Symptomatic Intraosseous Lipoma of the Calcaneum
Abstract
:1. Introduction
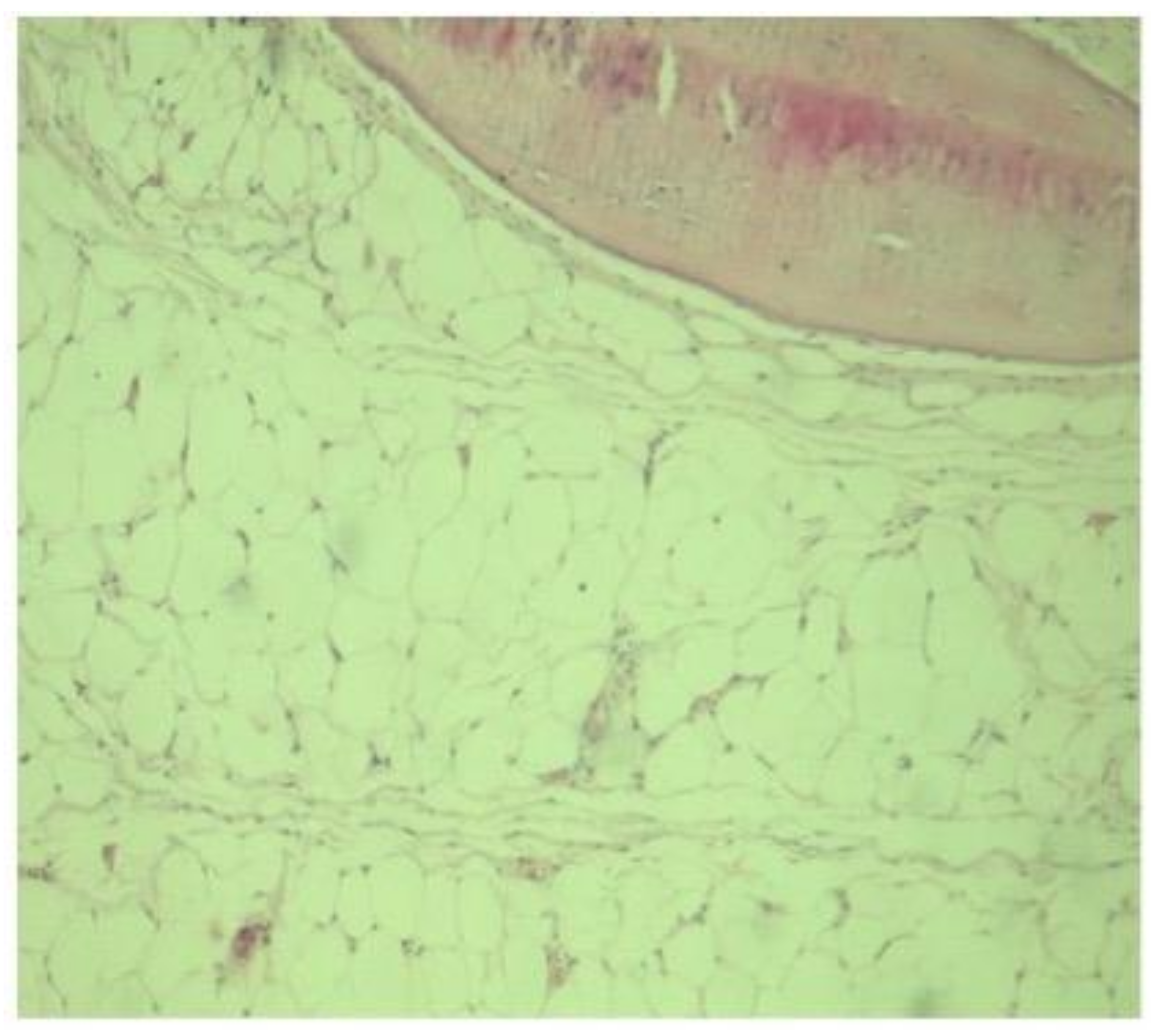
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Poussa, M.; Holmström, T. Intraosseous lipoma of the calcaneus. Report of a case and a short review of the literature. Acta Orthop. Scand. 1976, 47, 570–574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pappas, A.J.; Haffner, K.E.; Mendicino, S.S. An intraosseous lipoma of the calcaneus: A case report. J. Foot Ankle Surg. 2014, 53, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Milgram, J.W. Intraosseous lipomas: Radiologic and pathologic manifestations. Radiology 1988, 167, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Picci, P. Epidemiology. In Atlas of Musculoskeletal Tumors and Tumorlike Lesions; Picci, P., Manfrini, M., Fabbri, N., Gambarotti, M., Vanel, D., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2014; pp. 3–8. [Google Scholar] [CrossRef]
- Ulucay, C.; Altintas, F.; Ozkan, N.K.; Inan, M.; Ugutmen, E. Surgical treatment for calcaneal intraosseous lipomas. Foot 2009, 19, 93–97. [Google Scholar] [CrossRef]
- Murphey, M.D.; Carroll, J.F.; Flemming, D.J.; Pope, T.L.; Gannon, F.H.; Kransdorf, M.J. Benign musculoskeletal lipomatous lesions. Radiographics 2004, 24, 1433–1466. [Google Scholar] [CrossRef]
- Kang, H.S.; Kim, T.; Oh, S.; Park, S.; Chung, S.H. Intraosseous lipoma: 18 years of experience at a single institution. CiOS Clin. Orthop. Surg. 2018, 10, 234–239. [Google Scholar] [CrossRef]
- Campbell, R.S.D.; Grainger, A.J.; Mangham, D.C.; Beggs, I.; Teh, J.; Davies, A.M. Intraosseous lipoma: Report of 35 new cases and a review of the literature. Skeletal. Radiol. 2003, 32, 209–222. [Google Scholar] [CrossRef]
- Caranci, F.; Cirillo, M.; Piccolo, D.; Briganti, G.; Cicala, D.; Leone, G. A rare case of intraosseous lipoma involving the sphenoclival region. Neuroradiol. J. 2012, 25, 680–683. [Google Scholar] [CrossRef]
- Levin, M.F.; Vellet, A.D.; Munk, P.L.; McLean, C.A. Intraosseous lipoma of the distal femur: MRI appearance. Skeletal. Radiol. 1996, 25, 82–84. [Google Scholar] [CrossRef]
- Narang, S.; Gangopadhyay, M. Calcaneal intraosseous lipoma: A case report and review of the literature. J. Foot Ankle Surg. 2011, 50, 216–220. [Google Scholar] [CrossRef]
- Jung, H.G.; Carag, J.A.; Park, J.Y.; Bae, E.J.; Lim, S.D.; Kim, H.S. Osteochondroma of the calcaneus presenting as Haglund’s deformity. Foot Ankle Surg. 2011, 17, e20–e22. [Google Scholar] [CrossRef]
- Muramatsu, K.; Tominaga, Y.; Hashimoto, T.; Taguchi, T. Symptomatic Intraosseous Lipoma in the Calcaneus. Anticancer Res. 2014, 34, 963–966. [Google Scholar]
- Bruni, L. The “cockade” image: A diagnostic sign of calcaneum intraosseous lipoma. Rays 1987, 11, 51–54. [Google Scholar]
- Bagatur, A.E.; Yalcinkaya, M.; Dogan, A.; Gur, S.; Mumcuoglu, E.; Albayrak, M. Surgery is not always necessary in intraosseous lipoma. Orthopedics 2010, 33, 306. [Google Scholar] [CrossRef]
- Frangež, I.; Nizič-Kos, T.; Cimerman, M. Threatening Fracture of Intraosseous Lipoma Treated by Internal Fixation Case Report and Review of the Literature. J. Am. Podiatr. Med. Assoc. 2019, 109, 75–79. [Google Scholar] [CrossRef]
- Cao, Y. Internal fixation combined with bone grafting for large intraosseous calcaneal lipoma: A case report. Mol. Clin. Oncol. 2017, 7, 877–879. [Google Scholar] [CrossRef] [Green Version]
- Mawardi, M.; Hussin, P. Intraosseous lipoma of the calcaneum: A rare cause of heel pain. Malays. Fam. Physician 2019, 13, 38–39. [Google Scholar]
- Propeck, T.; Bullard, M.; Lin, J.; Doi, K.; Martel, W. Radiologic-pathologic correlation of intraosseous lipomas. AJR Am. J. Roentgenol. 2000, 175, 673–678. [Google Scholar] [CrossRef]
- De Vita, A.; Mercatali, L.; Recine, F.; Pieri, F.; Riva, N.; Bongiovanni, A.; Liverani, C.; Spadazzi, C.; Miserocchi, G.; Amadori, D.; et al. Current classification, treatment options, and new perspectives in the management of adipocytic sarcomas. Onco Targets Ther. 2016, 9, 6233–6246. [Google Scholar] [CrossRef] [Green Version]
- Greenspan, A.; Raiszadeh, K.; Riley, G.; Matthews, D. Intraosseous lipoma of the calcaneus. Foot Ankle Int. 1997, 18, 53–56. [Google Scholar] [CrossRef]
- Zheng, K.; Yu, X.; Hu, Y.; Wang, Z.; Wu, S.; Ye, Z. How to Fill the Cavity after Curettage of Giant Cell Tumors around the Knee? A Multicenter Analysis. Chin. Med. 2017, 130, 2541–2546. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khal, A.A.; Mihu, R.C.; Schiau, C.; Fetica, B.; Tomoaia, G.; Luna, M.V. Symptomatic Intraosseous Lipoma of the Calcaneum. Diagnostics 2021, 11, 2243. https://doi.org/10.3390/diagnostics11122243
Khal AA, Mihu RC, Schiau C, Fetica B, Tomoaia G, Luna MV. Symptomatic Intraosseous Lipoma of the Calcaneum. Diagnostics. 2021; 11(12):2243. https://doi.org/10.3390/diagnostics11122243
Chicago/Turabian StyleKhal, Adyb Adrian, Razvan Catalin Mihu, Calin Schiau, Bogdan Fetica, Gheorghe Tomoaia, and Manuel Vergillos Luna. 2021. "Symptomatic Intraosseous Lipoma of the Calcaneum" Diagnostics 11, no. 12: 2243. https://doi.org/10.3390/diagnostics11122243
APA StyleKhal, A. A., Mihu, R. C., Schiau, C., Fetica, B., Tomoaia, G., & Luna, M. V. (2021). Symptomatic Intraosseous Lipoma of the Calcaneum. Diagnostics, 11(12), 2243. https://doi.org/10.3390/diagnostics11122243






