Is There an Association between Temporomandibular Disorders and Articular Eminence Inclination? A Systematic Review
Abstract
1. Introduction
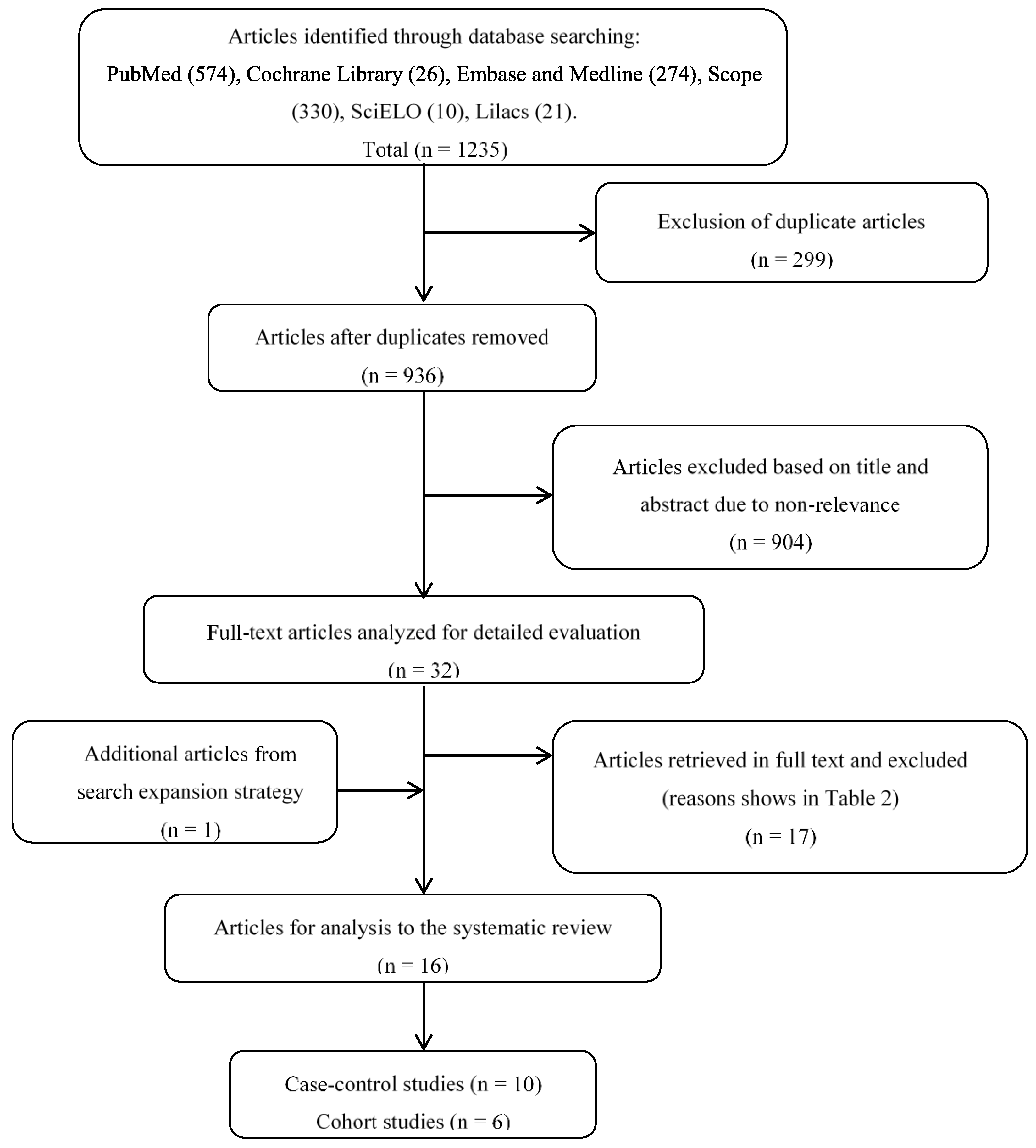
2. Materials and Methods
2.1. Protocol
2.2. Types of Studies
2.3. Language Studies
2.4. Types of Participants
2.5. Intervention Type
2.6. Type of Results
2.7. Data Collection
2.8. Databases Used
- PubMed database (article types, clinical trials, randomized controlled trials, controlled clinical trials; language, English; publication dates, 1 January 1966 to 27 January 2020);
- Cochrane Library (database, Trials; publication dates, 1966 to 2020);
- Embase (publication dates, 1974 to 2020)
- Medline (publication dates, 1946 to 2020)
- Scope (document type, article; language, English; publication dates, 1970 to 2020)
- SciELO (publication dates, to 2020)
- Lilacs (publication dates, to 2020).
2.9. Search Strategy
2.10. Study Selection
2.11. Extracting Data from the Studies
2.12. Quality Assessment
3. Results
3.1. Characteristics of Studies
3.2. Characteristics of Participants
3.3. Quality Assessment
4. Discussion
- The correlation between TMDs and AEI is still an unsolved issue. Definitive conclusions cannot be drawn based on the present studies.
- Evidence-based diagnosis with TMDs was not uniform. It is suggested to use multivariate statistical analyses for the evaluation of multifactorial complex pathologies such as TMDs.
- The insufficient number of articles considered of high methodological quality is a factor that hinders the acceptance or denial of this correlation.
- More quality and carefully designed prospective studies are required by future researchers to determine the causal relationship between TMDs and AEI.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wu, C.-K.; Hsu, J.-T.; Shen, Y.-W.; Chen, J.-H.; Shen, W.-C.; Fuh, L.-J. Assessments of inclinations of the mandibular fossa by computed tomography in an Asian population. Clin. Oral Investig. 2012, 16, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Som, P.M.; Curtin, H.D. Head and Neck Imaging, 5th ed.; Mosby, Inc.: St. Louis, MI, USA, 2011; p. 1547. [Google Scholar]
- Sümbüllü, M.A.; Çağlayan, F.; Akgül, H.M.; Yilmaz, A.B. Radiological examination of the articular eminence morphology using cone beam CT. Dentomaxillofac. Radiol. 2012, 41, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Granados, J.I. The influence of the loss of teeth and attrition on the articular eminence. J. Prosthet. Dent. 1979, 42, 78–85. [Google Scholar] [CrossRef]
- Gedrange, T.; Gredes, T.; Hietschold, V.; Kunert-Keil, C.; Dominiak, M.; Gerber, H.; Spassov, A.; Laniado, M. Comparison of reference points in different methods of temporomandibular joint imaging. Adv. Med Sci. 2012, 57, 157–162. [Google Scholar] [CrossRef] [PubMed]
- De Leeuw, R.; Klasser, G.D. The American Academy of Orofacial Pain. In Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management; Quintessence Publishing: Chicago, IL, USA, 2013. [Google Scholar]
- Manfredini, D.; Guarda-Nardini, L.; Winocur, E.; Piccotti, F.; Ahlberg, J.; Lobbezoo, F. Research diagnostic criteria for temporomandibular disorders: A systematic review of axis I epidemiologic findings. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2011, 112, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Morimoto, Y.; Tanaka, Y.; Kobayashi, S.; Okumura, Y.; Kito, S.; Okabe, S.; Ohba, T. Radiographic examination of the mandibular (glenoid) fossa in ancient and modern man. Oral Dis. 2004, 10, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Pullinger, A.; Seligman, D. Trauma history in diagnostic groups of temporomandibular disorders. Oral Surg. Oral Med. Oral Pathol. 1991, 71, 529–534. [Google Scholar] [CrossRef]
- Pullinger, A.; Seligman, D. Overbite and overjet characteristics of refined diagnostic groups of temporomandibular disorder patients. Am. J. Orthod. Dentofac. Orthop. 1991, 100, 401–415. [Google Scholar] [CrossRef]
- Melis, M.; Di Giosia, M. The role of genetic factors in the etiology of temporomandibular disorders: A review. Cranio® 2016, 34, 43–51. [Google Scholar] [CrossRef]
- Juniper, R.P. Temporomandibular joint dysfunction: A theory based upon electromyographic studies of the lateral pterygoid muscle. Br. J. Oral Maxillofac. Surg. 1984, 22, 1–8. [Google Scholar] [CrossRef]
- Isberg, A.; Westesson, P.-L. Steepness of articular eminence and movement of the condyle and disk in asymptomatic temporomandibular joints. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1998, 86, 152–157. [Google Scholar] [CrossRef]
- Paknahad, M.; Shahidi, S.; Akhlaghian, M.; Abolvardi, M. Is Mandibular Fossa Morphology and Articular Eminence Inclination Associated with Temporomandibular Dysfunction? J. Dent. (Shiraz Iran) 2016, 17, 134–141. [Google Scholar]
- Atkinson, W.B.; Bates, R.E. The effects of the angle of the articular eminence on anterior disk displacement. J. Prosthet. Dent. 1983, 49, 554–555. [Google Scholar] [CrossRef]
- Piancino, M.G.; Tepedino, M.; Cavarra, F.; Bramanti, E.; Laganà, G.; Chimenti, C.; Cirillo, S. Condylar long axis and articular eminence in MRI in patients with temporomandibular disorders. Cranio® 2018, 38, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Rabelo, K.A.; Melo, S.L.S.; Torres, M.G.G.; Campos, P.S.F.; Bentoe, P.M.; de Melo, D.P. Condyle Excursion Angle, Articular Eminence Inclination, and Temporomandibular Joint Morphologic Relations with Disc Displacement. J. Oral Maxillofac. Surg. 2017, 75, 938.e1–938.e10. [Google Scholar] [CrossRef] [PubMed]
- Shahidi, S.; Vojdani, M.; Paknahad, M. Correlation between articular eminence steepness measured with cone-beam computed tomography and clinical dysfunction index in patients with temporomandibular joint dysfunction. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Pullinger, A.G.; Seligman, D.A.; John, M.T.; Harkins, S. Multifactorial modeling of temporomandibular anatomic and orthopedic relationships in normal versus undifferentiated disk displacement joints. J. Prosthet. Dent. 2002, 87, 289–297. [Google Scholar] [CrossRef]
- Ren, Y.F.; Isberg, A.; Westesson, P.L. Steepness of the articular eminence in the temporomandibular joint: Tomographic comparison between asymptomatic volunteers with normal disk position and patients with disk displacement. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1995, 80, 258–266. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Dworkin, S.F.; LeResche, L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J. Craniomandib. Disord. 1992, 6, 301–355. [Google Scholar]
- Ohrbach, R.; Dworkin, S.F. The Evolution of TMD Diagnosis: Past, Present, Future. J. Dent. Res. 2016, 95, 1093–1101. [Google Scholar] [CrossRef] [PubMed]
- Pontes, M.L.C.; Melo, S.L.S.; Bento, P.M.; Campos, P.S.F.; de Melo, D.P. Correlation between temporomandibular joint morphometric measurements and gender, disk position, and condylar position. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 128, 538–542. [Google Scholar] [CrossRef] [PubMed]
- Shokri, A.; Zarch, H.H.; Hafezmaleki, F.; Khamechi, R.; Amini, P.; Ramezani, L. Comparative assessment of condylar position in patients with temporomandibular disorder (TMD) and asymptomatic patients using cone-beam computed tomography. Dent. Med Probl. 2019, 56, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Sa, S.C.; Melo, S.L.S.; de Melo, D.P.; Freitas, D.Q.; Campos, P.S.F. Relationship between articular eminence inclination and alterations of the mandibular condyle: A CBCT study. Braz. Oral Res. 2017, 31, 25. [Google Scholar] [CrossRef] [PubMed]
- Rabelo, K.A.; Melo, S.L.S.; Torres, M.G.G.; Peixoto, L.R.; Campos, P.S.F.; Rebello, I.M.C.R.; de Melo, D.P. Assessment of condyle position, fossa morphology, and disk displacement in symptomatic patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 124, 199–207. [Google Scholar] [CrossRef]
- Türp, J.C.; Schlenker, A.; Schröder, J.; Essig, M.; Schmitter, M. Disk displacement, eccentric condylar position, osteoarthrosis—Misnomers for variations of normality? Results and interpretations from an MRI study in two age cohorts. Bmc Oral Health 2016, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Su, N.; Liu, Y.; Yang, X.; Luo, Z.; Shi, Z. Correlation between bony changes measured with cone beam computed tomography and clinical dysfunction index in patients with temporomandibular joint osteoarthritis. J. Cranio Maxillofac. Surg. 2014, 42, 1402–1407. [Google Scholar] [CrossRef]
- İlgüy, D.; İlgüy, M.; Fişekçioğlu, E.; Dölekoğlu, S.; Ersan, N. Articular eminence inclination, height, and condyle morphology on cone beam computed tomography. Sci. World J. 2014, 2014, 761714. [Google Scholar] [CrossRef]
- Çağlayan, F.; Sümbüllü, M.A.; Akgül, H.M. Associations between the articular eminence inclination and condylar bone changes, condylar movements, and condyle and fossa shapes. Oral Radiol. 2013, 30, 84–91. [Google Scholar] [CrossRef]
- Learreta, J.A.; Barrientos, E.E. Application of a Cephalometric Method to the Temporomandibular Joint in Patients with or without Alteration in the Orientation of the Mandibular Condyle Axis. Cranio® 2013, 31, 46–55. [Google Scholar] [CrossRef]
- De Senna, B.R.; Marques, L.S.; França, J.P.; Ramos-Jorge, M.L.; Pereira, L.J. Condyle-disk-fossa position and relationship to clinical signs and symptoms of temporomandibular disorders in women. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 108, e117–e124. [Google Scholar] [CrossRef] [PubMed]
- Hirata, F.H.; Guimarães, A.S.; de Oliveira, J.X.; Moreira, C.R.; Ferreira, E.T.T.; Cavalcanti, M.G.P. Evaluation of TMJ articular eminence morphology and disc patterns in patients with disc displacement in MRI. Braz. Oral Res. 2007, 21, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Kurita, H.; Uehara, S.; Yokochi, M.; Nakatsuka, A.; Kobayashi, H.; Kurashina, K. A long-term follow-up study of radiographically evident degenerative changes in the temporomandibular joint with different conditions of disk displacement. Int. J. Oral Maxillofac. Surg. 2006, 35, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Pullinger, A.G.; Seligman, D.A. Multifactorial analysis of differences in temporomandibular joint hard tissue anatomic relationships between disk displacement with and without reduction in women. J. Prosthet. Dent. 2001, 86, 407–419. [Google Scholar] [CrossRef]
- Kurita, H.; Ohtsuka, A.; Kobayashi, H.; Kurashina, K. Flattening of the articular eminence correlates with progressive internal derangement of the temporomandibular joint. Dentomaxillofac. Radiol. 2000, 29, 277–279. [Google Scholar] [CrossRef]
- Toyama, M.; Kurita, K.; Westesson, P.-L.; Sakuma, S.; Ariji, E.; Rivera, R. Decreased disk-eminence ratio is associated with advanced stages of temporomandibular joint internal derangement. Dentomaxillofac. Radiol. 1999, 28, 301–304. [Google Scholar] [CrossRef]
- Newcastle Ottawa Scale. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 12 October 2005).
- Poluha, R.L.; Cunha, C.O.; Bonjardim, L.R.; Conti, P.C.R. Temporomandibular joint morphology does not influence the presence of arthralgia in patients with disk displacement with reduction: A magnetic resonance imaging–based study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 129, 149–157. [Google Scholar] [CrossRef]
- Aydin, O.; Ayberk, A.H.; Metin, S.; Bugra, S. Evaluation of articular eminence morphology and inclination in tmj internal derangement patients with MRI. Int. J. Morphol. 2012, 30, 740–744. [Google Scholar]
- Sulun, T.; Cemgil, A.T.; Duc, J.-M.P.; Rammelsberg, P.; Jäger, L.; Gernet, W. Morphology of the mandibular fossa and inclination of the articular eminence in patients with internal derangement and in symptom-free volunteers. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2001, 92, 98–107. [Google Scholar] [CrossRef]
- Al-Rawi, N.H.; Uthman, A.T.; Sodeify, S.M. Spatial analysis of mandibular condyles in patients with temporomandibular disorders and normal controls using cone beam computed tomography. Eur. J. Dent. 2017, 11, 099–105. [Google Scholar] [CrossRef]
- Imanimoghaddam, M.; Madani, A.S.; Mahdavi, P.; Bagherpour, A.; Darijani, M.; Ebrahimnejad, H. Evaluation of condylar positions in patients with temporomandibular disorders: A cone-beam computed tomographic study. Imaging Sci. Dent. 2016, 46, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Estomaguio, G.A.; Yamada, K.; Ochi, K.; Hayashi, T.; Hanada, K. Craniofacial Morphology and Inclination of the Posterior Slope of the Articular Eminence in Female Patients With and Without Condylar Bone Change. Cranio® 2005, 23, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Tsuruta, A.; Hanada, K.; Hayashi, T. Morphology of the articular eminence in temporomandibular joints and condylar bone change. J. Oral Rehabil. 2004, 31, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Sato, S.; Kawamura, H.; Motegi, K.; Takahashi, K. Morphology of the mandibular fossa and the articular eminence in temporomandibular joints with anterior disk displacement. Int. J. Oral Maxillofac. Surg. 1996, 25, 236–238. [Google Scholar] [CrossRef]
- Galante, G.; Paesani, D.; Tallents, R.; Hatala, M.; Katzberg, R.; Murphy, W. Angle of the articular eminence in patients with temporomandibular joint dysfunction and asymptomatic volunteers. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1995, 80, 242–249. [Google Scholar] [CrossRef]
- Panmekiate, S.; Petersson, A.; Åkerman, S. Angulation and prominence of the posterior slope of the eminence of the temporomandibular joint in relation to disc position. Dentomaxillofac. Radiol. 1991, 20, 205–208. [Google Scholar] [CrossRef]
- Türp, J.C.; Schindler, H. The dental occlusion as a suspected cause for TMDs: Epidemiological and etiological considerations. J. Oral Rehabil. 2012, 39, 502–512. [Google Scholar] [CrossRef]
- De Boever, J.A.; Carlsson, G.E.; Klineberg, I.J. Need for occlusal therapy and prosthodontic treatment in the management of temporomandibular disorders. Part I. Occlusal interferences and occlusal adjustment. J. Oral Rehabil. 2000, 27, 367–379. [Google Scholar] [CrossRef]
- Greene, C.S. Relationship between occlusion and temporomandibular disorders: Implications for the orthodontist. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 11–15. [Google Scholar] [CrossRef]
- Slade, G.D.; Diatchenko, L.; Ohrbach, R.; Maixner, W. Orthodontic Treatment, Genetic Factors, and Risk of Temporomandibular Disorder. Semin. Orthod. 2008, 14, 146–156. [Google Scholar] [CrossRef]
- Landi, N.; Manfredini, D.; Tognini, F.; Romagnoli, M.; Bosco, M. Quantification of the relative risk of multiple occlusal variables for muscle disorders of the stomatognathic system. J. Prosthet. Dent. 2004, 92, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Pullinger, A.; Seligman, D.; Gornbein, J. A Multiple Logistic Regression Analysis of the Risk and Relative Odds of Temporomandibular Disorders as a Function of Common Occlusal Features. J. Dent. Res. 1993, 72, 968–979. [Google Scholar] [CrossRef] [PubMed]
- Honey, O.B.; Scarfe, W.C.; Hilgers, M.J.; Klueber, K.; Silveira, A.M.; Haskell, B.S.; Farman, A.G. Accuracy of cone-beam computed tomography imaging of the temporomandibular joint: Comparisons with panoramic radiology and linear tomography. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Katsavrias, E.G. Changes in articular eminence inclination during the craniofacial growth period. Angle Orthod. 2002, 72, 258–264. [Google Scholar] [PubMed]
- Kikuchi, K.; Takeuchi, S.; Tanaka, E.; Shibaguchi, T.; Tanne, K. Association between condylar position, joint morphology and craniofacial morphology in orthodontic patients without temporomandibular joint disorders. J. Oral Rehabil. 2003, 30, 1070–1075. [Google Scholar] [CrossRef] [PubMed]
- Kollmann, J.; Ranke, J.; Virchow, R. Verständigung über ein gemeinsames craniometrisches Verfahren: Frankfurter Verständigung. Arch. Anthr. 1883, 15, 1–8. [Google Scholar]
- Schmidt, E. Die horizontalebene des menschlichen schädels. Arch. Anthr. 1876, 25, 9–60. [Google Scholar]
- Milano, V.; Desiate, A.; Bellino, R.; Garofalo, T. Magnetic resonance imaging of temporomandibular disorders: Classification, prevalence and interpretation of disc displacement and deformation. Dentomaxillofac. Radiol. 2000, 29, 352–361. [Google Scholar] [CrossRef]
- Peroz, I.; Seidel, A.; Griethe, M.; Lemke, A.-J. MRI of the TMJ: Morphometric comparison of asymptomatic volunteers and symptomatic patients. Quintessence Int. 2011, 42, 659–667. [Google Scholar]
- Warren, M.P.; Fried, J.L. Temporomandibular Disorders and Hormones in Women. Cells Tissues Organs 2001, 169, 187–192. [Google Scholar] [CrossRef]
- Öberg, T.; Carlsson, G.E.; Fajers, C.-M. The Temporomandibular Joint: A Morphologic Study on a Human Autopsy Material. Acta Odontol. Scand. 1971, 29, 349–384. [Google Scholar] [CrossRef] [PubMed]
- Katsavrias, E.G.; Dibbets, J. The growth of articular eminence height during craniofacial growth period. Cranio® 2001, 19, 13–20. [Google Scholar] [CrossRef] [PubMed]


| Database and Limits | Search Strategy and Terms | ||
|---|---|---|---|
| Semantic Fields: Temporomandibular Disorders | Semantic Fields:Articular Eminence Inclination | ||
| PubMed (n = 574) Article types, clinical trials, randomized controlled trials, controlled clinical trials Language, English Publication dates, 01 January 1966 to 27 January 2020 | Temporomandibular disorder [tiab] OR TMJ Dysfunction [tiab] OR disk displacement [tiab] OR Muscular pain [tiab] OR clicking [tiab] | AND | glenoid fossa [tiab] OR posterior slope [tiab] OR articular eminence [tiab] |
| Cochrane Library (n = 26) Database, trials Publication dates, 1966 to 2020 | Temporomandibular disorder OR TMJ Dysfunction OR disk displacement OR Muscular pain OR clicking | AND | glenoid fossa OR posterior slope OR articular eminence |
| Embase and Medline (n = 274) Publication dates, Embase 1974 to 2020 and Medline 1946 to 2020 | Temporomandibular disorder OR TMJ Dysfunction OR disk displacement OR Muscular pain OR clicking | AND | glenoid fossa OR posterior slope OR articular eminence |
| Scope (n = 330) Document type, article Language, English Publication dates, 1970 to 2020. | (TITLE-ABS-KEY (temporomandibular AND disorders) OR TITLE-ABS-KEY (tmj AND dysfunction) OR TITLE-ABS-KEY (disk AND displacement) OR TITLE-ABS-KEY (clicking) OR TITLE-ABS-KEY (muscular AND pain) AND TITLE-ABS-KEY (articular AND eminence) OR TITLE-ABS-KEY (glenoid AND fossa)) AND (LIMIT-TO (DOCTYPE, “ar”)) AND (LIMIT-TO (LANGUAGE, “English”)) | ||
| SciELO (n = 10) Publication dates, to 2020 | (Temporomandibular disorder OR TMJ Dysfunction OR disk displacement OR Muscular pain OR clicking) | AND | (glenoid fossa OR articular eminence) |
| Lilacs (n = 21) Publication dates, to 2020 | (Temporomandibular disorder OR TMJ Dysfunction OR disk displacement OR Muscular pain OR clicking) | AND | (glenoid fossa OR articular eminence) |
| First Author and Year | Reason for Exclusion |
|---|---|
| de Pontes, 2019 [24] | Morphological research |
| Shokri, 2019 [25] | Quantitative data of AEI is not shown |
| Piancino, 2020 [16] | Concerning on TMDs patients with or without condylar asymmetry |
| Sa, 2017 [26] | Patients with degenerative bone diseases |
| Rabelo, 2017 [27] | No direct relationship between fossa shape and TMDs |
| Türp, 2016 [28] | No direct relationship between AEI and TMDs |
| Su, 2014 [29] | Grouping of the glenoid fossa is not clear |
| İlgüy, 2014 [30] | The diagnosis of participates is not clear |
| Çağlayan, 2014 [31] | Same data as Sümbüllü, 2012 [3] |
| Learreta, 2013 [32] | Group divided based on alterations in the condylar axis |
| Robinson de Senna, 2009 [33] | No description of the morphology of the fossa |
| Hirata, 2007 [34] | Sample size is too small |
| Kurita, 2006 [35] | Morphological research |
| Tanaka, 2004 [8] | Dry skull study, no TMDs diagnosis |
| Pullinger, 2001 [36] | Same data as Pullinger, 2002 [19] |
| Kurita, 2000 [37] | Grouping is not clear |
| Toyama, 1999 [38] | Only the relationship between disk and fossa |
| First Author & Year | Type of Study | Population | Intervention | Comparison (Control Group) | Outcome | Conclusions |
|---|---|---|---|---|---|---|
| Poluha, 2020 [40] | Case-control study | 36 individuals: 12 DDWR and arthralgia (12F, m.a.: 33.58 ± 9.75), DDWR and no arthralgia (4M, 8F, m.a.: 32.58 ± 10.9), asymptomatic individuals (3M, 9F, m.a.: 29 ± 6.86) | TMDs: symptoms & signs, RDC/TMD AEI: best-fit line 1-way ANOVA, Logistic regression analysis, p < 0.05 | Case: Unilateral DDWR and arthralgia (n = 12) Bilateral DDWR and no arthralgia (n = 12) Control: asymptomatic individuals (n = 12) | No significant differences (p > 0.05) between groups for AEI | No factors associated with the concomitant presence of arthralgia in patients with DDWR |
| Rabelo, 2017 [17] | Cohort study | 199 joints of 104 patients (86F, 18M) m.a.:40.92 a.r.:18-88 | TMDs: with TMD symptom AEI: top-roof line 1-way ANOVA, Mann- Whitney rank-sum test, Tukey post hoc test, p < 0.05 | Classified by shape of fossa (Flattened n = 45; Sigmoid n = 78; Box n = 57; Deformed n = 19) | AEI was higher in box shaped group | Disc position is not influenced by articular eminence morphology AEI has an influence on disk reduction |
| Classified by position of disc (Normal n = 86, Displaced n = 113) | AEI were not related to the presence or absence of DD | |||||
| Classified into 8 groups based on types of DD | AEI were not related to the type of DD and AEI | |||||
| Displaced group (n = 113) divided into 2 subgroups (DDWR n = 85, DDWOR n = 28) | AEI was higher for DDWR group | |||||
| Aydin, 2012 [41] | Cohort study | 70 joints of 35 selected patients (17F, 18M) | TMDs: signs and symptoms AEI: best-fit line Mann–Whitney U- test | DDWR (n = 51) DDWOR (n = 19) Two groups then subdivided by distributions of AEI (shallow (15°–30°), moderate (30°–60°), steep (60°–90°)) | No correlation between the 2 groups and AEI (p >0.05) For the distributions of AEI in both groups, moderate was the most frequent, followed by shallow and steep | The AEI may not have a predisposing effect on development of DD |
| Sülün, 2001 [42] | Case-control study | 112 joints of 56 symptomatic patients (44F, 12M, m.a.: 33.35) 50 joints of 25 symptom-free volunteers (14F, 11M, m.a.: 23.87) | TMDs: symptoms, confirmed disk malpositions by MRI AEI: best-fit line Mann-Whitney U test, Wilcoxon matched pairs test, p < 0.05 | Case: DDWR: n = 61, DDWOR: n = 28, Asymptomatic side of the patients: n = 23 Control: AV: n = 50 | The AEI on the central and the medial slices in the DDWR group were steeper than those in the AV joints and in DDWOR joints The AEI of the medial slice was larger than the central and lateral slices in DDWR group | A steeper slope is a factor of DD. The flattening observed in the bone surface during the DDWOR stage |
| First Author & Year | Type of Study | Population | Intervention | Comparison (Control Group) | Outcome | Conclusions |
|---|---|---|---|---|---|---|
| Al-Rawi, 2017 [43] | Case-control study | 70 participants (a.r.: 16–44): 35 TMD patients (19M, 16F, m.a.: 27.9), 35 patients without TMD history (19M, 16F, m.a.: 24.7) | TMDs: RDC/TMD; AEI: top-roof line; Paired sample t-test, independent sample t-test, p < 0.05 | Case: TMD patients (n = 35); Control: patients without TMD history (n = 35) | AEI was significantly greater in the affected joints in male group, but no difference between affected and normal joints in female group | The condyles of the affected joints may rotate inward |
| Paknahad, 2016 [14] | Case-control study | 40 patients (28F, 12M) with TMD, a.r: 21-57; 23 participants (18F, 5M) without TMD, a.r.: 25-50 | TMDs: according to the Helkimo index; AEI: top-roof line; Paired t-test, Student’s t-test, p ≤ 0.05 | Case: patients with signs and symptoms of TMDs; Control: participants without signs and symptoms of TMDs | AEI was higher in patient group than in control group (p = 0.001) No significant difference between the two genders in control group and patient group (p > 0.05) | AEI was steeper in patients with TMD |
| Imanimoghaddam, 2016 [44] | Case-control study | 50 patients: 25 TMD patients (5M, 20F, m.a.: 28.84 ± 9.84), 25 normal patients (8M, 17F, m.a.: 28.43 ± 3.24) | TMDs: symptoms & signs, RDC/TMD; AEI: tangent line from the uppermost point of the glenoid fossa; independent t-test, p < 0.05 | Case: patients suffering from TMD (n = 25); Control: patients with normal TMJs and Class I occlusion (n = 25) | AEI did not differ between the normal and TMD patients | CBCT could be considered a useful diagnostic imaging modality for TMD patients |
| Shahidi, 2013 [18] | Cohort study | 60 joints of 30 patients (21 F, 9M), m.a.: 31.89, a.r: 18-52 | TMDs: according to the Helkimo index; AEI: top-roof line; Spearman’s correlation test, paired t test, p < 0.05 | Classified into 3 groups regarding the clinical Di of the Helkimo index (Di I (n = 5), Di II (n = 18), Di III (n = 7) | No correlation between the 3 groups (Di I, II, and III) and AEI in either joint (p > 0.05) | No apparent relationship between the AEI and the clinical Di in patients with TMD |
| Sümbüllü, 2012 [3] | Case-control study | 104 joints of 52 patients (41F, 11M) with TMDs and 82 joints of 41 patients (24F, 17M) without TMDs | TMDs: clinical signs and symptoms; AEI: top-roof line, best-fit line; One-way ANOVA, student’s t-test, p < 0.05 | Case: patients with TMJ dysfunction; Control: patients without TMJ dysfunction | There was a difference in AEI between the patient and control groups (p < 0.05) No differences in AEI according to gender and age in TMD group (p > 0.05) | AEI was steeper in healthy control group than in TMDs group |
| Estomaguio, 2005 [45] | Cohort study | 39 female orthodontic patients with TMDs | TMDs: signs and symptoms; AEI: best-fit line; Unpaired t-test, p < 0.05 | NBC: n = 18, m.a.: 19.1 ± 4.7, a.r.: 15-23; BCBC: n = 21, m.a.: 22.7 ± 7.5, a.r.: 14-30 | Lateral and central sections of AEI was steeper in NBC than in BCBC | Flattening of the eminence accompany condylar change |
| Yamada, 2004 [46] | Cohort study | 42 joints of 21 female TMD patients scheduled for orthognathic surgery | TMDs: signs and symptoms; AEI: best-fit line; Mann–Whitney U-test, one- factor ANOVA, p < 0.05 | Classified by bone change (NBC: n = 20, m.a.: 21.44, a.r.: 17.9-24.6; BCBC: n = 22, m.a.: 22.8, a.r.: 17.5-24.3) | AEI in the lateral and central sections were steeper in NBC group than BCBC group | Flattening of the eminence seems to occur during changes from erosion to osteophyte, and from DDWR to DDWOR. |
| BCBC subdivided by types of bone change (erosion: n = 10; osteophyte: n = 12), NBC: n = 20 | AEI in all three sections of the osteophyte group were less than in the NBC group | |||||
| Classified by DD (normal: n = 15; displacement: n = 27) | No significant differences between the normal group and displacement group | |||||
| Displacement group then subdivided into 2 groups (DDWR: n = 7; DDWOR: n = 20) | AEI of central and lateral sections in DDWR were steeper than DDWOR |
| First Author & Year | Type of Study | Population | Intervention | Comparison (Control group) | Outcome | Conclusions |
|---|---|---|---|---|---|---|
| Pullinger, 2002 [19] | Case-control study | 162 female patients with unilateral disk disorders (m.a.: 33.68 ± 13.89); 21 asymptomatic female subjects (m.a.: 24.2 ± 2.9) | TMDs: RDC/TMD; AEI: best-fit line; Classification tree analysis, independent samples t test, p < 0.05 | Case: patients with unilateral disk disorders (DDWR: n = 84; DDWOR: n = 78;) Control: asymptomatic female subjects (n = 21) | No difference in eminence slope angle between 2 groups | |
| Sato, 1996 [47] | Case-control study | 91 joints of 79 females with ADD (m.a.: 24.5 ± 4.90); 48 joints of 24 females without TMDs (m.a.: 21.5 ± 2.45) | TMDs: clinical sign, confirmed with arthrography; AEI: top-roof line, best-fit line; Student’s t-test, p < 0.05 | Case: joints with ADD (n = 91), then subdivided into DDWR (n = 46) and DDWOR (n = 45); Control: joints without TMJ dysfunction (n = 48) | AEI (best-fit line) of joints with ADD was significantly larger than control joints (p < 0.01); No difference of AEI (top-roof line) between the joints with ADD and the control joints; No difference in any variable studied (best-fit line and top-roof line) between DDWR and DDWOR | A steep AEI appears to be partly responsible for the genesis of ADD |
| Ren, 1995 [20] | Case-control study | 34 joints of 34 asymptomatic volunteers (18F, 16M, m.a.: 28, a.r: 18-44); 85 joints of 71 patients (50F, 21M, m.a.: 38, a.r: 21-70) | TMDs: pain in TMJ area, confirmed with arthrography; AEI: best-fit line; ANOVA, paired t-test, p < 0.05 | Case: ADD joints (n = 85) divided into DDWR (n = 37) and DDWOR (n = 48). Then subdivided by OC: with OC (DDWR = 7, DDWOR = 27), without OC (ADR = 30, ADNR = 21); Control: asymptomatic joints (n = 34) | No difference in the AEI between normal joints and joints with DD in the central and medial sections. (p > 0.05). A tendency of a flat eminence in the joints with DDWOR; Normal joints steeper than OC joints in lateral (p < 0.01) and medial (p < 0.05) section. Joints without OC steeper than Joints with OC (p < 0.05) | A steep eminence could not be verified as a predisposing factor for DD; Flattening of the eminence was not related to the DD but OC |
| Galante, 1995 [48] | Case-control study | 74 patients (62F, 12M); 35 asymptomatic volunteers (15F, 14M) | TMDs: with TMD symptom AEI: best-fit line; Chi-square tests, Student-Newman-Keuls tests, p < 0.05 | Case: patients are classified by MRI into 4 groups (SN, DDWR, DDWOR, DDN/DJD, the simple size of different groups was not mentioned); Control: volunteers are classified by MRI into 2 groups (AV: n = 29, ABN: n = 6) | No difference among the six diagnostic groups. | AEI may not represent a predisposing factor for the development of internal derangement of the TMJ |
| Panmekiate, 1991 [49] | Cohort study | 60 joint of 54 patients | TMDs: Disk position classified by arthrography; AEI: top-roof line; Two-tailed t test, p < 0.05. | Superior disc position (20 joints from 17 patients, m.a.: 38); DDWR (20 joints from 19 patients, m.a.: 32); DDWOR (20 joints from 18 patients, m.a.: 33) | No differences in angulation among 3 section in each 3 group | No correlation between a steep articular eminence and ADD. |
| Positive | Negative | ||||
|---|---|---|---|---|---|
| First Author & Year | Radiological Method | NOS Score | First Author & Year | Radiological Method | NOS Score |
| Rabelo, 2017 [17] | MRI | 4 | Poluha,2020 [40] | MRI | 6 |
| Al-Rawi, 2017 [43] | CBCT | 4 | Imanimoghaddam M, 2016 [42] | CBCT | 5 |
| Paknahad, 2016 [14] | CBCT | 5 | Shahidi, 2013 [18] | CBCT | 5 |
| Sümbüllü, 2012 [3] | CBCT | 5 | Aydin, 2012 [41] | MRI | 4 |
| Estomaguio, 2005 [44] | Helical CT | 4 | Pullinger, 2002 [19] | 2D (tomograms) | 5 |
| Yamada, 2004 [45] | Helical CT | 3 | Ren, 1995 [20] | 2D (tomograms) | 4 |
| Sülün, 2001 [46] | MRI | 4 | Galante, 1995 [48] | 2D (laminagraph) | 2 |
| Sato, 1996 [47] | 2D (transcranial radiographs) | 3 | Panmekiate, 1991 [49] | 2D (tomograms) | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, X.-C.; Singh, D.; Ma, L.-S.; Piehslinger, E.; Huang, X.-F.; Rausch-Fan, X. Is There an Association between Temporomandibular Disorders and Articular Eminence Inclination? A Systematic Review. Diagnostics 2021, 11, 29. https://doi.org/10.3390/diagnostics11010029
Fan X-C, Singh D, Ma L-S, Piehslinger E, Huang X-F, Rausch-Fan X. Is There an Association between Temporomandibular Disorders and Articular Eminence Inclination? A Systematic Review. Diagnostics. 2021; 11(1):29. https://doi.org/10.3390/diagnostics11010029
Chicago/Turabian StyleFan, Xiao-Chuan, Diwakar Singh, Lin-Sha Ma, Eva Piehslinger, Xiao-Feng Huang, and Xiaohui Rausch-Fan. 2021. "Is There an Association between Temporomandibular Disorders and Articular Eminence Inclination? A Systematic Review" Diagnostics 11, no. 1: 29. https://doi.org/10.3390/diagnostics11010029
APA StyleFan, X.-C., Singh, D., Ma, L.-S., Piehslinger, E., Huang, X.-F., & Rausch-Fan, X. (2021). Is There an Association between Temporomandibular Disorders and Articular Eminence Inclination? A Systematic Review. Diagnostics, 11(1), 29. https://doi.org/10.3390/diagnostics11010029






