Magnetic Resonance Accuracy in the Diagnosis of Anterior Talo-Fibular Ligament Acute Injury: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
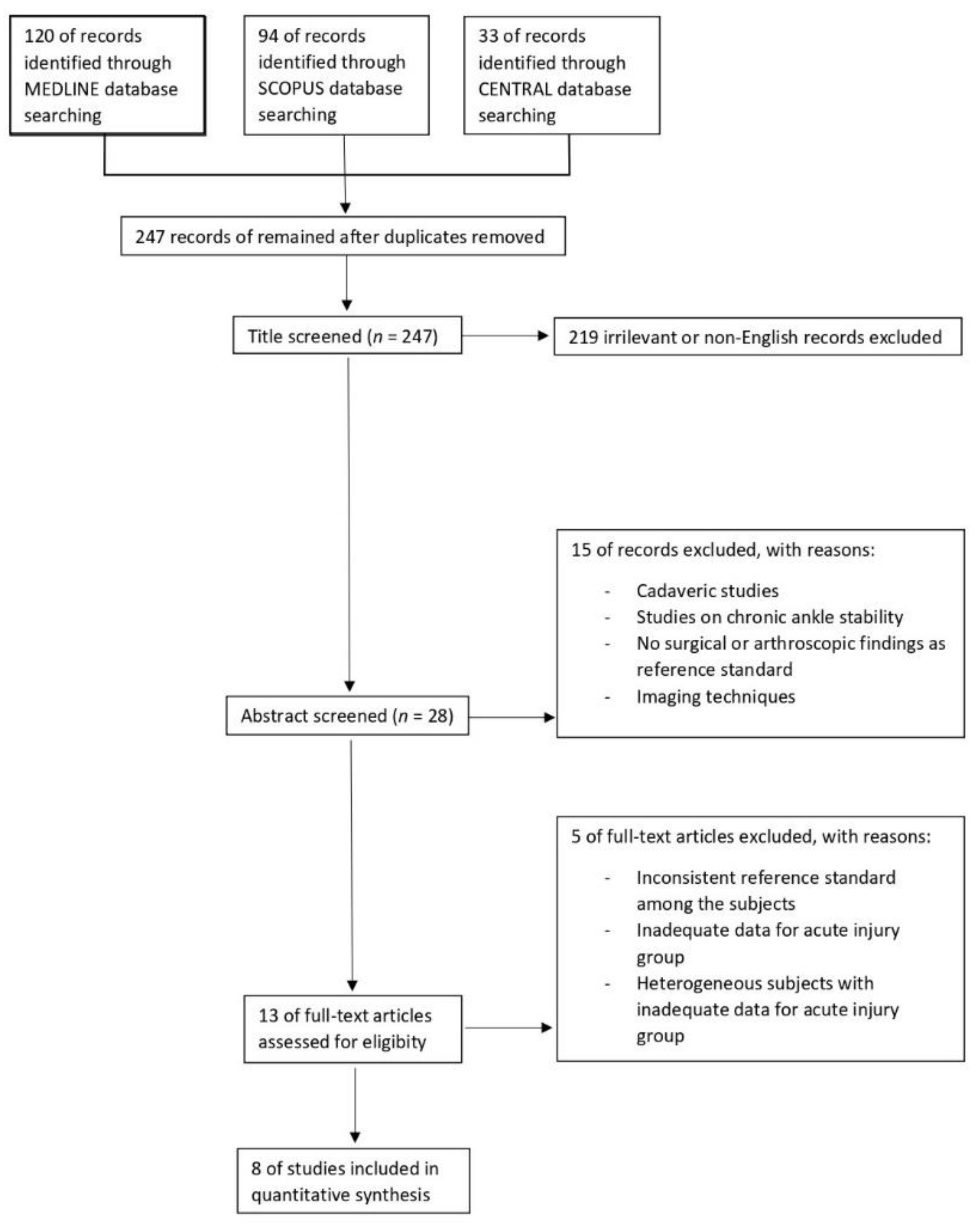
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Search Strategy
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Description of the Included Studies
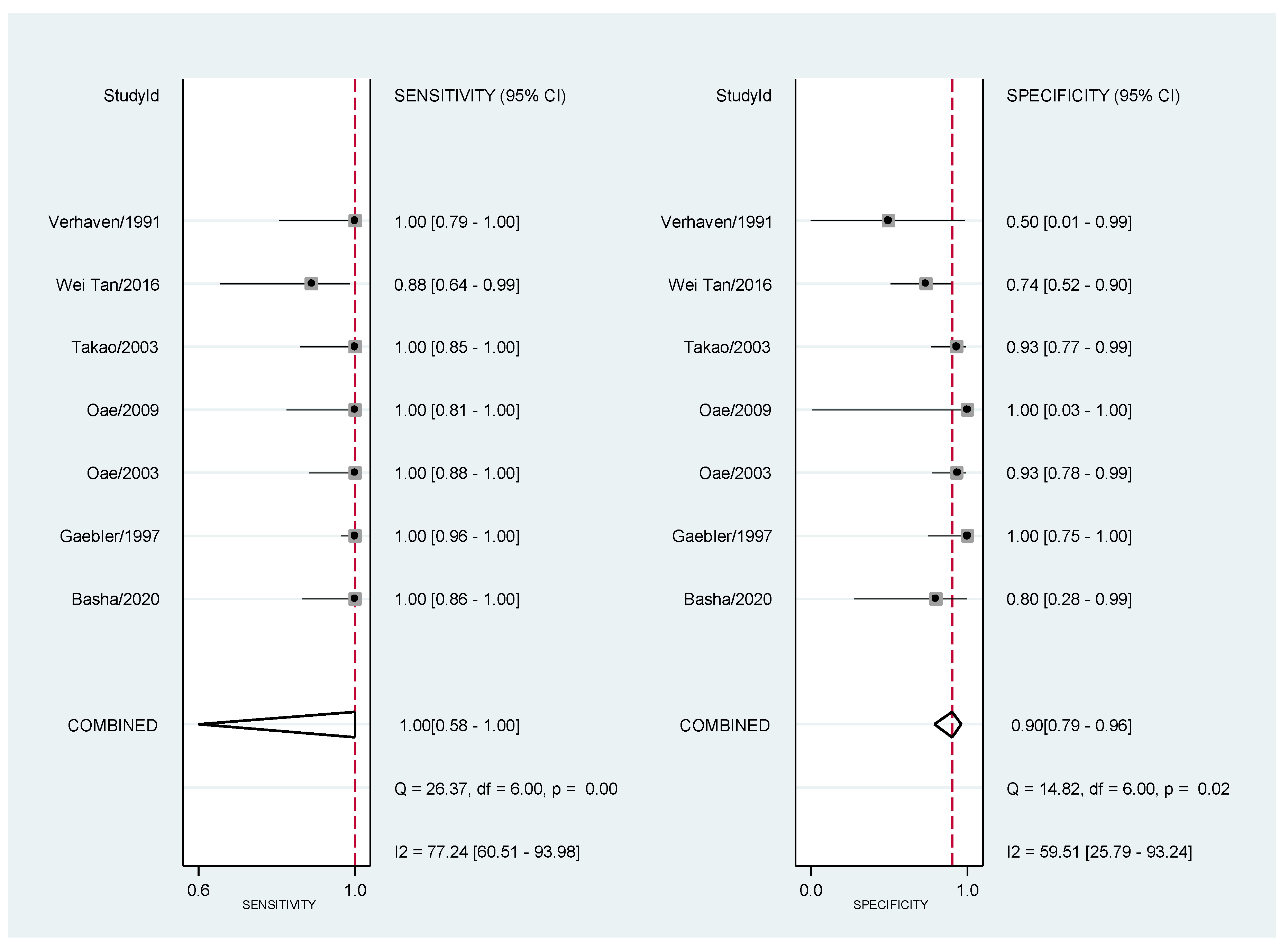
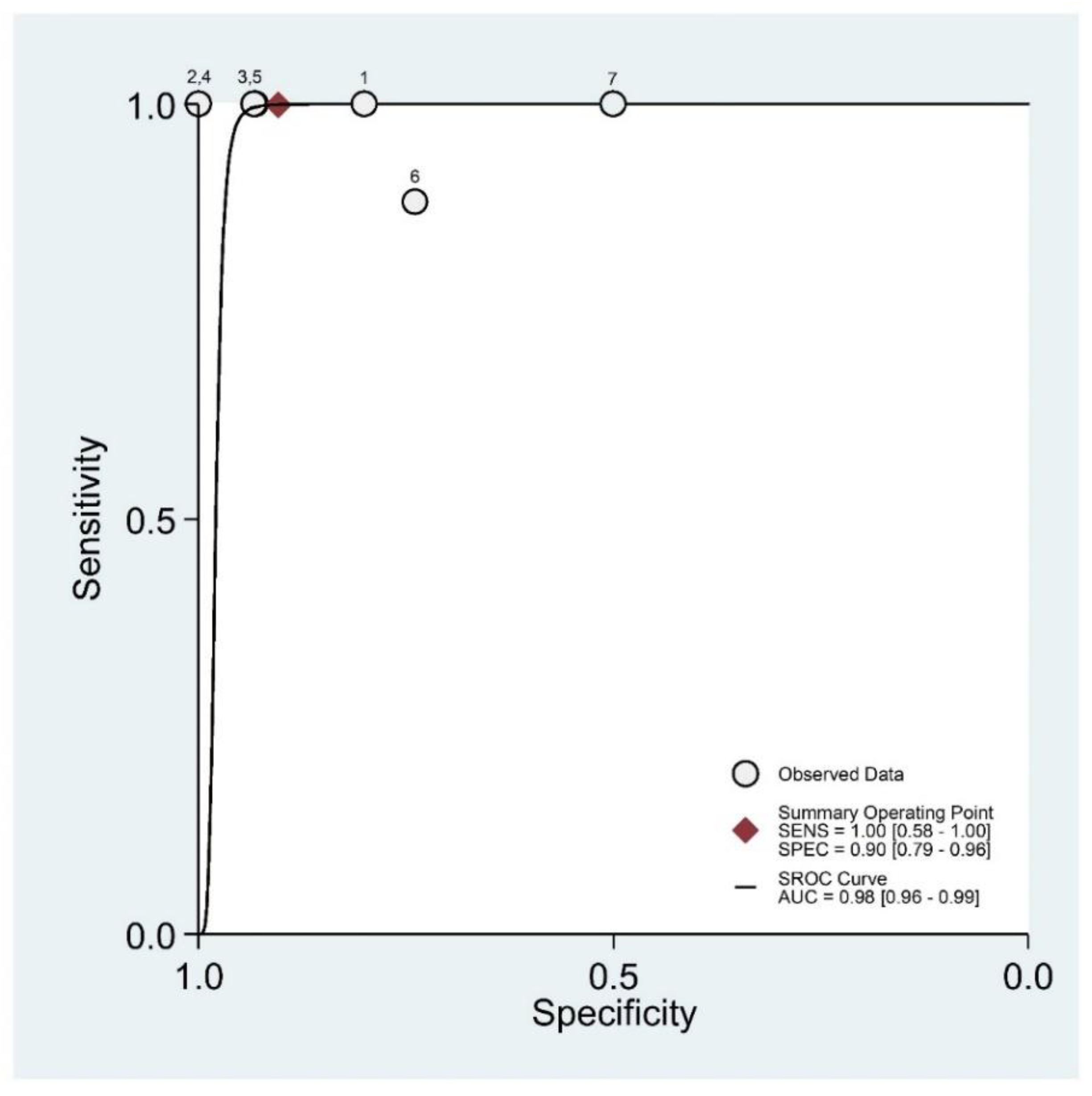
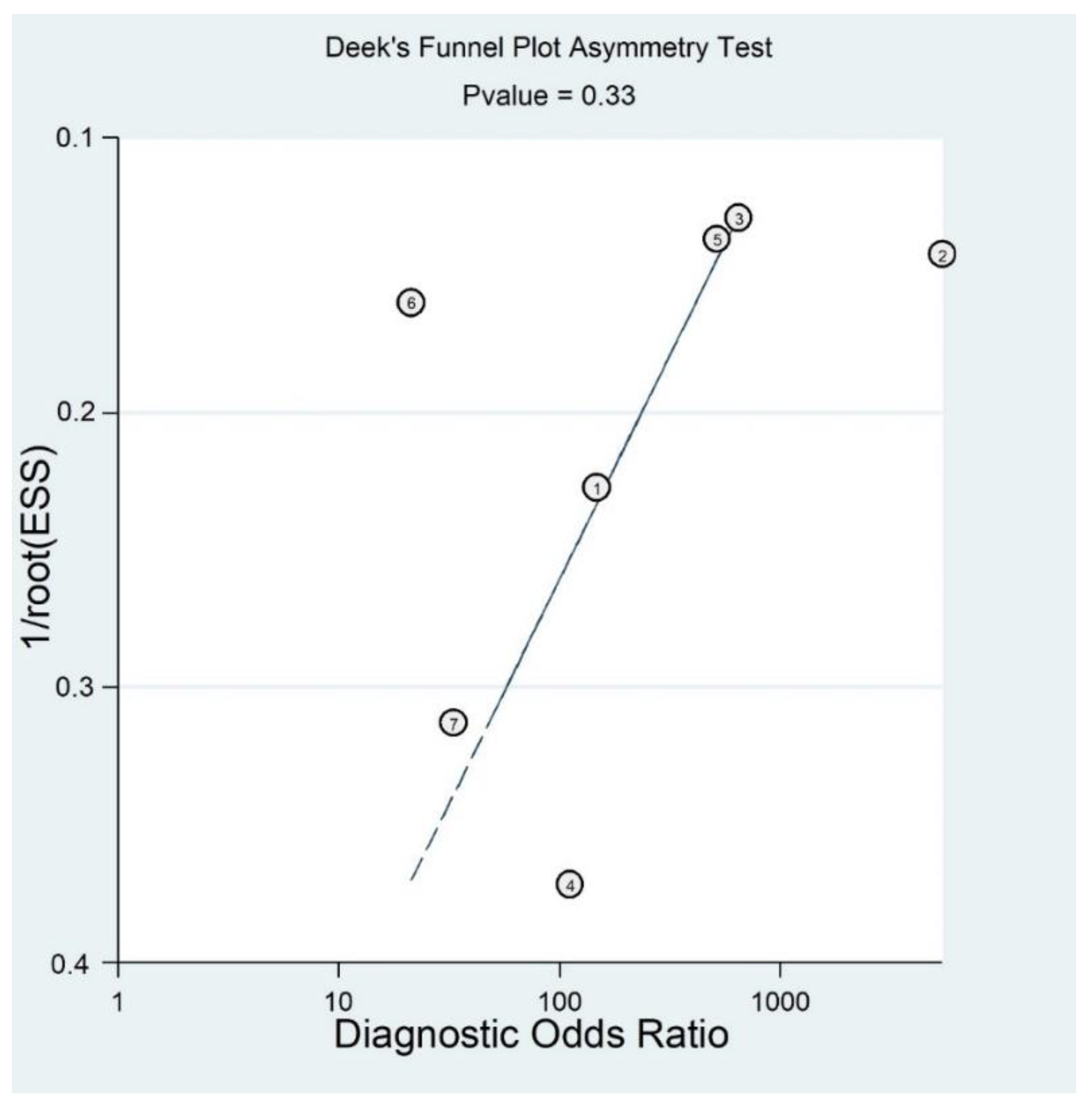
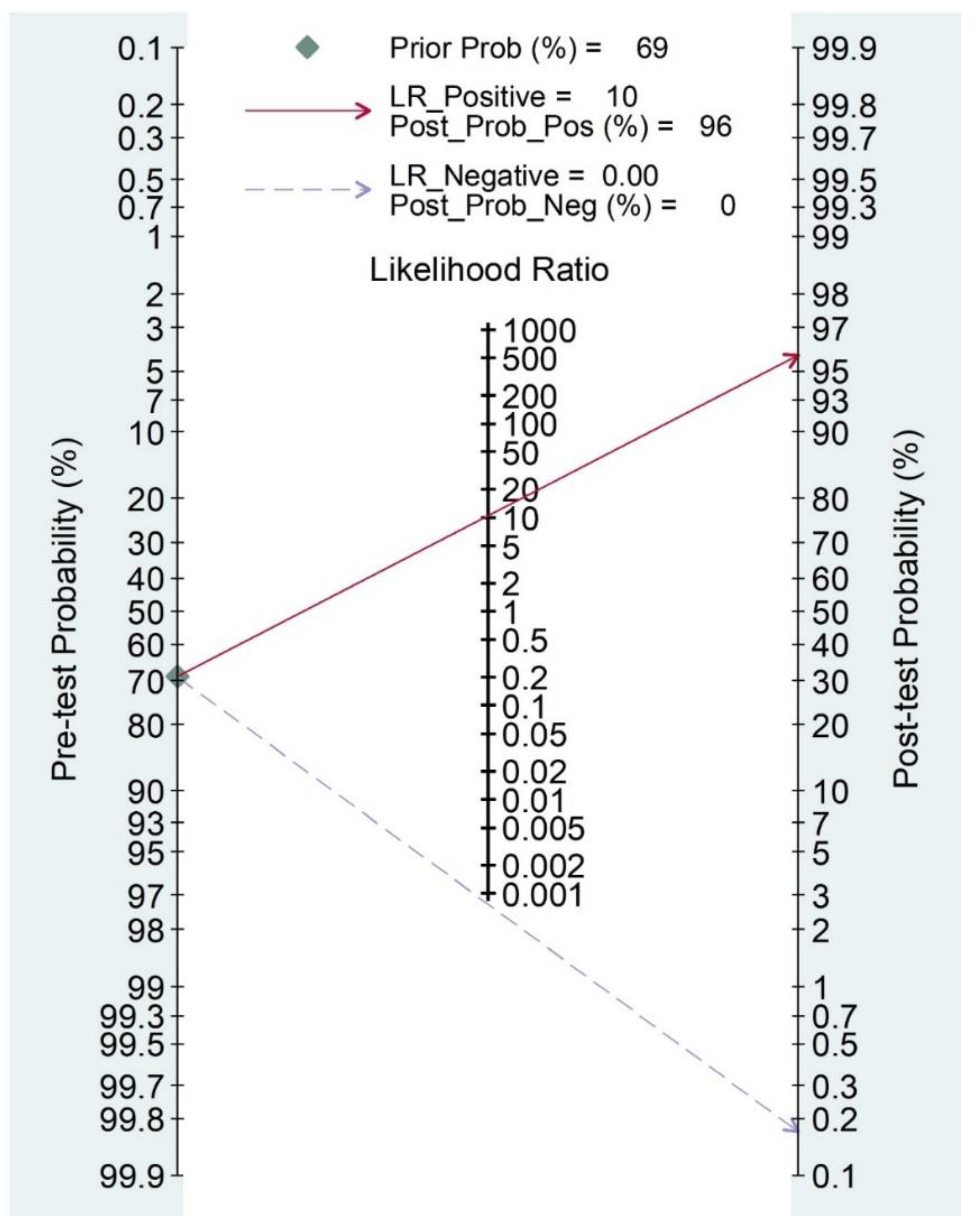
3.2. Results of Meta-Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Park, Y.-G.; Ha, C.-W.; Na, S.-E.; Kim, M.; Kim, T.S.; Chu, Y.Y. Is it worth to perform initial non-operative treatment for patients with acute ACL injury?: A prospective cohort prognostic study. Knee Surg. Relat. Res. 2021, 33, 11. [Google Scholar] [CrossRef] [PubMed]
- Fong, D.T.-P.; Hong, Y.; Chan, L.K.; Yung, P.S.-H.; Chan, K.-M. A Systematic Review on Ankle Injury and Ankle Sprain in Sports. Sports Med. 2007, 37, 73–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delahunt, E.; Bleakley, C.M.; Bossard, D.S.; Caulfield, B.M.; Docherty, C.L.; Doherty, C.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommenda-tions of the International Ankle Consortium. Br. J. Sports Med. 2018, 52, 1304–1310. [Google Scholar] [CrossRef] [Green Version]
- Pacheco, J.; Guerra-Pinto, F.; Araújo, L.; Flora, M.; Alçada, R.; Rocha, T.; Diniz, P.; Consciência, J.G. Chronic ankle instability has no correlation with the number of ruptured ligaments in severe anterolateral sprain: A systematic review and me-ta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2021, 247, 1–13. [Google Scholar]
- Wright, I.; Neptune, R.; Bogert, A.V.D.; Nigg, B. The influence of foot positioning on ankle sprains. J. Biomech. 2000, 33, 513–519. [Google Scholar] [CrossRef] [Green Version]
- Mugno, A.T.; Constant, D. Recurrent Ankle Sprain; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Chen, E.T.; Borg-Stein, J.; McInnis, K.C. Ankle Sprains: Evaluation, Rehabilitation, and Prevention. Curr. Sports Med. Rep. 2019, 18, 217–223. [Google Scholar] [CrossRef]
- Malanga, G.M.K. Musculoskeletal Physical Examination: An Evidencebased Approach, 2nd ed.; Elsevier, Inc.: Amsterdam, The Netherlands, 2017; pp. 199–217. [Google Scholar]
- Polzer, H.; Kanz, K.G.; Prall, W.C.; Haasters, F.; Ockert, B.; Mutschler, W.; Grote, S. Diagnosis and treatment of acute ankle injuries: Development of an evidence-based algorithm. Orthop. Rev. 2011, 4, e5. [Google Scholar] [CrossRef] [Green Version]
- Alves, T.; Dong, Q.; Jacobson, J.; Yablon, C.; Gandikota, G. Normal and Injured Ankle Ligaments on Ultrasonography with Magnetic Resonance Imaging Correlation. J. Ultrasound Med. 2019, 38, 513–528. [Google Scholar] [CrossRef] [Green Version]
- Vuurberg, G.; Hoorntje, A.; Wink, L.M.; Van Der Doelen, B.F.W.; Bekerom, M.P.V.D.; Dekker, R.; Van Dijk, C.N.; Krips, R.; Loogman, M.C.M.; Ridderikhof, M.L.; et al. Diagnosis, treatment and prevention of ankle sprains: Update of an evidence-based clinical guideline. Br. J. Sports Med. 2018, 52, 956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, Y.; Cai, Y.; Wang, Y. Value of ultrasonography for detecting chronic injury of the lateral ligaments of the ankle joint compared with ultrasonography findings. Br. J. Radiol. 2014, 87, 20130406. [Google Scholar] [CrossRef] [PubMed]
- Noda, Y.; Horibe, S.; Hiramatsu, K.; Takao, R.; Fujita, K. Quick and simple test to evaluate severity of acute lateral ankle sprain. Asia Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2021, 25, 30–34. [Google Scholar] [CrossRef]
- Kellett, J.J.; Lovell, G.A.; Eriksen, D.A.; Sampson, M.J. Diagnostic imaging of ankle syndesmosis injuries: A general review. J. Med. Imaging Radiat. Oncol. 2018, 62, 159–168. [Google Scholar] [CrossRef]
- Salat, P.; Le, V.; Veljkovic, A.; Cresswell, M.E. Imaging in foot and ankle instability. Foot Ankle Clin. 2018, 23, 499–522.e28. [Google Scholar] [CrossRef]
- Kim, Y.S.; Kim, Y.B.; Kim, T.G.; Lee, S.W.; Park, S.H.; Lee, H.J.; Choi, Y.J.; Koh, Y.G. Reliability and Validity of Magnetic Resonance Imaging for the Evaluation of the Anterior Talofibular Ligament in Patients Undergoing Ankle Arthroscopy. Arthroscopy 2015, 31, 1540–1547. [Google Scholar] [CrossRef] [PubMed]
- Hermans, J.J.; Beumer, A.; de Jong, T.A.; Kleinrensink, G.J. Anatomy of the distal tibiofibular syndesmosis in adults: A pictorial essay with a multimodality approach. J. Anat. 2010, 217, 633–645. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.; Cha, J.G.; Lee, Y.K.; Choi, G.C.; Paik, S.H.; Lee, H.K.; Park, S.J.; Kim, H.J. The bright rim sign on MRI for anterior talofibular ligament injury with arthroscopic correlation. AJR Am. J. Roentgenol. 2012, 198, 885–890. [Google Scholar] [CrossRef] [PubMed]
- Li, H.-Y.; Li, W.-L.; Chen, S.-Y.; Hua, Y.-H. Increased ATFL–PTFL angle could be an indirect MRI sign in diagnosis of chronic ATFL injury. Knee Surg. Sports Traumatol. Arthrosc. 2018, 28, 208–212. [Google Scholar] [CrossRef]
- Kim, M.; Choi, Y.S.; Jeong, M.S.; Park, M.; Chun, T.J.; Kim, J.S.; Young, K.W. Comprehensive Assessment of Ankle Syndes-mosis Injury Using 3D Isotropic Turbo Spin-Echo Sequences: Diagnostic Performance Compared with That of Conventional and Oblique 3-T MRI. AJR Am. J. Roentgenol. 2017, 208, 827–833. [Google Scholar] [CrossRef]
- Tao, H.; Hu, Y.; Qiao, Y.; Ma, K.; Yan, X.; Hua, Y.; Chen, S. T2-Mapping evaluation of early cartilage alteration of talus for chronic lateral ankle instability with isolated anterior talofibular ligament tear or combined with calcaneofibular ligament tear. J. Magn. Reson. Imaging 2018, 47, 69–77. [Google Scholar] [CrossRef]
- Elkaïm, M.; Thès, A.; Lopes, R.; Andrieu, M.; Cordier, G.; Molinier, F.; Benoist, J.; Colin, F.; Boniface, O.; Guillo, S.; et al. Agreement between arthroscopic and imaging study fndings in chronic anterior talo-fbular ligament injuries. Orthop. Traumatol. Surg. Res. 2018, 104, S213–S218. [Google Scholar] [CrossRef]
- Glazebrook, M.; Eid, M.; Alhadhoud, M.; Stone, J.; Matsui, K.; Takao, M. Percutaneous Ankle Reconstruction of Lateral Ligaments. Foot Ankle Clin. 2018, 23, 581–592. [Google Scholar] [CrossRef] [PubMed]
- Thordarson, D.B.; Bains, R.; Shepherd, L.E. The Role of Ankle Arthroscopy on the Surgical Management of Ankle Fractures. Foot Ankle Int. 2001, 22, 123–125. [Google Scholar] [CrossRef] [PubMed]
- Arnold, H. Post traumatic impingement syndrome of the ankle-indication and results of arthroscopic therapy. Foot Ankle Surg. 2011, 17, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meehan, T.M.; Martinez-Salazar, E.L.; Torriani, M. Aftermath of ankle inversion injuries: Spectrum of MR imaging findings. Magn. Reson. Imaging Clin. N. Am. 2017, 25, 45–61. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.G.; Sung, K.H.; Chung, C.Y.; Park, M.S.; Kim, T.W.; Lee, S.H.; Lee, K.M. Associations between MRI Findings and Symptoms in Patients with Chronic Ankle Sprain. J. Foot Ankle Surg. 2014, 53, 411–414. [Google Scholar] [CrossRef]
- Yao, X.; Florez, I.D.; Zhang, P.; Zhang, C.; Zhang, Y.; Wang, C.; Liu, X.; Nie, X.; Wei, B.; Ghert, M.A. Clinical research methods for treatment, diagnosis, prognosis, etiology, screening, and prevention: A narrative review. J. Evid.-Based Med. 2020, 13, 130–136. [Google Scholar] [CrossRef]
- Whiting, P.F.; Rutjes, A.W.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.; Sterne, J.A.; Bossuyt, P.M. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef]
- Arends, L.R.; Hamza, T.H.; van Houwelingen, H.C.; Heijenbrok-Kal, M.H.; Hunink, M.G.M.; Stijnen, T. Bivariate Random Effects Meta-Analysis of ROC Curves. Med. Decis. Mak. 2008, 28, 621–638. [Google Scholar] [CrossRef]
- Takwoingi, Y.; Guo, B.; Riley, R.; Deeks, J. Performance of methods for meta-analysis of diagnostic test accuracy with few studies or sparse data. Stat. Methods Med. Res. 2017, 26, 1896–1911. [Google Scholar] [CrossRef] [Green Version]
- Translator Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Fagan, T.J. Letter: Nomogram for Bayes theorem. N. Engl. J. Med. 1975, 293, 257. [Google Scholar]
- Deeks, J.J.; Macaskill, P.; Irwig, L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J. Clin. Epidemiol. 2005, 58, 882–893. [Google Scholar] [CrossRef] [PubMed]
- Dwamena Ben, A. MIDAS: A Program for Meta-Analytical Integration of Diagnostic Accuracy Studies in Stata; Stata Statistical Software: Release 15; Division of Nuclear Medicine, Department of Radiology, University of Michigan Medical School: Ann Arbor, MI, USA, 2017. [Google Scholar]
- Basha, M.A.A.; Eldib, D.B.; Zaitoun, M.M.; Ghandour, T.M.; Aly, T.; Mostafa, S.; Algazzar, H.Y. The Added Diagnostic Value of the Bright Rim Sign to Conventional MRI Assessment of Anterior Talofibular Ligament Disruption. Acad. Radiol. 2021, 28, e247–e257. [Google Scholar] [CrossRef]
- Gaebler, C.; Kukla, C.; Breitenseher, M.J.; Nellas, Z.J.; Mittlboeck, M.; Trattnig, S.; Vécsei, V. Diagnosis of lateral ankle ligament injuries: Comparison between talar tilt, MRI and operative findings in 112 athletes. Acta Orthop. Scand. 1997, 68, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Kreitner, K.F.; Ferber, A.; Grebe, P.; Runkel, M.; Berger, S.; Thelen, M. Injuries of the lateral collateral ligaments of the ankle: Assessment with MR imaging. Eur. Radiol. 1999, 9, 519–524. [Google Scholar] [CrossRef] [PubMed]
- Oae, K.; Takao, M.; Naito, K.; Uchio, Y.; Kono, T.; Ishida, J.; Ochi, M. Injury of the Tibiofibular Syndesmosis: Value of MR Imaging for Diagnosis. Radiology 2003, 227, 155–161. [Google Scholar] [CrossRef]
- Oae, K.; Takao, M.; Uchio, Y.; Ochi, M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skelet. Radiol. 2009, 39, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Takao, M.; Ochi, M.; Oae, K.; Naito, K.; Uchio, Y. Diagnosis of a tear of the tibiofibular syndesmosis: The role of arthroscopy of the ankle. J. Bone Jt. Surg. 2003, 85, 324–329. [Google Scholar] [CrossRef] [Green Version]
- Tan, D.W.; Teh, D.J.W.; Chee, Y.H. Accuracy of magnetic resonance imaging in diagnosing lateral ankle ligament injuries: A comparative study with surgical findings and timings of scans. Asia-Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2017, 7, 15–20. [Google Scholar] [CrossRef] [Green Version]
- Verhaven, E.F.; Shahabpour, M.; Handelberg, F.W.; Vaes, P.H.; Opdecam, P.J. The accuracy of three-dimensional magnetic resonance imaging in the diagnosis of ruptures of the lateral ligaments of the ankle. Am. J. Sports Med. 1991, 19, 583–587. [Google Scholar] [CrossRef] [PubMed]
- Macaskill, P.G.C.; Deeks, J.J.; Harbord, R.M.; Takwoingi, Y. Chapter 10: Analysing and Presenting Results. In Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy; Deeks, J.J., Bossuyt, P.M., Gatsonis, C., Eds.; Version 1.0.; The Cochrane Collaboration: London, UK, 2010; Available online: http://srdta.cochrane.org/ (accessed on 11 September 2021).
- Siegler, S.; Block, J.; Schneck, C.D. The Mechanical Characteristics of the Collateral Ligaments of the Human Ankle Joint. Foot Ankle 1988, 8, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yang, Y. Progress of diagnosis and treatment of ankle fractures combined with acute deltoid ligament injury. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi = Chin. J. Reparative Reconstr. Surg. 2017, 31, 624–628. [Google Scholar]
- Perrich, K.D.; Goodwin, D.W.; Hecht, P.J.; Cheung, Y. Ankle Ligaments on MRI: Appearance of Normal and Injured Ligaments. Am. J. Roentgenol. 2009, 193, 687–695. [Google Scholar] [CrossRef] [Green Version]
- van den Bekerom, M.P.; Kerkhoffs, G.M.; McCollum, G.A.; Calder, J.D.; van Dijk, C.N. Management of acute lateral ankle ligament injury in the athlete. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1390–1395. [Google Scholar] [CrossRef]
- Wolfe, M.W.; Uhl, T.L.; Mattacola, C.G.; McCluskey, L.C. Management of ankle sprains. Am. Fam. Physician 2001, 64, 386. [Google Scholar]
- Alghadir, A.H.; Iqbal, Z.A.; Iqbal, A.; Ahmed, H.; Ramteke, S.U. Effect of Chronic Ankle Sprain on Pain, Range of Motion, Proprioception, and Balance among Athletes. Int. J. Environ. Res. Public Health 2020, 17, 5318. [Google Scholar] [CrossRef]
- Cao, S.; Wang, C.; Ma, X.; Wang, X.; Huang, J.; Zhang, C. Imaging diagnosis for chronic lateral ankle ligament injury: A systemic review with meta-analysis. J. Orthop. Surg. Res. 2018, 13, 122. [Google Scholar] [CrossRef]
- Guillo, S.; Ankle Instability Group; Takao, M.; Calder, J.; Karlson, J.; Michels, F.; Bauer, T. Arthroscopic anatomical reconstruction of the lateral ankle ligaments. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 998–1002. [Google Scholar] [CrossRef]
- Leigheb, M.; Tricca, S.; Percivale, I.; Licandro, D.; Paladini, A.; Barini, M.; Guzzardi, G.; Grassi, F.; Stecco, A.; Carriero, A. Diagnostic Accuracy of the Magnetic Resonance Imaging in Adult Post-Ganglionic Brachial Plexus Traumatic Injuries: A Systematic Review and Meta-Analysis. Brain Sci. 2021, 11, 173. [Google Scholar] [CrossRef]
- Leigheb, M.; Guzzardi, G.; Barini, M.; Abruzzese, M.; Riva, S.; Paschè, A.; Pogliacomi, F.; Rimondini, L.; Stecco, A.; Grassi, F.A.; et al. Role of low field MRI in detecting knee lesions. Acta Biomed. 2018, 90, 116–122. [Google Scholar] [CrossRef]
- Tocci, S.L.; Madom, I.A.; Bradley, M.P.; Langer, P.R.; Di Giovanni, C.W. The Diagnostic Value of MRI in Foot and Ankle Surgery. Foot Ankle Int. 2007, 28, 166–168. [Google Scholar] [CrossRef] [PubMed]
- Romero-Morales, C.; López-Nuevo, C.; Fort-Novoa, C.; Palomo-López, P.; Rodríguez-Sanz, D.; López-López, D.; Calvo-Lobo, C.; De-La-Cruz-Torres, B. Ankle Taping Effectiveness for the Decreasing Dorsiflexion Range of Motion in Elite Soccer and Basketball Players U18 in a Single Training Session: A Cross-Sectional Pilot Study. Appl. Sci. 2020, 10, 3759. [Google Scholar] [CrossRef]
- Stiell, I.G.; McKnight, R.D.; Greenberg, G.H.; McDowell, I.; Nair, R.C.; Wells, G.A.; Johns, C.; Worthington, J.R. Implementation of the Ottawa ankle rules. JAMA 1994, 271, 827–832. [Google Scholar] [CrossRef] [PubMed]
- Abdelraouf, O.R.; Abdel-Aziem, A.A. Ankle and foot mechanics in individuals with chronic ankle instability during shod walk-ing and barefoot walking: A cross-sectional study. Chin. J. Traumatol. 2021, 27, S1008–S1275. [Google Scholar]
- Amrami, K.K.; Frick, M.A.; Matsumoto, J.M. Imaging for Acute and Chronic Scaphoid Fractures. Hand Clin. 2019, 35, 241–257. [Google Scholar] [CrossRef] [PubMed]
- Gorbachova, T.; Melenevsky, Y.; Cohen, M.; Cerniglia, B.W. Osteochondral Lesions of the Knee: Differentiating the Most Common Entities at MRI. Radiographics 2018, 38, 1478–1495. [Google Scholar] [CrossRef] [Green Version]
| Step | MEDLINE | SCOPUS | CENTRAL |
|---|---|---|---|
| 1 | Accuracy [Title/Abstract] OR accurate rate [Title/Abstract] OR diagnostic value [Title/Abstract] | Accuracy [Title/Abstract] | MeSH descriptor: [Sensitivity and Specificity] explode all trees |
| 2 | Sensibitivity and Specificity [MeSH term] | Sensibitivity and Specificity [MeSH term] | accuracy: ti, ab, kw or accurate rate: ti, ab, kw or diagnostic value: ti, ab, kw (Word variations have been searched) |
| 3 | Acute ankle injury OR ankle trauma | Acute ankle injury | MeSH descriptor: [Lateral ligament, Ankle] explode all trees |
| 4 | ATFL | ATFL | ATFL (Word variations have been searched) |
| 5 | Talofibular [Text Word] OR anterior talofibular [Text Word] | anterior talofibular [Text Word] | acute ankle injury OR ankle trauma (Word variations have been searched) |
| 6 | Lateral ligament [MeSH terms] | Lateral ligament [MeSH terms] | Talofibular OR anterior talofibular (Word variations have been searched) |
| 7 | (1 OR 2) AND (3 OR 4 OR 5 OR 6) | (1 OR 2) AND (3 OR 4 OR 5 OR 6) | (1 OR 2) AND (3 OR 4 OR 5 OR 6) |
| First Author (Year) | Subject Features | Age (Range) | Gender | Time from Injury to MRI Assessment | Gold Standard | MRI Protocol |
|---|---|---|---|---|---|---|
| Basha (2020) | 29 patients with positive clinical findings suggestive of ATFL disruption | 33 (23–43) | 19 men and 10 women | Less than 3 weeks | Arthroscopy | 1,5 T; axial T2-weighted images (T2), proton density |
| Gaebler (1997) | 112 patients with inversion trauma to the ankle and typical clinical symptoms of a ligament injury | 26 (16–35) | 67 men and 45 women | Less than 5 days | Surgery | (PD), PD fat sat (PDFS), and short tau inversion recovery (STIR) sequences |
| Kreitner (1998) | 18 patients with ankle injury | 27 (9–42) | 10 men and 8 women | Less than 7 days | Surgery | 1,5 Tesla; two proton-density- and T2-weighted double spin-echo (SE), or two T2-weighted turbo-spin-echo (TSE) sequences in oblique axial planes followed by a 3D acquisition in the axial plane. Short tan inversion recovery (STIR) sequences in the coronal plane were performed in only a few cases |
| Oae (2003) | 58 patients with ankle sprains and distal fibular fractures | 37 (12–79) | 32 men and 26 women | Not known | Arthroscopy and surgery | 1,5 Tesla; transverse T1-weighted spin-echo and T2-weighted fast spin-echo sequences. |
| Oae (2009) | 19 patients who needed an operation because of severe problems such as osteochondral lesions, synovitis and instability after acute ATFL injury | 29 (13–55) | Not known | Less than 7 days | Arthroscopy and surgery | 1,5 Tesla; transverse T2-weighted fast-spin-echo sequences |
| Takao (2003) | 52 patients with acute injuries of the ankle | 35 (14–67) | 31 men and 21 women | Not known | Arthroscopy | 1,5 Tesla; transverse T1-weighted spin-echo sequences and transverse T2-weighted fast spin-echo sequences |
| Wei Tan (2016) | 40 patients with history of acute ankle sprain injury | 26 (17–48) | 35 men and 5 women | Less than 3 months | Surgery | 3,0 Tesla; no other information about protocol |
| Verhavern (1991) | 18 patients with an acute varus trauma of the ankle | 21 (range not known) | Not known | Less than 6 hours | Surgery | 1,5 Tesla; coronal and sagittal plane in 3D FISP (fast imaging with steady-state free precession) |
| STUDY | RISK OF BIAS | APPLICABILITY CONCERN | |||||
|---|---|---|---|---|---|---|---|
| PATIENT SELECTION | INDEX TEST | REFERENCE STANDARD | FLOW AND TIMING | PATIENT SELECTION | INDEX TEST | REFERENCE STANDARD | |
| Basha 2020 | + | + | + | + | + | + | + |
| Gaebler 1997 | - | + | + | + | ? | + | + |
| Kreitner 1998 | ? | + | + | + | ? | + | + |
| Oae 2003 | + | + | ? | + | + | + | ? |
| Oae 2009 | + | + | + | + | + | + | + |
| Takao 2003 | + | + | + | ? | + | ? | + |
| Tan 2017 | + | - | + | + | + | + | + |
| Verhaven 1991 | + | + | ? | + | + | + | + |
| First Author (Year) | TP | TN | FP | FN | Se | 95% CI | Sp | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Basha (2020) | 24 | 1 | 0 | 4 | 1.00 | 0.79–1.00 | 0.50 | 0.01–0.99 |
| Gaebler (1997) | 99 | 0 | 0 | 13 | 0.88 | 0.64–0.99 | 0.74 | 0.52–0.90 |
| Kreitner (1998) * | 18 | 0 | 0 | 0 | ||||
| Oae (2003) | 28 | 2 | 0 | 28 | 1.00 | 0.85–1.00 | 0.93 | 0.77–0.99 |
| Oae (2009) | 18 | 0 | 0 | 1 | 1.00 | 0.81–1.00 | 1.00 | 0.03–1.00 |
| Takao (2003) | 23 | 2 | 0 | 27 | 1.00 | 0.88–1.00 | 0.93 | 0.78–0.99 |
| Wei Tan (2016) | 15 | 6 | 2 | 17 | 1.00 | 0.96–1.00 | 1.00 | 0.75–1.00 |
| Verhavern (1991) | 16 | 1 | 0 | 1 | 1.00 | 0.86–1.00 | 0.80 | 0.28–0.99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barini, M.; Zagaria, D.; Licandro, D.; Pansini, S.; Airoldi, C.; Leigheb, M.; Carriero, A. Magnetic Resonance Accuracy in the Diagnosis of Anterior Talo-Fibular Ligament Acute Injury: A Systematic Review and Meta-Analysis. Diagnostics 2021, 11, 1782. https://doi.org/10.3390/diagnostics11101782
Barini M, Zagaria D, Licandro D, Pansini S, Airoldi C, Leigheb M, Carriero A. Magnetic Resonance Accuracy in the Diagnosis of Anterior Talo-Fibular Ligament Acute Injury: A Systematic Review and Meta-Analysis. Diagnostics. 2021; 11(10):1782. https://doi.org/10.3390/diagnostics11101782
Chicago/Turabian StyleBarini, Michela, Domenico Zagaria, Davide Licandro, Sergio Pansini, Chiara Airoldi, Massimiliano Leigheb, and Alessandro Carriero. 2021. "Magnetic Resonance Accuracy in the Diagnosis of Anterior Talo-Fibular Ligament Acute Injury: A Systematic Review and Meta-Analysis" Diagnostics 11, no. 10: 1782. https://doi.org/10.3390/diagnostics11101782
APA StyleBarini, M., Zagaria, D., Licandro, D., Pansini, S., Airoldi, C., Leigheb, M., & Carriero, A. (2021). Magnetic Resonance Accuracy in the Diagnosis of Anterior Talo-Fibular Ligament Acute Injury: A Systematic Review and Meta-Analysis. Diagnostics, 11(10), 1782. https://doi.org/10.3390/diagnostics11101782









