Opportunistic Colonoscopy Cancer Screening Pays off in Romania—A Single-Centre Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Colonoscopy Procedure
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
Comparison between Age Groups and Gender
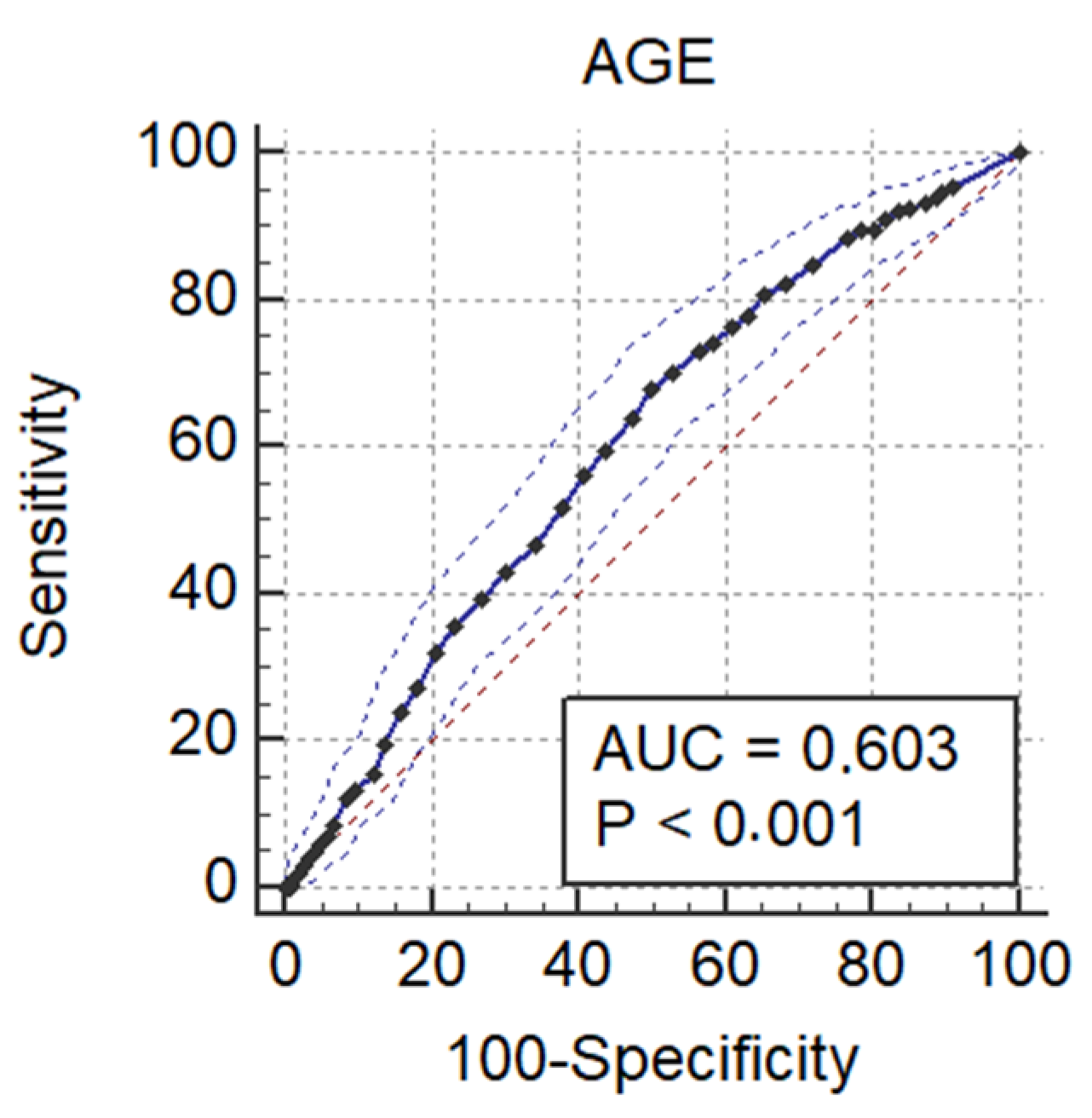
3.2. Factors Associated with ADR
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.; Jemal, A. Cancer statistics, 2021. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef] [PubMed]
- ECIS—European Cancer Information System. Available online: https://ecis.jrc.ec.europa.eu (accessed on 30 September 2021).
- Ionescu, E.M.; Tieranu, C.G.; Maftei, D.; Grivei, A.; Olteanu, A.O.; Arbanas, T.; Calu, V.; Musat, S.; Mihaescu-Pintia, C.; Cucu, I.C. Colorectal Cancer Trends of 2018 in Romania-an Important Geographical Variation Between Northern and Southern Lands and High Mortality Versus European Averages. J. Gastrointest. Cancer 2021, 52, 222–228. [Google Scholar] [CrossRef]
- Globocan 2020—New Global Cancer Data. Available online: https://www.uicc.org/news/globocan-2020-new-global-cancer-data (accessed on 30 September 2021).
- Lin, J.S.; Piper, M.A.; Perdue, L.A.; Rutter, C.M.; Webber, E.M.; O’Connor, E.; Smith, N.; Whitlock, E.P. Screening for colorectal cancer. An updated systematic review for the U.S. preventive services task force. JAMA 2016, 315, 2576–2594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lansdorp-Vogelaar, I.; Knudsen, A.B.; Brenner, H. Cost-effectiveness of colorectal cancer screening. Epidemiol. Rev. 2011, 33, 88–100. [Google Scholar] [CrossRef] [Green Version]
- Lin, J.S.; Perdue, L.A.; Henrikson, N.B.; Bean, S.I.; Blasi, P.R. Screening for colorectal cancer: Updated evidence report and systematic review for the US Preventive Services Task Force. JAMA 2021, 325, 1978–1997. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.; Mandrik, O.; Whyte, S.; Saunders, C.L.; Griffin, S.J.; Usher-Smith, J.A. Should colorectal cancer screening start at different ages for men and women? Cost-effectiveness analysis for a resource-constrained service. Cancer Rep. 2021, 4, e1344. [Google Scholar] [CrossRef]
- Shaukat, A.; Kahi, C.J.; Burke, C.A.; Rabeneck, L.; Sauer, B.G.; Rex, D.K. ACG Clinical Guidelines: Colorectal Cancer Screening 2021. Am. J. Gastroenterol. 2021, 116, 458–479. [Google Scholar] [CrossRef]
- Schoenfeld, P.; Cash, B.; Flood, A.; Dobhan, R.; Eastone, J.; Coyle, W.; Kikendall, J.W.; Kim, H.M.; Weiss, D.G.; Emory, T.; et al. Colonoscopic screening of average-risk women for colorectal neoplasia. N. Engl. J. Med. 2005, 352, 2061–2068. [Google Scholar] [CrossRef]
- Regula, J.; Rupinski, M.; Kraszewska, E. Colonoscopy in colorectal-cancer screening for detection of advanced neoplasia. N. Engl. J. Med. 2006, 355, 1863–1872. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, D.A.; Weiss, D.G.; Bond, J.H.; Ahnen, D.J.; Garewal, H.; Chejfec, G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N. Engl. J. Med. 2000, 343, 162–168. [Google Scholar] [CrossRef]
- Bielawska, B.; Dubé, C. Colorectal cancer screening: It is not time for a radical shift. CMAJ 2020, 192, E51–E52. [Google Scholar] [CrossRef] [Green Version]
- Lai, E.J.; Calderwood, A.H.; Doros, G.; Fix, O.K.; Jacobson, B.C. The Boston bowel preparation scale: A valid and reliable instrument for colonoscopy-oriented research. Gastrointest. Endosc. 2009, 69, 620–625. [Google Scholar] [CrossRef] [Green Version]
- Morson, B.C.; Sobin, L.H. Histological typing of intestinal tumours. In International Histological Classifcation of Tumours; World Health Organization: Geneva, Switzerland, 1976. [Google Scholar]
- Buskermolen, M.; Cenin, D.R.; Helsingen, L.M.; Guyatt, G.; Vandvik, P.O.; Haug, U.; Bretthauer, M.; Lansdorp-Vogelaar, I. Colorectal cancer screening with faecal immunochemical testing, sigmoidoscopy or colonoscopy: A microsimulation modelling study. BMJ 2019, 367, l5383. [Google Scholar] [CrossRef] [Green Version]
- Schlemper, R.J.; Riddell, R.H.; Kato, Y.; Borchard, F.; Cooper, H.S.; Dawsey, S.M.; Dixon, M.F.; Fenoglio-Preiser, C.M.; Fléjou, J.-F.; Geboes, K. Vienna classifcation of gastrointestinal epithelial neoplasia. Gut 2000, 47, 251–255. [Google Scholar] [CrossRef] [Green Version]
- Rex, D.K.; Boland, C.R.; Dominitz, J.A.; Giardiello, F.M.; Johnson, D.A.; Kaltenbach, T.; Levin, T.R.; Lieberman, D.; Robertson, D.J. Colorectal Cancer Screening: Recommendations for Physicians and Patients From the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2017, 153, 307–323. [Google Scholar] [CrossRef]
- Sporea, I.; Popescu, A.; Bataga, S. Opportunistic colorectal cancer screening—how often did we found pathology in clinical practice? J. Gastrointest. Liver Dis. 2014, 23 (Suppl. 1), 9–10. [Google Scholar]
- Ionescu, E.; Nicolaie, T.; Gologan, S.; Mocanu, A.; Ditescu, C.; Arbanas, T.; Stoicescu, A.; Teiusanu, A.; Andrei, M.; Diculescu, M.; et al. Opportunistic Colorectal Cancer Screening using colonoscopy. Comparative Results between two Historical Cohorts in Bucharest, Romania. J. Gastrointest. Liver Dis. JGLD 2015, 24, 171–176. [Google Scholar] [CrossRef] [Green Version]
- Delavari, A.; Bishehsari, F.; Salimzadeh, H.; Khosravi, P.; Delavari, F.; Nasseri-Moghaddam, S.; Merat, S.; Ansari, R.; Vahedi, H.; Shahbazkhani, B.; et al. Adenoma detection rates in an opportunistic screening colonoscopy program in Iran, a country with rising colorectal cancer incidence. BMC Gastroenterol. 2014, 14, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almadi, M.A.; Allehibi, A.; Aljebreen, M.A.; Alharbi, O.R.; Azzam, N.; Aljebreen, A.M. Findings during screening colonoscopies in a Middle Eastern cohort. Saudi J. Gastroenterol. 2019, 25, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Corley, D.A.; Jensen, C.D.; Marks, A.R.; Zhao, W.K.; Lee, J.K.; Doubeni, C.A.; Zauber, A.G.; de Boer, J.; Fireman, B.H.; Schottinger, J.E.; et al. Adenoma detection rate and risk of colorectal cancer and death. N. Engl. J. Med. 2014, 370, 1298–1306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vemulapalli, K.C.; Wilder, S.W.; Kahi, C.J.; Rex, D.K. Long-Term Assessment of the Cecal Intubation Rates in High-Performing Colonoscopists: Time for Review. Clin. Transl. Gastroenterol. 2020, 11, e00153. [Google Scholar] [CrossRef]
- Lee, J.K.; Jensen, C.D.; Levin, T.R.; Zauber, A.G.; Schottinger, J.E.; Quinn, V.P.; Udaltsova, N.; Zhao, W.K.; Fireman, B.H.; Quesenberry, C.P. Long-term Risk of Colorectal Cancer and Related Deaths After a Colonoscopy With Normal Findings. JAMA Intern. Med. 2019, 179, 153–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, G.; Feng, Z.; Liu, H.; Nie, Y.; Liang, Y.; Li, K. Mass screening for colorectal cancer in a population of two million older adults in Guangzhou, China. Sci. Rep. 2019, 9, 10424. [Google Scholar] [CrossRef] [Green Version]
- European Colorectal Cancer Screening Guidelines Working Group; von Karsa, L.; Patnick, J.; Segnan, N.; Atkin, W.; Halloran, S.; Lansdorp-Vogelaar, I.; Malila, N.; Minozzi, S.; Moss, S.; et al. European guidelines for quality assurance in colorectal cancer screening and diagnosis: Overview and introduction to the full supplement publication. Endoscopy 2013, 45, 51–59. [Google Scholar] [CrossRef] [Green Version]
- Melson, J.E.; Imperiale, T.F.; Itzkowitz, S.H.; Llor, X.; Kochman, M.L.; Grady, W.M.; Schoen, R.E.; Burke, C.A.; Shaukat, A.; Rabeneck, L.; et al. AGA White Paper: Roadmap for the Future of Colorectal Cancer Screening in the United States. Clin. Gastroenterol. Hepatol. 2020, 18, 2667–2678. [Google Scholar] [CrossRef]
- Chang, J.Y.; Moon, C.M.; Lee, H.J.; Yang, H.J.; Jung, Y.; Kim, S.W.; Jung, S.-A.; Byeon, J.-S. Predictive factors for missed adenoma on repeat colonoscopy in patients with suboptimal bowel preparation on initial colonoscopy: A KASID multicenter study. PLoS ONE 2018, 13, e0195709. [Google Scholar] [CrossRef] [Green Version]
- Adike, A.; Buras, M.R.; Gurudu, S.R.; Leighton, J.A.; Faigel, D.O.; Ruff, K.C.; Umar, S.B.; Ramirez, F.C. Is the level of cleanliness using segmental Boston bowel preparation scale associated with a higher adenoma detection rate? Ann. Gastroenterol. 2018, 31, 217–223. [Google Scholar] [CrossRef]
| Parameter | N (%), Mean ± SD |
|---|---|
| Age (years) | 59.0 ± 10.9 |
| Gender (female) | 1050 (59.5%) |
| Boston score | 6.8 ± 1.3 |
| Good to excellent preparation (≥6) | 1640 (92.2%) |
| Unsatisfactory to poor preparation (<6) | 138 (7.7%) |
| Caecal intubation | 1770 (99.5%) |
| Parameter | N (%) |
|---|---|
| Polyps | 873 (49.1%) |
| Hyperplastic polyps | 156 (8.7%) |
| Serrated polyps | 22 (1.2%) |
| Adenomas | 695 (39.0%) |
| Villous adenoma | 21 (3.1%) |
| Tubular adenoma | 378 (54.3%) |
| Tubular-villous adenoma | 296 (42.5%) |
| Advanced adenomas | 142 (7.9%) |
| Invasive carcinomas | 96 (5.4%) |
| High grade dysplasia | 246 (13.8%) |
| Overall | <50 Years | 50–75 Years | >75 Years | p-Value | |
|---|---|---|---|---|---|
| Number | 1.778 | 362 | 1305 | 111 | - |
| Age (years) | 59.0 ± 10.9 | 43.5 ± 1.6 | 61.6 ± 7.0 | 79.5 ± 2.9 | - |
| Female | 1050 (59.0%) | 202 (55.8%) | 788 (60.3%) | 60 (54.0%) | 0.17 |
| Adenoma | |||||
| Number | 695 (39.0%) | 105 (29.0%) | 555 (42.5%) | 38 (34.2%) | 0.01 |
| Right size | 501 (28.1%) | 55 (15.1%) | 374 (28.6%) | 45 (32.1%) | 0.001 |
| Advanced | 142 (7.9%) | 27 (7.2%) | 77 (5.9%) | 38 (34.2%) | <0.0001 |
| High dysplasia | 246 (13.8%) | 17 (4.6%) | 241 (16.3%) | 15 (13.5%) | <0.0001 |
| Colorectal cancer | 96 (5.4%) | 10 (2.7%) | 67 (5.1%) | 19 (17.1%) | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rațiu, I.; Lupușoru, R.; Vora, P.; Popescu, A.; Sporea, I.; Goldiș, A.; Dănilă, M.; Miuțescu, B.; Barbulescu, A.; Hnatiuc, M.; et al. Opportunistic Colonoscopy Cancer Screening Pays off in Romania—A Single-Centre Study. Diagnostics 2021, 11, 2393. https://doi.org/10.3390/diagnostics11122393
Rațiu I, Lupușoru R, Vora P, Popescu A, Sporea I, Goldiș A, Dănilă M, Miuțescu B, Barbulescu A, Hnatiuc M, et al. Opportunistic Colonoscopy Cancer Screening Pays off in Romania—A Single-Centre Study. Diagnostics. 2021; 11(12):2393. https://doi.org/10.3390/diagnostics11122393
Chicago/Turabian StyleRațiu, Iulia, Raluca Lupușoru, Prateek Vora, Alina Popescu, Ioan Sporea, Adrian Goldiș, Mirela Dănilă, Bogdan Miuțescu, Andreea Barbulescu, Madalina Hnatiuc, and et al. 2021. "Opportunistic Colonoscopy Cancer Screening Pays off in Romania—A Single-Centre Study" Diagnostics 11, no. 12: 2393. https://doi.org/10.3390/diagnostics11122393
APA StyleRațiu, I., Lupușoru, R., Vora, P., Popescu, A., Sporea, I., Goldiș, A., Dănilă, M., Miuțescu, B., Barbulescu, A., Hnatiuc, M., Diaconescu, R., Tăban, S., Lazar, F., & Șirli, R. (2021). Opportunistic Colonoscopy Cancer Screening Pays off in Romania—A Single-Centre Study. Diagnostics, 11(12), 2393. https://doi.org/10.3390/diagnostics11122393









