Preoperative Magnetic Resonance Imaging as a Diagnostic Aid for Hypermobile Lateral Meniscus
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Design
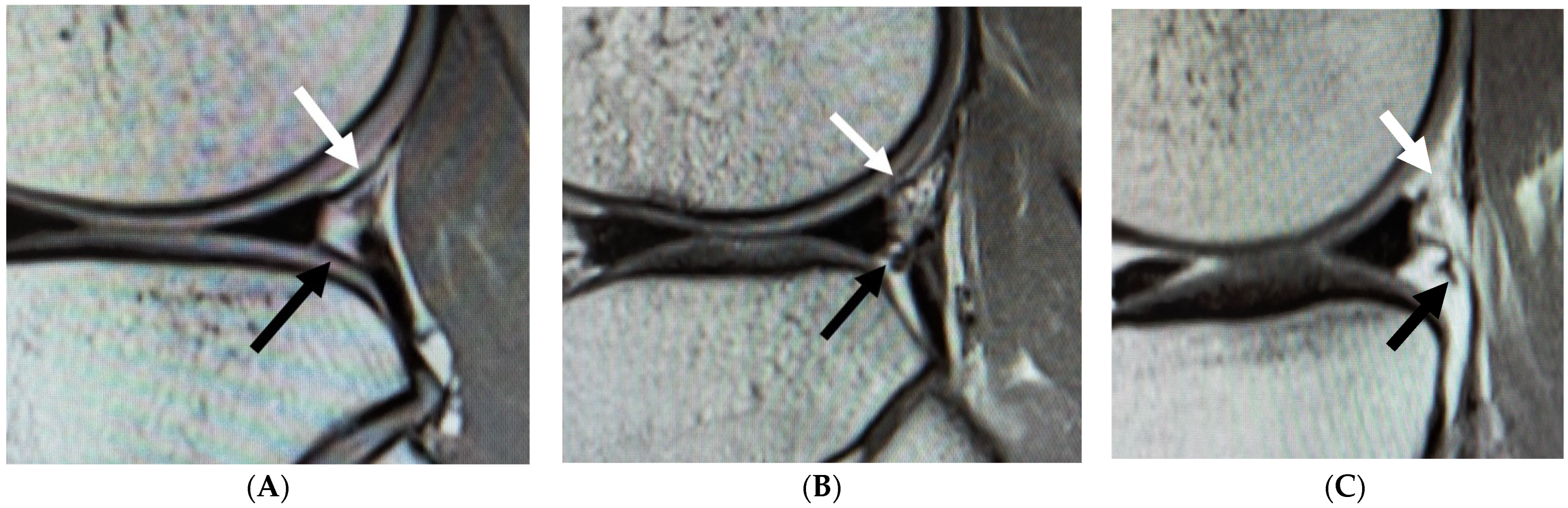
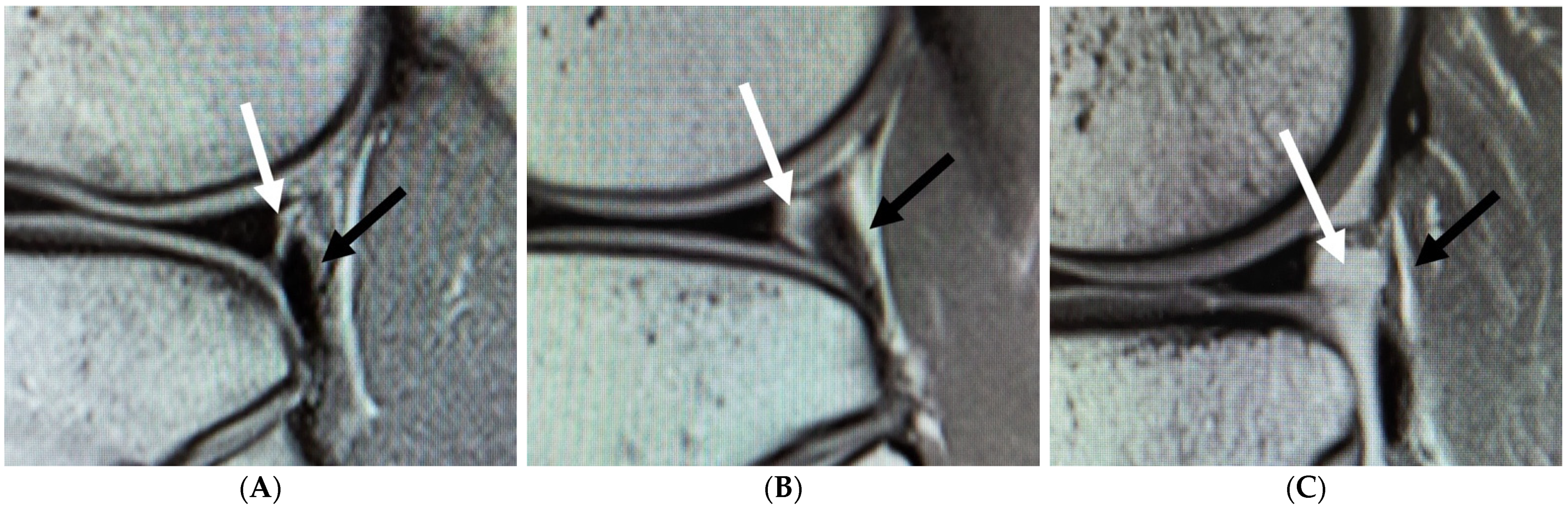
2.2. MRI Measurement
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zappia, M.; Reginelli, A.; Chianca, V.; Carfora, M.; Di Pietto, F.; Iannella, G.; Mariani, P.P.; Di Salvatore, M.; Bartollino, S.; Maggialetti, N.; et al. MRI of popliteo-meniscal fasciculi of the knee: A pictorial review. Acta Biomed. 2018, 89, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Steinbacher, G.; Alentorn-Geli, E.; Alvarado-Calderón, M.; Barastegui, D.; Álvarez-Díaz, P.; Cugat, R. Meniscal fixation is a successful treatment for hypermobile lateral meniscus in soccer players. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 354–360. [Google Scholar] [CrossRef]
- Kamiya, T.; Suzuki, T.; Otsubo, H.; Kuroda, M.; Matsumura, T.; Kubota, C.; Yamashita, T. Midterm outcomes after arthroscopic surgery for hypermobile lateral meniscus in adults: Restriction of paradoxical motion. J. Orthop. Sci. 2018, 23, 1000–1004. [Google Scholar] [CrossRef]
- Ohtoshi, K.; Kimura, M.; Kobayashi, Y.; Higuchi, H.; Kikuchi, S. Arthroscopic thermal shrinkage for hypermobile lateral meniscus. Am. J. Sports Med. 2004, 32, 1297–1301. [Google Scholar] [CrossRef]
- Van Steyn, M.O.; Mariscalco, M.W.; Pedroza, A.D.; Smerek, J.; Kaeding, C.C.; Flanigan, D.C. The hypermobile lateral meniscus: A retrospective review of presentation, imaging, treatment, and results. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1555–1559. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.H.; Lee, S.H.; Kim, K.I.; Nam, J. Arthroscopic meniscus repair for recurrent subluxation of the lateral meniscus. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 787–792. [Google Scholar] [CrossRef]
- Takahashi, T.; Kimura, M.; Takeshita, K. All-Inside Arthroscopic Meniscal Stacked Suture Repair for Hypermobile Lateral Meniscus with FASTFIX 360. Arthrosc. Tech. 2021, 10, e1757–e1761. [Google Scholar] [CrossRef]
- George, M.; Wall, E.J. Locked knee caused by meniscal subluxation: Magnetic resonance imaging and arthroscopic verification. Arthroscopy 2003, 19, 885–888. [Google Scholar] [CrossRef]
- Park, J.H.; Ro, K.H.; Lee, D.H. Snapping knee caused by a popliteomeniscal fascicle tear of the lateral meniscus in a professional Taekwondo athlete. Orthopedics 2012, 35, e1104–e1107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suganuma, J.; Mochizuki, R.; Inoue, Y.; Yamabe, E.; Ueda, Y.; Kanauchi, T. Magnetic resonance imaging and arthroscopic findings of the popliteomeniscal fascicles with and without recurrent subluxation of the lateral meniscus. Arthroscopy 2012, 28, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Zhao, H.; Dai, Z.; Chen, Z.; Liao, Y.; Fu, D.; Lei, Y.; Luo, T.; Liu, Q. Widening of the popliteal hiatus on magnetic resonance imaging leads to recurrent subluxation of the lateral meniscus. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3532–3538. [Google Scholar] [CrossRef]
- Aman, Z.S.; DePhillipo, N.N.; Storaci, H.W.; Moatshe, G.; Chahla, J.; Engebretsen, L.; LaPrade, R.F. Quantitative and Qualitative Assessment of Posterolateral Meniscal Anatomy: Defining the Popliteal Hiatus, Popliteomeniscal Fascicles, and the Lateral Meniscotibial Ligament. Am. J. Sports Med. 2019, 47, 1797–1803. [Google Scholar] [CrossRef]
- Shin, H.K.; Lee, H.S.; Lee, Y.K.; Bae, K.C.; Cho, C.H.; Lee, K.J. Popliteomeniscal fascicle tear: Diagnosis and operative technique. Arthrosc. Tech. 2012, 1, e101–e106. [Google Scholar] [CrossRef]
- Zheng, J.; Xiao, Q.; Wu, Q.; Deng, H.; Zhai, W.; Lin, D. Tears of the Popliteomeniscal Fascicles of the Lateral Meniscus: An Arthroscopic Classification. Cartilage 2020, 2020, 1947603520980156. [Google Scholar] [CrossRef]
- Singh, K.; Helms, C.A.; Jacobs, M.T.; Higgins, L.D. MRI appearance of Wrisberg variant of discoid lateral meniscus. AJR Am. J. Roentgenol. 2006, 187, 384–387. [Google Scholar] [CrossRef] [PubMed]
- Nair, R.; Dubey, N. MR Imaging of the Hypermobile Lateral Meniscus of the Knee: A Case Report. Acta Med. Acad. 2019, 48, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Peduzzi, P.; Concato, J.; Feinstein, A.R.; Holford, T.R. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J. Clin. Epidemiol. 1995, 48, 1503–1510. [Google Scholar] [CrossRef]
- Jose, J.; Buller, L.T.; Rivera, S.; Carvajal Alba, J.A.; Baraga, M. Wrisberg-variant discoid lateral meniscus: Current concepts, treatment options, and imaging features with emphasis on dynamic ultrasonography. Am. J. Orthop. 2015, 44, 135–139. [Google Scholar] [PubMed]
- Marchand, A.J.; Proisy, M.; Ropars, M.; Cohen, M.; Duvauferrier, R.; Guillin, R. Snapping knee: Imaging findings with an emphasis on dynamic sonography. AJR Am. J. Roentgenol. 2012, 199, 142–150. [Google Scholar] [CrossRef]
- Peduto, A.J.; Nguyen, A.; Trudell, D.J.; Resnick, D.L. Popliteomeniscal Fascicles: Anatomic Considerations Using MR Arthrography in Cadavers. AJR Am. J. Roentgenol. 2008, 190, 442–448. [Google Scholar] [CrossRef]
- Kalke, R.J.; Di Primio, G.A.; Schweitzer, M.E. MR and CT arthrography of the knee. Semin. Musculoskelet. Radiol. 2012, 16, 57–68. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Sasho, T.; Wada, Y.; Sano, S.; Iwasaki, J.; Morita, F.; Moriya, H. MRI of the popliteomeniscal fasciculi. AJR Am. J. Roentgenol. 2006, 186, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Choi, Y.J.; Park, H.J.; Kook, S.H.; Kang, K.A.; Kim, M.S.; Kwon, H.J.; Ahn, J.H. Types of posterolateral corner injury associated with both bundle and selective-bundle ACL tears. Acta Radiol. 2019, 2019, 284185119842833. [Google Scholar] [CrossRef]
- Guimaraes, J.B.; Facchetti, L.; Schwaiger, B.J.; Gersing, A.S.; Li, X.; Link, T.M. Natural evolution of popliteomeniscal fascicle tears over 2 years and its association with lateral articular knee cartilage degeneration in patients with traumatic anterior cruciate ligament tear. Eur. Radiol. 2018, 28, 3542–3549. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Hypermobile Meniscus Group (H Group) | Control Group (C Group) | |
|---|---|---|
| n | 22 | 44 |
| Mean age | 31.5 | 30.1 |
| Male:female | 10:12 | 20:24 |
| Operative procedure | Lateral meniscus suture: 22 | Anterior cruciate reconstruction: 28 |
| Medial patellar femoral ligament reconstruction: 8 | ||
| Medial meniscal suture: 4 | ||
| Ganglion resection: 2 | ||
| Plica resection: 2 | ||
| sPMF | Type 1: 10 | Type 1: 33 |
| Type 2: 7 | Type 2: 8 | |
| Type 3: 5 | Type 3: 3 | |
| iPMF | Type 1: 3 | Type 1: 22 |
| Type 2: 9 | Type 2: 16 | |
| Type 3: 10 | Type 3: 6 | |
| The widening of the popliteal hiatus | Type 1: 5 | Type 1: 25 |
| Type 2: 11 | Type 2: 13 | |
| Type 3: 6 | Type 3: 6 |
| Odds Ratio | 95% CI (Lower Limit) | 95% CI (Upper Limit) | p Value | |
|---|---|---|---|---|
| Intercept | 0.303 | 0.149 | 0.615 | 0.001 |
| Type 1 (reference) | ||||
| Type 2 | 2.890 | 0.838 | 0.950 | 0.093 |
| Type 3 | 5.500 | 1.110 | 27.200 | 0.036 |
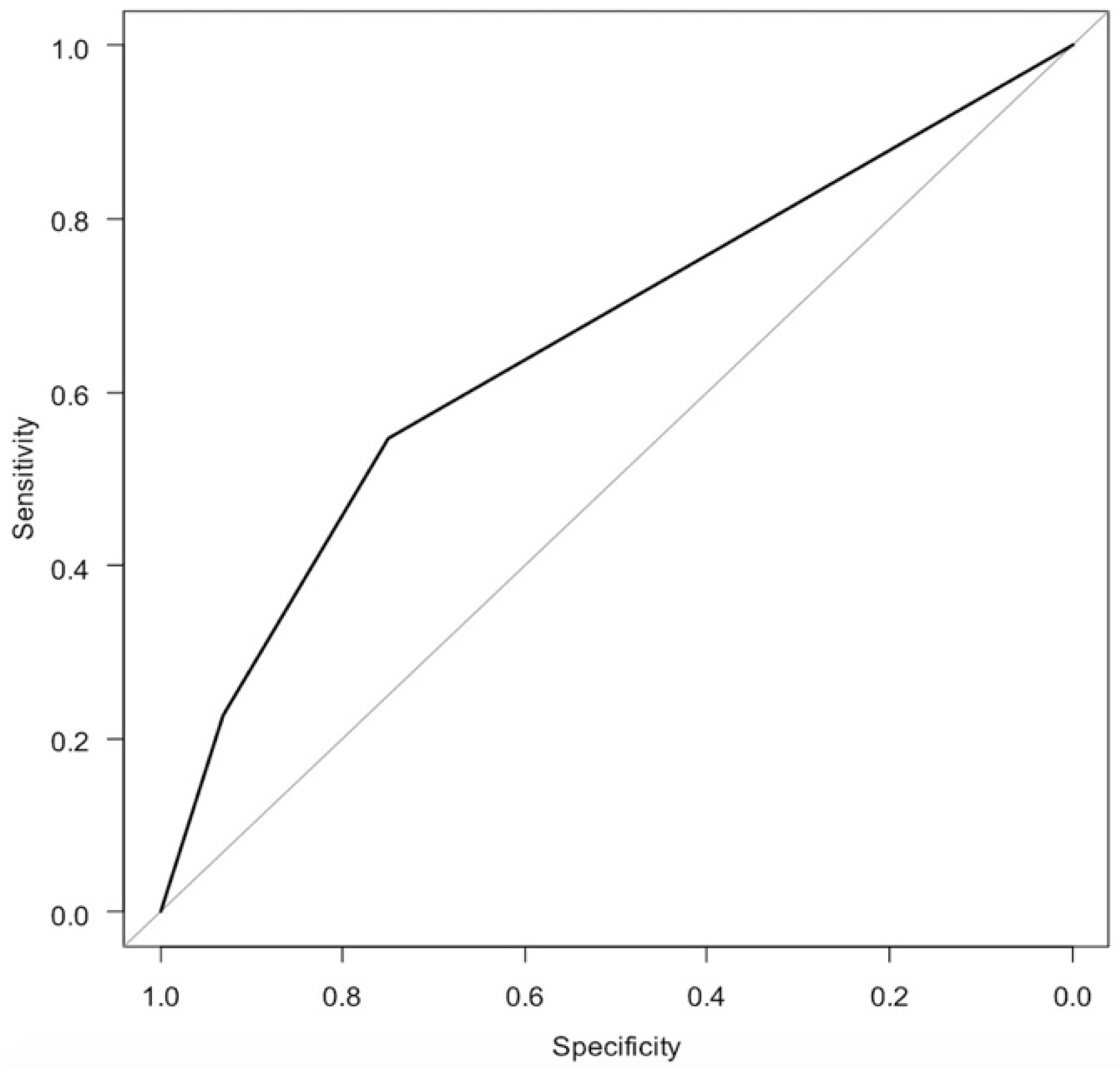
| AUC | 95% CI (lower limit) | 95% CI (upper limit) | ||
| 0.658 | 0.529 | 0.786 | ||
| Odds Ratio | 95% CI (Lower Limit) | 95% CI (Upper Limit) | p Value | |
|---|---|---|---|---|
| Intercept | 0.136 | 0.041 | 0.456 | 0.001 |
| Type 1 (reference) | ||||
| Type 2 | 4.120 | 0.961 | 17.700 | 0.057 |
| Type 3 | 12.200 | 2.530 | 59.000 | 0.002 |
| AUC | 95% CI (lower limit) | 95% CI (upper limit) | ||
| 0.737 | 0.617 | 0.856 | ||
| Odds Ratio | 95% CI (Lower Limit) | 95% CI (Upper Limit) | p Value | |
|---|---|---|---|---|
| Intercept | 0.200 | 0.077 | 0.522 | 0.001 |
| Type 1 (reference) | ||||
| Type 2 | 4.230 | 1.210 | 14.800 | 0.024 |
| Type 3 | 5.000 | 1.130 | 22.100 | 0.034 |
| AUC | 95% CI (lower limit) | 95% CI (upper limit) | ||
| 0.659 | 0.522 | 0.796 | ||
| Odds Ratio | 95% CI (Lower Limit) | 95% CI (Upper Limit) | p Value | |
|---|---|---|---|---|
| Intercept | 0.110 | 0.030 | 0.406 | 0.001 |
| sPMF Type 1 (reference) | ||||
| sPMF Type 2 | 2.900 | 0.570 | 14.800 | 0.199 |
| sPMF Type 3 | 6.980 | 1.040 | 46.900 | 0.046 |
| iPMF Type 1 (reference) | ||||
| iPMF Type 2 | 1.130 | 0.242 | 5.240 | 0.881 |
| iPMF Type 3 | 1.530 | 0.233 | 10.000 | 0.659 |
| Widening of popliteal hiatus Type 1 (reference) | ||||
| Widening of popliteal hiatus Type 2 | 2.070 | 0.461 | 9.300 | 0.343 |
| Widening of popliteal hiatus Type 3 | 1.910 | 0.344 | 10.700 | 0.459 |
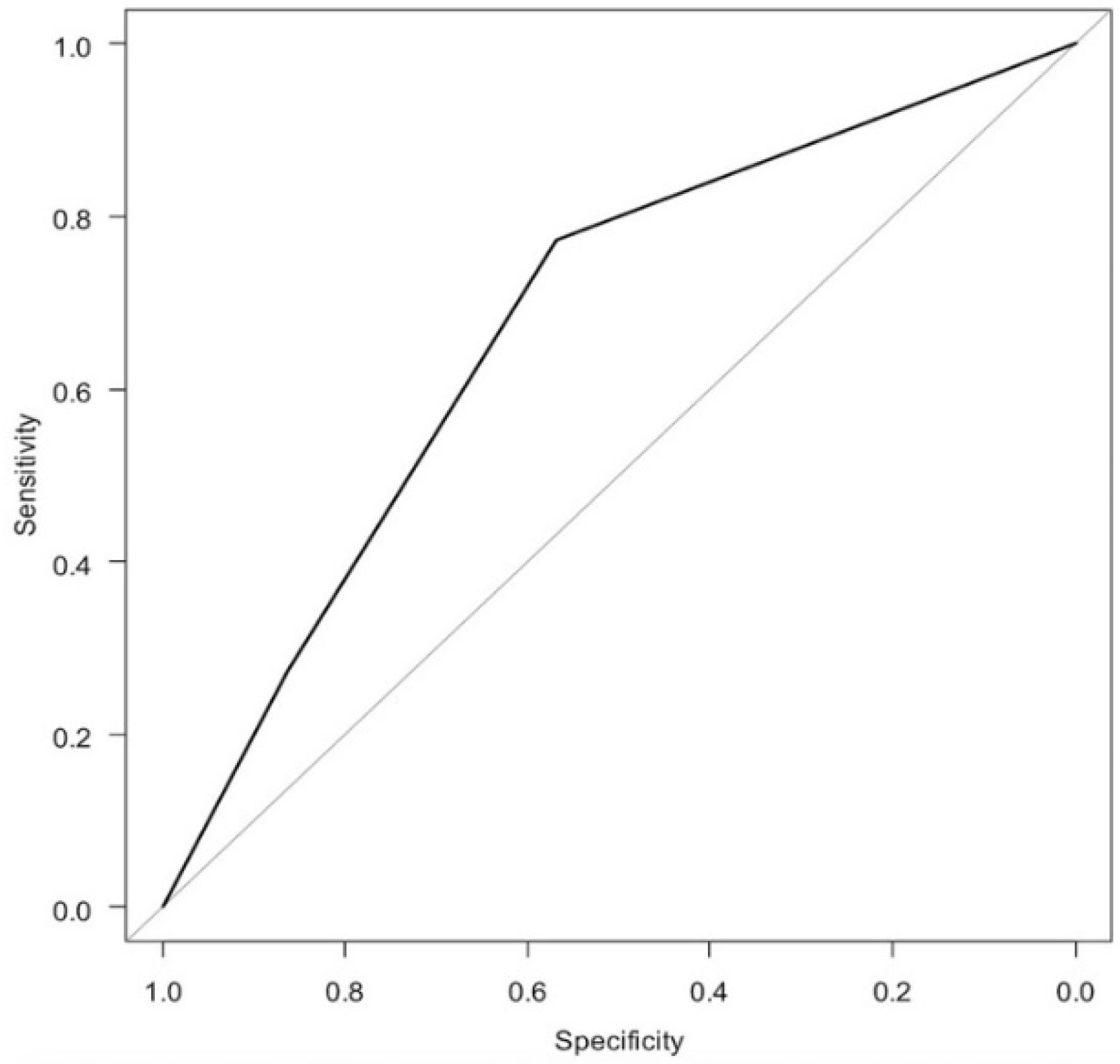
| AUC | 95% CI (lower limit) | 95% CI (upper limit) | ||
| 0.765 | 0.644 | 0.887 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toyooka, S.; Shimazaki, N.; Masuda, H.; Arai, N.; Miyamoto, W.; Ando, S.; Kawano, H.; Nakagawa, T. Preoperative Magnetic Resonance Imaging as a Diagnostic Aid for Hypermobile Lateral Meniscus. Diagnostics 2021, 11, 2276. https://doi.org/10.3390/diagnostics11122276
Toyooka S, Shimazaki N, Masuda H, Arai N, Miyamoto W, Ando S, Kawano H, Nakagawa T. Preoperative Magnetic Resonance Imaging as a Diagnostic Aid for Hypermobile Lateral Meniscus. Diagnostics. 2021; 11(12):2276. https://doi.org/10.3390/diagnostics11122276
Chicago/Turabian StyleToyooka, Seikai, Naoya Shimazaki, Hironari Masuda, Noriaki Arai, Wataru Miyamoto, Shuji Ando, Hirotaka Kawano, and Takumi Nakagawa. 2021. "Preoperative Magnetic Resonance Imaging as a Diagnostic Aid for Hypermobile Lateral Meniscus" Diagnostics 11, no. 12: 2276. https://doi.org/10.3390/diagnostics11122276
APA StyleToyooka, S., Shimazaki, N., Masuda, H., Arai, N., Miyamoto, W., Ando, S., Kawano, H., & Nakagawa, T. (2021). Preoperative Magnetic Resonance Imaging as a Diagnostic Aid for Hypermobile Lateral Meniscus. Diagnostics, 11(12), 2276. https://doi.org/10.3390/diagnostics11122276






