Unraveling Variations in Celiac Trunk and Hepatic Artery by CT Angiography to Aid in Surgeries of Upper Abdominal Region
Abstract
1. Introduction
2. Material and Methods
2.1. CT Examination
2.2. Image Analysis
3. Results
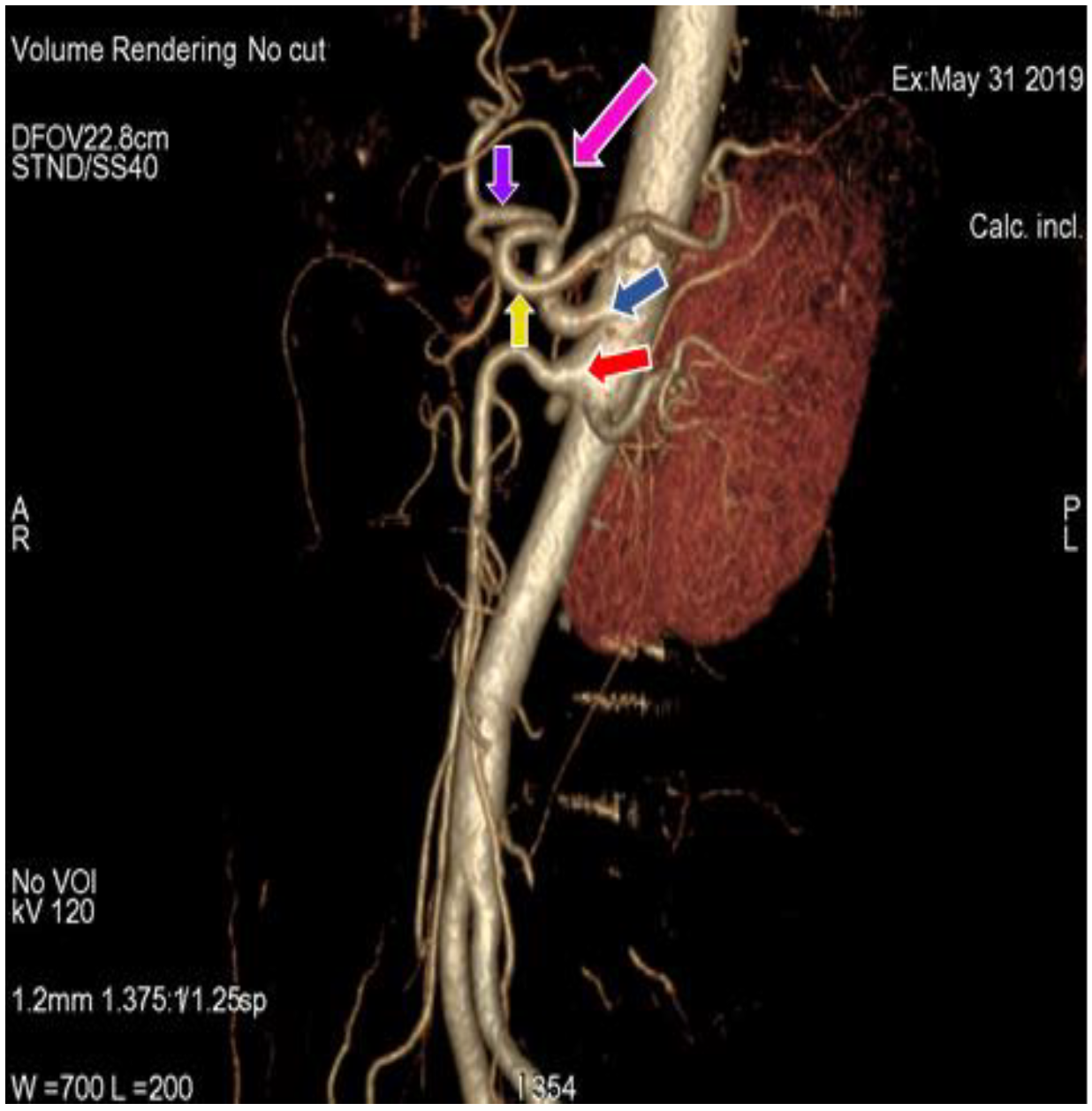
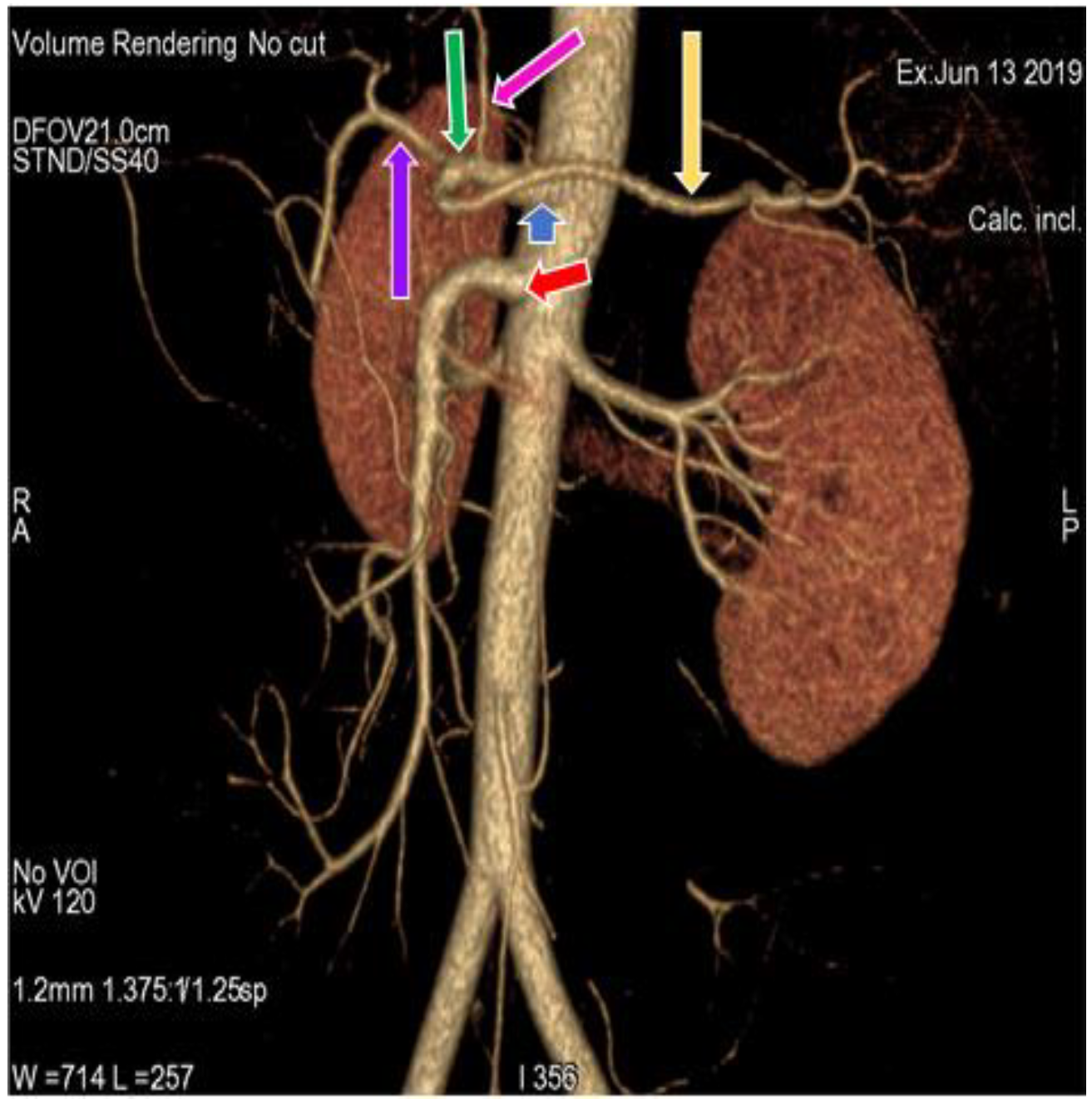
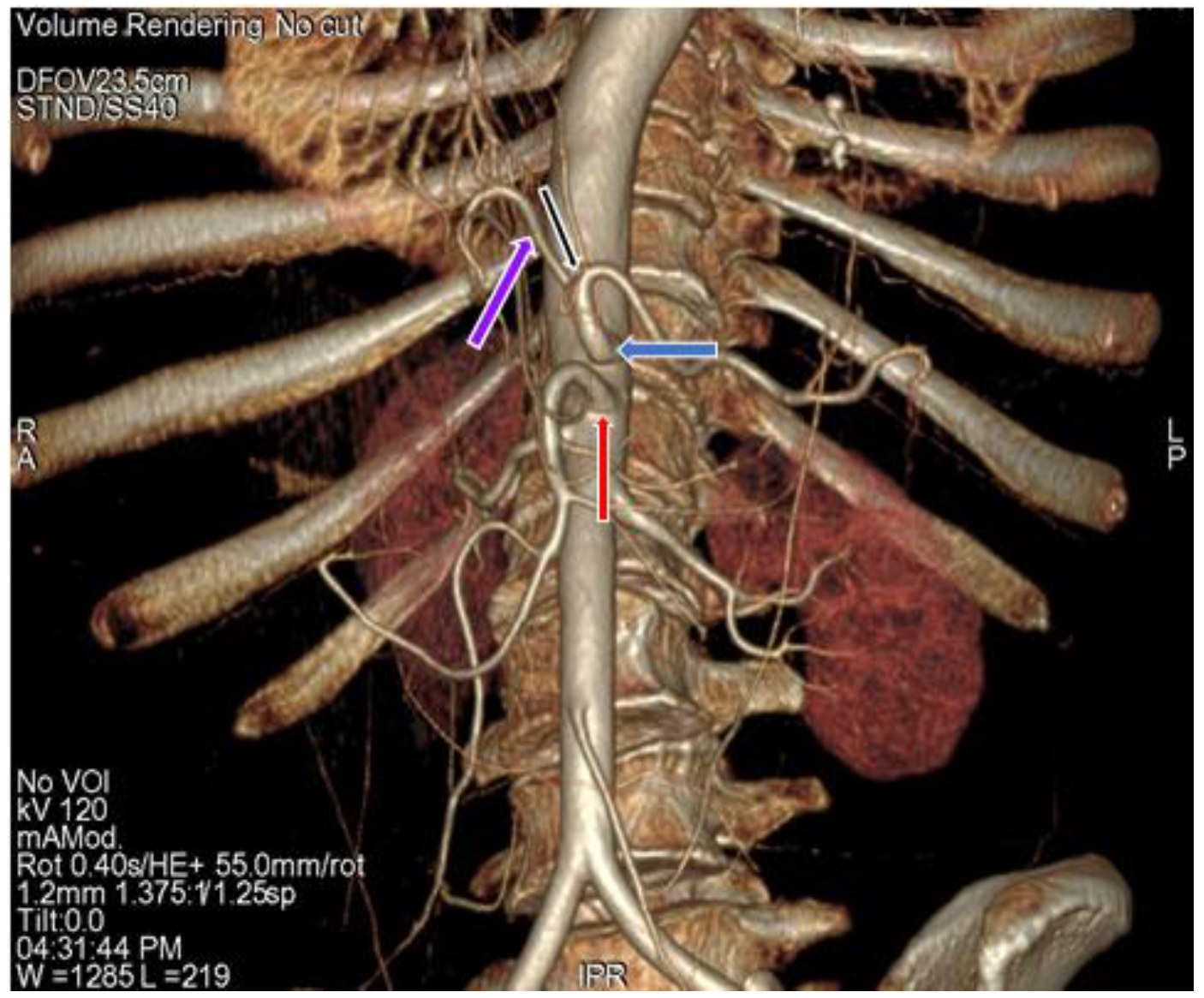
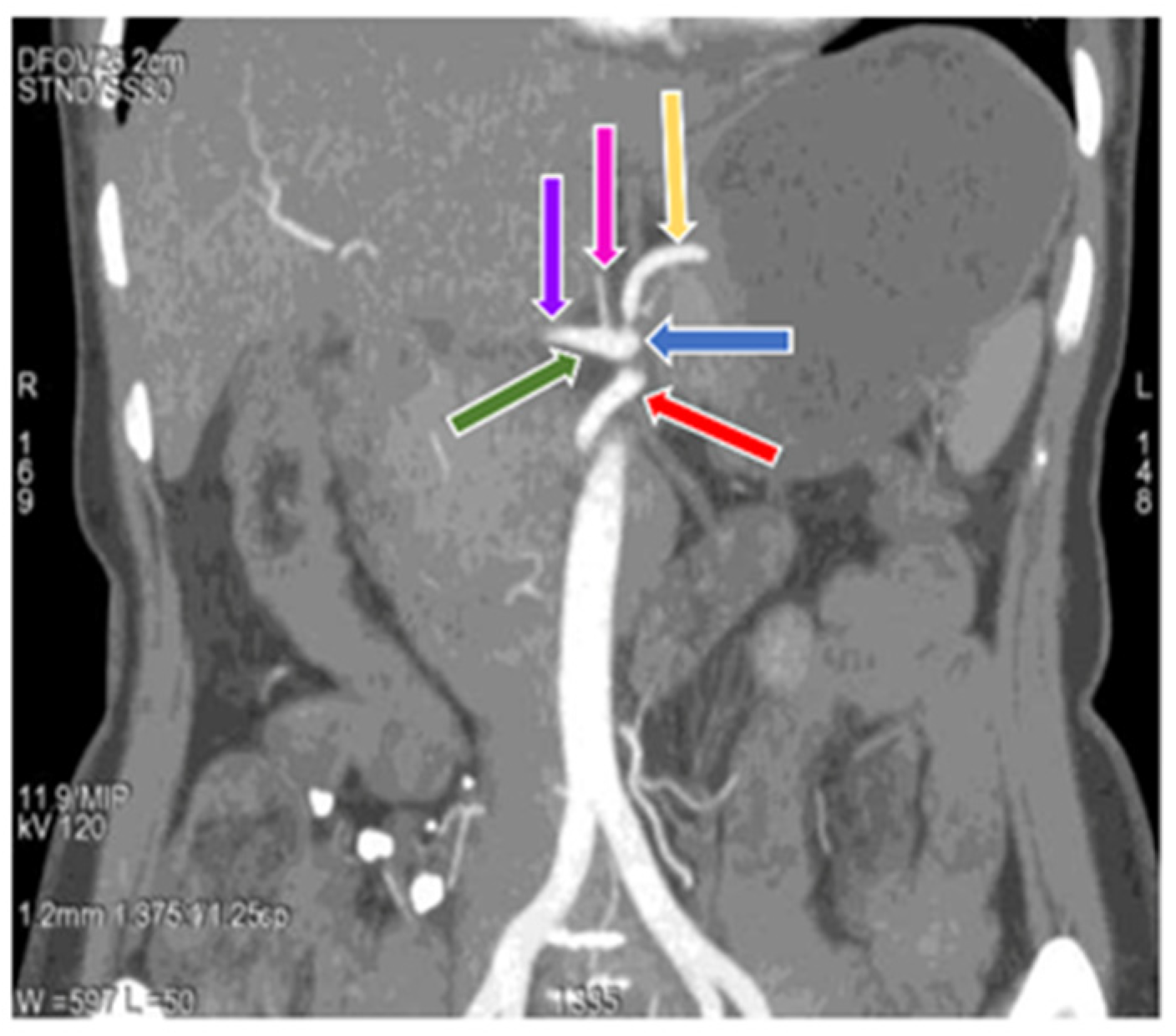
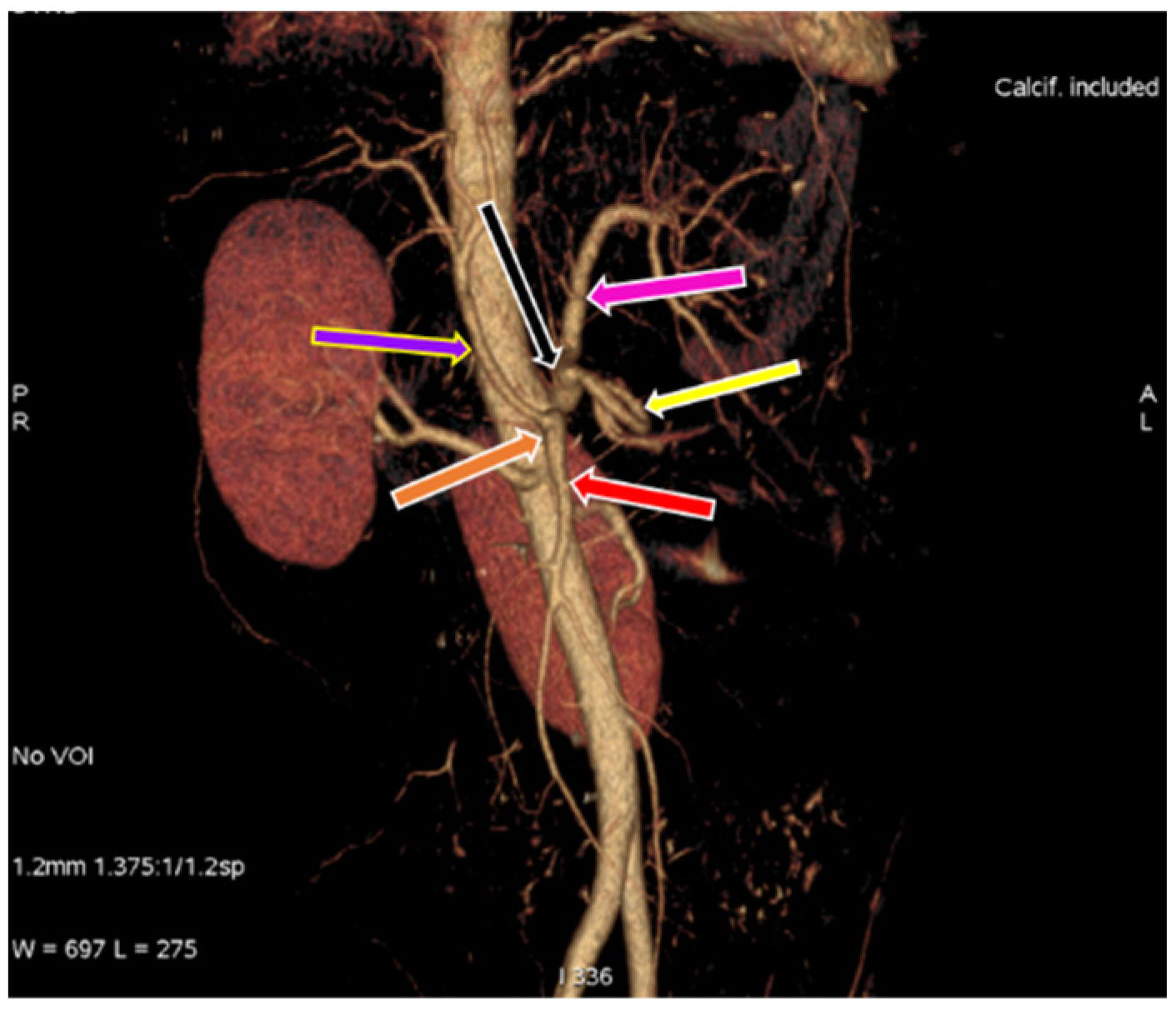
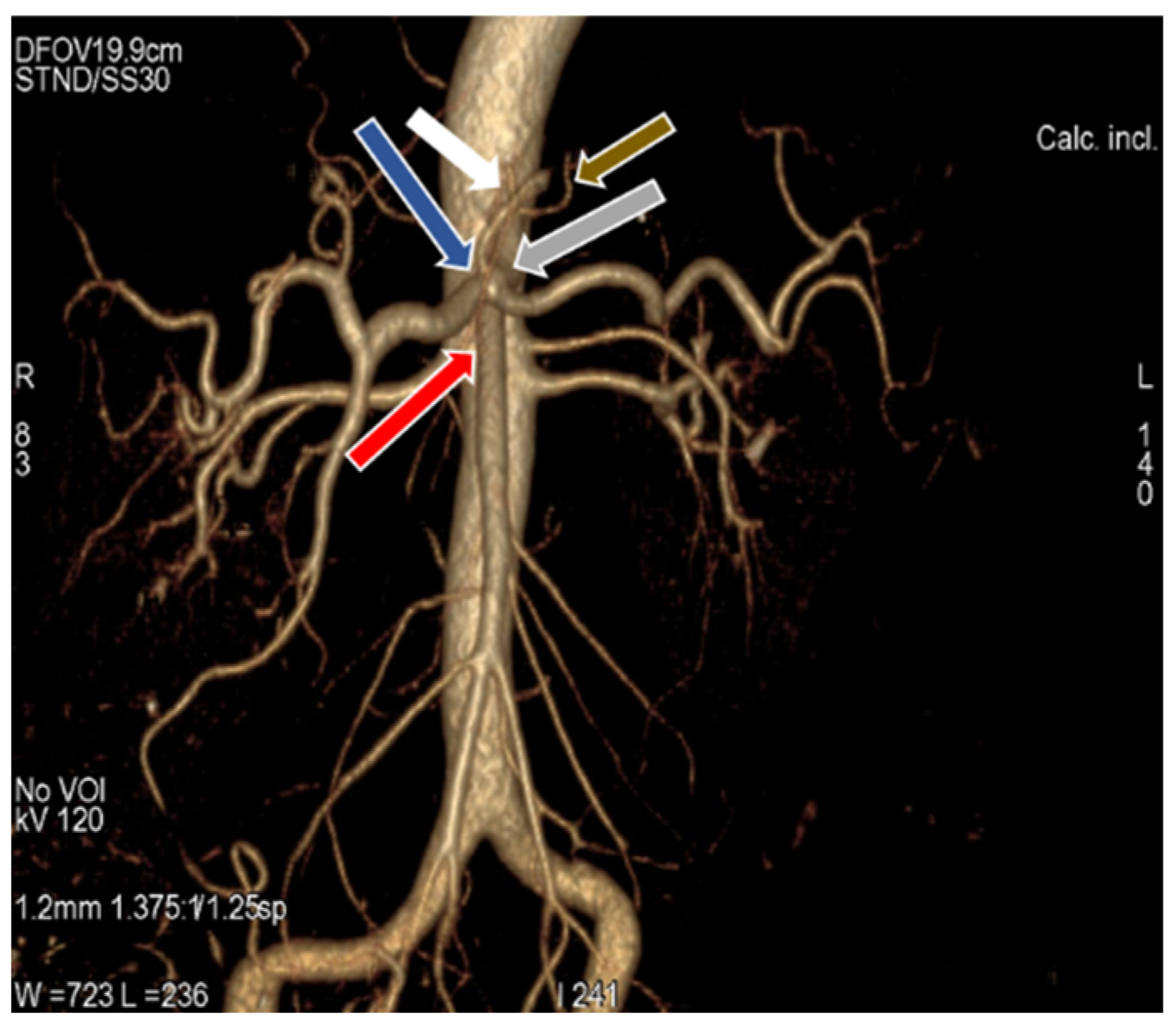
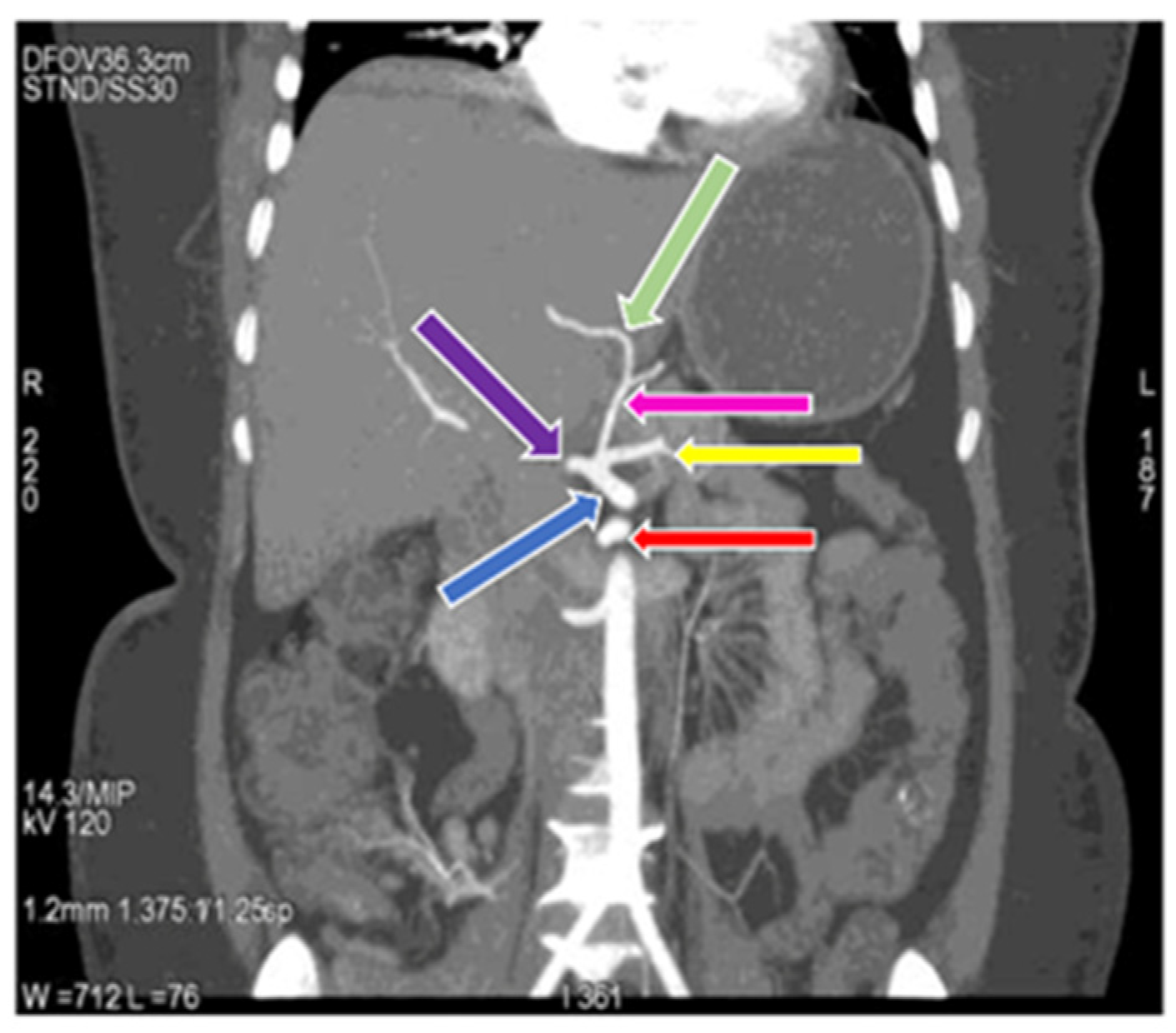
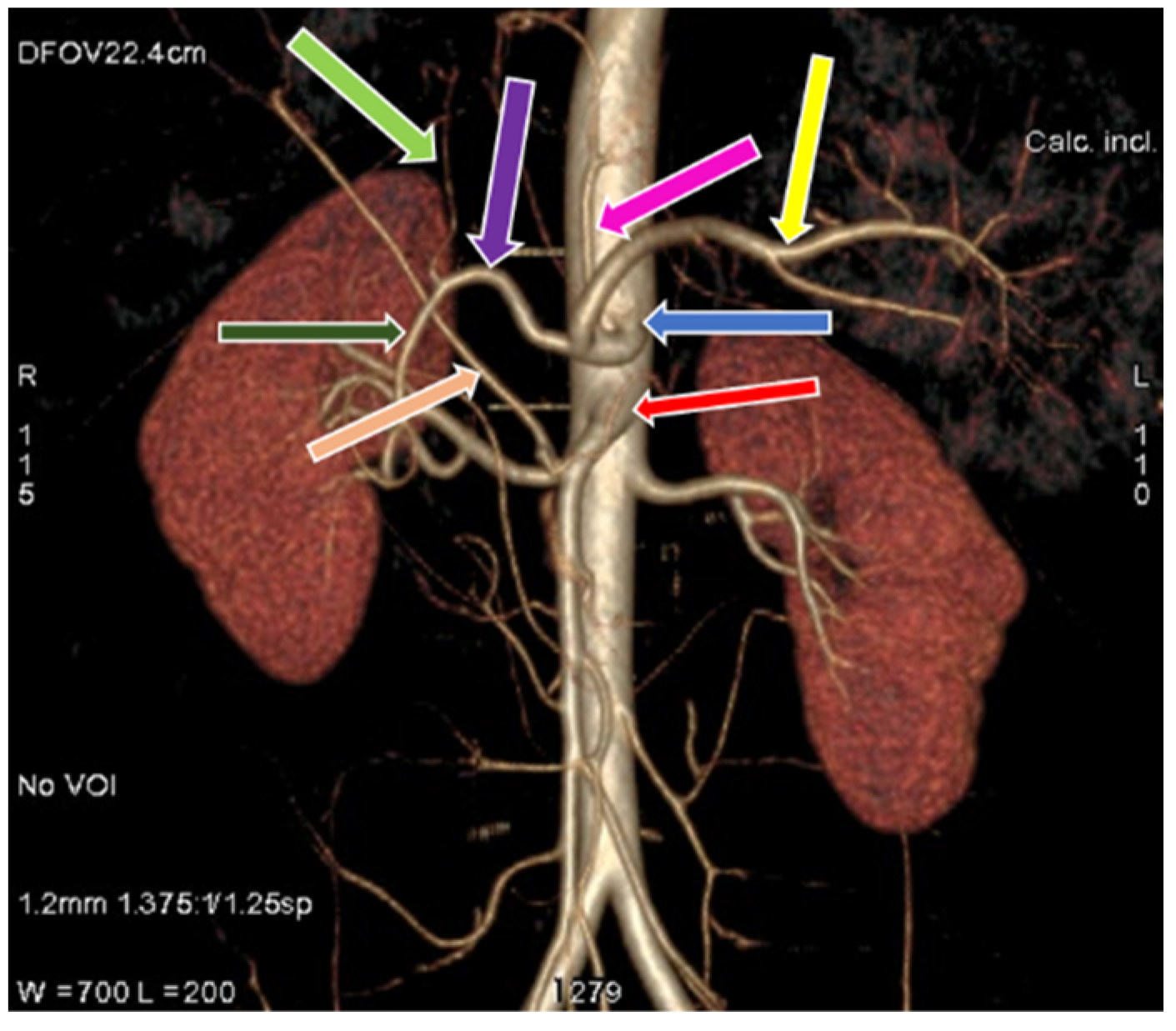
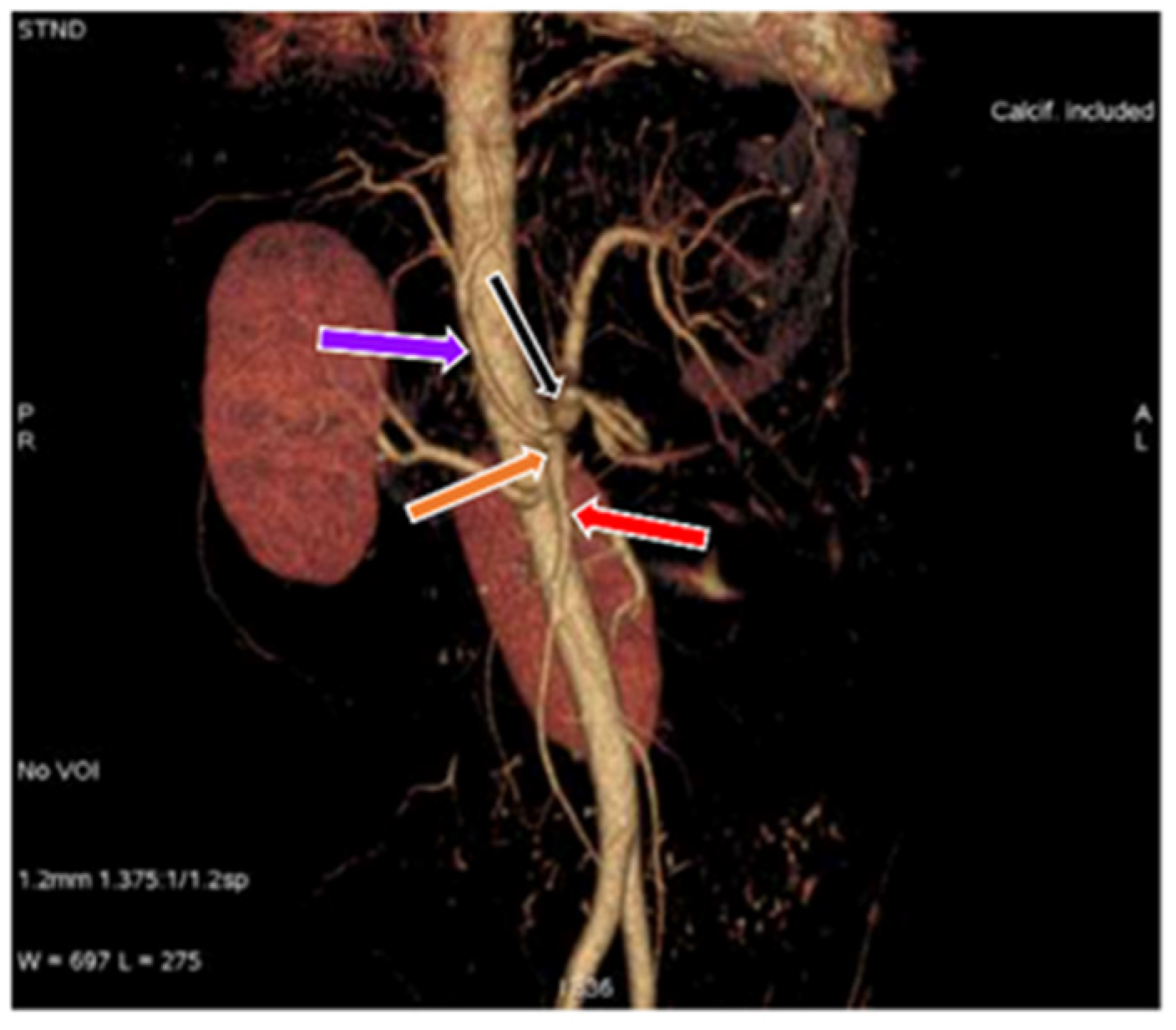
3.1. Variation in Origin and Branching Pattern of Celiac Trunk
3.2. Variation in Origin and Branching Pattern of Hepatic Artery
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Juszczak, A.; Czyżowski, J.; Mazurek, A.; Walocha, J.A.; Pasternak, A. Anatomical variants of coeliac trunk in Polish population using multidetector computed tomography angiography. Folia Morphol. 2021, 80, 290–296. [Google Scholar] [CrossRef]
- Juszczak, A.; Mazurek, A.; Walocha, J.A.; Pasternak, A. Coeliac trunk and its anatomic variations: A cadaveric study. Folia Morphol. 2021, 80, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Thangarajah, A.; Parthasarathy, R. Celiac axis, common hepatic and hepatic artery variants as evidenced on MDCT angiography in south indian population. J. Clin. Diagn. Res. JCDR 2016, 10, TC01–TC05. [Google Scholar] [CrossRef] [PubMed]
- Hogea, B.G.; Rusu, M.C.; Jianu, A.M.; Manta, B.A.; Ilie, A.C. Rare Anatomic Variation: The Hepatosplenomesentericophrenic Trunk. Medicina 2021, 57, 170. [Google Scholar] [CrossRef]
- Pinal-Garcia, D.F.; Nuno-Guzman, C.M.; Gonzalez-Gonzalez, M.E.; Ibarra-Hurtado, T.R. The celiac trunk and its anatomical variations: A cadaveric study. J. Clin. Med. Res. 2018, 10, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Bergman, R.A. Anatomy Atlases. 2008. Available online: www.anatomyatlases.org (accessed on 9 October 2021).
- Hiatt, J.R.; Gabbay, J.; Busuttil, R.W. Surgical anatomy of the hepatic arteries in 1000 cases. Ann. Surg. 1994, 220, 50–52. [Google Scholar] [CrossRef]
- Nelson, T.M.; Pollak, R.; Jonasson, O.; Abcarian, H. Anatomic variants of the celiac, superior mesenteric, and inferior mesenteric arteries and their clinical relevance. Clin. Anat. 1988, 1, 75–91. [Google Scholar] [CrossRef]
- Wacker, F.; Lippert, H.; Pabst, R. Arterial Variations in Humans: Key Reference for Radiologists and Surgeons: Classification and Frequency; Lippert, H., Pabst, R., Wacker, F., Eds.; Thieme: Stuggart, AR, USA; New York, NY, USA, 2017. [Google Scholar]
- Eaton, P.B. The coeliac axis. Anat. Rec. 1917, 13, 369–374. [Google Scholar] [CrossRef]
- Tandler, J. On the varieties of the coeliacae and their development. Anat. Bookl. 1904, 25, 473–500. [Google Scholar]
- Lipshutz, B. A composite study of the coeliac axis artery. Ann. Surg. 1917, 65, 159–169. [Google Scholar] [CrossRef]
- Petrella, S.; de Sousa Rodriguez, C.F.; Sgrott, E.A.; Fernandes, G.J.M.; Marques, S.R.; Prates, J.C. Anatomy and Variations of the Celiac Trunk. Int. J. Morphol. 2007, 25, 249–257. [Google Scholar] [CrossRef]
- Iezzi, R.; Cotroneo, A.R.; Giancristofaro, D.; Santoro, M.; Storto, M.L. Multidetector-row CT angiographic imaging of the celiac trunk: Anatomy and normal variants. Surg. Radiol. Anat. 2008, 30, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Higashi, N.; Shimada, H.; Simamura, E.; Hatta, T. Branching patterns of the celiac artery as the hepato-gastro-splenic trunk. Kaibogaku Zasshi J. Anat. 2009, 84, 7–10. [Google Scholar]
- Mburu, K.S.; Alexander, O.O.J.; Hassan, S.; Bernard, N.U. Variations in the branching pattern of the celiac trunk in a Kenyan population. Int. J. Morphol. 2010, 28, 199–204. [Google Scholar] [CrossRef]
- Okada, S.; Ohta, Y.; Shimizu, T.; Nakamura, M.; Yaso, K. A Rare Anomalous Case of Absence of the Celiac Trunk-the Left Gastric, the Splenic and the Common Hepatic Arteries Arose from the Abdominal Aorta Independently. Okajimas Folia Anat. Jpn. 1983, 60, 65–71. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cavdar, S.; Gürbüz, J.; Zeybek, A.; Sehirli, U.; Abik, L.; Ozdogmuş, O. A variation of coeliac trunk. Kaibogaku Zasshi J. Anat. 1998, 73, 505–508. [Google Scholar]
- Kahraman, G.; Marur, T.; Tanyeli, E.; Yildirim, M. Hepatomesenteric trunk. Surg. Radiol. Anat. 2002, 23, 433–435. [Google Scholar] [CrossRef]
- Saeed, M.; Murshid, K.R.; Rufai, A.A.; Elsayed, S.E.; Sadiq, M.S. Coexistence of multiple anomalies in the celiac-mesenteric arterial system. Clin. Anat. 2003, 16, 30–36. [Google Scholar] [CrossRef]
- Çiçekcibaşi, A.E.; Uysal, İ.İ.; Şeker, M.; Tuncer, I.; Büyükmumcu, M.; Salbacak, A. A rare variation of the coeliac trunk. Ann. Anat. 2005, 187, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Karakose, M.; Peker, T.; Gulekon, N.; Yucel, D.; Oktem, H. Numerical variation of the celiac trunk and anatomical variation in origin and course of the dorsal pancreatic artery. Saudi Med. J. 2006, 27, 1232–1235. [Google Scholar]
- Katagiri, H.; Ichimura, K.; Sakai, T. A case of celiacomesenteric trunk with some other arterial anomalies in a Japanese woman. Anat. Sci. Int. 2007, 82, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Yi, S.Q.; Terayama, H.; Naito, M.; Hirai, S.; Alimujang, S.; Yi, N.; Tanaka, S.; Itoh, M. Absence of the celiac trunk: Case report and review of the literature. Clin. Anat. 2008, 21, 283–286. [Google Scholar] [CrossRef] [PubMed]
- Omar, R.; Kisansa, M.; Dehnavi, A.D. The prevalence of anatomical variants of the coeliac trunk and renal arteries on contrast-enhanced abdominal computed tomography scans at Dr George Mukhari Academic Hospital. SA J. Radiol. 2021, 25, 1990. [Google Scholar] [CrossRef] [PubMed]
- Munshi, I.A.; Fusco, D.; Tashjian, D.; Kirkwood, J.R.; Polga, J.; Wait, R.B. Occlusion of an aberrant right hepatic artery, originating from the superior mesenteric artery, secondary to blunt trauma. J. Trauma Acute Care Surg. 2000, 48, 325–326. [Google Scholar] [CrossRef][Green Version]
- Michels, N.A. Blood supply and anatomy of the upper abdominal organs: With a descriptive atlas. Lippincott 1955, 137, 153–154. [Google Scholar]
- Adachi, B. Das Arteriensystem der Japaner, 1st ed.; Verlag der Kaiserlich Japanischen Universit: Kyoto, Japan, 1928. [Google Scholar]
- Morita, M. Reports and conception of three anomalous cases on the area of the celiac and superior mesenteric arteries. Igaku Kenkyu (Acta Med.) 1935, 9, 1993–2006. [Google Scholar]
- Tsukamoto, N. The branches of the abdominal visceral arteries in Japanese. Kaibogaku Zasshi 1929, 2, 780–829. [Google Scholar]
- Imakoshi, K. Study of the abdominal arterial supply. Achiev. Dep. Anat. Kanazawa Med. Univ. 1949, 37, 1–14. [Google Scholar]
- Kozhevnikova, N.T. Individual and developmental features of the structure of the human celiac trunk. Arkh Anat Histol. Embriol. 1977, 72, 19–24. [Google Scholar]
- Vandamme, J.P.J.; Bonte, J. The branches of the celiac trunk. Cells Tissues Organs 1985, 22, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Shoumura, S.; Emura, S.; Utsumi, M.; Chen, H.; Hayakawa, D.; Yamahira, T.; Isono, H. Anatomical study on the branches of the celiac trunk (IV). Comparison of the findings with Adachi’s classification. Kaibogaku Zasshi J. Anat. 1991, 66, 452–461. [Google Scholar]
- Aslaner, R.; Pekcevik, Y.; Sahin, H.; Toka, O. Variations in the origin of inferior phrenic arteries and their relationship to celiac axis variations on CT angiography. Korean J. Radiol. KJR 2017, 18, 336–344. [Google Scholar] [CrossRef]
- Ekingen, A.; Çetinçakmak, M.G. A comprehensive study of right and left inferior phrenic artery variations in 1000 patients with multidetector computed tomography angiography: An important study for HCC. Surg. Radiol. Anat. 2021, 43, 1471–1480. [Google Scholar] [CrossRef]
- Szewczyk, B.; Karauda, P.; Podgórski, M.; Waśniewska, A.; Haładaj, R.; Rapacka, E.; Oszukowski, P.; Polguj, M. Types of inferior phrenic arteries: A new point of view based on a cadaveric study. Folia Morphol. 2021, 80, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Noussios, G.; Dimitriou, I.; Chatzis, I.; Katsourakis, A. The main anatomic variations of the hepatic artery and their importance in surgical practice: Review of the literature. J. Clin. Med. Res. 2017, 9, 248–252. [Google Scholar] [CrossRef]
- Cirocchi, R.; D’Andrea, V.; Amato, B.; Renzi, C.; Henry, B.M.; Tomaszewski, K.A.; Gioia, S.; Lancia, M.; Artico, M.; Randolph, J. Aberrant left hepatic arteries arising from left gastric arteries and their clinical importance. Surgeon 2020, 18, 100–112. [Google Scholar] [CrossRef]
- Michels, N.A. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am. J. Surg. 1966, 112, 337–347. [Google Scholar] [CrossRef]
- Suzuki, T.; Nakayasu, A.; Kawabe, K.; Takeda, H.; Honjo, I. Surgical significance of anatomic variations of the hepatic artery. Am. J. Surg. 1971, 122, 505–512. [Google Scholar] [CrossRef]
- Mäkisalo, H.; Chaib, E.; Krokos, N.; Calne, R. Hepatic arterial variations and liver-related diseases of 100 consecutive donors. Transpl. Int. 1993, 6, 325–329. [Google Scholar] [CrossRef]
- Noah, E.M.; Klinzing, S.; Zwaan, M.; Schramm, U.; Bruch, H.P.; Weiss, H.D. Normal variation of arterial liver supply in mesenterico-celiacography. Ann. Anat. 1995, 177, 305–312. [Google Scholar] [CrossRef]
- Soin, A.S.; Friend, P.J.; Rasmussen, A.; Saxena, R.; Tokat, Y.; Alexander, G.J.M.; Jamieson, N.V.; Calne, R.Y. Donor arterial variations in liver transplantation: Management and outcome of 527 consecutive grafts. Br. J. Surg. 1996, 83, 637–641. [Google Scholar] [CrossRef]
- Gruttadauria, S.; Scotti Foglieni, C.; Doria, C.; Luca, A.; Lauro, A.; Marino, I.R. The hepatic artery in liver transplantation and surgery: Vascular anomalies in 701 cases. Clin. Transplant. 2001, 15, 359–363. [Google Scholar] [CrossRef]
- Varotti, G.; Gondolesi, G.E.; Goldman, J.; Wayne, M.; Florman, S.S.; Schwartz, M.E.; Miller, C.M.; Sukru, E. Anatomic variations in right liver living donors. J. Am. Coll. Surg. 2004, 198, 577–582. [Google Scholar] [CrossRef]
- Koops, A.; Wojciechowski, B.; Broering, D.C.; Adam, G.; Krupski-Berdien, G. Anatomic variations of the hepatic arteries in 604 selective celiac and superior mesenteric angiographies. Surg. Radiol. Anat. 2004, 26, 239–244. [Google Scholar] [CrossRef]
- Chen, H.; Yano, R.; Emura, S.; Shoumura, S. Anatomic variation of the celiac trunk with special reference to hepatic artery patterns. Ann. Anat. 2009, 191, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Sebben, G.A.; Rocha, S.L.; Sebben, M.A.; Parussolo Filho, P.R.; Gonçalves, B.H.H. Variations of hepatic artery: Anatomical study on cadavers. Rev. Col. Bras. Cir. 2013, 40, 221–226. [Google Scholar] [CrossRef]
- Sureka, B.; Mittal, M.K.; Mittal, A.; Sinha, M.; Bhambri, N.K.; Thukral, B.B. Variations of celiac axis, common hepatic artery and its branches in 600 patients. Indian J. Radiol. Imaging 2013, 23, 223. [Google Scholar] [CrossRef]
- Venieratos, D.; Panagouli, E.; Lolis, E.; Tsaraklis, A.; Skandalakis, P. A morphometric study of the celiac trunk and review of the literature. Clin. Anat. 2013, 26, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Jin, W.; Dong, M.; Pan, J.; Zhang, Q.; Li, M.; Guo, D.; Gao, Y.; Lv, Z.; Tan, T.; Ma, J. Rare combined variations of accessory left hepatic artery and accessory right hepatic artery: A case report and literature review. Surg. Radiol. Anat. 2020, 42, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Whitley, A.; Oliverius, M.; Kocián, P.; Havlůj, L.; Gürlich, R.; Kachlík, D. Variations of the celiac trunk investigated by multidetector computed tomography: Systematic review and meta-analysis with clinical correlations. Clin. Anat. 2020, 33, 1249–1262. [Google Scholar] [CrossRef] [PubMed]
- Gore, R.M.; Levine, M.S. Diseases of the upper GI tract. In Diseases of the Abdomen and Pelvis 2018–2021; Hodler, J., Kubik-Huch, R.A., von Schulthess, G.K., Eds.; IDKD Springer Series; Springer: New York, NY, USA, 2018. [Google Scholar]
- Cankal, F.; Kaya, M.; Guner, M.A. Evaluation of Celiac Trunk, Hepatic Artery Variations, and Their Collateral Arteries by Multi-Slice Computed Tomography. Sisli. Etfal. Hastan. Tip. Bul. 2021, 55, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Otsubo, T.; Koizumi, S.; Ariizumi, S.; Katagiri, S.; Watanabe, T.; Nakano, H.; Yamamoto, M. Anatomic variations of hepatic artery and new clinical classification based on abdominal angiographic images of 1200 cases. Hepato-Gastroenterology 2014, 61, 2337–2340. [Google Scholar]
- Brasil, I.R.C.; Araujo, I.F.D.; Lima, A.A.L.D.A.; Melo, E.L.A.; Esmeraldo, R.D.M. Computed tomography angiography study of variations of the celiac trunk and hepatic artery in 100 patients. Radiol. Bras. 2018, 51, 32–36. [Google Scholar] [CrossRef]
- Sankar, K.D.; Bhanu, P.S.; Susan, P.J. Variant anatomy of the celiac trunk and its branches. Int. J. Morphol. 2011, 29, 581–584. [Google Scholar] [CrossRef]
- Panagouli, E.; Venieratos, D.; Lolis, E.; Skandalakis, P. Variations in the anatomy of the celiac trunk: A systematic review and clinical implications. Ann. Anat. 2013, 195, 501–511. [Google Scholar] [CrossRef] [PubMed]
- Song, S.Y.; Chung, J.W.; Yin, Y.H.; Jae, H.J.; Kim, H.C.; Jeon, U.B.; Cho, B.H.; So, Y.H.; Park, J.H. Celiac axis and common hepatic artery variations in 5002 patients: Systematic analysis with spiral CT and DSA. Radiology 2010, 255, 278–288. [Google Scholar] [CrossRef]
- Araujo, S.A.; Franca, H.A.; Mello, C.F.D.; Silva, E.J.; Negromonte, G.R.P.; Duarte, C.M.A.; Cavalcanti, B.F.; Farias, R.D.D.F. Anatomical variations of the celiac trunk and hepatic arterial system: An analysis using multidetector computed tomography angiography. Radiol. Bras. 2015, 48, 358–362. [Google Scholar] [CrossRef]
- Ugurel, M.S.; Battal, B.; Bozlar, U.; Nural, M.S.; Tasar, M.; Ors, F.; Saglam, M.; Karademir, I. Anatomical variations of hepatic arterial system, coeliac trunk and renal arteries: An analysis with multidetector CT angiography. Br. J. Radiol. 2010, 83, 661–667. [Google Scholar] [CrossRef]
- Çavdar, S.; Şehirli, Ü.; Pekin, B. Celiacomesenteric trunk. Clin. Anat. 1997, 10, 231–234. [Google Scholar] [CrossRef]
- Yi, S.Q.; Terayama, H.; Naito, M.; Hayashi, S.; Moriyama, H.; Tsuchida, A.; Itoh, M. A common celiacomesenteric trunk, and a brief review of the literature. Ann. Anat. 2007, 189, 482–488. [Google Scholar] [CrossRef]
- Tang, W.; Shi, J.; Kuang, L.Q.; Tang, S.Y.; Wang, Y. Celiomesenteric trunk: New classification based on multidetector computed tomography angiographic findings and probable embryological mechanisms. World J. Clin. Cases 2019, 7, 3980. [Google Scholar] [CrossRef] [PubMed]
- León, R.A.E.; Aguirre, G.B.; Coronado, V.T.; Sánchez, D.A.; Nava, M.C.I.; Zamudio, M.D.; Mendizabal, J.A.; José, J.; De Anda, M.; Pineda-Martinez, D. Variations of the celiac trunk in Mexican population by MDCT angiography. Eur. J. Anat. 2021, 25, 57–64. [Google Scholar]
- Basile, A.; Tsetis, D.; Montineri, A.; Puleo, S.; Saluzzo, C.M.; Runza, G.; Coppolino, F.; Ettorre, G.C.; Patti, M.T. MDCT anatomic assessment of right inferior phrenic artery origin related to potential supply to hepatocellular carcinoma and its embolization. Cardiovasc Intervent. Radiol. 2008, 31, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Loukas, M.; Hullett, J.; Wagner, T. Clinical anatomy of the inferior phrenic artery. Clin. Anat. 2005, 18, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Piao, D.X.; Ohtsuka, A.; Murakami, T. Typology of abdominal arteries, with special reference to inferior phrenic arteries and their esophageal branches. Acta Med. Okayama 1998, 52, 189–196. [Google Scholar]
- Pulakunta, T.; Potu, B.K.; Gorantla, V.R.; Rao, M.S.; Madhyastha, S.; Vollala, V.R. The origin of the inferior phrenic artery: A study in 32 South Indian cadavers with a review of the literature. J. Vasc. Bras. 2007, 6, 225–230. [Google Scholar] [CrossRef]
- Akhilandeswari, B.; Ranganath, P. Variations in the source of origin of inferior phrenic artery: A cadaveric study. J. Anat. Soc. India 2013, 62, 6–9. [Google Scholar] [CrossRef]
- Zagyapan, R.; Kurkcuoglu, A.; Bayraktar, A.; Pelin, C.; Aytekin, C. Anatomic variations of the celiac trunk and hepatic arterial system with digital subtraction angiography. Turk. J. Gastroenterol. 2014, 25, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Freitas, A.C.T.D.; Coelho, J.C.U.; Matias, J.E.F.; Zeni Neto, C.; Martins, E.L.; Druszcz, C.C. Anatomia arterial hepática: Estudo em 150 transplantes hepáticos. Rev. Col. Bras. Cir. 2001, 28, 13–16. [Google Scholar] [CrossRef]
- Mugunthan, N.; Kannan, R.; Jebakani, C.F.; Anbalagan, J. Variations in the origin and course of right hepatic artery and its surgical significance. J. Clin. Diagn. Res. 2016, 10, AC01–AC04. [Google Scholar] [CrossRef]
| Anatomical Pattern of Celiac Trunk | Female Cases (66) | Male Cases (44) | Total Number of Cases |
|---|---|---|---|
| Regular celiac trunk | 20 (30.3%) | 14 (31.82%) | 34 (30.9%) |
| Hepatosplenic trunk and Left gastric artery | 39 (59.1%) | 27 (61.4%) | 66 (60%) |
| Gastrosplenic trunk and Common hepatic artery | 4 (6.1%) | 1 (2.3%) | 5 (4.55%) |
| Heapto-gastric trunk and splenic artery | 1 (1.52%) | 1 (2.3%) | 2 (1.82%) |
| Gastrosplenic and Hepato-mesentric trunk | 1 (1.52%) | 1 (2.3%) | 2 (1.82%) |
| Celiacomesentric trunk | 1 (1.52%) | 0 (0%) | 1 (0.91%) |
| Anatomical Variation of Hepatic Artery | Total Number of Cases (110) | Total Female Cases (66) | Total Male Cases (44) | Michels Classification | Hiatts Classification |
|---|---|---|---|---|---|
| Regular anatomy | 102 (92.72%) | 61 (92.43%) | 41 (93.18%) | Type I | Type I |
| LHA branch LGA | 2 (1.82%) | 2 (3.03%) | 0 (0%) | Type II | Type II |
| RHA branch SMA | 4 (3.64%) | 2 (3.03%) | 2 (4.54%) | Type III | Type III |
| Type I and II association | 0 | 0 | 0 | Type IV | Type IV |
| LHA accessory LGA | 0 | 0 | 0 | Type V | Type II |
| RHA accessory SMA | 0 | 0 | 0 | Type VI | Type III |
| LHA accessory LGA + RHA accessory SMA | 0 | 0 | 0 | Type VII | Type IV |
| LHA accessory LGA + RHA branch SMA | 0 | 0 | 0 | Type VIII | Type IV |
| CHA branch SMA | 2 (1.82%) | 1 (1.52%) | 1 (2.3%) | Type IX | Type V |
| RHA and LHA branch LGA | 0 | 0 | 0 | Type X | - |
| CHA aorta branch | 0 | 0 | 0 | - | Type VI |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malviya, K.K.; Verma, A.; Nayak, A.K.; Mishra, A.; More, R.S. Unraveling Variations in Celiac Trunk and Hepatic Artery by CT Angiography to Aid in Surgeries of Upper Abdominal Region. Diagnostics 2021, 11, 2262. https://doi.org/10.3390/diagnostics11122262
Malviya KK, Verma A, Nayak AK, Mishra A, More RS. Unraveling Variations in Celiac Trunk and Hepatic Artery by CT Angiography to Aid in Surgeries of Upper Abdominal Region. Diagnostics. 2021; 11(12):2262. https://doi.org/10.3390/diagnostics11122262
Chicago/Turabian StyleMalviya, Kapil Kumar, Ashish Verma, Amit Kumar Nayak, Anand Mishra, and Raghunath Shahaji More. 2021. "Unraveling Variations in Celiac Trunk and Hepatic Artery by CT Angiography to Aid in Surgeries of Upper Abdominal Region" Diagnostics 11, no. 12: 2262. https://doi.org/10.3390/diagnostics11122262
APA StyleMalviya, K. K., Verma, A., Nayak, A. K., Mishra, A., & More, R. S. (2021). Unraveling Variations in Celiac Trunk and Hepatic Artery by CT Angiography to Aid in Surgeries of Upper Abdominal Region. Diagnostics, 11(12), 2262. https://doi.org/10.3390/diagnostics11122262






