Measuring HCC Tumor Size in MRI—The Sequence Matters!
Abstract
:1. Introduction
2. Materials and Methods
2.1. Material and Methods
2.2. Patient Study Group and Settings
2.3. Histopathologic Size Measurement
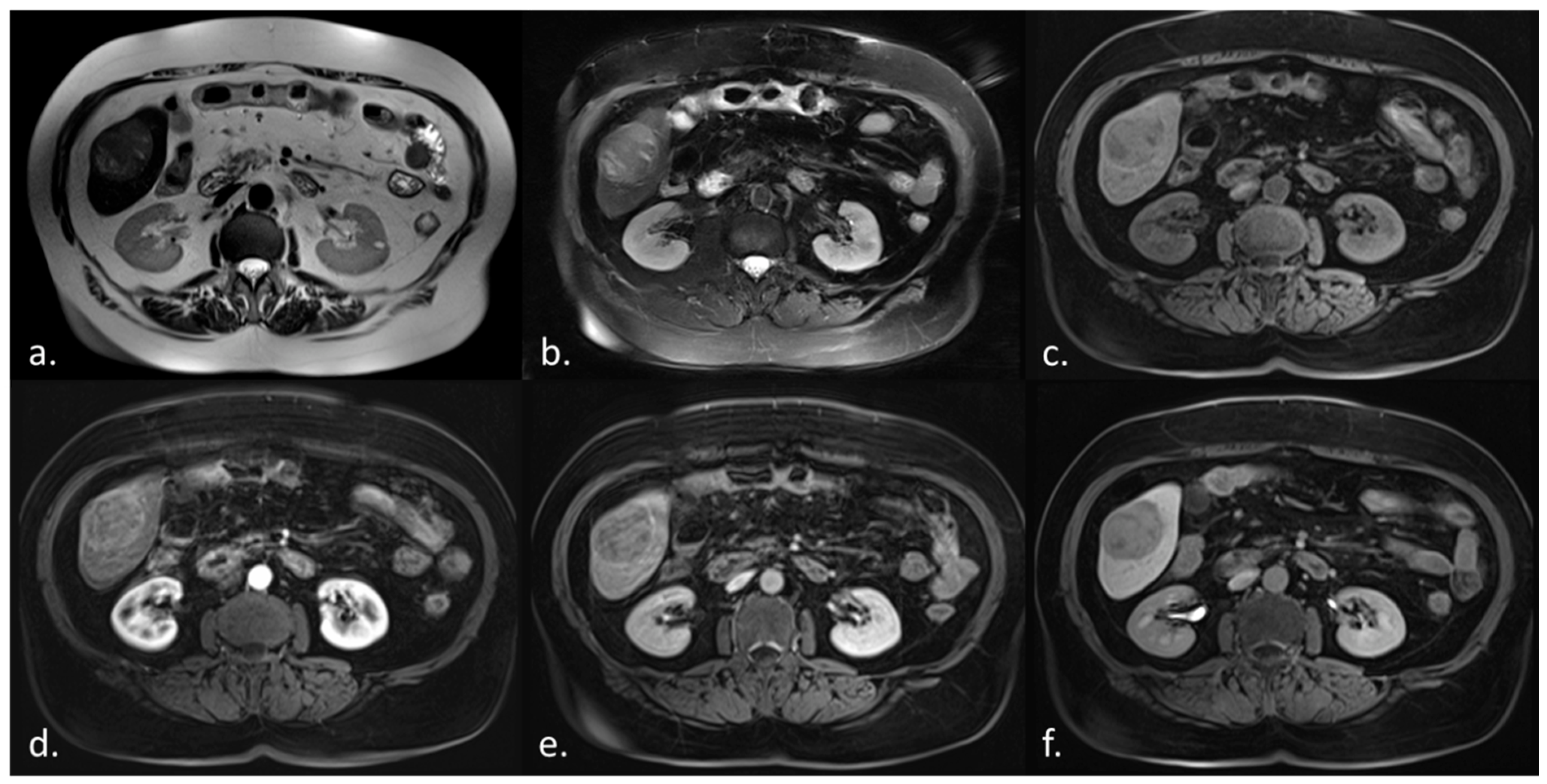
2.4. Magnetic Resonance Imaging (MRI)
2.5. Image Data Preparation
2.6. Lesion Measurements
2.7. Misclassification Regarding the Milan Criteria
2.8. Statistical Analysis
3. Results
3.1. HCC Visibility and Image Artifacts
3.2. Pearson Correlation and Absolute Error
3.3. Misclassification Regarding the Milan and OPTN/UNOS Criteria
3.4. Bland–Altman Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- El-Serag, H.B.; Davila, J.A.; Petersen, N.J.; McGlynn, K.A. The continuing increase in the incidence of hepatocellular carcinoma in the United States: An update. Ann. Intern. Med. 2003, 139, 817–823. [Google Scholar] [CrossRef]
- Jemal, A.; Bray, F.; Center, M.M.; Ferlay, J.; Ward, E.; Forman, D. Global cancer statistics. CA Cancer J. Clin. 2011, 61, 69–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellissimo, F.; Pinzone, M.R.; Cacopardo, B.; Nunnari, G. Diagnostic and therapeutic management of hepatocellular carcinoma. World J. Gastroenterol. 2015, 21, 12003–12021. [Google Scholar] [CrossRef]
- Ceausu, M.; Socea, B.; Serban, D.; Smarandache, C.G.; Predescu, D.; Bacalbasa, N.; Slavu, I.; Tulin, A.; Alecu, L.; Ceausu, Z. Heterogeneity of antigenic constellation in human hepatocellular carcinoma. Exp. Ther. Med. 2021, 21, 270. [Google Scholar] [CrossRef]
- Arslanoglu, A.; Seyal, A.R.; Sodagari, F.; Sahin, A.; Miller, F.H.; Salem, R.; Yaghmai, V. Current Guidelines for the Diagnosis and Management of Hepatocellular Carcinoma: A Comparative Review. AJR Am. J. Roentgenol. 2016, 207, W88–W98. [Google Scholar] [CrossRef] [PubMed]
- Elsayes, K.M.; Hooker, J.C.; Agrons, M.M.; Kielar, A.Z.; Tang, A.; Fowler, K.J.; Chernyak, V.; Bashir, M.R.; Kono, Y.; Do, R.K.; et al. 2017 Version of LI-RADS for CT and MR Imaging: An Update. Radiographics 2017, 37, 1994–2017. [Google Scholar] [CrossRef] [PubMed]
- Burk, K.S.; Singh, A.K.; Vagefi, P.A.; Sahani, D. Pretransplantation Imaging Workup of the Liver Donor and Recipient. Radiol. Clin. N. Am. 2016, 54, 185–197. [Google Scholar] [CrossRef]
- Kamath, P.S.; Wiesner, R.H.; Malinchoc, M.; Kremers, W.; Therneau, T.M.; Kosberg, C.L.; D’Amico, G.; Dickson, E.R.; Kim, W.R. A model to predict survival in patients with end-stage liver disease. Hepatology 2001, 33, 464–470. [Google Scholar] [CrossRef]
- Wald, C.; Russo, M.W.; Heimbach, J.K.; Hussain, H.K.; Pomfret, E.A.; Bruix, J. New OPTN/UNOS policy for liver transplant allocation: Standardization of liver imaging, diagnosis, classification, and reporting of hepatocellular carcinoma. Radiology 2013, 266, 376–382. [Google Scholar] [CrossRef] [Green Version]
- Mazzaferro, V.; Regalia, E.; Doci, R.; Andreola, S.; Pulvirenti, A.; Bozzetti, F.; Montalto, F.; Ammatuna, M.; Morabito, A.; Gennari, L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N. Engl. J. Med. 1996, 334, 693–699. [Google Scholar] [CrossRef]
- Mazzaferro, V.; Bhoori, S.; Sposito, C.; Bongini, M.; Langer, M.; Miceli, R.; Mariani, L. Milan criteria in liver transplantation for hepatocellular carcinoma: An evidence-based analysis of 15 years of experience. Liver Transpl. 2011, 17 (Suppl. 2), S44–S57. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver; European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: Management of hepatocellular carcinoma. Eur. J. Cancer 2012, 48, 599–641. [Google Scholar] [CrossRef]
- Bashir, M.R.; Hussain, H.K. Imaging in Patients with Cirrhosis: Current Evidence. Radiol. Clin. N. Am. 2015, 53, 919–931. [Google Scholar] [CrossRef]
- Bruix, J.; Sherman, M.; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: An update. Hepatology 2011, 53, 1020–1022. [Google Scholar] [CrossRef] [PubMed]
- Kudo, M.; Izumi, N.; Kokudo, N.; Matsui, O.; Sakamoto, M.; Nakashima, O.; Kojiro, M.; Makuuchi, M.; HCC Expert Panel of Japan Society of Hepatology. Management of hepatocellular carcinoma in Japan: Consensus-Based Clinical Practice Guidelines proposed by the Japan Society of Hepatology (JSH) 2010 updated version. Dig. Dis. 2011, 29, 339–364. [Google Scholar] [CrossRef] [PubMed]
- Neri, E.; Bali, M.A.; Ba-Ssalamah, A.; Boraschi, P.; Brancatelli, G.; Alves, F.C.; Grazioli, L.; Helmberger, T.; Lee, J.M.; Manfredi, R.; et al. ESGAR consensus statement on liver MR imaging and clinical use of liver-specific contrast agents. Eur. Radiol. 2016, 26, 921–931. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seuss, C.R.; Kim, M.J.; Triolo, M.J.; Hajdu, C.H.; Rosenkrantz, A.B. Comparison of MRI pulse sequences for prediction of size of hepatocellular carcinoma at explant evaluation. AJR Am. J. Roentgenol. 2014, 203, 300–305. [Google Scholar] [CrossRef]
- Choi, J.Y.; Lee, J.M.; Sirlin, C.B. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: Part II. Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology 2014, 273, 30–50. [Google Scholar] [CrossRef] [Green Version]
- Filippone, A.; Blakeborough, A.; Breuer, J.; Grazioli, L.; Gschwend, S.; Hammerstingl, R.; Heinz-Peer, G.; Kittner, T.; Laghi, A.; Leen, E.; et al. Enhancement of liver parenchyma after injection of hepatocyte-specific MRI contrast media: A comparison of gadoxetic acid and gadobenate dimeglumine. J. Magn. Reson. Imaging 2010, 31, 356–364. [Google Scholar] [CrossRef]
- Kim, A.Y.; Sinn, D.H.; Jeong, W.K.; Kim, Y.K.; Kang, T.W.; Ha, S.Y.; Park, C.K.; Choi, G.S.; Kim, J.M.; Kwon, C.H.D.; et al. Hepatobiliary MRI as novel selection criteria in liver transplantation for hepatocellular carcinoma. J. Hepatol. 2018, 68, 1144–1152. [Google Scholar] [CrossRef]
- Ricke, J.; Steffen, I.G.; Bargellini, I.; Berg, T.; Bilbao Jaureguizar, J.I.; Gebauer, B.; Iezzi, R.; Loewe, C.; Karcaaltincaba, M.; Pech, M.; et al. Gadoxetic acid-based hepatobiliary MRI in hepatocellular carcinoma. JHEP Rep. 2020, 2, 100173. [Google Scholar] [CrossRef]
- Sano, K.; Ichikawa, T.; Motosugi, U.; Sou, H.; Muhi, A.M.; Matsuda, M.; Nakano, M.; Sakamoto, M.; Nakazawa, T.; Asakawa, M.; et al. Imaging study of early hepatocellular carcinoma: Usefulness of gadoxetic acid-enhanced MR imaging. Radiology 2011, 261, 834–844. [Google Scholar] [CrossRef] [PubMed]
- Higaki, A.; Tamada, T.; Sone, T.; Kanki, A.; Sato, T.; Tanimoto, D.; Higashi, H.; Ito, K. Potential clinical factors affecting hepatobiliary enhancement at Gd-EOB-DTPA-enhanced MR imaging. Magn. Reson. Imaging 2012, 30, 689–693. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.Y.; Kim, Y.K.; Lee, M.W.; Park, M.J.; Hwang, J.; Lee, M.H.; Lee, J.W. Detection of hepatocellular carcinoma in gadoxetic acid-enhanced MRI and diffusion-weighted MRI with respect to the severity of liver cirrhosis. Acta Radiol. 2012, 53, 830–838. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Toyota, N.; Date, S.; Oda, S.; Namimoto, T.; Yamashita, Y.; Beppu, T.; Awai, K. Clinical significance of the transitional phase at gadoxetate disodium-enhanced hepatic MRI for the diagnosis of hepatocellular carcinoma: Preliminary results. J. Comput. Assist. Tomogr. 2011, 35, 723–727. [Google Scholar] [CrossRef]

| Characteristics | N |
|---|---|
| Sex | |
| Male | 36 |
| Female | 9 |
| Amount of HCC lesions | |
| Unifocal | 36 |
| Bifocal | 4 |
| Trifocal | 3 |
| Multifocal | 2 |
| Risk factors | |
| Cirrhosis | 16 |
| Early stage fibrosis | 9 |
| HCV | 8 |
| HBV | 5 |
| Hemochromatosis | 1 |
| Hepatic porphyria | 1 |
| Surgical procedure | |
| Right hemihepatectomy | 11 |
| Left hemihepatectomy | 1 |
| Extended right hemihepatectomy | 1 |
| Segment resection | 13 |
| Atypical resection | 3 |
| LT | 16 |
| Slice Thickness (mm) | Matrix | TE (ms) | TR (ms) | FA (°) | BW (Hz) | |
|---|---|---|---|---|---|---|
| T2 TSE | 6 | 270 × 320 | 105 | 2730 | 180 | 220 |
| T2 HASTE | 6 | 320 × 384 | 78 | 800 | 180 | 390 |
| T1 VIBE * | 3 | 230 × 256 | 1.35 | 3.44 | 15 | 455 |
| Sequence | Percentage of HCCs Visible | Percentage of Lesions with Fuzzy Circumscription | Percentage of Artifacts with Each Sequence |
|---|---|---|---|
| T2w HASTE | 37/41 (90%) | 16/41 (43%) | 1/41 (2%) |
| T2w TSE | 40/42 (95%) | 15/42 (38%) | 4/42 (10%) |
| T1w precontrast | 42/44 (95%) | 9/44 (21%) | 0/44 (0%) |
| Arterial phase | 44/44 (100%) | 23/44 (52%) | 2/44 (5%) |
| Portal venous phase | 43/45 (96%) | 19/45 (44%) | 3/45 (7%) |
| Venous phase | 44/44 (100%) | 21/45 (47%) | 1/44 (2%) |
| Hepatobiliary phase | 41/41 (100%) | 6/41 (15%) | 0/41 (0%) |
| Sequence | Mean ± SD (cm) | 95% CI (cm) | Range (cm) | r |
|---|---|---|---|---|
| T2w HASTE | 0.83 ± 0.81 | 0.57–1.09 | 0.1–3.3 | 0.94 |
| T2w TSE | 0.87 ± 0.82 | 0.62–1.13 | 0.0–3.7 | 0.94 |
| T1w precontrast | 0.79 ± 0.77 | 0.56–1.02 | 0.0–3.2 | 0.95 |
| Arterial phase | 0.81 ± 0.92 | 0.55–1.08 | 0.0–3.8 | 0.94 |
| Portal venous phase | 0.82 ± 0.85 | 0.57–1.07 | 0.0–3.5 | 0.94 |
| Venous phase | 0.78 ± 0.84 | 0.53–1.03 | 0.0–3.5 | 0.95 |
| Hepatobiliary phase | 0.75 ± 0.75 | 0.52–0.97 | 0.0–3.3 | 0.96 |
| Category | T2w HASTE | T2w TSE | T1w VIBE Pre-Contrast | T1w VIBE Arterial | T1w VIBE pv | T1w VIBE Venous | T1w VIBE HPB |
|---|---|---|---|---|---|---|---|
| Pathologically inside Milan Criteria | |||||||
| Unifocal ≤ 5 cm (8) | 1 | 2 | 1 | 2 | 2 | 2 | 1 |
| Up to three ≤ 3 cm (1) | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Pathologically outside of Milan Criteria | |||||||
| At least one > 5 cm (25) | 1 | 2 | 2 | 1 | 2 | 1 | 1 |
| Bi-/Trifocal > 3 cm (1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 8.6% (3) | 14.3% (5) | 11.4% (4) | 11.4% (4) | 14.3% (5) | 11.4% (4) | 8.6% (3) |
| Sequence | Mean Difference (cm) | 95% Limits of Agreement (cm) | Range (cm) |
|---|---|---|---|
| 95% CI | |||
| T2w HASTE | −0.13 | −2.45 to 2.19 | 2.30 to 14.20 |
| −0.52 to 0.27 | |||
| T2w TSE | +0.20 | −2.06 to 2.45 | 1.20 to 15.20 |
| −0.17 to 0.56 | |||
| T1w precontrast | +0.11 | −2.02 to 2.25 | 1.50 to 14.10 |
| −0.22 to 0.45 | |||
| Arterial phase | +0.41 | −2.37 to 2.45 | 1.6 to 14.0 |
| −0.33 to 0.41 | |||
| Portal venous phase | +0.10 | −2.16 to 2.36 | 1.50 to 14.20 |
| −0.25 to 0.46 | |||
| Venous phase | +0.22 | −1.92 to 2.35 | 1.60 to 13.80 |
| −0.11 to 0.55 | |||
| Hepatobiliary phase | +0.12 | −1.84 to 2.09 | 1.50 to 14.00 |
| −0.19 to 0.44 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Armbruster, M.; Guba, M.; Andrassy, J.; Rentsch, M.; Schwarze, V.; Rübenthaler, J.; Knösel, T.; Ricke, J.; Kramer, H. Measuring HCC Tumor Size in MRI—The Sequence Matters! Diagnostics 2021, 11, 2002. https://doi.org/10.3390/diagnostics11112002
Armbruster M, Guba M, Andrassy J, Rentsch M, Schwarze V, Rübenthaler J, Knösel T, Ricke J, Kramer H. Measuring HCC Tumor Size in MRI—The Sequence Matters! Diagnostics. 2021; 11(11):2002. https://doi.org/10.3390/diagnostics11112002
Chicago/Turabian StyleArmbruster, Marco, Markus Guba, Joachim Andrassy, Markus Rentsch, Vincent Schwarze, Johannes Rübenthaler, Thomas Knösel, Jens Ricke, and Harald Kramer. 2021. "Measuring HCC Tumor Size in MRI—The Sequence Matters!" Diagnostics 11, no. 11: 2002. https://doi.org/10.3390/diagnostics11112002
APA StyleArmbruster, M., Guba, M., Andrassy, J., Rentsch, M., Schwarze, V., Rübenthaler, J., Knösel, T., Ricke, J., & Kramer, H. (2021). Measuring HCC Tumor Size in MRI—The Sequence Matters! Diagnostics, 11(11), 2002. https://doi.org/10.3390/diagnostics11112002






