Borderline Personality Disorder: Risk Factors and Early Detection
Abstract
:1. Introduction
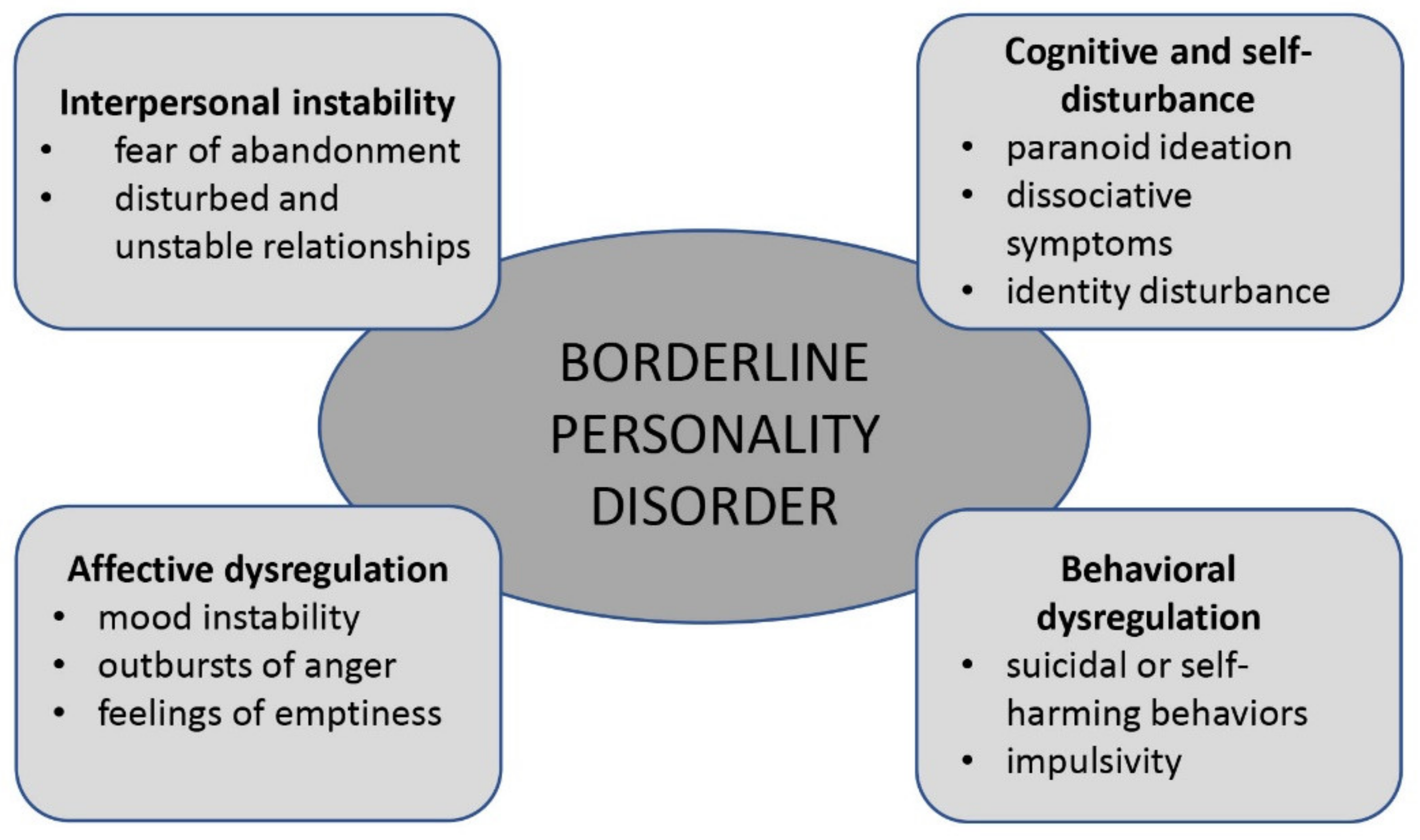
A pervasive pattern of instability in several areas (interpersonal relationships, self-image and affects) associated with marked impulsivity, which arises in adolescence or early adulthood and can be recognized in a variety of contexts, as indicated by five (or more) of the following criteria:
|
| Modified from DSM-5, APA, 2013 |
2. Materials and Methods
3. Results
4. Discussion
4.1. Risk Factors
4.1.1. Precocious Environmental Factors
Family-Related Factors
Trauma-Related Factors
4.1.2. Temperamental and Personality Factors
4.1.3. Genetic and Neurobiological Factors
4.2. Diagnosis of BPD
4.2.1. Diagnostic Criteria: DSM-5 and ICD-10
4.2.2. Clinical Assessment
4.2.3. Structured Diagnostic Interviews and Self-Report Questionnaires
4.2.4. Laboratory and Instrumental Assessment
4.2.5. Differential Diagnosis and Comorbidities
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; APA: Arlington, VA, USA, 2013. [Google Scholar]
- Stern, A. Psychoanalytic Investigation of and Therapy in the Border Line Group of Neuroses. Psychoanal. Q. 1938, 7, 467–489. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Endicott, J.; Gibbon, M. Crossing the Border into Borderline Personality and Borderline Schizophrenia. Arch. Gen. Psychiatry 1979, 36, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Tomko, R.; Trull, T.J.; Wood, P.K.; Sher, K.J. Characteristics of Borderline Personality Disorder in a Community Sample: Comorbidity, Treatment Utilization, and General Functioning. J. Pers. Disord. 2014, 28, 734–750. [Google Scholar] [CrossRef] [PubMed]
- Stepp, S.D.; Lazarus, S.A. Identifying a borderline personality disorder prodrome: Implications for community screening. Pers. Ment. Health 2017, 11, 195–205. [Google Scholar] [CrossRef]
- Miller, A.L.; Muehlenkamp, J.J.; Jacobson, C.M. Fact or fiction: Diagnosing borderline personality disorder in adolescents. Clin. Psychol. Rev. 2008, 28, 969–981. [Google Scholar] [CrossRef]
- Kaess, M.; Brunner, R.; Chanen, A. Borderline Personality Disorder in Adolescence. Pediatrics 2014, 134, 782–793. [Google Scholar] [CrossRef] [Green Version]
- Stepp, S.D.; Lazarus, S.A.; Byrd, A.L. A systematic review of risk factors prospectively associated with borderline personality disorder: Taking stock and moving forward. Pers. Disord. Theory. Res. Treat. 2016, 7, 316–323. [Google Scholar] [CrossRef]
- Johnson, J.G.; Cohen, P.; Kasen, S.; Skodol, A.E.; Oldham, J.M. Cumulative prevalence of personality disorders between adolescence and adulthood. Acta Psychiatr. Scand. 2008, 118, 410–413. [Google Scholar] [CrossRef]
- Coid, J.; Yang, M.; Tyrer, P.; Roberts, A.; Ullrich, S. Prevalence and correlates of personality disorder in Great Britain. Br. J. Psychiatry 2006, 188, 423–431. [Google Scholar] [CrossRef]
- Chanen, A.M.; McCutcheon, L.K. Personality disorder in adolescence: The diagnosis that dare not speak its name. Pers. Ment. Health 2008, 2, 35–41. [Google Scholar] [CrossRef]
- Oldham, J.M. Borderline Personality Disorder and Suicidality. Am. J. Psychiatry 2006, 163, 20–26. [Google Scholar] [CrossRef]
- Walter, M.; Gunderson, J.G.; Zanarini, M.C.; Sanislow, C.A.; Grilo, C.M.; McGlashan, T.H.; Morey, L.C.; Yen, S.; Stout, R.L.; Skodol, A.E. New onsets of substance use disorders in borderline personality disorder over 7 years of follow-ups: Findings from the Collaborative Longitudinal Personality Disorders Study. Addiction 2009, 104, 97–103. [Google Scholar] [CrossRef]
- Gunderson, J.G.; Stout, R.L.; McGlashan, T.H.; Shea, M.T.; Morey, L.C.; Grilo, C.M.; Zanarini, M.C.; Yen, S.; Markowitz, J.C.; Sanislow, C.; et al. Ten-Year Course of Borderline Personality Disorder. Arch. Gen. Psychiatry 2011, 68, 827–837. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Videler, A.C.; Hutsebaut, J.; Schulkens, J.E.M.; Sobczak, S.; Van Alphen, S.P.J. A Life Span Perspective on Borderline Personality Disorder. Curr. Psychiatry Rep. 2019, 21, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soeteman, M.S.D.I.; van Roijen, L.H.; Verheul, R.; Busschbach, J.J.V. The Economic Burden of Personality Disorders in Mental Health Care. J. Clin. Psychiatry 2008, 69, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Guilé, J.M.; Greenfield, B. Introduction personality disorders in childhood and adolescence. Can. Child Adolesc. Psychiatry Rev. 2004, 13, 51–52. [Google Scholar]
- Ha, C.; Balderas, J.C.; Zanarini, M.C.; Oldham, J.; Sharp, C. Psychiatric Comorbidity in Hospitalized Adolescents With Borderline Personality Disorder. J. Clin. Psychiatry 2014, 75, e457–e464. [Google Scholar] [CrossRef]
- Chanen, A.M.; Jovev, M.; Jackson, H.J. Adaptive Functioning and Psychiatric Symptoms in Adolescents with Borderline Personality Disorder. J. Clin. Psychiatry 2007, 68, 297–306. [Google Scholar] [CrossRef]
- Taylor, J.; James, L.M.; Reeves, M.D.; Kistner, J.A. Borderline Personality Traits are Associated with Poor Clinical and Psychosocial Functioning in Delinquent Boys. J. Psychopathol. Behav. Assess. 2009, 31, 94–103. [Google Scholar] [CrossRef]
- Zanarini, M.C.; Temes, C.M.; Frankenburg, F.R.; Reich, D.B.; Fitzmaurice, G.M. Description and prediction of time-to-attainment of excellent recovery for borderline patients followed prospectively for 20 years. Psychiatry Res. 2018, 262, 40–45. [Google Scholar] [CrossRef]
- Winsper, C.; Wolke, D.; Lereya, T. Prospective associations between prenatal adversities and borderline personality disorder at 11–12 years. Psychol. Med. 2015, 45, 1025–1037. [Google Scholar] [CrossRef] [PubMed]
- Bozzatello, P.; Bellino, S.; Bosia, M.; Rocca, P. Early Detection and Outcome in Borderline Personality Disorder. Front. Psychiatry 2019, 10, 710. [Google Scholar] [CrossRef] [PubMed]
- Westen, D.; Shedler, J.; Durrett, C.; Glass, S.; Martens, A. Personality Diagnoses in Adolescence: DSM-IV Axis II Diagnoses and an Empirically Derived Alternative. Am. J. Psychiatry 2003, 160, 952–966. [Google Scholar] [CrossRef] [PubMed]
- Sharp, C.; Tackett, J.L. Introduction: An Idea Whose Time Has Come. In Handbook of Borderline Personality Disorder in Children and Adolescents; Springer: New York, NY, USA, 2014; pp. 3–8. [Google Scholar] [CrossRef]
- Irwin, L.; Malhi, G.S. Borderline personality disorder and ICD-11: A chance for change. Aust. N. Z. J. Psychiatry 2019, 53, 698–700. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Borderline Personality Disorder: Treatment and Management; NICE: London, UK, 2009. [Google Scholar]
- National Health and Medical Research Council. Clinical Practice Guideline for the Management of Borderline Personality Disorder; National Health and Medical Research Council: Melbourne, VIC, Australia, 2012. [Google Scholar]
- Sharp, C. Bridging the gap: The assessment and treatment of adolescent personality disorder in routine clinical care. Arch. Dis. Child. 2017, 102, 103–108. [Google Scholar] [CrossRef]
- Fonagy, P.; Speranza, M.; Luyten, P.; Kaess, M.; Hessels, C.; Bohus, M. ESCAP Expert Article: Borderline personality disorder in adolescence: An expert research review with implications for clinical practice. Eur. Child Adolesc. Psychiatry 2015, 24, 1307–1320. [Google Scholar] [CrossRef] [Green Version]
- Beatson, J.A.; Broadbear, J.H.; Duncan, C.; Bourton, D.; Rao, S. Avoiding Misdiagnosis When Auditory Verbal Hallucinations Are Present in Borderline Personality Disorder. J. Nerv. Ment. Dis. 2019, 207, 1048–1055. [Google Scholar] [CrossRef]
- LeQuesne, E.R.; Hersh, R.G. Disclosure of a Diagnosis of Borderline Personality Disorder. J. Psychiatr. Pr. 2004, 10, 170–176. [Google Scholar] [CrossRef]
- Lawrence, K.A.; Allen, J.S.; Chanen, A. A Study of Maladaptive Schemas and Borderline Personality Disorder in Young People. Cogn. Ther. Res. 2011, 35, 30–39. [Google Scholar] [CrossRef]
- Fonagy, P.; Luyten, P. A Multilevel Perspective on the Development of Borderline Personality Disorder. In Developmental Psychopathology; Wiley & Sons: Hoboken, NJ, USA, 2019; Volume 29. [Google Scholar]
- Zanarini, M.C.; Frankenburg, F.R.; Khera, G.S.; Bleichmar, J. Treatment histories of borderline inpatients. Compr. Psychiatry 2001, 42, 144–150. [Google Scholar] [CrossRef]
- Clarkin, J.F.; Levy, K.N.; Lenzenweger, M.F.; Kernberg, O.F. The Personality Disorders Institute/Borderline Personality Disorder Research Foundation randomized control trial for borderline personality disorder: Rationale, methods, and patient characteristics. J. Pers. Disord. 2004, 18, 52–72. [Google Scholar] [CrossRef]
- Stepp, S.D.; Keenan, K.; Hipwell, A.E.; Krueger, R.F. The impact of childhood temperament on the development of borderline personality disorder symptoms over the course of adolescence. Borderline Pers. Disord. Emot. Dysregulation 2014, 1, 18. [Google Scholar] [CrossRef] [Green Version]
- Winsper, C.; Marwaha, S.; Lereya, S.T.; Thompson, A.; Eyden, J.; Singh, S.P. Clinical and psychosocial outcomes of borderline personality disorder in childhood and adolescence: A systematic review. Psychol. Med. 2015, 45, 2237–2251. [Google Scholar] [CrossRef] [PubMed]
- Distel, M.A.; Middeldorp, C.; Trull, T.J.; Derom, C.; Willemsen, G.; Boomsma, D.I. Life events and borderline personality features: The influence of gene–environment interaction and gene–environment correlation. Psychol. Med. 2011, 41, 849–860. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.; Chen, H.; Gordon, K.; Johnson, J.; Brook, J.; Kasen, S. Socioeconomic background and the developmental course of schizotypal and borderline personality disorder symptoms. Dev. Psychopathol. 2008, 20, 633–650. [Google Scholar] [CrossRef] [Green Version]
- Crawford, T.N.; Cohen, P.R.; Chen, H.; Anglin, D.M.; Ehrensaft, M. Early maternal separation and the trajectory of borderline personality disorder symptoms. Dev. Psychopathol. 2009, 21, 1013–1030. [Google Scholar] [CrossRef] [Green Version]
- Stepp, S.D.; Scott, L.N.; Jones, N.P.; Whalen, D.J.; Hipwell, A.E. Negative emotional reactivity as a marker of vulnerability in the development of borderline personality disorder symptoms. Dev. Psychopathol. 2015, 28, 213–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stepp, S.D.; Whalen, D.J.; Scott, L.N.; Zalewski, M.; Loeber, R.; Hipwell, A.E. Reciprocal effects of parenting and borderline personality disorder symptoms in adolescent girls. Dev. Psychopathol. 2014, 26, 361–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ibrahim, J.; Cosgrave, N.; Woolgar, M. Childhood maltreatment and its link to borderline personality disorder features in children: A systematic review approach. Clin. Child Psychol. Psychiatry 2018, 23, 57–76. [Google Scholar] [CrossRef] [Green Version]
- Boucher, M.; Pugliese, J.; Allard-Chapais, C.; Lecours, S.; Ahoundova, L.; Chouinard, R.; Gaham, S. Parent-child relationship associated with the development of borderline personality disorder: A systematic review. Pers. Ment. Health 2017, 11, 229–255. [Google Scholar] [CrossRef]
- Keinänen, M.T.; Johnson, J.G.; Richards, E.S.; Courtney, E.A. A systematic review of the evidence-based psychosocial risk factors for understanding of borderline personality disorder. Psychoanal. Psychother. 2012, 26, 65–91. [Google Scholar] [CrossRef]
- Winsper, C.; Lereya, S.T.; Marwaha, S.; Thompson, A.; Eyden, J.; Singh, S.P. The aetiological and psychopathological validity of borderline personality disorder in youth: A systematic review and meta-analysis. Clin. Psychol. Rev. 2016, 44, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Petfield, L.; Startup, H.; Droscher, H.; Cartwright-Hatton, S. Parenting in mothers with borderline personality disorder and impact on child outcomes. Evid.-Based Ment. Health 2015, 18, 67–75. [Google Scholar] [CrossRef] [Green Version]
- Laulik, S.; Chou, S.; Browne, K.D.; Allam, J. The link between personality disorder and parenting behaviors: A systematic review. Aggress. Violent Behav. 2013, 18, 644–655. [Google Scholar] [CrossRef]
- Eyden, J.; Winsper, C.; Wolke, D.; Broome, M.R.; MacCallum, F. A systematic review of the parenting and outcomes experienced by offspring of mothers with borderline personality pathology: Potential mechanisms and clinical implications. Clin. Psychol. Rev. 2016, 47, 85–105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steele, K.R.; Townsend, M.L.; Grenyer, B.F.S. Parenting and personality disorder: An overview and meta-synthesis of systematic reviews. PLoS ONE 2019, 14, e0223038. [Google Scholar] [CrossRef] [PubMed]
- Stepp, S.D.; Olino, T.M.; Klein, D.N.; Seeley, J.R.; Lewinsohn, P.M. Unique influences of adolescent antecedents on adult borderline personality disorder features. Pers. Disord. Theory. Res. Treat. 2013, 4, 223–229. [Google Scholar] [CrossRef] [Green Version]
- Vanwoerden, S.; Kalpakci, A.; Sharp, C. The relations between inadequate parent-child boundaries and borderline personality disorder in adolescence. Psychiatry Res. 2017, 257, 462–471. [Google Scholar] [CrossRef]
- Lyons-Ruth, K.; Brumariu, L.E.; Bureau, J.-F.; Hennighausen, K.; Holmes, B. Role Confusion and Disorientation in Young Adult-Parent Interaction Among Individuals with Borderline Symptomatology. J. Pers. Disord. 2015, 29, 641–662. [Google Scholar] [CrossRef]
- Infurna, M.R.; Fuchs, A.; Fischer-Waldschmidt, G.; Reichl, C.; Holz, B.; Resch, F.; Brunner, R.; Kaess, M. Parents′ childhood experiences of bonding and parental psychopathology predict borderline personality disorder during adolescence in offspring. Psychiatry Res. 2016, 246, 373–378. [Google Scholar] [CrossRef]
- Carlson, E.A.; Egeland, B.; Sroufe, L.A. A prospective investigation of the development of borderline personality symptoms. Dev. Psychopathol. 2009, 21, 1311–1334. [Google Scholar] [CrossRef]
- Greenfield, B.; Henry, M.; Lis, E.; Slatkoff, J.; Guilé, J.-M.; Dougherty, G.; Zhang, X.; Raz, A.; Arnold, L.E.; Daniel, L.; et al. Correlates, stability and predictors of borderline personality disorder among previously suicidal youth. Eur. Child Adolesc. Psychiatry 2015, 24, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Hammen, C.; Bower, J.E.; Cole, S.W. Oxytocin Receptor Gene Variation and Differential Susceptibility to Family Environment in Predicting Youth Borderline Symptoms. J. Pers. Disord. 2015, 29, 177–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Winsper, C.; Zanarini, M.; Wolke, D. Prospective study of family adversity and maladaptive parenting in childhood and borderline personality disorder symptoms in a non-clinical population at 11 years. Psychol. Med. 2012, 42, 2405–2420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lenzenweger, M.F.; Cicchetti, D. Toward a developmental psychopathology approach to borderline personality disorder. Dev. Psychopathol. 2005, 17, 893–898. [Google Scholar] [CrossRef] [Green Version]
- MacFie, J. Development in Children and Adolescents Whose Mothers Have Borderline Personality Disorder. Child Dev. Perspect. 2009, 3, 66–71. [Google Scholar] [CrossRef]
- Reinelt, E.; Stopsack, M.; Aldinger, M.; Ulrich, I.; Grabe, H.J.; Barnow, S. Longitudinal Transmission Pathways of Borderline Personality Disorder Symptoms: From Mother to Child? Psychopathology 2013, 47, 10–16. [Google Scholar] [CrossRef]
- Barnow, S.; Aldinger, M.; Arens, E.A.; Ulrich, I.; Spitzer, C.; Grabe, H.-J.; Stopsack, M. Maternal Transmission of Borderline Personality Disorder Symptoms in the Community-Based Greifswald Family Study. J. Pers. Disord. 2013, 27, 806–819. [Google Scholar] [CrossRef]
- Mahan, R.M.; Kors, S.B.; Simmons, M.L.; Macfie, J. Maternal psychological control, maternal borderline personality disorder, and adolescent borderline features. Pers. Disord. Theory. Res. Treat. 2018, 9, 297–304. [Google Scholar] [CrossRef]
- Steele, K.R.; Townsend, M.L.; Grenyer, B.F.S. Parenting stress and competence in borderline personality disorder is associated with mental health, trauma history, attachment and reflective capacity. Borderline Pers. Disord. Emot. Dysregul. 2020, 7, 8. [Google Scholar] [CrossRef]
- Conway, C.C.; Hammen, C.; Brennan, P.A. Adolescent Precursors of Adult Borderline Personality Pathology in a High-Risk Community Sample. J. Pers. Disord. 2015, 29, 316–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bezirganian, S.; Cohen, P.; Brook, J.S. The impact of mother-child interaction on the development of borderline personality disorder. Am. J. Psychiatry 1993, 150, 1836–1842. [Google Scholar] [CrossRef] [PubMed]
- Herzog, J.I.; Schmahl, C. Adverse Childhood Experiences and the Consequences on Neurobiological, Psychosocial, and Somatic Conditions Across the Lifespan. Front. Psychiatry 2018, 9, 420. [Google Scholar] [CrossRef]
- Bozzatello, P.; Rocca, P.; Bellino, S. Trauma and psychopathology associated with early onset BPD: An empirical contribution. J. Psychiatr. Res. 2020, 131, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Rogosch, F.A.; Cicchetti, D. Child Maltreatment and Emergent Personality Organization: Perspectives from the Five-Factor Model. J. Abnorm. Child Psychol. 2004, 32, 123–145. [Google Scholar] [CrossRef] [PubMed]
- Geselowitz, B.; Whalen, D.J.; Tillman, R.; Barch, D.M.; Luby, J.L.; Vogel, A. Preschool Age Predictors of Adolescent Borderline Personality Symptoms. J. Am. Acad. Child Adolesc. Psychiatry 2020, 60, 612–622. [Google Scholar] [CrossRef]
- Biskin, R.S.; Paris, J.; Renaud, J.; Raz, A.; Zelkowitz, P. Outcomes in Women Diagnosed with Borderline Personality Disorder in Adolescence. J. Can. Acad. Child Adolesc. Psychiatry 2011, 20, 168–174. [Google Scholar]
- Goodman, M.; Hazlett, E.A.; Avedon, J.B.; Siever, D.R.; Chu, K.-W.; New, A.S. Anterior cingulate volume reduction in adolescents with borderline personality disorder and co-morbid major depression. J. Psychiatr. Res. 2010, 45, 803–807. [Google Scholar] [CrossRef]
- Venta, A.; Kenkel-Mikelonis, R.; Sharp, C. A preliminary study of the relation between trauma symptoms and emerging BPD in adolescent inpatients. Bull. Menn. Clin. 2012, 76, 130–146. [Google Scholar] [CrossRef]
- Infurna, M.R.; Brunner, R.; Holz, B.; Parzer, P.; Giannone, F.; Reichl, C.; Fischer, G.; Resch, F.; Kaess, M. The Specific Role of Childhood Abuse, Parental Bonding, and Family Functioning in Female Adolescents with Borderline Personality Disorder. J. Pers. Disord. 2016, 30, 177–192. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, C.; Tarlow, N.; Stewart, J.G.; Aguirre, B.; Galen, G.; Auerbach, R.P. Borderline personality disorder in youth: The prospective impact of child abuse on non-suicidal self-injury and suicidality. Compr. Psychiatry 2016, 71, 86–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajan, G.; Syding, S.; Ljunggren, G.; Wändell, P.; Wahlström, L.; Philips, B.; Svedin, C.G.; Carlsson, A.C. Health care consumption and psychiatric diagnoses among adolescent girls 1 and 2 years after a first-time registered child sexual abuse experience: A cohort study in the Stockholm Region. Eur. Child Adolesc. Psychiatry 2020, 30, 1803–1811. [Google Scholar] [CrossRef]
- Horesh, N.; Ratner, S.; Laor, N.; Toren, P. A Comparison of Life Events in Adolescents with Major Depression, Borderline Personality Disorder and Matched Controls: A Pilot Study. Psychopathology 2008, 41, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Horesh, N.; Nachshoni, T.; Wolmer, L.; Toren, P. A comparison of life events in suicidal and nonsuicidal adolescents and young adults with major depression and borderline personality disorder. Compr. Psychiatry 2009, 50, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Sengutta, M.; Gawęda, L.; Moritz, S.; Karow, A. The mediating role of borderline personality features in the relationship between childhood trauma and psychotic-like experiences in a sample of help-seeking non-psychotic adolescents and young adults. Eur. Psychiatry 2019, 56, 84–90. [Google Scholar] [CrossRef]
- Turniansky, H.; Ben-Dor, D.; Krivoy, A.; Weizman, A.; Shoval, G. A history of prolonged childhood sexual abuse is associated with more severe clinical presentation of borderline personality disorder in adolescent female inpatients—A naturalistic study. Child Abus. Negl. 2019, 98, 104222. [Google Scholar] [CrossRef]
- Hecht, K.F.; Cicchetti, D.; Rogosch, F.A.; Crick, N.R. Borderline personality features in childhood: The role of subtype, developmental timing, and chronicity of child maltreatment. Dev. Psychopathol. 2014, 26, 805–815. [Google Scholar] [CrossRef] [Green Version]
- Belsky, D.W.; Caspi, A.; Arseneault, L.; Bleidorn, W.; Fonagy, P.; Goodman, M.; Houts, R.; Moffitt, T. Etiological features of borderline personality related characteristics in a birth cohort of 12-year-old children. Dev. Psychopathol. 2012, 24, 251–265. [Google Scholar] [CrossRef] [Green Version]
- Jovev, M.; McKenzie, T.; Whittle, S.; Simmons, J.G.; Allen, N.; Chanen, A.M. Temperament and Maltreatment in the Emergence of Borderline and Antisocial Personality Pathology during Early Adolescence. J. Can. Acad. Child Adolesc. Psychiatry 2013, 22, 220–229. [Google Scholar]
- Johnson, J.G.; Cohen, P.; Smailes, E.M.; Skodol, A.E.; Brown, J.; Oldham, J.M. Childhood verbal abuse and risk for personality disorders during adolescence and early adulthood. Compr. Psychiatry 2001, 42, 16–23. [Google Scholar] [CrossRef] [Green Version]
- Johnson, J.G.; Smailes, E.M.; Cohen, P.; Brown, J.; Bernstein, D.P. Associations Between Four Types of Childhood Neglect and Personality Disorder Symptoms During Adolescence and Early Adulthood: Findings of a Community-Based Longitudinal Study. J. Pers. Disord. 2000, 14, 171–187. [Google Scholar] [CrossRef] [PubMed]
- Lyons-Ruth, K.; Bureau, J.-F.; Holmes, B.; Easterbrooks, A.; Brooks, N.H. Borderline symptoms and suicidality/self-injury in late adolescence: Prospectively observed relationship correlates in infancy and childhood. Psychiatry Res. 2013, 206, 273–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Staebler, K.; Renneberg, B.; Stopsack, M.; Fiedler, P.; Weiler, M.; Roepke, S. Facial emotional expression in reaction to social exclusion in borderline personality disorder. Psychol. Med. 2011, 41, 1929–1938. [Google Scholar] [CrossRef] [PubMed]
- Wolke, D.; Schreier, A.; Zanarini, M.C.; Winsper, C. Bullied by peers in childhood and borderline personality symptoms at 11 years of age: A prospective study. J. Child Psychol. Psychiatry 2012, 53, 846–855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lereya, S.T.; Winsper, C.; Heron, J.; Lewis, G.; Gunnell, D.; Fisher, H.; Wolke, D. Being Bullied During Childhood and the Prospective Pathways to Self-Harm in Late Adolescence. J. Am. Acad. Child Adolesc. Psychiatry 2013, 52, 608–618.e2. [Google Scholar] [CrossRef] [Green Version]
- Winsper, C.; Hall, J.; Strauss, V.Y.; Wolke, D. Aetiological pathways to Borderline Personality Disorder symptoms in early adolescence: Childhood dysregulated behaviour, maladaptive parenting and bully victimisation. Borderline Pers. Disord. Emot. Dysregul. 2017, 4, 10. [Google Scholar] [CrossRef]
- Haltigan, J.D.; Vaillancourt, T. Identifying trajectories of borderline personality features in adolescence: Antecedent and interactive risk factors. Can. J. Psychiatry 2016, 61, 166–175. [Google Scholar] [CrossRef] [Green Version]
- Antila, H.; Arola, R.; Hakko, H.; Riala, K.; Riipinen, P.; Kantojärvi, L. Bullying involvement in relation to personality disorders: A prospective follow-up of 508 inpatient adolescents. Eur. Child Adolesc. Psychiatry 2017, 26, 779–789. [Google Scholar] [CrossRef] [Green Version]
- Bornovalova, M.A.; Huibregtse, B.M.; Hicks, B.M.; Keyes, M.; McGue, M.; Iacono, W.G. Tests of a direct effect of childhood abuse on adult borderline personality disorder traits: A longitudinal discordant twin design. J. Abnorm. Psychol. 2013, 122, 180–194. [Google Scholar] [CrossRef] [Green Version]
- Cicchetti, D.; Rogosch, F.A.; Hecht, K.F.; Crick, N.R.; Hetzel, S. Moderation of maltreatment effects on childhood borderline personality symptoms by gender and oxytocin receptor and FK506 binding protein 5 genes. Dev. Psychopathol. 2014, 26, 831–849. [Google Scholar] [CrossRef] [Green Version]
- Crick, N.R.; Murray–Close, D.; Woods, K. Borderline personality features in childhood: A short-term longitudinal study. Dev. Psychopathol. 2005, 17, 1051–1070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nelson, D.A.; Coyne, S.M.; Swanson, S.M.; Hart, C.H.; Olsen, J.A. Parenting, relational aggression, and borderline personality features: Associations over time in a Russian longitudinal sample. Dev. Psychopathol. 2014, 26, 773–787. [Google Scholar] [CrossRef]
- Vaillancourt, T.; Brittain, H.L.; McDougall, P.; Krygsman, A.; Boylan, K.; Duku, E.; Hymel, S. Predicting borderline personality disorder symptoms in adolescents from childhood physical and relational aggression, depression, and attention-deficit/hyperactivity disorder. Dev. Psychopathol. 2014, 26, 817–830. [Google Scholar] [CrossRef] [PubMed]
- Conway, C.C.; Hipwell, A.E.; Stepp, S. Seven-Year Course of Borderline Personality Disorder Features: Borderline Pathology Is as Unstable as Depression During Adolescence. Clin. Psychol. Sci. 2017, 5, 742–749. [Google Scholar] [CrossRef] [Green Version]
- Joyce, P.R.; McKenzie, J.M.; Luty, S.E.; Mulder, R.T.; Carter, J.D.; Sullivan, P.F.; Cloninger, C.R. Temperament, childhood environment and psychopathology as risk factors for avoidant and borderline personality disorders. Aust. N. Z. J. Psychiatry 2003, 37, 756–764. [Google Scholar] [CrossRef]
- Tragesser, S.L.; Robinson, R.J. The Role of Affective Instability and UPPS Impulsivity in Borderline Personality Disorder Features. J. Pers. Disord. 2009, 23, 370–383. [Google Scholar] [CrossRef]
- Gratz, K.L.; Tull, M.T.; Reynolds, E.K.; Bagge, C.L.; Latzman, R.D.; Daughters, S.B.; Lejuez, C.W. Extending extant models of the pathogenesis of borderline personality disorder to childhood borderline personality symptoms: The roles of affective dysfunction, disinhibition, and self- and emotion-regulation deficits. Dev. Psychopathol. 2009, 21, 1263–1291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tragesser, S.L.; Solhan, M.; Brown, W.C.; Tomko, R.; Bagge, C.; Trull, T.J. Longitudinal Associations in Borderline Personality Disorder Features: Diagnostic Interview for Borderlines-Revised (DIB-R) Scores over Time. J. Pers. Disord. 2010, 24, 377–391. [Google Scholar] [CrossRef] [Green Version]
- Underwood, M.K.; Beron, K.J.; Rosen, L.H. Joint trajectories for social and physical aggression as predictors of adolescent maladjustment: Internalizing symptoms, rule-breaking behaviors, and borderline and narcissistic personality features. Dev. Psychopathol. 2011, 23, 659–678. [Google Scholar] [CrossRef] [Green Version]
- Kaess, M.; Resch, F.; Parzer, P.; von Ceumern-Lindenstjerna, I.-A.; Henze, R.; Brunner, R. Temperamental Patterns in Female Adolescents with Borderline Personality Disorder. J. Nerv. Ment. Dis. 2013, 201, 109–115. [Google Scholar] [CrossRef]
- Martín-Blanco, A.; Soler, J.; Villalta, L.; Feliu-Soler, A.; Elices, M.; Pérez, V.; Arranz, M.J.; Ferraz, L.; Álvarez, E.; Pascual, J.C. Exploring the interaction between childhood maltreatment and temperamental traits on the severity of borderline personality disorder. Compr. Psychiatry 2014, 55, 311–318. [Google Scholar] [CrossRef]
- Jovev, M.; Whittle, S.; Yücel, M.; Simmons, J.G.; Allen, N.B.; Chanen, A.M. The relationship between hippocampal asymmetry and temperament in adolescent borderline and antisocial personality pathology. Dev. Psychopathol. 2013, 26, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Hallquist, M.N.; Hipwell, A.E.; Stepp, S.D. Poor self-control and harsh punishment in childhood prospectively predict borderline personality symptoms in adolescent girls. J. Abnorm. Psychol. 2015, 124, 549–564. [Google Scholar] [CrossRef]
- Sharp, C.; Kalpakci, A.; Mellick, W.; Venta, A.; Temple, J.R. First evidence of a prospective relation between avoidance of internal states and borderline personality disorder features in adolescents. Eur. Child Adolesc. Psychiatry 2015, 24, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Cramer, P. Childhood Precursors of Adult Borderline Personality Disorder Features: A Longitudinal Study. J. Nerv. Ment. Dis. 2016, 204, 494–499. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, J.G.; Herpertz, S.C.; Skodol, A.E.; Torgersen, S.; Zanarini, M.C. Borderline personality disorder. Nat. Rev. Dis. Prim. 2018, 4, 18029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torgersen, S.; Lygren, S.; Øien, P.A.; Skre, I.; Onstad, S.; Edvardsen, J.; Tambs, K.; Kringlen, E. A twin study of personality disorders. Compr. Psychiatry 2000, 41, 416–425. [Google Scholar] [CrossRef]
- Torgersen, S.; Myers, J.; Reichborn-Kjennerud, T.; Roysamb, E.; Kubarych, T.S.; Kendler, K.S. The Heritability of Cluster B Personality Disorders Assessed Both by Personal Interview and Questionnaire. J. Pers. Disord. 2012, 26, 848–866. [Google Scholar] [CrossRef] [PubMed]
- Reichborn-Kjennerud, T.; Czajkowski, N.; Ystrom, E.; Orstavik, R.E.; Aggen, S.H.; Tambs, K.; Torgersen, S.; Neale, M.C.; Roysamb, E.; Krueger, R.F.; et al. A longitudinal twin study of borderline and antisocial personality disorder traits in early to middle adulthood. Psychol. Med. 2015, 45, 3121–3131. [Google Scholar] [CrossRef]
- Torgersen, S.; Czajkowski, N.; Jacobson, K.; Reichborn-Kjennerud, T.; Røysamb, E.; Neale, M.C.; Kendler, K.S. Dimensional representations of DSM-IV cluster B personality disorders in a population-based sample of Norwegian twins: A multivariate study. Psychol. Med. 2008, 38, 1617–1625. [Google Scholar] [CrossRef] [Green Version]
- Kendler, K.S.; Aggen, S.H.; Czajkowski, N.; Roysamb, E.; Tambs, K.; Torgersen, S.; Neale, M.C.; Reichborn-Kjennerud, T. The Structure of Genetic and Environmental Risk Factors for DSM-IV Personality Disorders. Arch. Gen. Psychiatry 2008, 65, 1438–1446. [Google Scholar] [CrossRef] [Green Version]
- Bornovalova, M.A.; Hicks, B.M.; Iacono, W.G.; McGue, M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: A longitudinal twin study. Dev. Psychopathol. 2009, 21, 1335–1353. [Google Scholar] [CrossRef] [PubMed]
- Feldman, R.; Gordon, I.; Schneiderman, I.; Weisman, O.; Zagoory-Sharon, O. Natural variations in maternal and paternal care are associated with systematic changes in oxytocin following parent–infant contact. Psychoneuroendocrinology 2010, 35, 1133–1141. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, J.G.; Zanarini, M.C.; Choi-Kain, L.; Mitchell, K.S.; Jang, K.L.; Hudson, J.I. Family Study of Borderline Personality Disorder and Its Sectors of Psychopathology. Arch. Gen. Psychiatry 2011, 68, 753–762. [Google Scholar] [CrossRef] [Green Version]
- Veer, I.M.; Oei, N.Y.; Spinhoven, P.; van Buchem, M.A.; Elzinga, B.M.; Rombouts, S.A. Endogenous cortisol is associated with functional connectivity between the amygdala and medial prefrontal cortex. Psychoneuroendocrinology 2012, 37, 1039–1047. [Google Scholar] [CrossRef] [Green Version]
- Perroud, N.; Salzmann, A.; Prada, P.; Nicastro, R.; Hoeppli, M.-E.; Furrer, S.; Ardu, S.; Krejci, I.; Karege, F.; Malafosse, A. Response to psychotherapy in borderline personality disorder and methylation status of the BDNF gene. Transl. Psychiatry 2013, 3, e207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prados, J.; Stenz, L.; Courtet, P.; Prada, P.; Nicastro, R.; Adouan, W.; Guillaume, S.; Olié, E.; Aubry, J.-M.; Dayer, A.; et al. Borderline personality disorder and childhood maltreatment: A genome-wide methylation analysis. Genes Brain Behav. 2015, 14, 177–188. [Google Scholar] [CrossRef]
- Martín-Blanco, A.; Ferrer, M.; Soler, J.; Arranz, M.J.; Vega, D.; Calvo, N.; Elices, M.; Sánchez-Mora, C.; Garcia-Martínez, I.; Salazar, J.; et al. The role of hypothalamus-pituitary-adrenal genes and childhood trauma in borderline personality disorder. Eur. Arch. Psychiatry Clin. Neurosci. 2016, 266, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Witt, S.H.; Streit, F.; Jungkunz, M.; Frank, J.; Awasthi, S.; Reinbold, C.S.; Treutlein, J.; Degenhardt, F.; Forstner, A.J.; Bipolar Disorders Working Group of the Psychiatric Genomics Consortium; et al. Genome-wide association study of borderline personality disorder reveals genetic overlap with bipolar disorder, major depression and schizophrenia. Transl. Psychiatry 2017, 7, e1155. [Google Scholar] [CrossRef]
- Di Iorio, C.R.; Carey, C.E.; Michalski, L.J.; Corral-Frias, N.; Conley, E.D.; Hariri, A.R.; Bogdan, R. Hypothalamic-pituitary-adrenal axis genetic variation and early stress moderates amygdala function. Psychoneuroendocrinology 2017, 80, 170–178. [Google Scholar] [CrossRef] [Green Version]
- Pratt, M.; Apter-Levi, Y.; Vakart, A.; Kanat-Maymon, Y.; Zagoory-Sharon, O.; Feldman, R. Mother-child adrenocortical synchrony; Moderation by dyadic relational behavior. Horm. Behav. 2017, 89, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Amad, A.; Ramoz, N.; Thomas, P.; Jardri, R.; Gorwood, P. Genetics of borderline personality disorder: Systematic review and proposal of an integrative model. Neurosci. Biobehav. Rev. 2014, 40, 6–19. [Google Scholar] [CrossRef] [PubMed]
- Cattane, N.; Rossi, R.; Lanfredi, M.; Cattaneo, A. Borderline personality disorder and childhood trauma: Exploring the affected biological systems and mechanisms. BMC Psychiatry 2017, 17, 221. [Google Scholar] [CrossRef] [Green Version]
- De Kloet, E.R.; Joels, M.; Holsboer, F. Stress and the brain: From adaptation to disease. Nat. Rev. Neurosci. 2005, 6, 463–475. [Google Scholar] [CrossRef] [PubMed]
- Carrion, V.G.; Wong, S.S. Can Traumatic Stress Alter the Brain? Understanding the Implications of Early Trauma on Brain Development and Learning. J. Adolesc. Health 2012, 51, S23–S28. [Google Scholar] [CrossRef]
- Zimmerman, M.; Chelminski, I.; Young, D.; Dalrymple, K.; Martinez, J. Does the Presence of One Feature of Borderline Personality Disorder Have Clinical Significance? J. Clin. Psychiatry 2012, 73, 8–12. [Google Scholar] [CrossRef]
- Zimmerman, M.; Chelminski, I.; Young, D.; Dalrymple, K.; Martinez, J. Is Dimensional Scoring of Borderline Personality Disorder Important Only for Subthreshold Levels of Severity? J. Pers. Disord. 2013, 27, 244–251. [Google Scholar] [CrossRef]
- Ellison, W.; Rosenstein, L.; Chelminski, I.; Dalrymple, K.; Zimmerman, M. The Clinical Significance of Single Features of Borderline Personality Disorder: Anger, Affective Instability, Impulsivity, and Chronic Emptiness in Psychiatric Outpatients. J. Pers. Disord. 2016, 30, 261–270. [Google Scholar] [CrossRef] [Green Version]
- Ramklint, M.; von Knorring, L.-A.; von Knorring, L.; Ekselius, L. Child and adolescent psychiatric disorders predicting adult personality disorder: A follow-up study. Nord. J. Psychiatry 2003, 57, 23–28. [Google Scholar] [CrossRef]
- Thatcher, D.L.; Cornelius, J.R.; Clark, D.B. Adolescent alcohol use disorders predict adult borderline personality. Addict. Behav. 2005, 30, 1709–1724. [Google Scholar] [CrossRef]
- Sharp, C.; Wall, K. Personality pathology grows up: Adolescence as a sensitive period. Curr. Opin. Psychol. 2018, 21, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.J.; Flory, J.D.; Miller, S.R.; Harty, S.C.; Newcorn, J.; Helperin, J.M. Childhood Attention-Deficit/Hyperactivity Disorder and the Emergence of Personality Disorders in Adolescence. J. Clin. Psychiatry 2008, 69, 1477–1484. [Google Scholar] [CrossRef] [PubMed]
- Stepp, S.D.; Burke, J.D.; Hipwell, A.E.; Loeber, R. Trajectories of Attention Deficit Hyperactivity Disorder and Oppositional Defiant Disorder Symptoms as Precursors of Borderline Personality Disorder Symptoms in Adolescent Girls. J. Abnorm. Child Psychol. 2012, 40, 7–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krabbendam, A.A.; Colins, O.F.; Doreleijers, T.A.H.; van der Molen, E.; Beekman, A.T.F.; Vermeiren, R.R.J.M. Personality disorders in previously detained adolescent females: A prospective study. Am. J. Orthopsychiatry 2015, 85, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Bo, S.; Kongerslev, M. Self-reported patterns of impairments in mentalization, attachment, and psychopathology among clinically referred adolescents with and without borderline personality pathology. Borderline Pers. Disord. Emot. Dysregul. 2017, 4, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koenig, J.; Brunner, R.; Schmidt, J.M.; Parzer, P.; Resch, F.; Kaess, M. Psychopathology and Borderline Personality Pathology Associated with Lifetime Self-Injurious Behavior in Adolescent Psychiatric Inpatients and Detainees; 2017; Volume 45, pp. 441–451. [Google Scholar] [CrossRef]
- Zanarini, M.C.; Skodol, A.E.; Bender, D.; Dolan, R.; Sanislow, C.; Schaefer, E.; Morey, L.; Grilo, C.M.; Shea, M.T.; McGlashan, T.H.; et al. The Collaborative Longitudinal Personality Disorders Study: Reliability of Axis I and II Diagnoses. J. Pers. Disord. 2000, 14, 291–299. [Google Scholar] [CrossRef] [Green Version]
- Samuel, D.B.; Sanislow, C.A.; Hopwood, C.; Shea, M.T.; Skodol, A.E.; Morey, L.C.; Ansell, E.B.; Markowitz, J.C.; Zanarini, M.C.; Grilo, C.M. Convergent and incremental predictive validity of clinician, self-report, and structured interview diagnoses for personality disorders over 5 years. J. Consult. Clin. Psychol. 2013, 81, 650–659. [Google Scholar] [CrossRef] [Green Version]
- Zimmerman, M.; Multach, M.D.; Dalrymple, K.; Chelminski, I. Clinically useful screen for borderline personality disorder in psychiatric out-patients. Br. J. Psychiatry 2017, 210, 165–166. [Google Scholar] [CrossRef] [Green Version]
- Fung, H.W.; Chan, C.; Lee, C.Y.; Yau, C.; Chung, H.M.; Ross, C.A. Validity of A Web-based Measure of Borderline Personality Disorder: A Preliminary Study. J. Evid.-Based Soc. Work. 2020, 17, 443–456. [Google Scholar] [CrossRef]
- Chanen, A.M.; Velakoulis, D.; Carison, K.; Gaunson, K.; Wood, S.; Yuen, H.P.; Yücel, M.; Jackson, H.; McGorry, P.D.; Pantelis, C. Orbitofrontal, amygdala and hippocampal volumes in teenagers with first-presentation borderline personality disorder. Psychiatry Res. Neuroimaging 2008, 163, 116–125. [Google Scholar] [CrossRef]
- Whittle, S.; Chanen, A.; Fornito, A.; McGorry, P.D.; Pantelis, C.; Yücel, M. Anterior cingulate volume in adolescents with first-presentation borderline personality disorder. Psychiatry Res. Neuroimaging 2009, 172, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Brunner, R.; Henze, R.; Parzer, P.; Kramer, J.; Feigl, N.; Lutz, K.; Essig, M.; Resch, F.; Stieltjes, B. Reduced prefrontal and orbitofrontal gray matter in female adolescents with borderline personality disorder: Is it disorder specific? NeuroImage 2010, 49, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Walterfang, M.; Chanen, A.; Barton, S.; Wood, A.; Jones, S.; Reutens, D.; Chen, J.; Velakoulis, D.; McGorry, P.D.; Pantelis, C. Corpus callosum morphology and relationship to orbitofrontal and lateral ventricular volume in teenagers with first-presentation borderline personality disorder. Psychiatry Res. Neuroimaging 2010, 183, 30–37. [Google Scholar] [CrossRef]
- Doering, S.; Enzi, B.; Faber, C.; Hinrichs, J.; Bahmer, J.; Northoff, G. Personality Functioning and the Cortical Midline Structures—An Exploratory fMRI Study. PLoS ONE 2012, 7, e49956. [Google Scholar] [CrossRef] [PubMed]
- New, A.S.; Carpenter, D.M.; Rodriguez, M.D.P.; Ripoll, L.H.; Avedon, J.; Patil, U.; Hazlett, E.A.; Goodman, M. Developmental differences in diffusion tensor imaging parameters in borderline personality disorder. J. Psychiatr. Res. 2013, 47, 1101–1109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maier-Hein, K.H.; Brunner, R.; Lutz, K.; Henze, R.; Parzer, P.; Feigl, N.; Kramer, J.; Meinzer, H.-P.; Resch, F.; Stieltjes, B. Disorder-Specific White Matter Alterations in Adolescent Borderline Personality Disorder. Biol. Psychiatry 2014, 75, 81–88. [Google Scholar] [CrossRef]
- Richter, J.; Brunner, R.; Parzer, P.; Resch, F.; Stieltjes, B.; Henze, R. Reduced cortical and subcortical volumes in female adolescents with borderline personality disorder. Psychiatry Res. Neuroimaging 2014, 221, 179–186. [Google Scholar] [CrossRef]
- Beeney, J.E.; Hallquist, M.N.; Ellison, W.D.; Levy, K.N. Self–other disturbance in borderline personality disorder: Neural, self-report, and performance-based evidence. Pers. Disord. Theory. Res. Treat. 2016, 7, 28–39. [Google Scholar] [CrossRef] [Green Version]
- Bozzatello, P.; Morese, R.; Valentini, M.C.; Rocca, P.; Bosco, F.; Bellino, S. Autobiographical memories, identity disturbance and brain functioning in patients with borderline personality disorder: An fMRI study. Heliyon 2019, 5, e01323. [Google Scholar] [CrossRef] [Green Version]
- Pop-Jordanova, N.; Markovska-Simoska, S.; Milovanovic, M.; Lecic-Tosevski, D. Analysis of EEG Characteristics and Coherence in Patients Diagnosed as Borderline Personality. PRILOZI 2019, 40, 57–68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arikan, M.K.; Metin, B.; Gunver, M.G.; Tarhan, N.; Metin, B. Borderline Personality and Bipolar Disorders Cannot Be Differentiated Electrophysiologically. Clin. EEG Neurosci. 2019, 50, 383–388. [Google Scholar] [CrossRef]
- Orbach, I.; Mikulincer, M.; Gilboa-Schechtman, E.; Sirota, P. Mental Pain and Its Relationship to Suicidality and Life Meaning. Suicide Life-Threatening Behav. 2003, 33, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, J.G.; Morey, L.C.; Stout, R.L.; Skodol, A.E.; Shea, M.T.; McGlashan, T.H.; Zanarini, M.C.; Grilo, C.M.; Sanislow, C.A.; Yen, S.; et al. Major Depressive Disorder and Borderline Personality Disorder Revisited. J. Clin. Psychiatry 2004, 65, 1049–1056. [Google Scholar] [CrossRef]
- Eaton, N.R.; Krueger, R.F.; Keyes, K.M.; Skodol, A.E.; Markon, K.E.; Grant, B.F.; Hasin, D.S. Borderline personality disorder co-morbidity: Relationship to the internalizing–externalizing structure of common mental disorders. Psychol. Med. 2011, 41, 1041–1050. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hasin, D.; Fenton, M.C.; Skodol, A.; Krueger, R.; Keyes, K.; Geier, T.; Greenstein, E.; Blanco, C.; Grant, B. Personality Disorders and the 3-Year Course of Alcohol, Drug, and Nicotine Use Disorders. Arch. Gen. Psychiatry 2011, 68, 1158–1167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skodol, A.E.; Grilo, C.M.; Keyes, K.M.; Geier, T.; Grant, B.F.; Hasin, D.S. Relationship of Personality Disorders to the Course of Major Depressive Disorder in a Nationally Representative Sample. Am. J. Psychiatry 2011, 168, 257–264. [Google Scholar] [CrossRef]
- Gunderson, J.G.; Stout, R.; Shea, M.T.; Grilo, C.M.; Markowitz, J.C.; Morey, L.; Sanislow, C.; Yen, S.; Zanarini, M.C.; Keuroghlian, A.; et al. Interactions of Borderline Personality Disorder and Mood Disorders over 10 Years. J. Clin. Psychiatry 2014, 75, 829–834. [Google Scholar] [CrossRef]
- Keuroghlian, A.S.; Gunderson, J.G.; Pagano, M.E.; Markowitz, J.C.; Ansell, E.B.; Shea, M.T.; Morey, L.C.; Sanislow, C.; Grilo, C.M.; Stout, R.L.; et al. Interactions of Borderline Personality Disorder and Anxiety Disorders Over 10 Years. J. Clin. Psychiatry 2015, 76, 1529–1534. [Google Scholar] [CrossRef]
- Boritz, T.; Barnhart, R.; McMain, S.F. The Influence of Posttraumatic Stress Disorder on Treatment Outcomes of Patients with Borderline Personality Disorder. J. Pers. Disord. 2016, 30, 395–407. [Google Scholar] [CrossRef] [PubMed]
- Chanen, A.M.; Kaess, M. Developmental Pathways to Borderline Personality Disorder. Curr. Psychiatry Rep. 2012, 14, 45–53. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision ICD-10; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Bagby, R.M.; Widiger, T.A. Assessment of the ICD-11 dimensional trait model: An introduction to the special section. Psychol. Assess. 2020, 32, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bornovalova, M.A.; Verhulst, B.; Webber, T.; McGue, M.; Iacono, W.G.; Hicks, B.M. Genetic and environmental influences on the codevelopment among borderline personality disorder traits, major depression symptoms, and substance use disorder symptoms from adolescence to young adulthood. Dev. Psychopathol. 2018, 30, 49–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Livesley, W.J.; Jang, K.L. Toward an empirically based classification of personality disorder. J. Pers. Disord. 2000, 14, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Morey, L.C.; Benson, K.T. An Investigation of Adherence to Diagnostic Criteria, Revisited: Clinical Diagnosis of theDSM-IV/DSM-5Section II Personality Disorders. J. Pers. Disord. 2016, 30, 130–144. [Google Scholar] [CrossRef]
- Chanen, A.M.; Nicol, K.; Betts, J.K.; Thompson, K.N. Diagnosis and Treatment of Borderline Personality Disorder in Young People. Curr. Psychiatry Rep. 2020, 22, 25. [Google Scholar] [CrossRef] [PubMed]
- Kotov, R.; Krueger, R.F.; Watson, D.; Achenbach, T.M.; Althoff, R.R.; Bagby, R.M.; Brown, T.A.; Carpenter, W.T.; Caspi, A.; Clark, L.A.; et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. J. Abnorm. Psychol. 2017, 126, 454–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amad, A.; Radua, J.; Vaiva, G.; Williams, S.C.; Fovet, T. Similarities between borderline personality disorder and post traumatic stress disorder: Evidence from resting-state meta-analysis. Neurosci. Biobehav. Rev. 2019, 105, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Brewin, C.R.; Cloitre, M.; Hyland, P.; Shevlin, M.; Maercker, A.; Bryant, R.A.; Humayun, A.; Jones, L.M.; Kagee, A.; Rousseau, C.; et al. A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clin. Psychol. Rev. 2017, 58, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Ford, J.D.; Courtois, C.A. Complex PTSD, affect dysregulation, and borderline personality disorder. Borderline Pers. Disord. Emot. Dysregulation 2014, 1, 9. [Google Scholar] [CrossRef] [Green Version]
| Family-related factors | ||||
|---|---|---|---|---|
| Study | Study Design | Sample | Trial Duration | Outcomes |
| Cohen et al., 2008 [40] | Longitudinal study; community population | A random residence-based cohort of children and young adults between ages 10 and 36 | 26 years | Low family socioeconomic status → STPD and BPD in offspring |
| Crawford et al., 2009 [41] | Longitudinal study; community population | 766 youths aged 13 to 33 | 21 years | Extended maternal separations before age 5 → offspring BPD symptoms |
| Carlson et al., 2009 [56] | Longitudinal study; community population | A sample of young mothers and their first-born children (N = 162; 82 males, 80 females) | 28 years | BPD symptoms in adulthood related to endogenous and environmental history in early childhood |
| Winsper et al., 2012 [59] | Cohort study; community population | 6050 mothers and their children (age range 10.4–13.6 years, mean age 11.7 years) | 11 years | Family adversity → BPD symptoms of offspring |
| Stepp et al., 2013 [52] | Longitudinal cohort study; community population | 1709 students 14–18 years old (360 with a history of a depressive disorder and 284 with a history of mood disorders) vs. 457 HC | 16 years | Maternal-child discord, maternal BPD, paternal SUD + proband depression, SUD and suicidality associated with later BPD symptoms |
| Reinelt et al., 2013 [62] | Longitudinal cohort study; community population | 295 children (15–20 years old) and their biological mothers drawn from the population-based Greifswald Family Study | 5 years | Maladaptive mother-child interactions → longitudinal transmission of borderline symptoms from mother to child |
| Barnow et al., 2013 [63] | Longitudinal cohort study; community population | 323 offspring (15–20 years old) and their mothers from the community-based Greifswald Family Study | 5 years | Maternal BPD symptoms and depression → BPD and general psychopathology in offspring |
| Stepp, Whalen et al., 2014 [43] | Longitudinal cohort study; community population | 2451 girls aged 14–17 drawn from the Pittsburgh Girls Study | 3 years | Only-child characteristics, and not caregiver psychopathology, predicted BPD symptoms |
| Stepp et al., 2015 [37] | Longitudinal study; community population | 113 at-risk adolescent girls aged 16–18 | 3 years | Family adversity → ↑ BPD symptoms during late adolescence in offspring |
| Lyons-Ruth et al., 2015 [54] | Cross-sectional study; community population | 120 young adults | - | BPD traits → more role for confusion and more disoriented behavior in the interaction with the parent |
| Hammen et al., 2015 [58] | Longitudinal study; community population | 385 youths (235 females, 150 males, offspring of mothers with a probable history of depression) | 20 years | OXTR rs53576 moderates the link between early family quality and later BPD symptoms |
| Conway et al., 2015 [66] | Longitudinal study; community population | 700 at-risk youths (15–20 years old) | 5 years | Maternal externalizing disorder history, offspring internalizing disorder history, family stressors and school-related stressors → ↑ BPD risk |
| Winsper et al., 2015 [22] | Longitudinal study; community population | 6050 mothers and their children (11–12-year-olds) | 12 years | Prenatal anxiety and depression → BPD in offspring |
| Infurna et al., 2016 [55] | Cross-sectional study; clinical inpatient population | 91 female adolescent psychiatric inpatients (Mage = 15.57 years), along with 87 mothers and 59 fathers | - | Low maternal care and paternal psychiatric symptoms → adolescent BPD in offspring |
| Vanwoerden et al., 2017 [53] | Cross-sectional study; clinical inpatient population | 301 adolescent (65.1% female; ages 12–17) inpatients | - | Parental guilt induction and psychological control → children’s BPD features |
| Mahan et al., 2018 [64] | Cross-sectional study; clinical outpatients and community population | 28 mothers with a diagnosis of BPD and 28 HC with male and female adolescents aged 14–18 | - | Mothers with BPD use more total psychological control with their children → adolescent affective instability |
| Steele et al., 2020 [65] | Cross-sectional study; community population | 284 parents (94.72% female, Mage = 37.37), of which 69 (24.30%) met BPD criteria | - | Individuals high in BPD features → ↑ stress and ↓ competence in their parenting role |
| Trauma-related factors | ||||
| Study | Study Design | Sample | Trial Duration | Outcomes |
| Johnson et al., 2000 [86] | Longitudinal study; community population | 738 youths and their mothers | 18 years | Childhood emotional, physical and supervision neglect → ↑ risk for PDs + ↑ PD symptom levels during adolescence and early adulthood |
| Johnson et al., 2001 [85] | Longitudinal study; community population | 793 mothers and their offspring assessed in four waves (at ages 5, 14, 16 and 22 years) | 18 years | Maternal verbal abuse during childhood → BPD, NPD, OCPD and PPD during adolescence or early adulthood |
| Rogosch et al., 2004 [70] | Longitudinal study; community population | 211 six-year-old children (135 maltreated and 76 non-maltreated) | 3 years | Six-year-old maltreated children → ↓ agreeableness, conscientiousness and openness to experience + ↑ neuroticism, maintained at age 9 |
| Horesh et al., 2008 [78] | Cross-sectional study; community and clinical population | 19 adolescents with MDD, 20 with BPD and 20 matched controls | - | The BPD group reported more sexual abuse LE than the control and MDD groups |
| Horesh et al., 2009 [79] | Retrospective study; community and clinical population | 40 suicidal adolescents and young adults with MDD (22) or BPD (18), 40 non-suicidal adolescents and young adults with MDD (20) and BPD (20), 40 HC | - | Suicidal BPD participants reported more lifetime sex-abuse-related LE compared with non-suicidal BPD participants |
| Biskin et al., 2011 [71] | Longitudinal study; community and clinical population | 47 adolescent girls (31 with BPD, 16 HC) | 10 years | Unremitting BPD associated with a current episode of MDD, lifetime SUD and self-reported childhood sexual abuse |
| Staebler et al., 2011 [88] | Cross-sectional study; community and clinical population | 35 patients with BPD and 33 HC | - | A negative bias for perceived social participation and ambiguous facial emotional expressions → disturbed relatedness in patients with BPD |
| Venta et al., 2012 [74] | Cross-sectional study; clinical inpatient population | 147 adolescent BPD inpatients | - | Adolescents with BPD more likely to have a history of sexual trauma and to report sexual concerns |
| Belsky et al., 2012 [83] | Longitudinal cohort study; community population | 1116 pairs of same-sex twins | 12 years | Exposure to harsh treatment in the family environment through age 10 → BPD-related characteristics at age 12 |
| Wolke et al., 2012 [89] | Longitudinal study; community population | 6050 mothers and their children drawn from the Avon Longitudinal Study of Parents and Children (ALSPAC) | 11 years | Victims of peer bullying and of chronic victimization → ↑ risk of BPD symptoms |
| Jovev et al., 2013 [84] | Longitudinal study; community population | 245 children (aged 11–13) | 2 years | Childhood neglect → ↑ BPD symptoms; childhood abuse → ↑ ASPD symptoms |
| Lyons-Ruth et al., 2013 [87] | Longitudinal study; community population | Adolescents (Mage 19.9 years) from 56 families participating in a longitudinal study since infancy | 18 years | Maternal withdrawal in infancy → BPD symptoms + suicidality/self-injury in late adolescence |
| Lereya et al., 2013 [90] | Longitudinal study; community population | 4810 children and adolescents drawn from the Avon Longitudinal Study of Parents and Children (ALSPAC) cohort assessed for bullying exposure (7–10 years old) and self-harm (16–17 years old) | 10 years | Being bullied → ↑ risk of self-harm, directly and indirectly, via depression symptoms in early adolescence |
| Bornovalova et al., 2013 [94] | Longitudinal study; community population (twins) | Over 1300 pairs of twins (11 to 24 years old) | 13 years | Common genetic influences that also overlap with internalizing and externalizing disorders → association between childhood abuse and BPD traits |
| Hecht et al., 2014 [82] | Cross-sectional study; community population | 314 maltreated and 285 non-maltreated children (Mage = 11.30) from comparable low socioeconomic backgrounds | - | Maltreated children had more severe BPD features, according to chronicity, patterns of onset and recency of maltreatment |
| Cicchetti et al., 2014 [95] | Cross-sectional study; community population | 1051 maltreated and non-maltreated low-income children | - | Different pattern of gene-environment interaction according to gender |
| Stepp et al., 2015 [42] | Longitudinal study; community population | 113 at-risk adolescent girls aged 16–18 | 3 years | Exposure to adversity → ↑association between negative emotional reactivity and BPD symptoms |
| Infurna et al., 2016 [75] | Cross-sectional study; clinical population | 44 female adolescent inpatients with BPD and 47 CC with mixed psychiatric diagnoses | - | Sexual abuse, general family functioning and low maternal care → adolescent BPD |
| Kaplan et al., 2016 [76] | Longitudinal study; clinical population | 58 female youths with BPD aged 13–21 years with (n = 29) and without (n = 29) a history of child abuse | 2 months | Child abuse (particularly co-occurring physical and sexual abuse) → ↑ risk for NSSI + suicidality among BPD youths. |
| Haltigan et al., 2016 [92] | Longitudinal study; community population | 566 Canadian children assessed yearly from ages 8 to 16 | 8 years | Parent- and child-reported mental health symptoms + peer relations risk factors + intra-individual risk factors: significant predictors of personality psychopathology |
| Winsper et al., 2017 [91] | Retrospective study; community population | 7159 children drawn from the Avon Longitudinal Study of Parents and Children (ALSPAC), assessed from birth to 14 years | 14 years | Bully victimization associated with BPD symptoms |
| Antila et al., 2017 [93] | Longitudinal study; clinical inpatient population | 508 adolescent inpatients (300 girls, 208 boys) | 12 years | Female victims of bullying (but not boys) → ↑ likelihood of developing a PD later in life, especially BPD |
| Sengutta et al., 2019 [80] | Cross-sectional study; clinical inpatient population | 200 inpatients aged 16–21 years with non-psychotic disorders | - | Childhood trauma (emotional neglect and sexual abuse) → psychotic-like experiences, with the mediation of BPD features |
| Turniansky et al., 2019 [81] | Retrospective study; clinical inpatient population | 78 female adolescent inpatients with BPD with (n = 38) and without (n = 40) a history of prolonged childhood sexual abuse (CSA) | 8 years | Prolonged CSA → ↑ duration and ↑ number of psychiatric hospitalizations + ↑ rate of NSSI and suicidal attempts, smoking, alcohol use and sexual impulsivity. |
| Bozzatello et al., 2020 [69] | Cross-sectional study; clinical outpatient population | 68 BPD outpatients | - | Earlier onset of BPD mainly associated with traumatic events (abuse, neglect, dysfunction in household environment and bullying) |
| Rajan et al., 2020 [77] | Longitudinal cohort study; community population | 519 girls aged 12–17 with registration of CSA experience in their medical record and 4920 age-matched HC | 7 years | CSA → ↑ risk for suicide attempts, stress disorders, psychosis and alcohol abuse + ↑ healthcare consumption patterns and drug prescriptions |
| Geselowitz et al., 2021 [71] | Longitudinal cohort study; community population | 170 children drawn from a prospective longitudinal study of early childhood depression, assessed at ages 3, 6, 14 and 19 | 16 years | Preschool ACEs, internalizing symptoms and low maternal support → BPD symptoms + preschool and school-age suicidality |
| Study | Study Design | Sample | Trial Duration | Outcomes |
|---|---|---|---|---|
| Joyce et al., 2003 [100] | Cross-sectional study; clinical outpatient population | 180 depressed outpatients | - | Childhood abuse and/or neglect + borderline temperament + childhood and adolescent depression, hypomania, conduct disorder and alcohol and drug dependence → BPD |
| Crick et al., 2005 [96] | Longitudinal study; community population | 400 (54% female) fourth through sixth graders | 1 year | BPD features moderately stable over the course of the study, with girls reporting higher levels of BPD features than boys |
| Carlson et al., 2009 [56] | Longitudinal study; community population | A sample of young mothers and their first -born children (N = 162; 82 males, 80 females) | 28 years | Endogenous and environmental history in early childhood → disturbance of child functioning in middle childhood/early adolescence → BPD symptoms in adulthood |
| Tragesser et al., 2009 [101] | Cross-sectional study; community population | 141 undergraduates | - | Both affective instability and impulsivity uniquely associated with BPD features |
| Gratz et al., 2009 [102] | Cross-sectional study; community population | 263 children aged 9 to 13 | - | Effect of affective dysfunction and disinhibition in childhood BPD symptoms mediated by self- and emotion-regulation deficits |
| Tragesser et al., 2010 [103] | Longitudinal study; community population | 353 young adults (aged 18–20) | 2 years | Negative affect predictive of most BPD symptoms but not future impulsive behavior |
| Underwood et al., 2011 [104] | Longitudinal study; community population | 255 children aged 9 to 13 (131 girls and 124 boys) | 5 years | High levels of social and physical aggression in middle childhood → greatest risk for adolescent psychopathology (BPD and NPD) |
| Belsky et al., 2012 [83] | Longitudinal cohort study; community population | 1,116 pairs of same-sex twins followed from birth through age 12 years | 12 years | BPD-related characteristics more common in children who had exhibited poor cognitive function, impulsivity and more behavioral and emotional problems at age 5 years |
| Bornalova et al., 2013 [94] | Longitudinal study; community population (twins) | A large sample of twins (over 1300 pairs) aged 11–24 | 13 years | Common genetic influences that also overlap with internalizing and externalizing disorders → association between childhood abuse and BPD traits |
| Kaess et al., 2013 [105] | Cross-sectional study; community and clinical population | 33 adolescents with BPD, 35 clinical controls (CCs) and 31 healthy controls (HCs), all females | - | ↑ novelty seeking + ↑ harm avoidance + ↓ reward dependence in the adolescents with BPD |
| Stepp, Keenan et al., 2014 [37] | Longitudinal cohort study; community population | 2450 girls aged 5–8 at first evaluation, 14–19 at second evaluation, drawn from the Pittsburgh Girls Study | 5 years | Childhood temperament dimensions of emotionality, activity, low sociability and shyness predict adolescent BPD symptom development |
| Nelson et al., 2014 [97] | Longitudinal cohort study; community population | 168 preschool children (84 boys, 84 girls) living in intact, two-parent biological households | 10 years | Preschool relational aggression + aversive parenting → ↑ aggression + BPD features in adolescent females; preschool authoritative parenting → ↓ aggression and BPD features in boys, vs. authoritarian parenting → ↑ aggression |
| Vaillancourt et al., 2014 [98] | Longitudinal cohort study; community population | 484 youths (aged 10 to 14) | 4 years | Childhood relational aggression + depression for boys; physical and relational aggression + depression + ADHD for girls → BPD features at age 14 |
| Martín-Blanco et al., 2014 [106] | Cross-sectional study; clinical population | 130 BPD subjects | - | Temperamental traits + childhood emotional abuse → development + severity of BPD |
| Jovev et al., 2014 [107] | Cross-sectional study; community population | 153 healthy adolescents (Mage = 12.6 years) | - | Boys: ↑/↓ affiliation + hippocampal asymmetry → ↑ BPD symptoms; girls: ↓ effortful control + hippocampal asymmetry → ↑ BPD symptoms |
| Hallquist et al., 2015 [108] | Longitudinal study; community population | A sample of girls (aged 5 to 17) taken from the Pittsburgh Girls Study (n = 2450) | 12 years | Harsh punishment + poor self-control + negative emotionality → BPD symptom severity at age 14; ↓ self-control ages 12–14 → ↑BPD symptoms from 14 to 17 |
| Sharp et al., 2015 [109] | Longitudinal study; community population | 730 adolescents | 1 year | Experiential avoidance → BPD features + severity of BPD symptoms at 1-year follow-up |
| Cramer et al., 2016 [110] | Longitudinal study; community population | 100 youths (aged 11 to 23) | 12 years | Childhood personality traits (impulsivity + nonconformity/aggression) → adult BPD features |
| Conway et al., 2017 [99] | Longitudinal study; community population | 2450 high-risk adolescent girls aged 14 to 20 | 6 years | BPD pathology fluctuates in response to situational influences |
| Study | Study Design | Sample | Trial Duration | Outcomes |
|---|---|---|---|---|
| Torgersen et al., 2000 [112] | Cross-sectional study; community population | 92 monozygotic and 129 dizygotic twin pairs | - | PDs more strongly influenced by genetic effects than almost any axis I disorder and more than most broad personality dimensions (BPD heritability of 0.69) |
| Torgersen et al., 2008 [115] | Cross-sectional study; community population | 1386 Norwegian twin pairs between the age of 19 and 35 years | - | Heritability of PD traits: ASPD 38%, HPD 31%, NPD 24%, BPD 35% |
| Kendler et al., 2008 [116] | Cross-sectional study; community population | 2794 young-adult members of the Norwegian Institute of Public Health Twin Panel | - | Genetic risk factors → broad vulnerability to PD pathology and/or negative emotionality; environmental experiences → tendency of cluster A, B and C PDs to co-occur. |
| Bornovalova et al., 2009 [117] | Longitudinal study; community population | A large sample of adolescent female twins (aged 14–24) taking part in the Minnesota Twin Family Study (MTFS) | 10 years | Both the stability and change of BPD traits are highly influenced by genetic factors and modestly by nonshared environmental factors. |
| Feldman et al., 2010 [118] | Cross-sectional study; community population | 112 parents (71 mothers and 41 fathers) and their 4–6-month-old infants | - | Mothers with high levels of affectionate contact → ↑oxytocin following mother–infant interaction; fathers with high levels of stimulatory contact → ↑ oxytocin |
| Gunderson et al., 2011 [119] | Cross-sectional study; community and clinical population | A total of 368 probands (132 with BPD, 134 without BPD and 102 with MDD) and 885 siblings and parents of probands | - | Substantial familial aggregation of BPD |
| Torgersen et al., 2012 [113] | Cross-sectional study; community population | 2,794 twins from the Norwegian Institute of Public Health Twin Panel | - | Heritability of Cluster B PDs: 0.30 if assessed by interview, 0.40-0.50 if assessed by self-report questionnaire (0.67 for BPD) |
| Veer et al., 2012 [120] | Cross-sectional study; community population | 20 healthy male participants | - | Endogenous cortisol levels may modulate amygdala functional connectivity with specific regions in the medial PFC, even under relatively stress-free circumstances |
| Perroud et al., 2013 [121] | Cross-sectional study; community and clinical population | 115 subjects with borderline personality disorder (BPD) and 52 controls | - | BPD subjects → ↑ methylation status in BDNF gene; after I-DBT ↓ methylation status in responders (→ changes in depression, hopelessness and impulsivity scores), ↑ in non-responders |
| Reichborn-Kjennerud et al., 2015 [114] | Longitudinal study; community population | 2282 Norwegian twins in early adulthood | 10 years | Genetic risk factors → ASPD and BPD trait stability from early to middle adulthood; transient environmental risk factors → phenotypic change. |
| Prados et al., 2015 [122] | Cross-sectional study; clinical population | 96 BPD subjects suffering from a high level of child adversity and 93 subjects suffering from MDD and reporting a low rate of child maltreatment | - | Several genes differently methylated, either in BPD compared with MDD or in relation to the severity of childhood maltreatment |
| Martín-Blanco et al., 2016 [123] | Cross-sectional study; community and clinical population | 481 subjects with BPD and 442 controls | - | Several HPA axis genetic variants in BPD subjects with sexual and physical abuse |
| Witt et al., 2017 [124] | Cross-sectional study; community and clinical population | 998 BPD patients and 1545 controls | - | BPD overlaps with BD, MDD and schizophrenia on the genetic level |
| Iorio et al., 2017 [125] | Cross-sectional study; community population | 308 college-attending, non-Hispanic European-Americans who completed the Duke Neurogenetics Study | - | Polygenic variation linked to HPA axis function → risk for anxiety symptomatology |
| Pratt et al., 2017 [126] | Cross-sectional study; community and clinical population | 97 mothers (28 with MDD, 69 HC) with their 6-year-old children | - | Higher adrenocortical synchrony between mother and child → ↑ physiological stress and < adaptive dyadic relational patterns |
| Diagnostic Criteria | ||||
|---|---|---|---|---|
| Study | Study Design | Sample | Trial Duration | Outcomes |
| Zimmerman et al., 2012 [131] | Cross-sectional study; clinical population | 3,200 psychiatric outpatients (1,976 with 0 or 1 DSM-IV criterion for BPD) | - | Low-severity levels of borderline personality disorder pathology can be determined reliably and have validity |
| Zimmerman et al., 2013 [132] | Cross-sectional study; clinical population | 3,069 psychiatric outpatients | - | Dimensional scoring of BPD more important for subthreshold levels of pathology, less critical once a patient meets the diagnostic threshold |
| Ellison et al., 2016 [133] | Cross-sectional study; clinical population | 1,870 adult psychiatric outpatients | - | BPD criteria of impulsivity, affective instability, emptiness and anger → dysfunction; emptiness → marker of impairment on all indices of psychosocial morbidity |
| Clinical assessment | ||||
| Study | Study design | Sample | Trial duration | Outcomes |
| Ramklint et al., 2003 [134] | Cross-sectional study; clinical population | 158 former inpatients (Mage = 30.5 years) | - | Identification + treatment of childhood psychiatric disorders → ↓ risk for development of an adult PD |
| Thatcher et al., 2005 [135] | Longitudinal study; community and clinical population | 355 adolescents with AUD and 169 adolescents without AUD aged 16 to 22 years | 6 years | AUD and other adolescent psychopathology can culminate in BPD symptomatology |
| Chanen et al., 2007 [136] | Cross-sectional study; clinical population | 177 psychiatric outpatients aged 15 to 18 years (46 with BPD, 88 with other PDs and 43 with no PDs) | - | BPD → psychopathology, general functioning, peer relationships, self-care and family and relationship functioning (> than Axis I disorders and other PDs) |
| Miller et al., 2008 [137] | Longitudinal study; community and clinical population | 96 adolescents with ADHD and 85 HCs, aged 16 to 26 years old | 3 years | Childhood ADHD → ↑ risk for PDs in late adolescence. |
| Belsky et al., 2012 [83] | Longitudinal cohort study; community population | 1,116 pairs of same-sex twins followed from birth through age 12 years | 12 years | BPD-related characteristics at age 12 years co-occurred with symptoms of conduct disorder, depression, anxiety and psychosis |
| Wolke et al., 2012 [89] | Longitudinal study; community population | 6,050 mothers and their children drawn from the Avon Longitudinal Study of Parents and Children (ALSPAC) | 11 years | Peer bullying and chronic victimization → ↑risk of BPD symptoms |
| Stepp et al., 2012 [138] | Longitudinal cohort study; community population | 1,233 girls drawn from the Pittsburgh Girls Study, aged 10 to 14 years | 4 years | ↑ levels of ADHD and ODD scores at age 8 → BPD symptoms at age 14 |
| Stepp et al., 2013 [52] | Longitudinal cohort study; community population | 1,709 students (14–18 years old), of which 360 had a history of a depressive disorder and 284 had a history of mood disorders, compared with 457 HC | 16 years | Maternal-child discord, maternal BPD, paternal SUD, + proband depression, SUD, and suicidality → later BPD symptoms |
| Ha et al., 2014 [20] | Cross-sectional study; clinical population | 335 adolescent inpatients (aged 12–17 years), 33% with BPD | - | Adolescent inpatients with BPD → ↑rates of psychiatric comorbidity |
| Stepp, Whalen et al., 2014 [43] | Longitudinal cohort study; community population | 2,451 girls aged 14 -17 drawn from the Pittsburgh Girls Study | 3 years | Child impulsivity and negative affectivity, as well as caregiver psychopathology, were related to parenting trajectories, while only child characteristics predicted BPD trajectories. |
| Conway et al., 2015 [66] | Longitudinal study; community population | 700 at-risk youths (15–20 years old) | 5 years | Maternal externalizing disorders + offspring internalizing disorders + family stressors + school-related stressors → BPD risk |
| Sharp et al., 2015 [109] | Longitudinal study; community population | 730 adolescents | 1 year | Experiential avoidance → BPD features + levels of borderline symptoms at 1-year follow-up |
| Krabbendam et al., 2015 [139] | Longitudinal study; community population | 229 detained adolescent females (mean age = 15.5 years) | 6 years | Post-traumatic stress, depressive symptoms and dissociation during detention → ↑ risk for BPD in adulthood |
| Bo et al., 2017 [140] | Cross-sectional study; clinical population | 109 adolescent patients with consecutive referrals to psychiatric clinic (45 with BPD, 64 CCs) | - | BPD group → ↓ mentalizing abilities + ↑ problematic attachments to parents and peers + ↑ self-reported levels of psychopathology |
| Koenig et al., 2017 [141] | Cross-sectional study; clinical and community population | 77 adolescent psychiatric inpatients and 50 detainees | - | Lifetime self-injury behavior among adolescent psychiatric inpatients and detainees is associated with similar patterns of psychopathology and BPD |
| Bornovalova et al., 2018 [137] | Longitudinal study; community population | 1,763 female twins aged 14 to 24 | 10 years | ↑ levels of BPD traits → earlier onset and faster escalation of AUD and DUD → ↓ normative decline in BPD traits |
| Structured diagnostic interviews and self-report questionnaires | ||||
| Study | Study design | Sample | Trial duration | Outcomes |
| Zanarini et al., 2000 [142] | Cross-sectional study; clinical population | 12 master’s or doctoral-level raters | - | Axis II disorders can be diagnosed reliably when using appropriate semi-structured interviews |
| Samuel et al., 2013 [143] | Longitudinal study; clinical population | 320 patients in the Collaborative Longitudinal Personality Disorders Study diagnosed with PDs by therapist, self-report and semi-structured interview at baseline | 5 years | Self-report questionnaire and semi-structured interview PD diagnoses → > predictive validity vs. PD diagnoses assigned by a treating clinician |
| Morey et al., 2016 [136] | Cross-sectional study; clinical population | 337 clinicians and their target patients | - | Clinical diagnoses of PDs diverge from the rules designated in the DSM |
| Zimmerman et al., 2017 [144] | Cross-sectional study; clinical population | 3674 psychiatric outpatients | - | Affective instability criterion: sensitivity of 92.8% (> than other 8 BPD criteria) + negative predictive value of 99% |
| Fung et al., 2020 [145] | Cross-sectional study; clinical population | 828 subjects with web-based diagnosis of BPD | - | The web-based BPD measure could discriminate between participants with and without BPD |
| Laboratory and instrumental assessment | ||||
| Study | Study design | Sample | Trial duration | Outcomes |
| Chanen et al., 2008 [146] | Cross-sectional study; clinical and community population | 20 BPD patients and 20 HCs | - | BPD patients → right-sided OFC grey-matter loss; no significant differences in amygdala or hippocampal volumes |
| Whittle et al., 2009 [147] | Cross-sectional study; clinical and community population | 15 female BPD patients and 15 female HCs | - | ↓ volume of the left ACC in BPD patients → parasuicidal behavior, impulsivity and fear of abandonment |
| Brunner et al., 2010 [148] | Cross-sectional study; clinical and community population | 60 female right-handed individuals (aged 14–18 years): 20 with BPD, 20 CCs and 20 HCs | - | Early morphological changes in BPD are located in the PFC: reduced gray matter in the DLPFC bilaterally and in the left orbitofrontal cortex OFC |
| Walterfang et al., 2010 [149] | Cross-sectional study; clinical and community population | 20 teenaged first-presentation BPD patients and 20 HCs | - | Gross neuroanatomical changes in the callosum are not present in teenagers with first-presentation BPD |
| Goodman et al., 2011 [73] | Cross-sectional study; clinical and community population | 13 adolescent inpatients with co-morbid BPD and MDD and 13 HCs | - | ↓ BA24 volume → ↑ number of suicide attempts and BPD symptom severity but not depressive symptoms |
| Doering et al., 2012 [150] | Cross-sectional study; clinical and community population | 17 female BPD patients and 17 female HCs | - | Deactivation in the anterior and posterior cortical midline structures → ↓ personality functioning + ↓ identity integration |
| New et al., 2013 [151] | Cross-sectional study; clinical and community population | 38 BPD patients (14 adolescents, 24 adults) and 32 HCs (13 adolescents, 19 adults) | - | In early onset BPD, the normal developmental “peak” in fractional anisotropy in ILF is not achieved → possible neural substrate for the OFC-amygdala disconnection in adults with BPD |
| Maier-Hein et al., 2014 [152] | Cross-sectional study; clinical and community population | 20 adolescent patients with BPD (aged 14–18 years), 20 HCs, and 20 CCs | - | In BPD, white-matter alterations in pathways involved in emotion regulation + parts of the heteromodal association cortex related to emotion recognition |
| Jovev et al., 2014 [107] | Cross-sectional study; community population | 153 healthy adolescents (Mage = 12.6 years) | - | Boys: ↑/↓ affiliation + hippocampal asymmetry → ↑ BPD symptoms; girls: ↓ effortful control + hippocampal asymmetry → ↑ BPD symptoms. |
| Richter et al., 2014 [153] | Cross-sectional study; clinical and community population | 60 right-handed female adolescents between 14 and 18 years of age (20 patients with BPD, 20 CCs and 20 HCs) | - | In BPD, differences in the right and left hippocampus and in the right amygdala + ↓volume in frontal and parietal regions |
| Beeney et al., 2016 [154] | Cross-sectional study; clinical and community population | 8 right-handed females (17 with BPD, 21 HCs) aged 18–60. | - | In BPD, ↓ maintenance of self and other representations + ↑ activation in medial PFC, temporal parietal junction, regions of the frontal pole, precuneus and middle temporal gyrus (areas crucial for social cognition) |
| Bozzatello et al., 2019 [155] | Cross-sectional study; clinical and community population | 24 BPD patients and 24 HCs | - | Inefficient attempt to reconstruct a coherent narrative of life events → hyperactivity in ACC and DLPFC in BPD patients |
| Pop-Jordanova et al., 2019 [156] | Cross-sectional study; clinical and community population | 10 BPD patients (5 males and 5 females, mean age 20.4 years), 10 HCs (6 males and 4 females, mean age 24.2 years). | - | EEG characteristics in BPD without statistical differences, except in low bands (delta and theta) → lower frequencies and coherence |
| Arikan et al., 2019 [157] | Cross-sectional study; clinical and community population | 111 subjects (11 HCs, 25 BPD, 75 BD) | - | No significant differences in EEG characteristics between the two clinical groups |
| Differential diagnosis and comorbidities | ||||
| Study | Study design | Sample | Trial duration | Outcomes |
| Orbach et al., 2003 [158] | Cross-sectional study; clinical and community population | 32 suicidal inpatients (14 males, 18 females), 29 non-suicidal inpatients (11 males, 18 females), aged 25–60; 98 HCs (75 females and 23 males), aged 19–39 | - | Intense mental pain related to loss of life meaning and suicide |
| Gunderson et al., 2004 [159] | Longitudinal study; clinical population | 161 BPD patients, with and without co-occurring MDD | 3 years | Rate of remissions of BPD → not affected by co-occurring MDD; rate of MDD remissions → ↓ by co-occurring BPD |
| Eaton et al., 2011 [160] | Cross-sectional study; community population | 34,653 civilian, non-institutionalized individuals aged ≥18 years | - | Complex patterns of co-morbidity in BPD → connections to other disorders (latent internalizing and externalizing dimensions) |
| Hasin et al., 2011 [161] | Longitudinal study; clinical population | 1172 subjects with alcohol dependence, 454 with cannabis use disorder and 4017 with nicotine dependence, drawn from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) | 3 years | ASPD, BPD and STPD associated with persistent alcohol, cannabis and nicotine use disorders |
| Skodol et al., 2011 [162] | Longitudinal study; community population | 1,996 participants in a national survey | 3 years | APD, HPD, PPD, SPD, STPD and especially BPD → ↑ risk for MDD persistence |
| Gunderson et al., 2014 [163] | Longitudinal study; clinical population | 223 BPD patients with co-occurring MDD (n = 161), bipolar I disorder (n = 34) and bipolar II disorder (n = 28) | 10 years | BPD and MDD strongly related: ↑ time to remission and ↑ time to relapse; BPD and BD largely independent disorders, except BD II → ↑ BPD’s time to remission |
| Keuroghlian et al., 2015 [164] | Longitudinal study; clinical population | 164 BPD patients with co-occurring GAD (n = 42), panic disorder with agoraphobia (n = 39), panic disorder without agoraphobia (n = 36), social phobia (n = 48), OCD (n = 36) and PTSD (n = 88) | 10 years | BPD negatively affects the course of GAD, social phobia and PTSD; anxiety disorders have little effect on BPD course |
| Boritz et al., 2016 [165] | Randomized controlled trial | 180 BPD patients | 3 years | BPD + PTSD → ↑ levels of global psychological distress |
| Name (Abbreviation) | Personality Disorders Assessed | Characteristics | Validated for Adolescents |
|---|---|---|---|
| Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II) | All personality disorders | Items grouped by personality-disorder type | Yes |
| Diagnostic interview for DSM-IV Personality Disorders (DIPD-IV) | All personality disorders | Items grouped by personality-disorder type | |
| International Personality Disorders Examination (IPDE) | All personality disorders in DSM-IV and ICD-10 | Items grouped by topic (i.e., work, self, interpersonal, affect, reality testing, impulse control) | |
| Structured Interview for DSM-IV Personality Disorders (SIDP-IV) | All personality disorders | Items grouped by personality-disorder type or by topic | |
| Structured Clinical Interview for the DSM-5 Alternative Model for Personality Disorders Module III (SCID-5-AMPD) | BPD and five other personality disorders | Items grouped by personality-disorder type, based on DSM-5 AMPD | |
| Revised Diagnostic Interview for Borderlines (DIR-B) | BPD only | Items grouped by area of functioning (impulsivity, affect, cognition, interpersonal relationships) | |
| Childhood Interview for DSM-IV Borderline Personality Disorder (CI-BPD) | BPD only | Specifically designed for adolescents | Yes |
| Borderline Personality Disorder Severity Index-IV (BPDSI-IV) | BPD only | Dimensional, short-interval change measure, with adolescent and parent versions | Yes |
| Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD) | BPD only | Dimensional, short-interval change measures | |
| Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5) | BPD, antisocial personality disorder (ASPD) and schizotypal personality disorder (STPD) | Structured interview for lay-person administration used in the NESARC (National Epidemiologic Survey on Alcohol and Related Conditions) |
| Name (Abbreviation) | Personality Disorders Dssessed | Aim | Characteristics | Validated for Adolescents |
|---|---|---|---|---|
| Personality Diagnostic Questionnaire-4 (PDQ-4) | All personality disorders | Diagnosis | Includes questions on clinical significance | |
| Personality Assessment Inventory (PAI) | BPD and ASPD | Diagnosis | Assesses identity problems, negative relationships, affective instability and self-harm; has an adolescent version | Yes |
| Borderline Symptom List (BSL) | BPD | Diagnosis | Full and short version | |
| Five-Factor Borderline Inventory (FFBI) | BPD | Diagnosis | Based on the Five-Factor Model of personality traits | |
| Schedule for Nonadaptive and Adaptive Personality-II (SNAP-II) | All personality disorders and traits | Pathological personality traits assessment; can be scored for diagnosis | Distinguishes higher-order factors and lower-order traits | Yes |
| Dimensional Assessment of Personality Pathology-Basic Questionnaire (DAPP-BQ) | All personality disorders and traits | Pathological personality traits assessment | Assesses identity problems, insecure attachment, affective lability and self-harm | |
| Minnesota Multiphasic Personality Inventory-2-Restructured Form (MMPI-2-RF) | All personality disorders and traits | Pathological personality traits assessment | Dimensional | |
| Personality Inventory for DSM-5 (PID-5) | All personality disorders and traits | Pathological personality traits assessment | Based on the DSM-5 Alternative Model for Personality Disorders (AMPD) | |
| McLean Screening Instrument for BPD (MSI-BPD) | BPD | Screening | Ten items; translated into multiple languages; used in adults and adolescents | Yes |
| Borderline Personality Questionnaire (BPQ) | BPD | Screening | Used in adults and adolescents | Yes |
| Borderline Personality Features Scale for Children (BPFSC) | BPD | Screening | Dimensional scale designed to assess children and adolescents; has child and parent version | Yes |
| Severity Indices of Personality Problems (SIPP-118) | - | Impairment in personality functioning assessment | Includes five domains of personality functioning | |
| General Assessment of Personality Disorder (GAPD) | - | Impairment in personality functioning assessment | Assesses self or identity problems and interpersonal dysfunction | |
| Level of Personality Functioning Scale Self-Report (LPFS-SR) | - | Impairment in personality functioning assessment | Based on the DSM-5 AMPD |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bozzatello, P.; Garbarini, C.; Rocca, P.; Bellino, S. Borderline Personality Disorder: Risk Factors and Early Detection. Diagnostics 2021, 11, 2142. https://doi.org/10.3390/diagnostics11112142
Bozzatello P, Garbarini C, Rocca P, Bellino S. Borderline Personality Disorder: Risk Factors and Early Detection. Diagnostics. 2021; 11(11):2142. https://doi.org/10.3390/diagnostics11112142
Chicago/Turabian StyleBozzatello, Paola, Claudia Garbarini, Paola Rocca, and Silvio Bellino. 2021. "Borderline Personality Disorder: Risk Factors and Early Detection" Diagnostics 11, no. 11: 2142. https://doi.org/10.3390/diagnostics11112142
APA StyleBozzatello, P., Garbarini, C., Rocca, P., & Bellino, S. (2021). Borderline Personality Disorder: Risk Factors and Early Detection. Diagnostics, 11(11), 2142. https://doi.org/10.3390/diagnostics11112142







