Multimodal Diagnostics of Microrheologic Alterations in Blood of Coronary Heart Disease and Diabetic Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
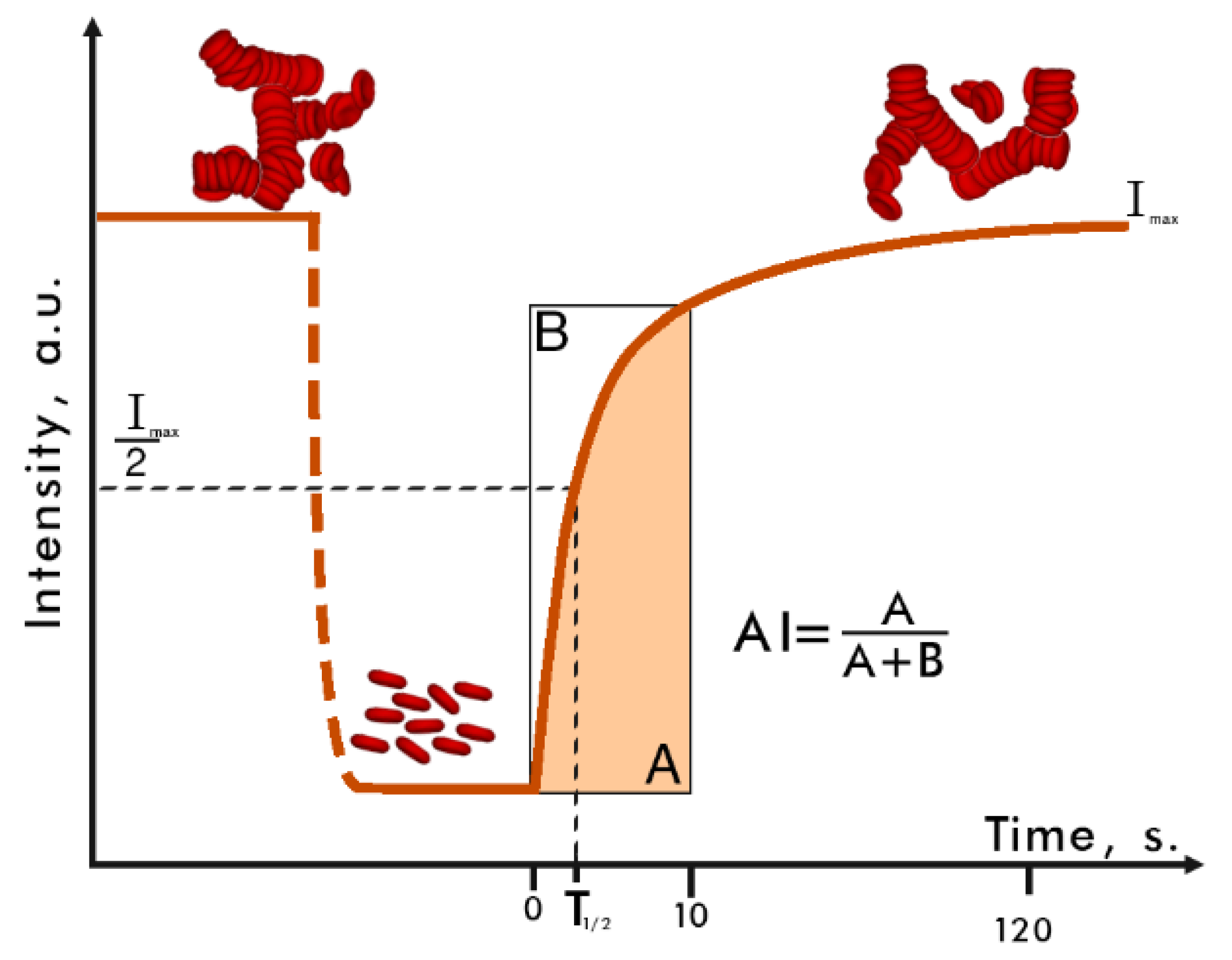
2.2. Laser Aggregometry Method
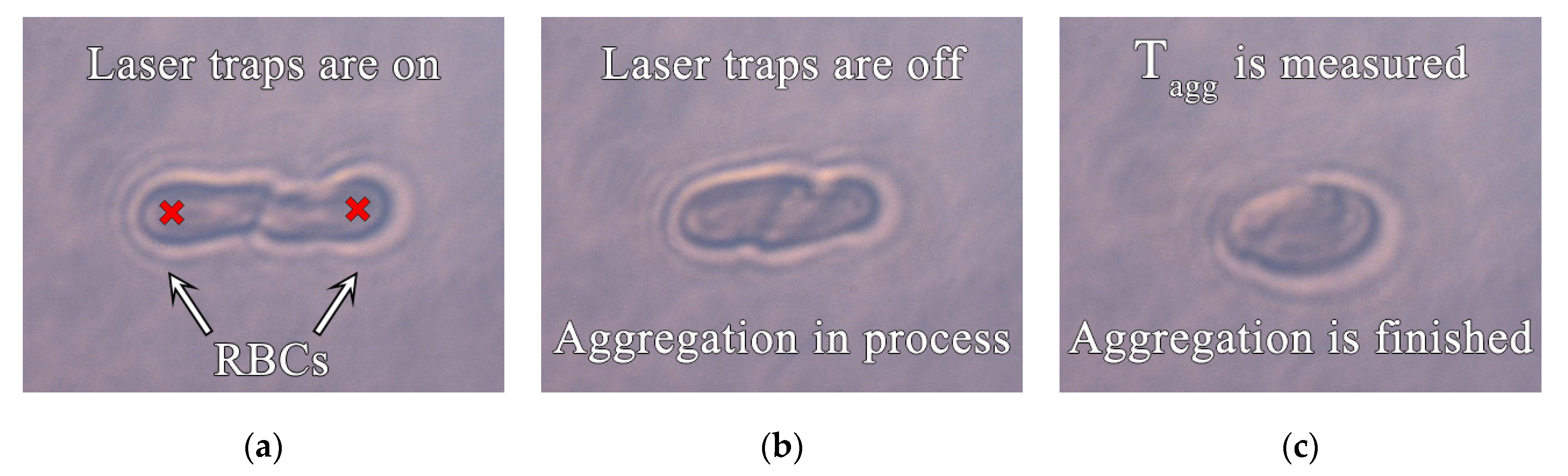
2.3. Laser Tweezers
2.4. Digital Capillaroscopy
2.5. Statistical Analysis
3. Results
3.1. Comparison of CHD Patients and Healthy Volunteers
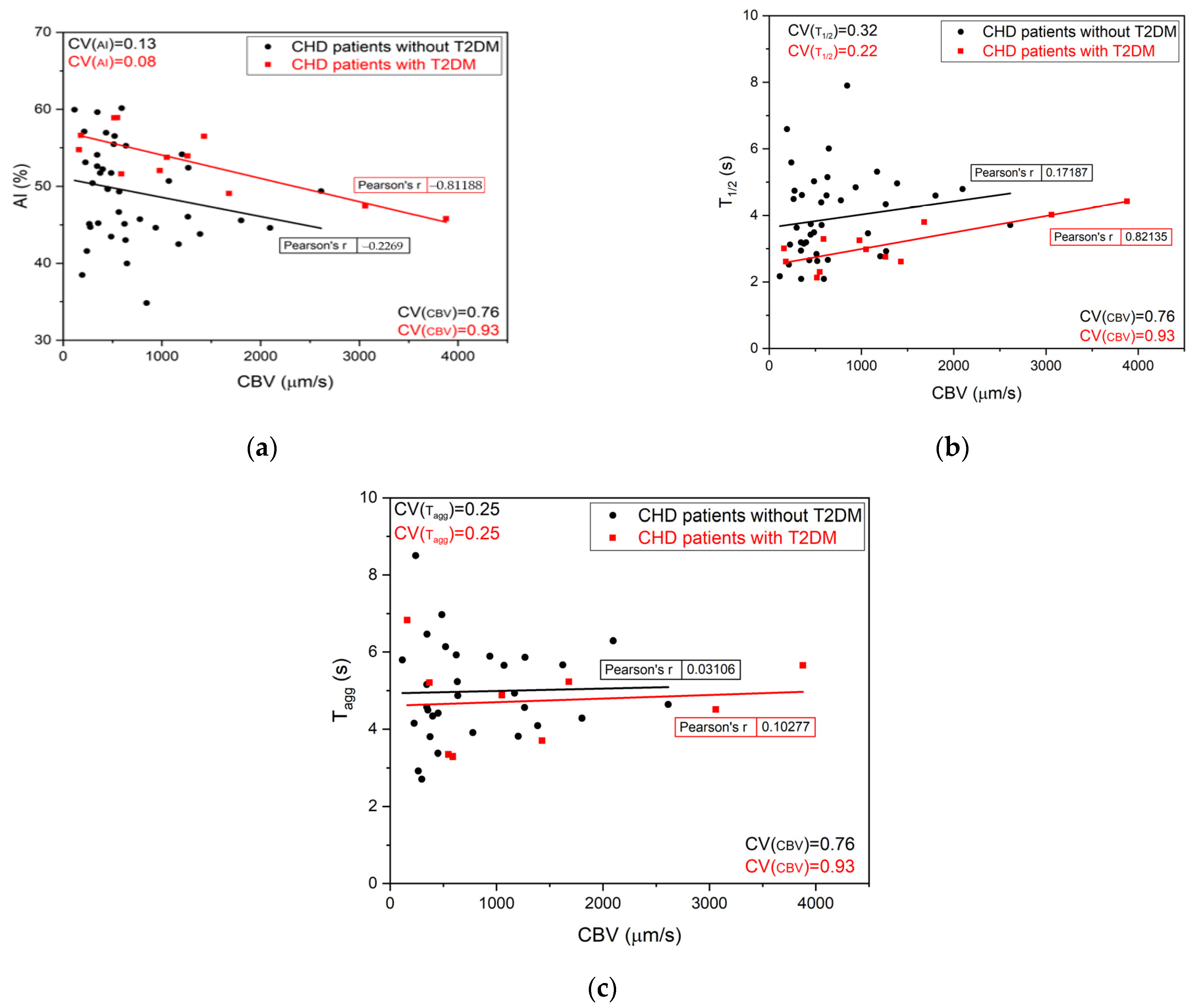
3.2. Digital Capillaroscopy Results Matched with In Vitro Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tuchin, V. (Ed.) Handbook of Optical Biomedical Diagnostics; SPIE: Bellingham, WA, USA, 2016; Volume 2. [Google Scholar]
- Patrícia, S.; Fernando, P.; Manuel, A.; Mónica, O. A review of hemorheology: Measuring techniques and recent advances. Korea-Aust. Rheol. J. 2016, 28, 1–22. [Google Scholar] [CrossRef]
- Baskurt, O.; Neu, B.; Meiselman, H. Red Blood Cell Aggregation; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar]
- Priezzhev, A.; Lee, K.; Firsov, N.; Lademann, J. Optical Study of RBC Aggregation in Whole Blood Samples and Single Cells. In Handbook on Optical Biomedical Diagnostics, 2nd ed.; Tuchin, V., Ed.; SPIE Press: Bellingham, WA, USA, 2016; pp. 5–36. [Google Scholar]
- Muravyov, A.; Tikhomirova, I.; Maimistova, A.; Bulaeva, S.; Mikhailov, P.; Kislov, N. Red blood cell aggregation changes are dependent on its initial value: Effect of long-term drug treatment and short-term cell incubation with drug. Clin. Hemorheol. Microcirc. 2011, 48, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Hochmuth, R. Micropipette aspiration of living cells. J. Biomech. 2000, 33, 15–22. [Google Scholar] [CrossRef]
- Kyriacou, P.; Budidha, K.; Abay, T.Y. Optical Techniques for Blood and Tissue Oxygenation. Ref. Modul. Biomed. Sci. 2019, 3, 461–472. [Google Scholar] [CrossRef]
- Gurfinkel, Y.; Suchkova, O.; Sasonko, M.; Priezzhev, A. Implementation of digital optical capillaroscopy for quantifying and estimating the microvascular abnormalities in diabetes mellitus. Proc. SPIE SFM 2015 2015, 9917, 991703. [Google Scholar] [CrossRef]
- Baskurt, O.; Boynard, M.; Cokelet, G.; Connes, P.; Cooke, B.; Forconi, S.; Liao, F.; Hardeman, M.; Jung, F.; Meiselman, H.; et al. New guidelines for hemorheological laboratory techniques. Clin. Hemorheol. Microcirc. 2009, 42, 75–97. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.; Yang, Y.; Suh, J. Measurement of erythrocyte aggregation in a microchip stirring system by light transmission. Clin. Hemorheol. Microcirc. 2009, 41, 197–207. [Google Scholar] [CrossRef]
- Lopatin, V.V.; Priezzhev, A.V. Multiple light scattering by suspensions of erythrocytes in geometrical optics approximation. Proc. SPIE 2002, 4749, 267–274. [Google Scholar] [CrossRef]
- Lopatin, V.N.; Priezzhev, A.V.; Aponasenko, A.D.; Shepelevich, N.V.; Lopatin, V.V.; Pozhilenkova, P.V.; Prostakova, I.V. Metody Svetorassejanija v Analize Dispersnykh Biologicheskikh Sred; Fizmatlit: Moscow, Russia, 2004. (In Russian) [Google Scholar]
- Mauer, J.; Peltomäki, M.; Poblete, S.; Gompper, G.; Fedosov, D.A. Static and dynamic light scattering by red blood cells: A numerical study. PLoS ONE 2017, 12, e0176799. [Google Scholar] [CrossRef]
- Ashkin, A.; Dziedzic, J. Optical trapping and manipulation of single living cells using infra-red laser beams. Berichte der Bunsen-Gesellschaft für Physikalische Chemie 1989, 98, 254–260. [Google Scholar] [CrossRef]
- Arne, G. (Ed.) Optical Tweezers. Methods and Protocols; Humana Press: New York, NY, USA, 2017. [Google Scholar]
- Ermolinskiy, P.; Lugovtsov, A.; Maslyanitsina, A.; Semenov, A.; Dyachuk, L.; Priezzhev, A. Interaction of erythrocytes in the process of pair aggregation in blood samples from patients with arterial hypertension and healthy donors: Measurements with laser tweezers. J. Biomed. Photonics Eng. 2018, 4, 030303. [Google Scholar] [CrossRef]
- Lee, K.; Kinnunen, M.; Khokhlova, M.; Lyubin, E.; Priezzhev, A.; Meglinski, I.; Fedyanin, A. Optical tweezers study of red blood cell aggregation and disaggregation in plasma and protein solutions. J. Biomed. Opt. 2016, 21, 035001. [Google Scholar] [CrossRef] [PubMed]
- Grover, S.; Gauthier, P.; Skirtach, A. Analysis of the behaviour of erythrocytes in an optical trapping system. Opt. Express 2000, 7, 533–539. [Google Scholar] [CrossRef]
- Gurfinkel, Y.; Sasonko, M. Potentialities of Digital Capillaroscopy in the Diagnostics of Oedema Syndrome. J. Biomed. Photonics Eng. 2017, 3, 030401. [Google Scholar] [CrossRef][Green Version]
- Parker, M.J.S.; McGill, N.W. The Established and Evolving Role of Nailfold Capillaroscopy in Connective-Tissue Disease. Chapter in book Connective-Tissue Disease, Connective Tissue Disease—Current State of the Art, Akira Takeda; IntechOpen: Rijeka, Croatia, 2018. [Google Scholar]
- Baskurt, O.K. In vivo correlates of altered blood rheology. Biorheology 2008, 45, 629–638. [Google Scholar] [CrossRef] [PubMed]
- Nemeth, N.; Deak, A.; Szentkereszty, Z.; Peto, K. Effects and influencing factors on hemorheological variables taken into consideration in surgical pathophysiology research. Clin. Hemorheol. Microcirc. 2018, 69, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Hahn, R.; Müller-Seydlitz, P.M.; Jöckel, K.H.; Hubert, H.; Heimburg, P. Viscoelasticity and red blood cell aggregation in patients with coronary heart disease. Angiology 1989, 40, 914–920. [Google Scholar] [CrossRef]
- Cicco, G.; Pirrelli, A. Red Blood Cell (RBC) Deformability, RBC Aggregability and Tissue Oxygenation in Hypertension. Clin. Hemorheol. Microcirc. 1999, 21, 169–177. [Google Scholar]
- Arbel, Y.; Banai, S.; Benhorin, J.; Finkelstein, A.; Herz, I.; Halkin, A.; Keren, G.; Yedgar, S.; Barshtein, G.; Berliner, S. Erythrocyte aggregation as a cause of slow flow in patients of acute coronary syndromes. Int. J. Cardiol. 2011, 154, 322–327. [Google Scholar] [CrossRef]
- Bogar, L. Hemorheology and hypertension: Not “chicken or egg” but two chickens from similar eggs. Clin. Hemorheol. Microcirc. 2002, 26, 81–83. [Google Scholar]
- Li, Q.; Li, L.; Li, Y. Enhanced RBC Aggregation in Type 2 Diabetes Patients. J. Clin. Lab. Anal. 2015, 29, 387–389. [Google Scholar] [CrossRef] [PubMed]
- Ermolinkiy, P.B.; Semenov, A.N.; Lugovtsov, A.E.; Poeschl, C.; Windberger, U.; Kaliviotis, E.; Priezzhev, A.V. Effect of different macromolecules on viscous and microrheologic properties of blood at various temperatures. Proc. SPIE 2019, 11065, 1106507. [Google Scholar]
- Lee, K.; Priezzhev, A.; Shin, S.; Yaya, F.; Meglinsky, I. Characterization of shear stress preventing red blood cells aggregation at the individual cell level: The temperature dependence. Clin. Hemorheol. Microcirc. 2016, 64, 853–857. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Wang, J.H.; Huang, D.D.; Li, D.G.; Chen, B.; Zhang, L.M.; Yuan, C.L.; Cai, L.J. Clinical significance of analysis of the level of blood fat, CRP and hemorheological indicators in the diagnosis of elder coronary heart disease. Saudi J. Biol. Sci. 2018, 25, 1812–1816. [Google Scholar] [CrossRef] [PubMed]
- Brun, J.F.; Varlet-Marie, E.; Raynaud de Mauverger, E.; Mercier, J. Both overall adiposity and abdominal adiposity increase blood viscosity by separate mechanisms. Clin. Hemorheol. Microcirc. 2011, 48, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Koscielny, J.; Jung, E.M.; Mrowietz, C.; Kiesewetter, H.; Latza, R. Blood fluidity, fibrinogen, and cardiovascular risk factors of occlusive arterial disease: Results of the Aachen study. Clin. Hemorheol. Microcirc. 2004, 31, 185–195. [Google Scholar]
- Kwaan, H.C. Role of plasma proteins in whole blood viscosity: A brief clinical review. Clin. Hemorheol. Microcirc. 2010, 44, 167–176. [Google Scholar] [CrossRef]
- Haszon, I.; Papp, F.; Kovács, J.; Bors, M.; Németh, I.; Bereczki, C.; Túri, S. Platelet aggregation, blood viscosity and serum lipids in hypertensive and obese children. Eur. J. Pediatr. 2003, 162, 385–390. [Google Scholar] [CrossRef]
| Parameter | Overall Patient Data (n = 56) | Patients with CHD and without T2DM (n = 42) | Patients with CHD and T2DM (n = 14) |
|---|---|---|---|
| Number (percentage) of males | 38 (68%) | 29 (69%) | 9 (64%) |
| Number (percentage) of females | 18 (32%) | 13 (31%) | 5 (36%) |
| Mean age (range), years | 69.2 (51–92) | 70.5 (51–92) | 65.3 (52–81) |
| Number (percentage) of smokers | 10 (18%) | 6 (14%) | 4 (29%) |
| Body mass index, kg/m2 | 29 ± 5 | 28 ± 5 | 31 ± 5 |
| Systolic blood pressure, mm Hg | 139 ± 27 | 142 ± 22 | 137 ± 20 |
| Diastolic blood pressure, mm Hg | 82 ± 12 | 82 ± 13 | 83 ± 9 |
| Heart rate, bpm | 71 ± 9 | 72 ± 9 | 69 ± 10 |
| LV ejection fraction, % | 57 ± 7 | 56 ± 6 | 58 ± 8 |
| Previous myocardial infarction | 22 (39%) | 18 (43%) | 4 (29%) |
| Angina pectoris | 48 (86%) | 36 (86%) | 12 (86%) |
| Bypass grafts | 5 (9%) | 4 (9%) | 1 (7%) |
| Stents | 17 (30%) | 12 (29%) | 4 (31%) |
| Antiaggregants | 39 (70%) | 29 (69%) | 10 (71%) |
| Anticoagulants | 12 (23%) | 10 (24%) | 3 (21%) |
| Diuretics | 28 (50%) | 19 (45%) | 9 (64%) |
| Parameter/Group | Control Group A (n = 15) | Control Group B (n = 10) | CHD Patients (n = 56) |
|---|---|---|---|
| AI, % | 41.0 ± 1.3 | 44 ± 3 | 49.0 ± 1.2 * |
| T1/2, s | 5.9 ± 0.4 | 5.6 ± 1.0 | 4.2 ± 0.4 * |
| Tagg, s | 6.6 ± 0.4 | - | 4.8 ± 0.2 * |
| CBV, mcm/s | - | 1290 ± 230 | 850 ± 100 |
| Parameter/Group | CHD Patients (n = 42) | CHD + T2DM Patients (n = 14) |
|---|---|---|
| AI, % | 48.6 ± 1.0 | 53.0 ± 1.1 * |
| T1/2, s | 4.1 ± 0.2 | 3.1 ± 0.2 * |
| Tagg, s | 5.0 ± 1.2 | 4.6 ± 0.4 |
| CBV, mcm/s | 750 ± 90 | 1150 ± 300 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maslianitsyna, A.; Ermolinskiy, P.; Lugovtsov, A.; Pigurenko, A.; Sasonko, M.; Gurfinkel, Y.; Priezzhev, A. Multimodal Diagnostics of Microrheologic Alterations in Blood of Coronary Heart Disease and Diabetic Patients. Diagnostics 2021, 11, 76. https://doi.org/10.3390/diagnostics11010076
Maslianitsyna A, Ermolinskiy P, Lugovtsov A, Pigurenko A, Sasonko M, Gurfinkel Y, Priezzhev A. Multimodal Diagnostics of Microrheologic Alterations in Blood of Coronary Heart Disease and Diabetic Patients. Diagnostics. 2021; 11(1):76. https://doi.org/10.3390/diagnostics11010076
Chicago/Turabian StyleMaslianitsyna, Anastasia, Petr Ermolinskiy, Andrei Lugovtsov, Alexandra Pigurenko, Maria Sasonko, Yury Gurfinkel, and Alexander Priezzhev. 2021. "Multimodal Diagnostics of Microrheologic Alterations in Blood of Coronary Heart Disease and Diabetic Patients" Diagnostics 11, no. 1: 76. https://doi.org/10.3390/diagnostics11010076
APA StyleMaslianitsyna, A., Ermolinskiy, P., Lugovtsov, A., Pigurenko, A., Sasonko, M., Gurfinkel, Y., & Priezzhev, A. (2021). Multimodal Diagnostics of Microrheologic Alterations in Blood of Coronary Heart Disease and Diabetic Patients. Diagnostics, 11(1), 76. https://doi.org/10.3390/diagnostics11010076




