Prediction of Atrial Fibrillation Recurrence after Thoracoscopic Surgical Ablation Using Machine Learning Techniques
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Characteristics
2.2. Procedure and Outcome
- Outcome 1: any episode of atrial tachyarrhythmia (AF, atrial flutter, atrial tachycardia) lasting > 30 s [10].
- Outcome 2: any episode of AF (but not atrial flutter or atrial tachycardia) lasting > 30 s.
- Outcome 3: one single episode of any atrial tachyarrhythmia lasting > 1 h.
- Outcome 4: one single episode of any atrial tachyarrhythmia lasting > 6 h.
- Outcome 5: one single episode of AF (but not atrial flutter or atrial tachycardia), lasting > 1 h.
2.3. Missing Data
2.4. Machine Learning Algorithms
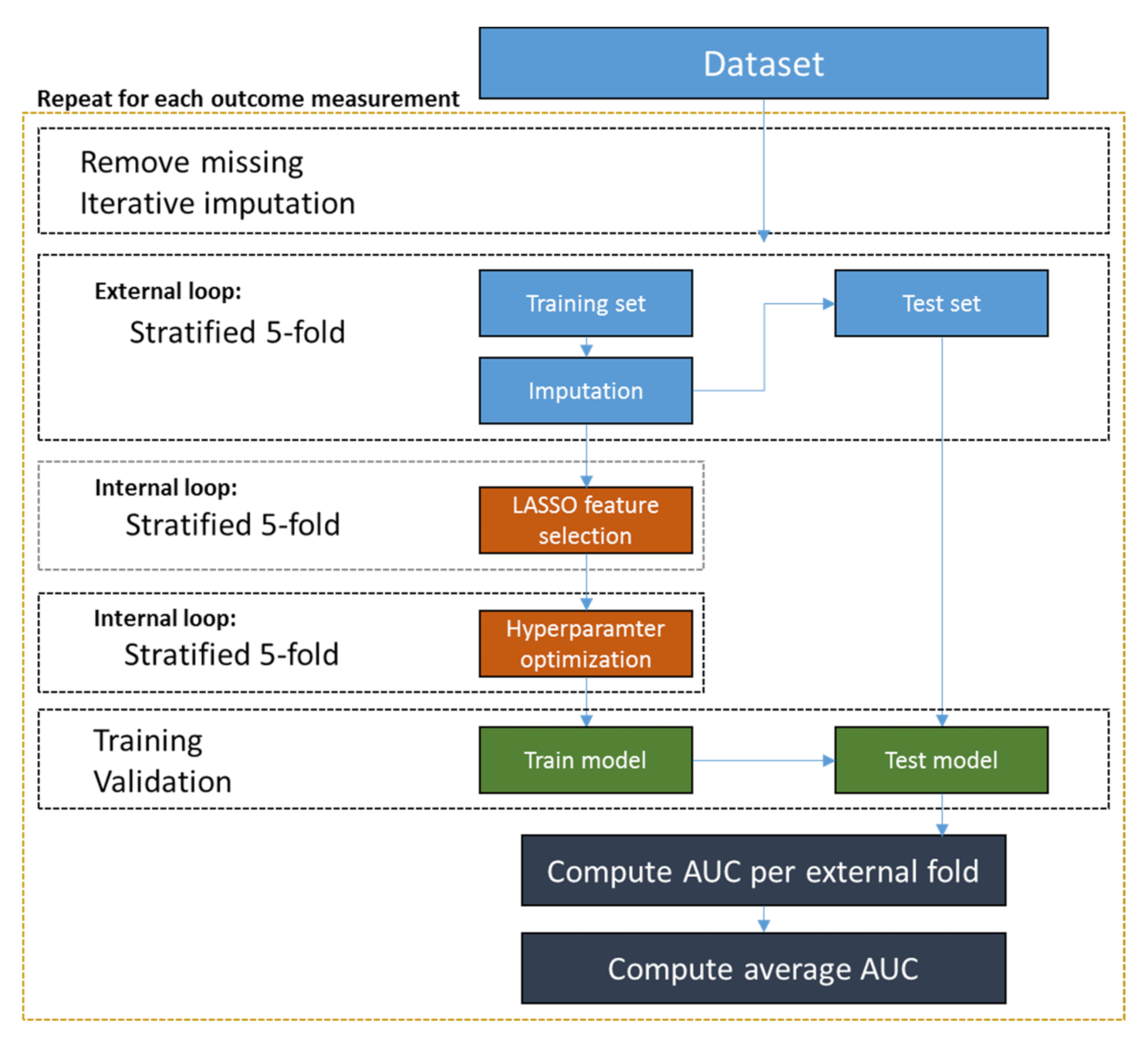
2.5. Analysis Pipeline and Variable Selection
2.6. Model Evaluation
2.7. Subgroup Analysis
2.8. Model Interpretation
2.9. Statistical Analysis
3. Results
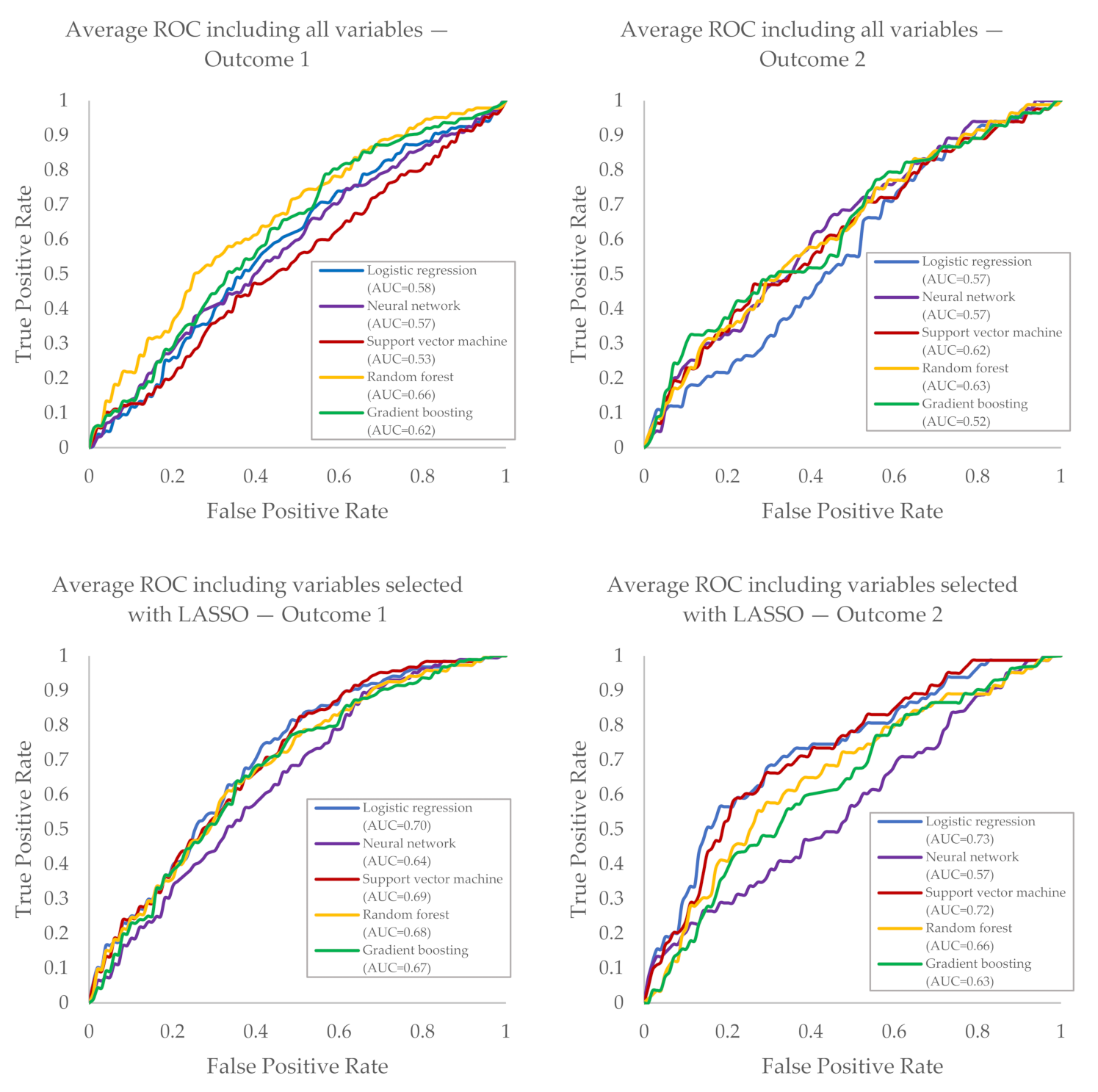
3.1. Prediction of AF Recurrence within Two Years after SA
3.1.1. Outcome 1
3.1.2. Outcomes 2–5
3.2. Variable Selection
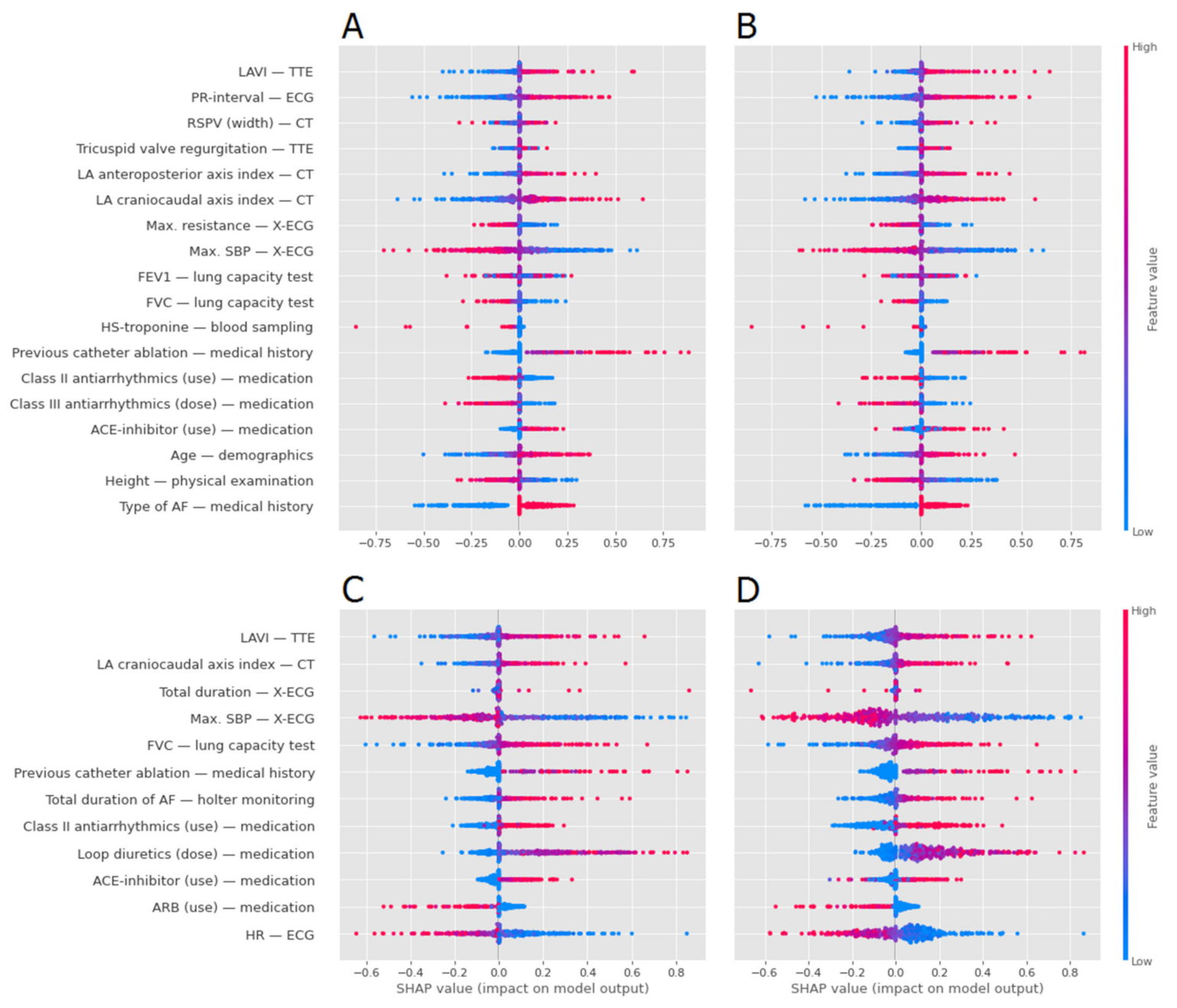
3.3. Model Interpretation Analysis
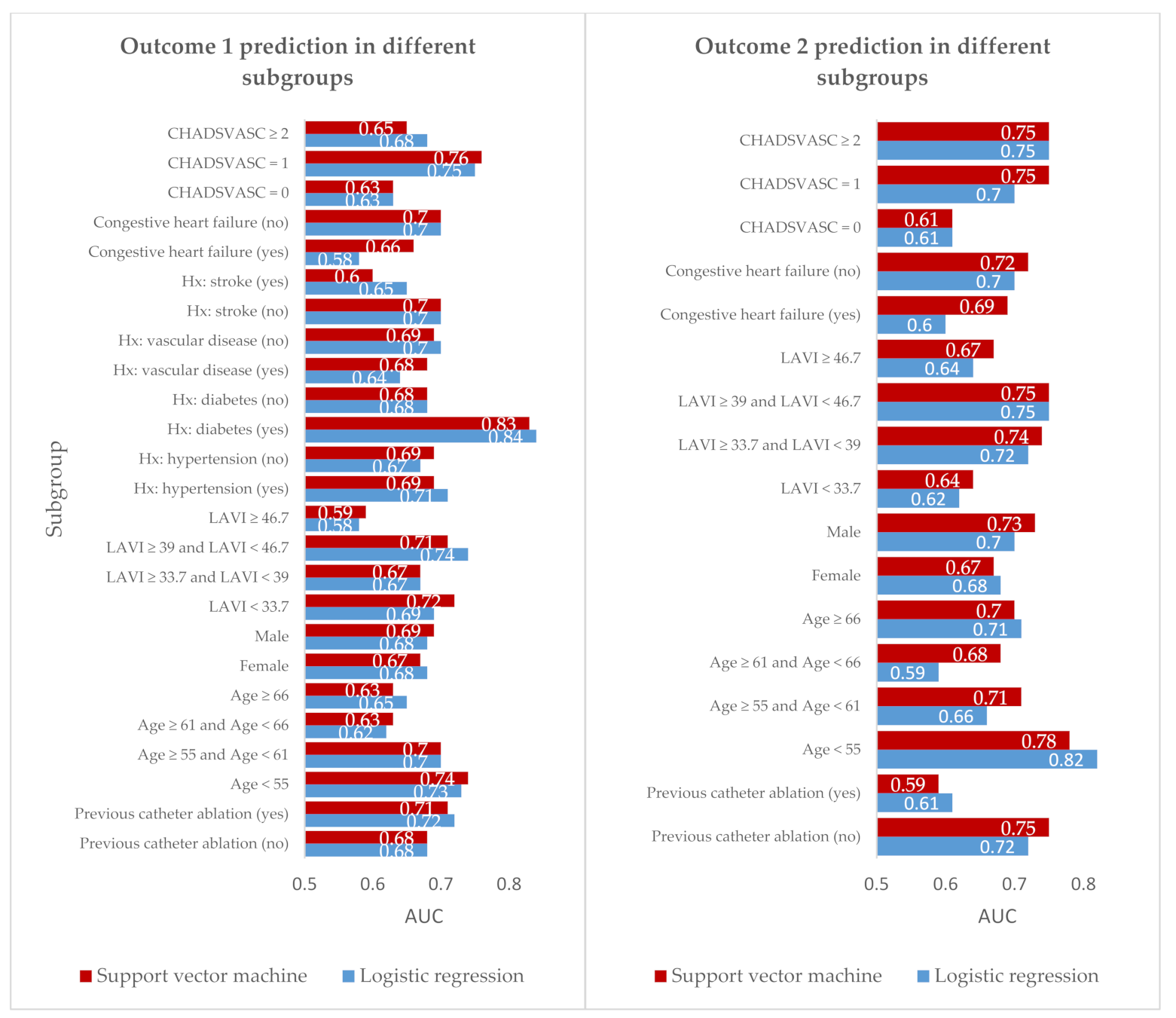
3.4. Analysis of AF Recurrence Prediction in Subgroups
4. Discussion
4.1. Prediction of AF Recurrence after Thoracoscopic Surgery
4.2. AF Recurrence Definition and Measurement
4.3. Additional Value of ML Techniques in the Prediction of AF Recurrence
4.4. Clinical Implications
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boersma, L.V.A.; Castella, M.; Boven, W.V.; Berruezo, A.; Yilmaz, A.; Nadal, M.; Sandoval, E.; Calvo, N.; Brugada, J.; Kelder, J.; et al. Atrial Fibrillation Catheter Ablation Versus Surgical Ablation Treatment (FAST). Circulation 2012, 125, 23–30. [Google Scholar] [CrossRef]
- Driessen, A.H.G.; Berger, W.R.; Krul, S.P.J.; van den Berg, N.W.E.; Neefs, J.; Piersma, F.R.; Chan Pin Yin, D.; de Jong, J.; van Boven, W.P.; de Groot, J.R. Ganglion Plexus Ablation in Advanced Atrial Fibrillation: The AFACT Study. J. Am. Coll. Cardiol. 2016, 68, 1155–1165. [Google Scholar] [CrossRef]
- Dretzke, J.; Chuchu, N.; Agarwal, R.; Herd, C.; Chua, W.; Fabritz, L.; Bayliss, S.; Kotecha, D.; Deeks, J.J.; Kirchhof, P.; et al. Predicting recurrent atrial fibrillation after catheter ablation: A systematic review of prognostic models. EP Eur. 2020, 22, 748–760. [Google Scholar] [CrossRef]
- Suzuki, S.; Yamashita, T.; Sakama, T.; Arita, T.; Yagi, N.; Otsuka, T.; Semba, H.; Kano, H.; Matsuno, S.; Kato, Y.; et al. Comparison of risk models for mortality and cardiovascular events between machine learning and conventional logistic regression analysis. PLoS ONE 2019, 14, e0221911. [Google Scholar] [CrossRef]
- Rizwan, A.; Zoha, A.; Mabrouk, I.B.; Sabbour, H.M.; Al-Sumaiti, A.S.; Alomainy, A.; Imran, M.A.; Abbasi, Q.H. A review on the state of the art in atrial fibrillation detection enabled by machine learning. IEEE Rev. Biomed. Eng. 2020, 14, 219–239. [Google Scholar] [CrossRef] [Green Version]
- Lopes, R.R.; van Mourik, M.S.; Schaft, E.V.; Ramos, L.A.; Baan, J.; Jr Vendrik, J.; de Mol, B.; Vis, M.M.; Marquering, H.A. Value of machine learning in predicting TAVI outcomes. Neth Heart J. 2019, 27, 443–450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, L.Y.W.; Ho, K.; Tam, R.C.; Hawkins, N.M.; Lim, M.; Andrade, J.G. Predicting Catheter Ablation Outcomes with Pre-ablation Heart Rhythm Data: Less Is More. Mach. Learn. Med Imaging 2020, 563–571. [Google Scholar]
- Krul, S.P.; Driessen, A.H.; van Boven, W.J.; Linnenbank, A.C.; Geuzebroek, G.S.; Jackman, W.M.; Wilde, A.A.; de Bakker, J.M.; de Groot, J.R. Thoracoscopic video-assisted pulmonary vein antrum isolation, ganglionated plexus ablation, and periprocedural confirmation of ablation lesions: First results of a hybrid surgical-electrophysiological approach for atrial fibrillation. Circ Arrhythm Electrophysiol. 2011, 4, 262–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Groot, J.R.; Driessen, A.H.; Van Boven, W.J.; Krul, S.P.; Linnenbank, A.C.; Jackman, W.M.; De Bakker, J.M. Epicardial confirmation of conduction block during thoracoscopic surgery for atrial fibrillation--a hybrid surgical-electrophysiological approach. Minim Invasive Ther. Allied Technol. 2012, 21, 293–301. [Google Scholar] [CrossRef]
- Calkins, H.; Hindricks, G.; Cappato, R.; Kim, Y.H.; Saad, E.B.; Aguinaga, L.; Akar, J.G.; Badhwar, V.; Brugada, J.; Camm, J.; et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017, 14, e275–e444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stekhoven, D.J.; Bühlmann, P. MissForest—Non-parametric missing value imputation for mixed-type data. Bioinformatics 2011, 28, 112–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-learn: Machine learning in Python. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- Tibshirani, R. Regression Shrinkage and Selection via the Lasso. J. R. Stat. Soc. Ser. B 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Cai, J.; Luo, J.; Wang, S.; Yang, S. Feature selection in machine learning: A new perspective. Neurocomputing 2018, 300, 70–79. [Google Scholar] [CrossRef]
- Njoku, A.; Kannabhiran, M.; Arora, R.; Reddy, P.; Gopinathannair, R.; Lakkireddy, D.; Dominic, P. Left atrial volume predicts atrial fibrillation recurrence after radiofrequency ablation: A meta-analysis. Europace 2018, 20, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef]
- Lundberg, S.M.; Lee, S.I. A unified approach to interpreting model predictions. Neural Inf. Process. Syst. 2017, 4768–4777. [Google Scholar]
- Van Gelder, I.C.; Healey, J.S.; Crijns, H.J.G.M.; Wang, J.; Hohnloser, S.H.; Gold, M.R.; Capucci, A.; Lau, C.-P.; Morillo, C.A.; Hobbelt, A.H.; et al. Duration of device-detected subclinical atrial fibrillation and occurrence of stroke in ASSERT. Eur. Heart J. 2017, 38, 1339–1344. [Google Scholar] [CrossRef]
- Bulava, A.; Mokracek, A.; Hanis, J.; Kurfirst, V.; Eisenberger, M.; Pesl, L. Sequential hybrid procedure for persistent atrial fibrillation. J. Am. Heart Assoc. 2015, 4, e001754. [Google Scholar] [CrossRef] [Green Version]
- Kron, J.; Kasirajan, V.; Wood, M.A.; Kowalski, M.; Han, F.T.; Ellenbogen, K.A. Management of Recurrent Atrial Arrhythmias after Minimally Invasive Surgical Pulmonary Vein Isolation and Ganglionic Plexi Ablation for Atrial Fibrillation. Heart Rhythm Off. J. Heart Rhythm Soc. 2010, 7, 445–451. [Google Scholar] [CrossRef]
- Driessen, A.H.; Berger, W.R.; Chan Pin Yin, D.R.; Piersma, F.R.; Neefs, J.; van den Berg, N.W.; Krul, S.P.; van Boven, W.P.; de Groot, J.R. Electrophysiologically Guided Thoracoscopic Surgery for Advanced Atrial Fibrillation: 5-Year Follow-up. J. Am. Coll. Cardiol. 2017, 69, 1753–1754. [Google Scholar] [CrossRef]
| Variable | No. of Patients (%) | |
|---|---|---|
| n | 446 | |
| Sex, n (%) | ||
| Male | 335 (75.1) | |
| Female | 111 (24.9) | |
| BMI, mean (SD) | 25.8 (7.5) | |
| Age, mean (SD) | 60.0 (8.7) | |
| CHA2DS2-VASc, n (%) | ||
| 0 | 122 (27.4) | |
| 1 | 141 (31.6) | |
| ≥2 | 183 (41.0) | |
| AF type, n (%) | ||
| Paroxysmal | 180 (40.4) | |
| Persistent | 266 (59.6) | |
| Models, AUCs (95% CI) | Logistic Regression | Neural Network | Support Vector Machine | Random Forest | Gradient Boosting |
|---|---|---|---|---|---|
| Outcome 1 | 0.58 (0.54–0.61) | 0.57 (0.44–0.71) | 0.53 (0.38–0.68) | 0.66 (0.59–0.72) | 0.62 (0.55–0.68) |
| Outcome 1 with LASSO | 0.70 (0.62–0.78) | 0.64 (0.61–0.67) | 0.69 (0.66–0.73) | 0.68 (0.63–0.73) | 0.67 (0.65–0.69) |
| Outcome 2 | 0.57 (0.50–0.64) | 0.57 (0.50–0.64) | 0.62 (0.55–0.70) | 0.63 (0.57–0.69) | 0.52 (0.48–0.57) |
| Outcome 2 with LASSO | 0.73 (0.68–0.77) | 0.57 (0.50–0.64) | 0.72 (0.66–0.78) | 0.66 (0.55–0.76) | 0.63 (0.54–0.72) |
| Outcome 3 | 0.54 (0.48–0.60) | 0.54 (0.42–0.65) | 0.56 (0.47–0.65) | 0.67 (0.61–0.72) | 0.68 (0.59–0.76) |
| Outcome 3 with LASSO | 0.69 (0.65–0.74) | 0.68 (0.62–0.74) | 0.67 (0.63–0.71) | 0.69 (0.64–0.75) | 0.67 (0.56–0.78) |
| Outcome 4 | 0.56 (0.48–0.63) | 0.61 (0.57–0.64) | 0.56 (0.43–0.69) | 0.63 (0.55–0.72) | 0.64 (0.52–0.75) |
| Outcome 4 with LASSO | 0.68 (0.59–0.77) | 0.62 (0.52–0.73) | 0.66 (0.58–0.74) | 0.67 (0.58–0.76) | 0.65 (0.56–0.73) |
| Outcome 5 | 0.56 (0.51–0.62) | 0.54 (0.37–0.70) | 0.55 (0.42–0.67) | 0.55 (0.51–0.59) | 0.51 (0.43–0.59) |
| Outcome 5 with LASSO | 0.69 (0.60–0.78) | 0.55 (0.35–0.75) | 0.66 (0.57–0.75) | 0.67 (0.61–0.73) | 0.63 (0.58–0.68) |
| Outcome 1 | Outcome 2 | ||
|---|---|---|---|
| Variable—Assessment at Baseline | Selection | Variable | Selection |
| LAVI—TTE | 100% | Max. SBP—X-ECG | 100% |
| PR-interval—ECG | 100% | ACE-inhibitor (use)—medication | 100% |
| LA craniocaudal axis index—CT | 100% | ARB (use)—medication | 80% |
| Max. SBP—X-ECG | 100% | LAVI—TTE | 60% |
| ACE-inhibitor (use)—medication | 100% | Total duration—X-ECG | 60% |
| Age—demographics | 100% | FVC—lung capacity test | 60% |
| LA anteroposterior axis index—CT | 80% | Class II antiarrhythmics (use)—medication | 60% |
| Max. resistance—X-ECG | 80% | Loop diuretics (dose)—medication | 60% |
| Previous catheter ablation—medical history | 80% | HR—ECG | 60% |
| RSPV (width)—CT | 60% | LA craniocaudal axis index—CT | 40% |
| FEV1—lung capacity test | 60% | Previous catheter ablation—medical history | 40% |
| Height—physical examination | 60% | Total duration of AF — Holter monitoring | 40% |
| Type of AF—medical history | 60% | ||
| Tricuspid valve regurgitation—TTE | 40% | ||
| FVC—lung capacity test | 40% | ||
| Hs-troponine—blood sampling | 40% | ||
| Class II antiarrhythmics (use)—medication | 40% | ||
| Class III antiarrhythmics (dose)—medication | 40% | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baalman, S.W.E.; Lopes, R.R.; Ramos, L.A.; Neefs, J.; Driessen, A.H.G.; van Boven, W.P.; de Mol, B.A.J.M.; Marquering, H.A.; de Groot, J.R. Prediction of Atrial Fibrillation Recurrence after Thoracoscopic Surgical Ablation Using Machine Learning Techniques. Diagnostics 2021, 11, 1787. https://doi.org/10.3390/diagnostics11101787
Baalman SWE, Lopes RR, Ramos LA, Neefs J, Driessen AHG, van Boven WP, de Mol BAJM, Marquering HA, de Groot JR. Prediction of Atrial Fibrillation Recurrence after Thoracoscopic Surgical Ablation Using Machine Learning Techniques. Diagnostics. 2021; 11(10):1787. https://doi.org/10.3390/diagnostics11101787
Chicago/Turabian StyleBaalman, Sarah W. E., Ricardo R. Lopes, Lucas A. Ramos, Jolien Neefs, Antoine H. G. Driessen, WimJan P. van Boven, Bas A. J. M. de Mol, Henk A. Marquering, and Joris R. de Groot. 2021. "Prediction of Atrial Fibrillation Recurrence after Thoracoscopic Surgical Ablation Using Machine Learning Techniques" Diagnostics 11, no. 10: 1787. https://doi.org/10.3390/diagnostics11101787
APA StyleBaalman, S. W. E., Lopes, R. R., Ramos, L. A., Neefs, J., Driessen, A. H. G., van Boven, W. P., de Mol, B. A. J. M., Marquering, H. A., & de Groot, J. R. (2021). Prediction of Atrial Fibrillation Recurrence after Thoracoscopic Surgical Ablation Using Machine Learning Techniques. Diagnostics, 11(10), 1787. https://doi.org/10.3390/diagnostics11101787







