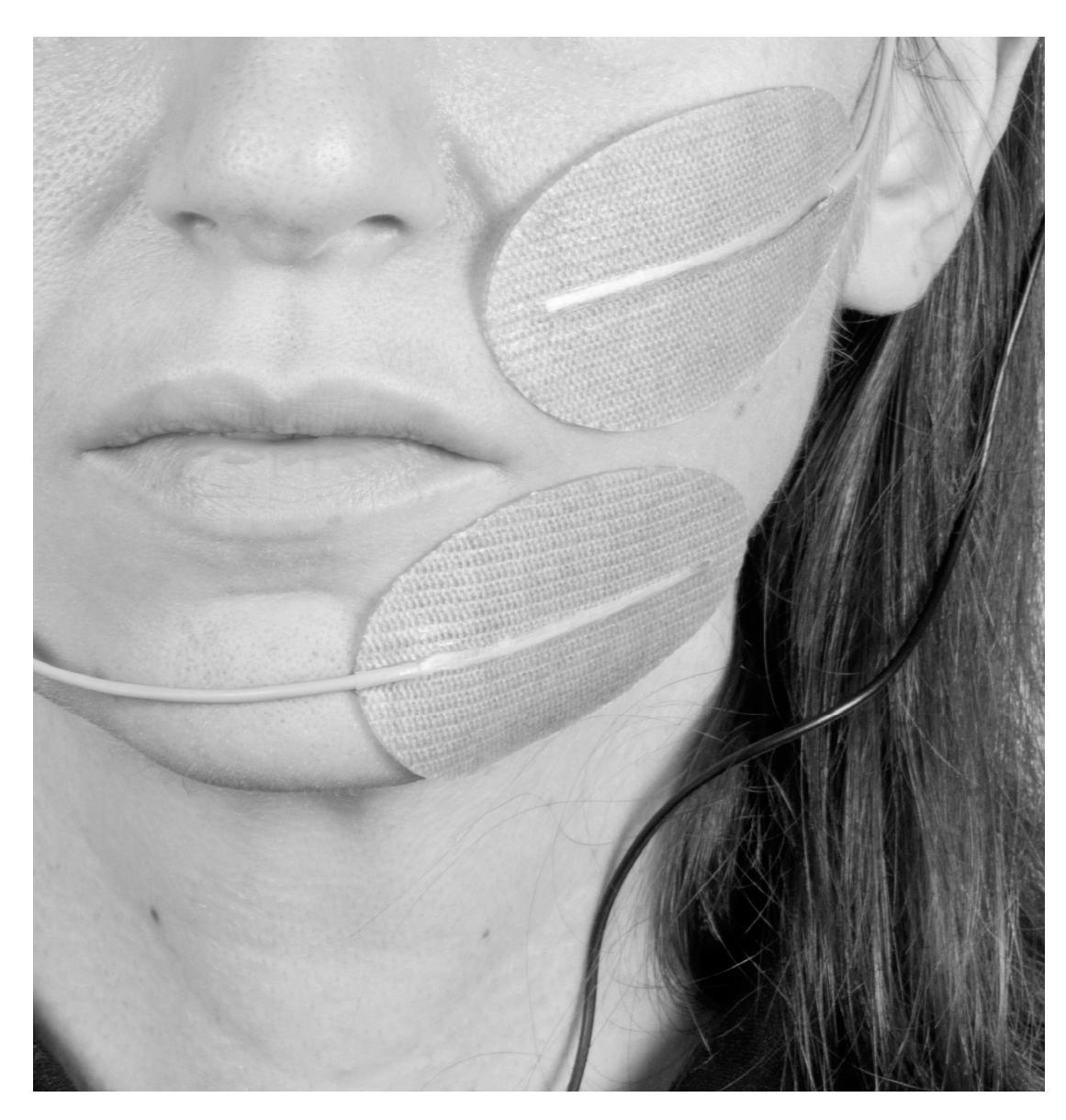
2.5. Electrode Placement
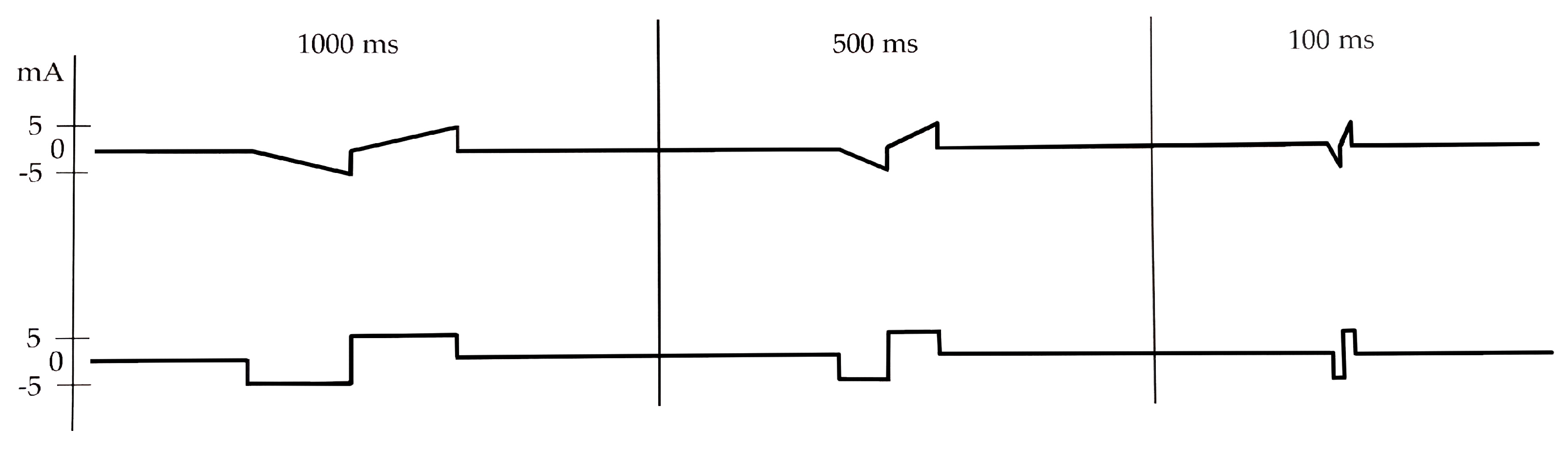
2.6. Stimulation Parameters
2.7. Outcome Measures
2.8. Parameter/Electrode Position Adjustment
2.9. Statistical Analysis
3. Results
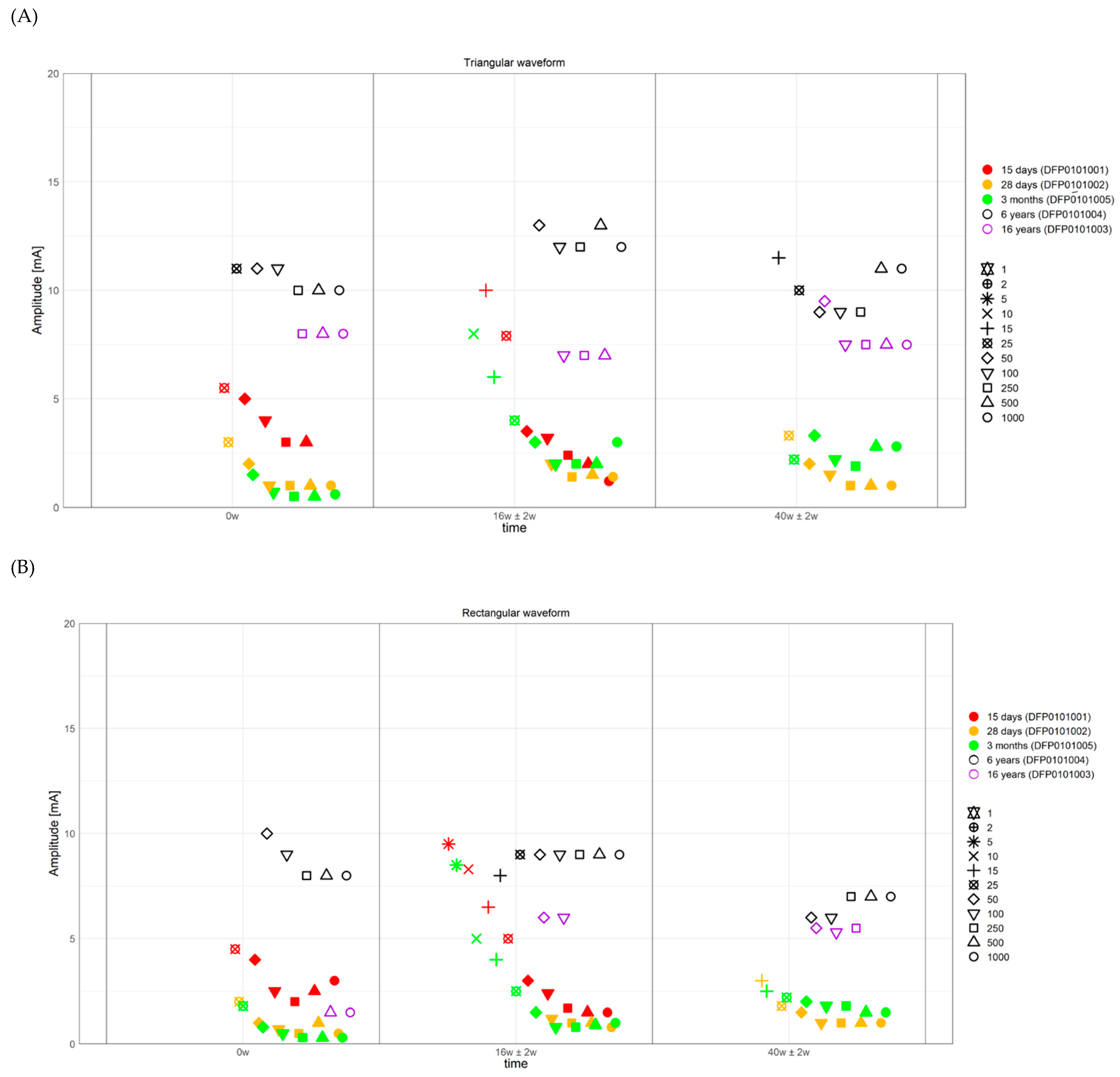
3.1. ZYG Response to Triangular and Rectangular Wave Stimulation
3.2. Use of Trains of Stimulation Bursts
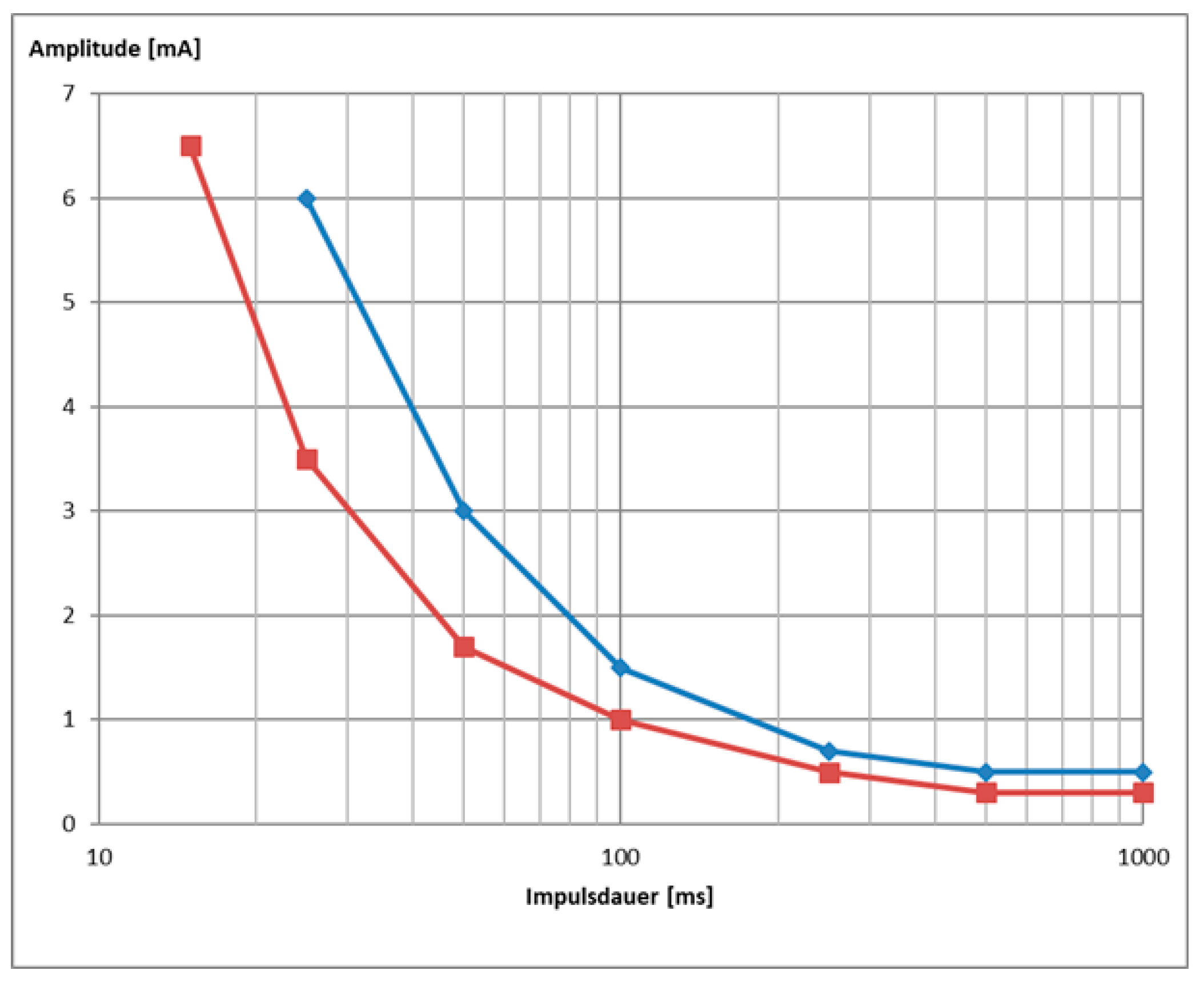
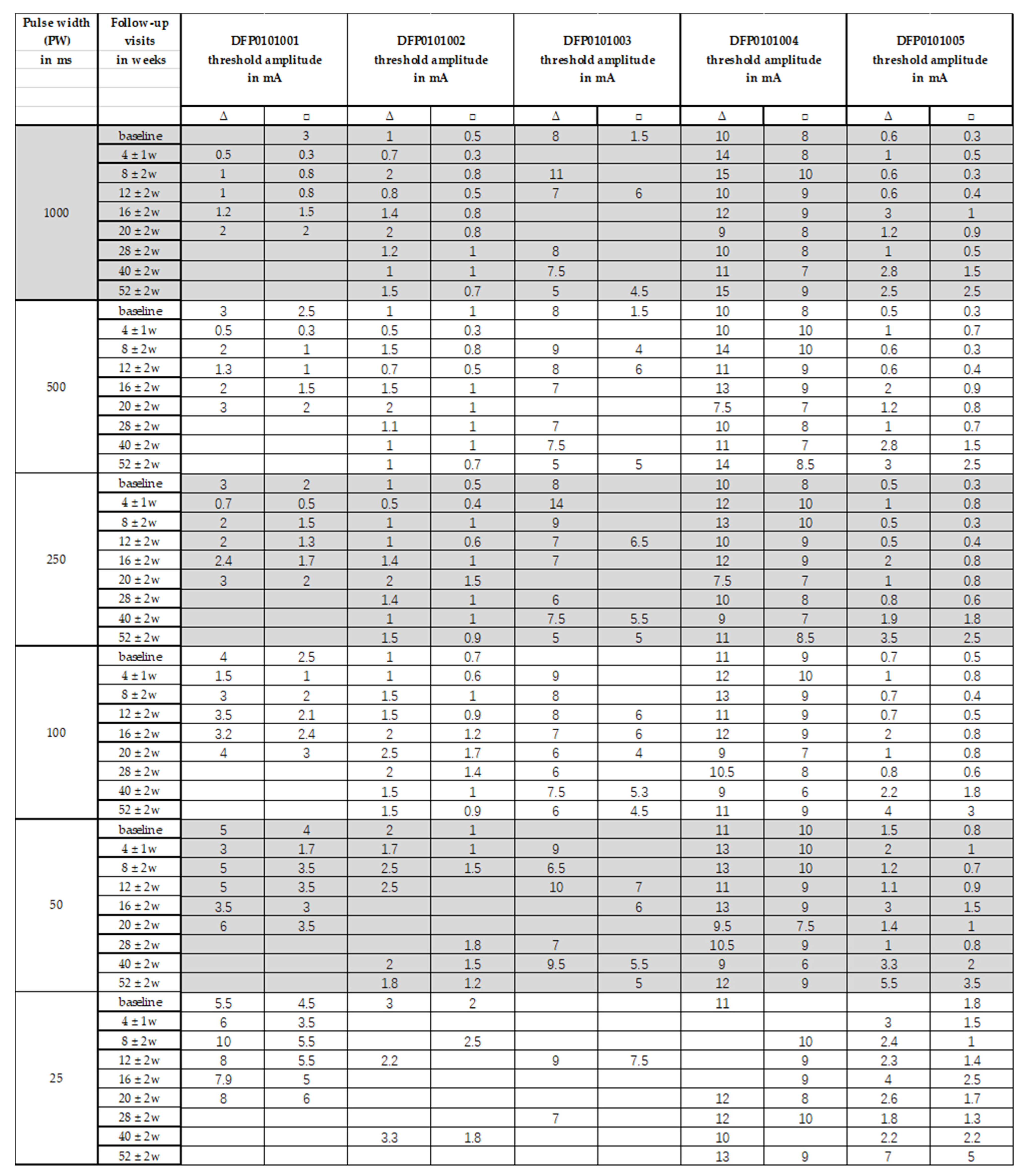
3.3. Strength/Duration Curves
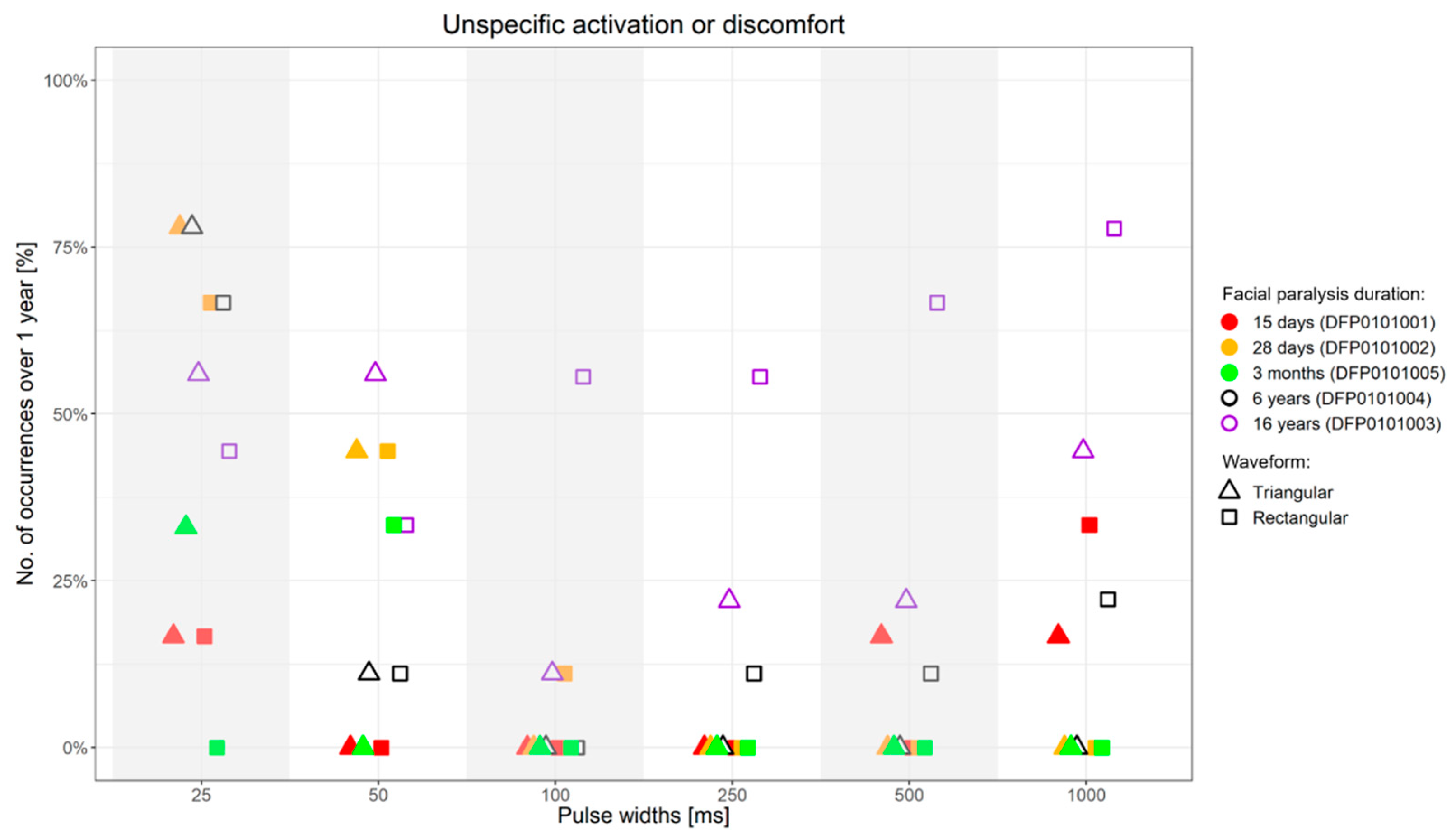
3.4. Side-Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, Y.S.; Choi, J.E.; Kim, S.W.; Baek, S.Y.; Cho, Y.S. Prevalence and associated factors of facial palsy and lifestyle characteristics: Data from the Korean National Health and Nutrition Examination Survey 2010–2012. BMJ Open 2016, 6, e012628. [Google Scholar] [CrossRef] [PubMed]
- Junior, N.; Junior, J.; Gignon, V.; Kitice, A.; Prado, L.; Santos, V. Facial Nerve Palsy: Incidence of Different Ethiologies in a Tertiary Ambulatory. Int. Arch. Otorhinolaryngol. 2009, 13, 167–171. [Google Scholar]
- Odebode, T.; Ologe, F. Facial nerve palsy after head injury: Case incidence, causes, clinical profile and outcome. J. Trauma 2006, 61, 388–391. [Google Scholar] [CrossRef]
- Peitersen, E. Bell’s palsy: The spontaneous course of 2500 peripheral facial nerve palsies of different etiologies. Acta Otolaryngol. Suppl. 2002, 122, 4–30. [Google Scholar] [CrossRef]
- Rahman, I.; Sadiq, S.A. Ophthalmic management of facial nerve palsy: A review. Surv. Ophthalmol. 2007, 52, 121–144. [Google Scholar] [CrossRef] [PubMed]
- Saadi, R.; Shokri, T.; Schaefer, E.; Hollenbeak, C.; Lighthall, J.G. Depression Rates After Facial Paralysis. Ann. Plast. Surg. 2019, 83, 190–194. [Google Scholar] [CrossRef]
- Hohman, M.H.; Bhama, P.K.; Hadlock, T.A. Epidemiology of iatrogenic facial nerve injury: A decade of experience. Laryngoscope 2014, 124, 260–265. [Google Scholar] [CrossRef]
- de Almeida, J.R.; Guyatt, G.H.; Sud, S.; Dorion, J.; Hill, M.D.; Kolber, M.R.; Lea, J.; Reg, S.L.; Somogyi, B.K.; Westerberg, B.D.; et al. Management of Bell palsy: Clinical practice guideline. CMAJ 2014, 186, 917–922. [Google Scholar] [CrossRef]
- Iseli, T.A.; Harris, G.; Dean, N.R.; Iseli, C.E.; Rosenthal, E.L. Outcomes of static and dynamic facial nerve repair in head and neck cancer. Laryngoscope 2010, 120, 478–483. [Google Scholar] [CrossRef]
- Kosins, A.M.; Hurvitz, K.A.; Evans, G.R.; Wirth, G.A. Facial paralysis for the plastic surgeon. Can. J. Plast. Surg. 2007, 15, 77–82. [Google Scholar] [CrossRef]
- Mehta, R.P. Surgical treatment of facial paralysis. Clin. Exp. Otorhinolaryngol. 2009, 2, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Pavese, C.; Cecini, M.; Lozza, A.; Biglioli, F.; Lisi, C.; Bejor, M.; Dalla Toffola, E. Rehabilitation and functional recovery after masseteric-facial nerve anastomosis. Eur. J. Phys. Rehabil. Med. 2016, 52, 379–388. [Google Scholar] [PubMed]
- Volk, G.F.; Geitner, M.; Geissler, K.; Thielker, J.; Raslan, A.; Mothes, O.; Dobel, C.; Guntinas-Lichius, O. Functional Outcome and Quality of Life After Hypoglossal-Facial Jump Nerve Suture. Front. Surg. 2020, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Volk, G.F.; Pantel, M.; Guntinas-Lichius, O. Modern concepts in facial nerve reconstruction. Head Face Med. 2010, 6, 25. [Google Scholar] [CrossRef] [PubMed]
- Volk, G.F.; Thielker, J.; Moller, M.C.; Majcher, D.; Mastryukova, V.; Altmann, C.S.; Dobel, C.; Guntinas-Lichius, O. Tolerability of facial electrostimulation in healthy adults and patients with facial synkinesis. Eur. Arch. Otorhinolaryngol. 2020, 277, 1247–1253. [Google Scholar] [CrossRef]
- Heckmann, J.G.; Urban, P.P.; Pitz, S.; Guntinas-Lichius, O.; Gagyor, I. The Diagnosis and Treatment of Idiopathic Facial Paresis (Bell’s Palsy). Dtsch. Arztebl. Int. 2019, 116, 692–702. [Google Scholar] [CrossRef]
- Jacobson, S.; Guth, L. An Electrophysiological Study of the Early Stages of Peripheral Nerve Regeneration. Exp. Neurol. 1965, 11, 48–60. [Google Scholar] [CrossRef]
- Jenkins, D.W.; Carruthers, R.R.; Litofsky, A.; Collins, W.F. Electrophysiological Study of Regenerating Peripheral Nerve. Relationship of Size of Fibers and Rate of Growth. J. Neurosurg. 1963, 20, 344–347. [Google Scholar] [CrossRef]
- Jowett, N.; Kearney, R.E.; Knox, C.J.; Hadlock, T.A. Toward the Bionic Face: A Novel Neuroprosthetic Device Paradigm for Facial Reanimation Consisting of Neural Blockade and Functional Electrical Stimulation. Plast. Reconstr. Surg. 2019, 143, 62e–76e. [Google Scholar] [CrossRef]
- Puls, W.C.; Jarvis, J.C.; Ruck, A.; Lehmann, T.; Guntinas-Lichius, O.; Volk, G.F. Surface electrical stimulation for facial paralysis is not harmful. Muscle Nerve 2020, 61, 347–353. [Google Scholar] [CrossRef]
- Kern, H.; Hofer, C.; Loefler, S.; Zampieri, S.; Gargiulo, P.; Baba, A.; Marcante, A.; Piccione, F.; Pond, A.; Carraro, U. Atrophy, ultra-structural disorders, severe atrophy and degeneration of denervated human muscle in SCI and Aging. Implications for their recovery by Functional Electrical Stimulation, updated 2017. Neurol. Res. 2017, 39, 660–666. [Google Scholar] [CrossRef] [PubMed]
- Hofer, C.; Mayr, W.; Stöhr, H.; Unger, E.; Kern, H. A stimulator for functional activation of denervated muscles. Artif. Organs 2002, 26, 276–279. [Google Scholar] [CrossRef] [PubMed]
- Kern, H.; Carraro, U. Home-Based Functional Electrical Stimulation of Human Permanent Denervated Muscles: A Narrative Review on Diagnostics, Managements, Results and Byproducts Revisited 2020. Diagnostics 2020, 10, 529. [Google Scholar] [CrossRef] [PubMed]
- Edmunds, K.J.; Gislason, M.K.; Arnadottir, I.D.; Marcante, A.; Piccione, F.; Gargiulo, P. Quantitative Computed Tomography and Image Analysis for Advanced Muscle Assessment. Eur. J. Transl. Myol. 2016, 26, 6015. [Google Scholar] [CrossRef] [PubMed]
- Carraro, U.; Boncompagni, S.; Gobbo, V.; Rossini, K.; Zampieri, S.; Mosole, S.; Ravara, B.; Nori, A.; Stramare, R.; Ambrosio, F.; et al. Persistent Muscle Fiber Regeneration in Long Term Denervation. Past, Present, Future. Eur. J. Transl. Myol. 2015, 25, 4832. [Google Scholar] [CrossRef] [PubMed]
- Kern, H.; Carraro, U.; Adami, N.; Biral, D.; Hofer, C.; Forstner, C.; Modlin, M.; Vogelauer, M.; Pond, A.; Boncompagni, S.; et al. Home-based functional electrical stimulation rescues permanently denervated muscles in paraplegic patients with complete lower motor neuron lesion. Neurorehabil. Neural Repair 2010, 24, 709–721. [Google Scholar] [CrossRef]
- Geddes, L.A.; Bourland, J.D. The strength-duration curve. IEEE Trans. Biomed. Eng. 1985, 32, 458–459. [Google Scholar] [CrossRef]
- Carlson, B.M. The Biology of Long-Term Denervated Skeletal Muscle. Eur. J. Transl. Myol. 2014, 24, 3293. [Google Scholar] [CrossRef]
- Cummings, J.P. Conservative management of peripheral nerve injuries utilizing selective electrical stimulation of denervated muscle with exponentially progressive—current forms. J. Orthop. Sports Phys. Ther. 1985, 7, 11–15. [Google Scholar] [CrossRef]
- Woodcock, A.H.; Taylor, P.N.; Ewins, D.J. Long pulse biphasic electrical stimulation of denervated muscle. Artif. Organs 1999, 23, 457–459. [Google Scholar] [CrossRef]
- Thomas, D.S. Muscle Preservation in Denervation Injury Using Continuous Implantable Electrical Stimulation. Master’s Thesis, McGill University, Montreal, QC, Canada, 1992. [Google Scholar]
- Ravara, B.; Hofer, C.; Kern, H.; Guidolin, D.; Porzionato, A.; De Caro, R.; Albertin, G. Dermal papillae flattening of thigh skin in Conus Cauda Syndrome. Eur. J. Transl. Myol. 2018, 28, 7914. [Google Scholar] [CrossRef] [PubMed]
- Albertin, G.; Kern, H.; Hofer, C.; Guidolin, D.; Porzionato, A.; Rambaldo, A.; De Caro, R.; Piccione, F.; Marcante, A.; Zampieri, S. Two years of Functional Electrical Stimulation by large surface electrodes for denervated muscles improve skin epidermis in SCI. Eur. J. Transl. Myol. 2018, 28, 7373. [Google Scholar] [CrossRef] [PubMed]

| Subject’s Code | Gender | Age | FP Duration | FP Side | FP Origin | FP Surgery | FP Surgery Time | SR-nEMG Time |
|---|---|---|---|---|---|---|---|---|
| DFP0101001 | F | 37 | 15 d | R | FP after resection of a intraparotideal facial nerve schwannoma treated with direct nerve suture | FNSAMG | 2 w before study start | 6m |
| DFP0101002 | F | 29 | 28 d | R | Postoperative FP after resection of a vestibular schwannoma | HFJA | 8 m after study start | 12 m |
| DFP0101003 | F | 37 | 16 y 2 m | R | Postoperative FP after resection of multiple meningiomas of the temporal bone | None | N/A | N/A |
| DFP0101004 | M | 59 | 5 y 11 m | L | Intramastoidal facial nerve schwannoma, schwannoma resection and nerve suture with interposition | HFJA | 2 w before study start | 8 m (single fiber activity) |
| DFP0101005 | F | 53 | 3 m 24 d | L | Postoperative FP after resection of a vestibular schwannoma | None | N/A | 12 m |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arnold, D.; Thielker, J.; Klingner, C.M.; Puls, W.C.; Misikire, W.; Guntinas-Lichius, O.; Volk, G.F. Selective Surface Electrostimulation of the Denervated Zygomaticus Muscle. Diagnostics 2021, 11, 188. https://doi.org/10.3390/diagnostics11020188
Arnold D, Thielker J, Klingner CM, Puls WC, Misikire W, Guntinas-Lichius O, Volk GF. Selective Surface Electrostimulation of the Denervated Zygomaticus Muscle. Diagnostics. 2021; 11(2):188. https://doi.org/10.3390/diagnostics11020188
Chicago/Turabian StyleArnold, Dirk, Jovanna Thielker, Carsten M. Klingner, Wiebke Caren Puls, Wengelawit Misikire, Orlando Guntinas-Lichius, and Gerd Fabian Volk. 2021. "Selective Surface Electrostimulation of the Denervated Zygomaticus Muscle" Diagnostics 11, no. 2: 188. https://doi.org/10.3390/diagnostics11020188
APA StyleArnold, D., Thielker, J., Klingner, C. M., Puls, W. C., Misikire, W., Guntinas-Lichius, O., & Volk, G. F. (2021). Selective Surface Electrostimulation of the Denervated Zygomaticus Muscle. Diagnostics, 11(2), 188. https://doi.org/10.3390/diagnostics11020188








