Effect of Exercise on Inflamed Psoas Muscle in Women with Obesity: A Pilot Prospective 18F-FDG PET/CT Study
Abstract
1. Introduction
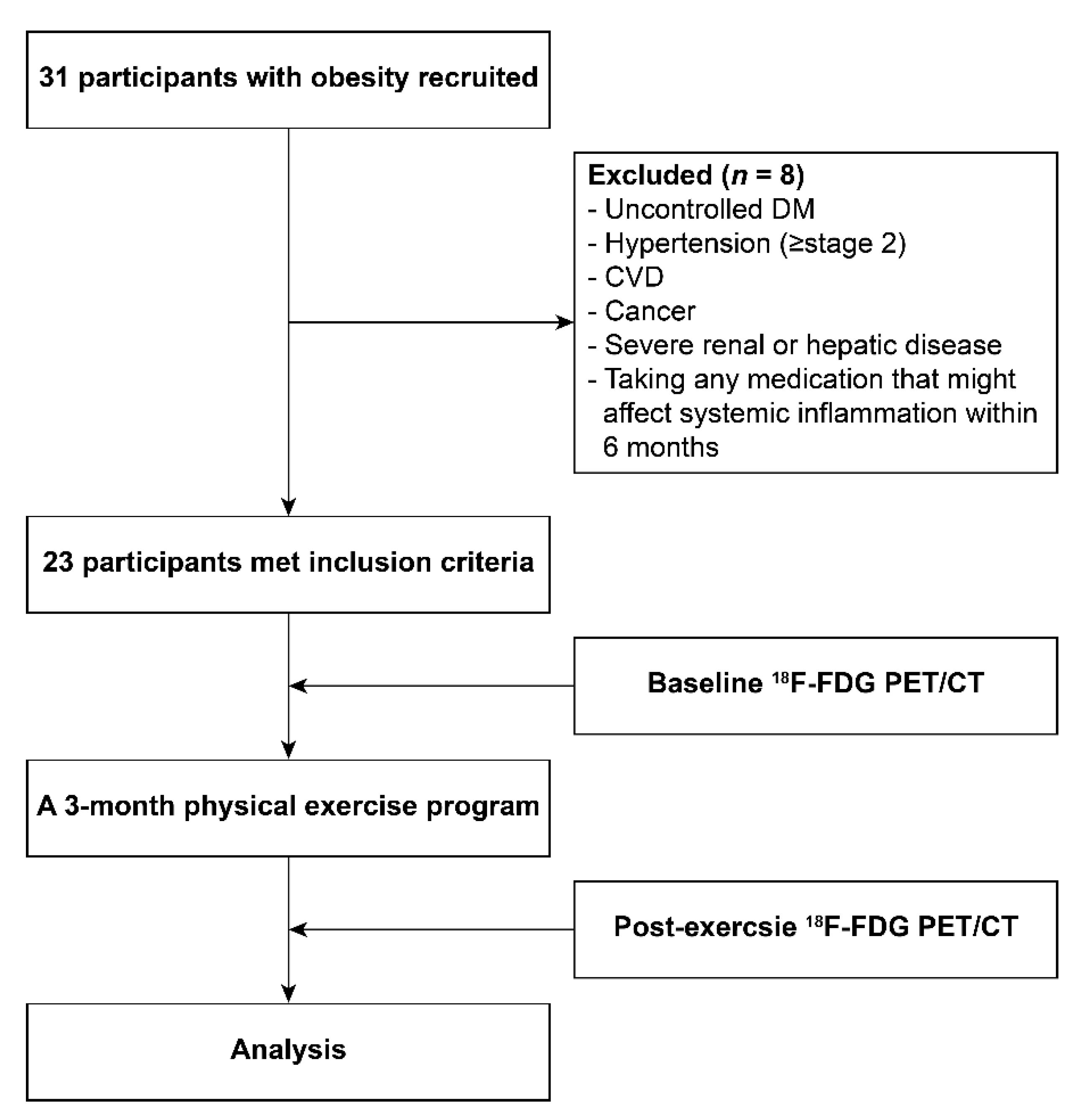
2. Materials and Methods
2.1. Study Participants
2.2. Study Design
2.3. Exercise Program
2.4. Anthropometric and Clinical Laboratory Parameters
2.5. 18F-FDG PET/CT Protocol
2.6. Image Analysis
2.7. Statistical Analysis
3. Results
3.1. Association between PM SUVmax and Systemic Inflammation at Baseline
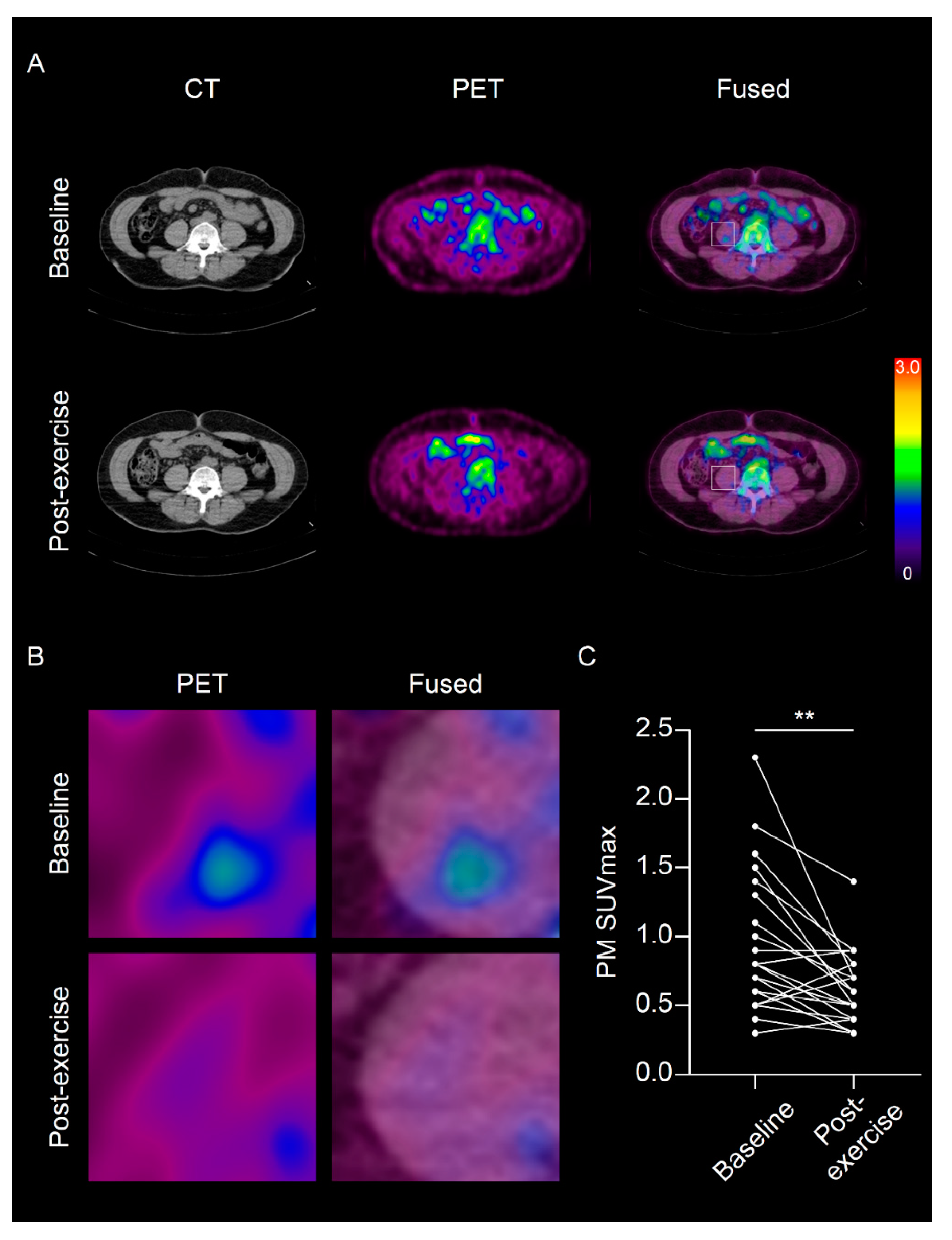
3.2. The Effect of Physical Exercise on PM SUVmax and Systemic Inflammation
3.3. Association between PM SUVmax and Systemic Inflammation after a 3-Month of Physical Exercise Program
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Finucane, M.M.; Stevens, G.A.; Cowan, M.J.; Danaei, G.; Lin, J.K.; Paciorek, C.J.; Singh, G.M.; Gutierrez, H.R.; Lu, Y.; Bahalim, A.N.; et al. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9 1 million participants. Lancet 2011, 377, 557–567. [Google Scholar] [CrossRef]
- Poirier, P.; Giles, T.D.; Bray, G.A.; Hong, Y.; Stern, J.S.; Pi-Sunyer, F.X.; Eckel, R.H. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: An update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2006, 113, 898–918. [Google Scholar] [PubMed]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Aderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Osborn, O.; Olefsky, J.M. The cellular and signaling networks linking the immune system and metabolism in disease. Nat. Med. 2012, 18, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Lumeng, C.N.; Saltiel, A.R. Inflammatory links between obesity and metabolic disease. J. Clin. Investig. 2011, 121, 2111–2117. [Google Scholar] [CrossRef] [PubMed]
- Varma, V.; Yao-Borengasser, A.; Rasouli, N.; Nolen, G.T.; Phanavanh, B.; Starks, T.; Gurley, C.; Simpson, P.; McGehee, R.E., Jr.; Kern, P.A.; et al. Muscle inflammatory response and insulin resistance: Synergistic interaction between macrophages and fatty acids leads to impaired insulin action. Am. J. Physiol. Endocrinol. Metab. 2009, 296, E1300–E1310. [Google Scholar] [CrossRef]
- Libby, P.; Tabas, I.; Fredman, G.; Fisher, E.A. Inflammation and its resolution as determinants of acute coronary syndromes. Circ. Res. 2014, 114, 1867–1879. [Google Scholar] [CrossRef]
- Wu, H.; Ballantyne, C.M. Skeletal muscle inflammation and insulin resistance in obesity. J. Clin. Investig. 2017, 127, 43–54. [Google Scholar] [CrossRef]
- DeFronzo, R.A.; Jacot, E.; Jequier, E.; Maeder, E.; Wahren, J.; Felber, J.P. The effect of insulin on the disposal of intravenous glucose: Results from indirect calorimetry and hepatic and femoral venous catheterization. Diabetes 1981, 30, 1000–1007. [Google Scholar] [CrossRef]
- Petersen, K.F.; Shulman, G.I. Pathogenesis of skeletal muscle insulin resistance in type 2 diabetes mellitus. Am. J. Cardiol. 2002, 90, 11G–18G. [Google Scholar] [CrossRef]
- Ganeshan, K.; Chawla, A. Metabolic regulation of immune responses. Annu. Rev. Immunol. 2014, 32, 609–634. [Google Scholar] [CrossRef] [PubMed]
- Tarkin, J.M.; Joshi, F.R.; Rudd, J.H. PET imaging of inflammation in atherosclerosis. Nat. Rev. Cardiol. 2014, 11, 443–457. [Google Scholar] [CrossRef] [PubMed]
- Dasarathy, S.; Merli, M. Sarcopenia from mechanism to diagnosis and treatment in liver disease. J. Hepatol. 2016, 65, 1232–1244. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Jun, D.W.; Choi, J.; Nam, E.; Son, D.; Choi, Y.Y. Psoas muscle fluorine-18-labelled fluoro-2-deoxy-d-glucose uptake associated with the incidence of existing and incipient metabolic derangement. J. Cachexia Sarcopenia Muscle 2019, 10, 894–902. [Google Scholar] [CrossRef] [PubMed]
- Gleeson, M.; Bishop, N.C.; Stensel, D.J.; Lindley, M.R.; Mastana, S.S.; Nimmo, M.A. The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease. Nat. Rev. Immunol. 2011, 11, 607–615. [Google Scholar] [CrossRef]
- Vissers, D.; Hens, W.; Taeymans, J.; Baeyens, J.P.; Poortmans, J.; Van Gaal, L. The effect of exercise on visceral adipose tissue in overweight adults: A systematic review and meta-analysis. PLoS ONE 2013, 8, e56415. [Google Scholar] [CrossRef]
- Verheggen, R.J.; Maessen, M.F.; Green, D.J.; Hermus, A.R.; Hopman, M.T.; Thijssen, D.H. A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: Distinct effects on body weight and visceral adipose tissue. Obes. Rev. 2016, 17, 664–690. [Google Scholar] [CrossRef]
- Pahk, K.; Kim, E.J.; Joung, C.; Seo, H.S.; Kim, S. Exercise training reduces inflammatory metabolic activity of visceral fat assessed by 18F-FDG PET/CT in obese women. Clin. Encocrinol. 2020, 93, 127–134. [Google Scholar] [CrossRef]
- Gielen, S.; Adams, V.; Möbius-Winkler, S.; Linke, A.; Erbs, S.; Yu, J.; Kempf, W.; Schubert, A.; Schuler, G.; Hambrecht, R. Anti-inflammatory effects of exercise training in the skeletal muscle of patients with chronic heart failure. J. Am. Coll. Cardiol. 2003, 42, 861–868. [Google Scholar] [CrossRef]
- Samaan, M.C.; Marcinko, K.; Sikkema, S.; Fullerton, M.D.; Ziafazeli, T.; Khan, M.I.; Steinberg, G.R. Endurance interval training in obese mice reduces muscle inflammation and macrophage content independently of weight loss. Physiol. Rep. 2014, 2, e12012. [Google Scholar] [CrossRef]
- Kim, M.K.; Lee, W.Y.; Kang, J.H.; Kang, J.H.; Kim, B.T.; Kim, S.M.; Kim, E.M.; Suh, S.H.; Shin, H.J.; Lee, K.R.; et al. 2014 clinical practice guidelines for overweight and obesity in Korea. Endocrinol. Metab. 2014, 29, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Maceral, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A.; et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1081–1093. [Google Scholar] [CrossRef] [PubMed]
- Zuckerman, J.; Ades, M.; Mullie, L.; Trnkus, A.; Morin, J.F.; Langlois, Y.; Ma, F.; Levental, M.; Morais, J.A.; Afilalo, J. Psoas muscle area and length of stay in older adults undergoing cardiac operations. Ann. Thorac. Surg. 2017, 103, 1498–1504. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.J.; Kim, S.; Kang, D.O.; Seo, H.S. Metabolic activity of the spleen and bone marrow in patients with acute myocardial infarction evaluated by 18f-fluorodeoxyglucose positron emission tomograpic imaging. Circ. Cardiovasc. Imaging 2014, 7, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Emami, H.; Singh, P.; MacNabb, M.; Vucic, E.; Lavender, Z.; Rudd, J.H.; Fayad, Z.A.; Lehrer-Graiwer, J.; Korsgren, M.; Figueroa, A.L.; et al. Splenic metabolic activity predicts risk of future cardiovascular events: Demonstration of a cardiosplenic axis in humans. JACC Cardiovasc. Imaging 2015, 8, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Lackey, D.E.; Olefsky, J.M. Regulation of metabolism by the innate immune system. Nat. Rev. Endocrinol. 2016, 12, 15–28. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.M.; Perrard, X.Y.; Brunner, G.; Lui, H.; Sparks, L.M.; Smith, S.R.; Wang, X.; Shi, Z.Z.; Lewis, D.E.; Wu, H.; et al. Intermuscular and perimuscular fat expansion in obesity correlates with skeletal muscle T cell and macrophage infiltration and insulin resistance. Int. J. Obes. 2015, 39, 1607–1618. [Google Scholar] [CrossRef]
- Fink, L.N.; Costford, S.R.; Lee, Y.S.; Jensen, T.E.; Bilan, P.J.; Oberbach, A.; Blüher, M.; Olefsky, J.M.; Sams, A.; Klip, A. Pro-inflammatory macrophages increase in skeletal muscle of high fat-fed mice and correlate with metabolic risk markers in humans. Obesity 2014, 22, 747–757. [Google Scholar] [CrossRef]
- Lumeng, C.N.; Deyoung, S.M.; Saltiel, A.R. Macrophages block insulin action in adipocytes by altering expression of signaling and glucose transport proteins. Am. J. Physiol. Endocrinol. Metab. 2007, 292, E166–E174. [Google Scholar] [CrossRef]
- Freemerman, A.J.; Johnson, A.R.; Sacks, G.N.; Milner, J.J.; Kirk, E.L.; Troester, M.A.; Macintyre, A.N.; Goraksha-Hicks, P.; Rathmell, J.C.; Makowski, L. Metabolic reprogramming of macrophages glucose transporter 1 (GLUT1)-mediated glucose metabolism drives a proinflammatory phenotype. J. Biol. Chem. 2014, 289, 7884–7896. [Google Scholar] [CrossRef]
- Weisberg, S.P.; McCann, D.; Desai, M.; Rosenbaum, M.; Leibel, R.L.; Ferrante, A.W., Jr. Obesity is associated with macrophage accumulation in adipose tissue. J. Clin. Investig. 2003, 112, 1796–1808. [Google Scholar] [PubMed]
- Kewalramani, G.; Fink, L.N.; Asadi, F.; Klip, A. Palmitate-activated macrophages confer insulin resistance to muscle cells by a mechanism involving protein kinase C θ and ε. PLoS ONE 2011, 6, e26947. [Google Scholar]
- Samokhvalov, V.; Bilan, P.J.; Schertzer, J.D.; Antonescu, C.N.; Klip, A. Palmitate-and lipopolysaccharide-activated macrophages evoke contrasting insulin responses in muscle cells. Am. J. Physiol. Endocrinol. Metab. 2009, 296, E37–E46. [Google Scholar] [PubMed]
- Timmerman, K.L.; Flynn, M.G.; Coen, P.M.; Markofski, M.M.; Pence, B.D. Exercise training-induced lowering of inflammatory (CD14+ CD16+) monocytes: A role in the anti-inflammatory influence of exercise? J. Leukoc. Biol. 2008, 84, 1271–1278. [Google Scholar]
- Le, N.H.; Kim, C.S.; Park, T.; Park, J.H.; Sung, M.K.; Lee, D.G.; Hong, S.M.; Choe, S.Y.; Goto, T.; Kawada, T.; et al. Quercetin protects against obesity-induced skeletal muscle inflammation and atrophy. Mediat. Inflamm. 2014, 2014, 834294. [Google Scholar]
- Shabani, M.; Sadeghi, A.; Hosseini, H.; Teimouri, M.; Babaei Khorzoughi, R.; Pasalar, P.; Meshkani, R. Resveratrol alleviates obesity-induced skeletal muscle inflammation via decreasing M1 macrophage polarization and increasing the regulatory T cell population. Sci. Rep. 2020, 10, 3791. [Google Scholar]
- Haffner, S.; Temprosa, M.; Crandall, J.; Fowler, S.; Goldberg, R.; Horton, E.; Marcovina, S.; Mather, K.; Orchard, T.; Ratner, R.; et al. Intensive lifestyle intervention or metformin on inflammation and coagulation in participants with impaired glucose tolerance. Diabetes 2005, 54, 1566–1572. [Google Scholar]
| Baseline Characteristics | n = 23 |
|---|---|
| Age (years) | 46 ± 8.0 |
| Height (cm) | 156.8 ± 5.5 |
| Smoking (current), n (%) | 0 (0) |
| Alcohol drinking, n (%) | 8 (34.8) |
| Menopause, n (%) | 12 (52.2) |
| Hypertension (stage 1), n (%) | 4 (17.4) |
| Diabetes, n (%) | 0 (0) |
| Dyslipidemia, n (%) | 7 (30.4) |
| Medication, n (%) | 0 (0) |
| Parameters | Baseline | Post-Exercise | p |
|---|---|---|---|
| Body weight (kg) | 65.3 ± 7.5 | 62.4 ± 8 | <0.001 * |
| BMI (kg/m2) | 26.5 ± 2.2 | 25.3 ± 2.5 | <0.001 * |
| Waist circumference (cm) | 83.2 ± 5.5 | 81.3 ± 5.9 | 0.05 * |
| Hip circumference (cm) | 98.6 ± 5.1 | 95.4 ± 4.6 | <0.001 * |
| AST (IU/L) | 12.3 ± 3.9 | 11.7 ± 5.1 | 0.47 |
| ALT (IU/L) | 21 ± 3.9 | 21 ± 4.2 | 0.69 |
| Triglyceride (mg/dL) | 105.7 ± 47.3 | 112.1 ± 46.6 | 0.26 |
| Total cholesterol (mg/dL) | 177.4 ± 30.6 | 178.3 ± 30 | 0.89 |
| HDL-C (mg/dL) | 49.9 ± 11.3 | 49.9 ± 9.2 | 0.71 |
| LDL-C (mg/dL) | 106.3 ± 29.5 | 101.3 ± 37.9 | 0.77 |
| Glucose (mg/dL) | 89 ± 8.3 | 88 ± 9.6 | 0.47 |
| SBP (mmHg) | 123.7 ± 16.4 | 116.4 ± 10.3 | 0.002 * |
| DBP (mmHg) | 75 ± 11 | 71.6 ± 8 | 0.009 * |
| VAT area (cm2) | 154.4 ± 32.7 | 142.3 ± 37.5 | 0.007 * |
| PM area (cm2) | 18.5 ± 2.5 | 18.4 ± 2.3 | 0.402 |
| hsCRP (mg/L) | 1.98 ± 3.42 | 0.86 ± 1.34 | 0.006 * |
| Spleen SUVmax | 1.73 ± 0.28 | 1.6 ± 3.21 | 0.004 * |
| BM SUVmax | 1.55 ± 0.26 | 1.43 ± 0.22 | 0.018 * |
| Status | Parameters | PM SUVmax | |
|---|---|---|---|
| r | p | ||
| Baseline | hsCRP | 0.611 | 0.002 * |
| Spleen SUVmax | 0.435 | 0.038 * | |
| BM SUVmax | 0.315 | 0.145 | |
| PM area (cm2) | −0.104 | 0.637 | |
| Post-exercise | hsCRP | −0.021 | 0.923 |
| Spleen SUVmax | 0.075 | 0.735 | |
| BM SUVmax | 0.244 | 0.263 | |
| PM area (cm2) | 0.071 | 0.748 | |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| Variable | Coefficients (95% CI) | p | r | p |
| Age | 0.008 (−0.02–0.036) | 0.549 | ||
| BMI (kg/m2) | 0.15 (0.073–0.227) | 0.001 * | 0.177 | 0.468 |
| Waist circumference (cm) | 0.044 (0.008–0.08) | 0.02 * | −0.032 | 0.897 |
| Hip circumference (cm) | 0.043 (0.002–0.083) | 0.039 * | 0.031 | 0.9 |
| AST (IU/L) | −0.009 (−0.068–0.05) | 0.752 | ||
| ALT (IU/L) | 0.029 (−0.027–0.086) | 0.292 | ||
| Triglyceride (mg/dL) | 0.002 (−0.003–0.007) | 0.445 | ||
| Total cholesterol (mg/dL) | 0 (−0.007–0.008) | 0.946 | ||
| HDL-C (mg/dL) | −0.01 (−0.03–0.009) | 0.297 | ||
| LDL-C (mg/dL) | 0.001 (−0.007–0.009) | 0.797 | ||
| Glucose (mg/dL) | −0.003 (−0.031–0.024) | 0.804 | ||
| SBP (mmHg) | 0.006 (−0.008–0.019) | 0.382 | ||
| DBP (mmHg) | 0.012 (−0.008–0.032) | 0.228 | ||
| VAT area (cm2) | 0.004 (−0.003–0.011) | 0.295 | ||
| PM area (cm2) | −0.047 (−0.135–0.042) | 0.284 | ||
| Spleen SUVmax | 0.798 (0.077–1.519) | 0.032 * | 0.347 | 0.145 |
| BM SUVmax | 0.278 (−0.579–1.135) | 0.508 | ||
| hsCRP (mg/L) | 0.111 (0.068–0.155) | <0.001 * | 0.636 | 0.003 ** |
| Univariate | ||
|---|---|---|
| Variable | Coefficients (95% CI) | p |
| Age | 0 (−0.016–0.015) | 0.956 |
| BMI (kg/m2) | 0.024 (−0.025–0.072) | 0.325 |
| Waist circumference (cm) | 0.007 (−0.014–0.027) | 0.508 |
| Hip circumference (cm) | 0.011 (−0.016–0.037) | 0.406 |
| AST (IU/L) | −0.001 (−0.026–0.024) | 0.914 |
| ALT (IU/L) | 0 (−0.003–0.003) | 0.753 |
| Triglyceride (mg/dL) | −0.001 (−0.004–0.001) | 0.321 |
| Total cholesterol (mg/dL) | −0.00009 (−0.004–0.004) | 0.965 |
| HDL-C (mg/dL) | 0.004 (−0.01–0.017) | 0.576 |
| LDL-C (mg/dL) | 0.001 (−0.002–0.004) | 0.587 |
| Glucose (mg/dL) | −0.003 (−0.016–0.01) | 0.662 |
| SBP (mmHg) | 0 (−0.013–0.012) | 0.973 |
| DBP (mmHg) | −0.003 (−0.019–0.013) | 0.712 |
| VAT area (cm2) | −0.001 (−0.004–0.002) | 0.54 |
| PM area (cm2) | 0.006 (−0.047–0.06) | 0.802 |
| Spleen SUVmax | 0.117 (−0.456–0.689) | 0.676 |
| BM SUVmax | 0.287 (−0.268–0.841) | 0.295 |
| hsCRP (mg/L) | −0.031 (−0.141–0.079) | 0.567 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pahk, K.; Kim, E.J.; Joung, C.; Kwon, H.W.; Seo, H.S.; Kim, S. Effect of Exercise on Inflamed Psoas Muscle in Women with Obesity: A Pilot Prospective 18F-FDG PET/CT Study. Diagnostics 2021, 11, 164. https://doi.org/10.3390/diagnostics11020164
Pahk K, Kim EJ, Joung C, Kwon HW, Seo HS, Kim S. Effect of Exercise on Inflamed Psoas Muscle in Women with Obesity: A Pilot Prospective 18F-FDG PET/CT Study. Diagnostics. 2021; 11(2):164. https://doi.org/10.3390/diagnostics11020164
Chicago/Turabian StylePahk, Kisoo, Eung Ju Kim, Chanmin Joung, Hyun Woo Kwon, Hong Seog Seo, and Sungeun Kim. 2021. "Effect of Exercise on Inflamed Psoas Muscle in Women with Obesity: A Pilot Prospective 18F-FDG PET/CT Study" Diagnostics 11, no. 2: 164. https://doi.org/10.3390/diagnostics11020164
APA StylePahk, K., Kim, E. J., Joung, C., Kwon, H. W., Seo, H. S., & Kim, S. (2021). Effect of Exercise on Inflamed Psoas Muscle in Women with Obesity: A Pilot Prospective 18F-FDG PET/CT Study. Diagnostics, 11(2), 164. https://doi.org/10.3390/diagnostics11020164






