The Route to Autism Spectrum Diagnosis in Pediatric Practice in Bulgaria
Abstract
1. Introduction
2. Materials and Methods
- (1)
- Structured questionnaire for the history of pregnancy, birth and neurodevelopment;
- (2)
- Structured questionnaire on behavioral peculiarities
- (3)
- Semi-structured history on parental neurodevelopmental concerns that motivated their visit.
- (4)
- Semi-structured history and examination for ASD according to previously describes methodology [17] that included observation and parental information on: spontaneous behavior; spontaneous play; attitude to toy-cars, building blocks, puzzles, books, pencil and paper; attitude to parents; attitude to the physician; joint attention tests—looking at a pointed picture, pointing towards wanted or interesting object; nonverbal communication tests—understanding of gestures for ”Take that!”, “Give me!”, “Come here!”, etc.; spontaneous speech—idiosyncratic, melody, prosody, content, grammar, vocabulary, echolalia, etc.; verbal communication—understands commands, verbal production.
- (5)
- ASD diagnostic checklist based on DSM-5 criteria and filled in with the data from the objective examination and the history (list of signs is given in Table 2; additional signs observed or in history were also recorded)
- (6)
- Childhood Autism Rating Scale (CARS)
- (7)
- Modified Checklist for Autism in Toddlers (M-CHAT) [18].
Statistical Analysis
3. Results
3.1. Passport and Premorbid Anamnestic Data
3.2. Behavior Peculiarities
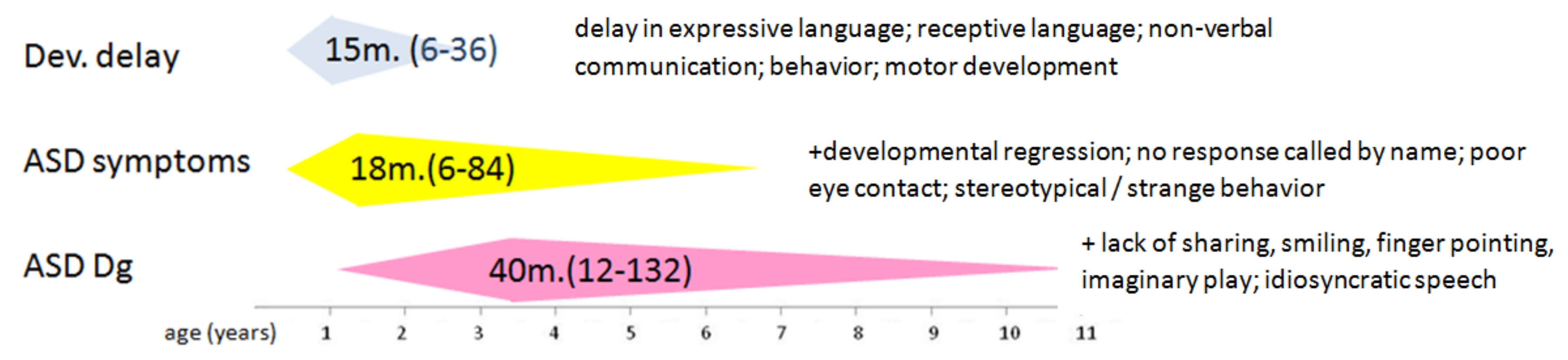
3.3. First Impairments in Neurodevelopment
3.4. Neurodevelopmental Regression
3.5. First ASD Symptoms
3.6. Reasons for Consulting a Specialist
3.7. ASD Diagnosis by Age, Specialist, and Delay
3.8. ASD without Language Delay at Diagnosis
3.9. ASD Symptoms
3.10. CARS
3.11. M-CHAT
4. Discussion
4.1. ASD Diagnosis
4.2. ASD Group Characteristics
4.3. Age of Diagnosis
- The 7-months delay of patients living in villages may replace, to some extent, the missing data on education and socio-economic status, assuming that there is some inferiority of these variables in rural inhabitants compared to urban ones.
- The smaller delay in preterm babies, which are regularly and actively followed-up, combined with the absence of correlation between delay magnitude and severity of autism, reflected in CARS, proves the yield of proactive monitoring of neurodevelopmental issues.
- Most parents perceive initially that their children have only language problems, which are thought as “benign, self-healing”. They overlook nonverbal socio-communicative and behavioral problems. These assumptions and the imminent stigma lead frequently to a delay in the search of medical help and cause search of second, third, etc., opinion instead of starting intervention.
4.4. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zwaigenbaum, L.; Penner, M. Autism Spectrum Disorder: Advances in Diagnosis and Evaluation. BMJ 2018, 361, k1674. [Google Scholar]
- Hansen, S.N.; Schendel, D.E.; Partner, E.T. Explaining the Increase in the Prevalence of Autism Spectrum Disorders: The Proportion Attributable to Changes in Reporting Practices. JAMA Pediatr. 2015, 169, 56–62. [Google Scholar]
- Nevison, C.D. A Comparison of Temporal Trends in the United States Autism Prevalence to Trends in Suspended Environmental Factors. Environ. Health 2014, 13, 73. [Google Scholar] [CrossRef]
- Philippat, C.; Heude, B.; Botton, J.; Alfaidy, N.; Calafat, A.M.; Slama, R.; EDEN Mother–Child Cohort Study Group. Prenatal Exposure to Select Phthalates and Phenols and Associations with Fetal and Placental Weight among Male Births in the EDEN Cohort (France). Environ. Health Perspect. 2019, 127, 17002. [Google Scholar]
- Bistrian, A.; Staykova, C.; Avramova, A.; Polnareva, N. Autism Spectrum Disorders—Challenges of Classification, Diagnosis and Interventions. In Pediatric Aspects of Autism in the Light of Evidence Based Medicine; Ivanov, I., Pilosof, V., Eds.; Lax Book: Plovdiv, Bulgaria, 2016; pp. 122–133. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Burns, C.O.; Matson, J.L. An Evaluation of the Clinical Application of the DSM-5 for the Diagnosis of Autism Spectrum Disorder. Expert Rev. Neurother. 2017, 17, 909–917. [Google Scholar]
- Johnson, C.P.; Myers, S.M.; Council on Children with Disabilities. Identification and Evaluation of Children with Autism Spectrum Disorders. Pediatrics 2007, 120, 1183–1215. [Google Scholar]
- Myers, S.M.; Johnson, C.P. American Academy of Pediatrics Council on Children with Disabilities. Management of Children with Autism Spectrum Disorders. Pediatrics 2007, 120, 1162–1182. [Google Scholar]
- Lappé, M.; Lau, L.; Dudovitz, R.N.; Nelson, B.B.; Karp, E.A.; Kuo, A.A. The Diagnostic Odyssey of Autism Spectrum Disorder. Pediatrics 2018, 141, S272–S279. [Google Scholar]
- Kelly, B.; Williams, S.; Collins, S.; Mushtaq, F.; Mon-Williams, M.; Wright, B.; Mason, D.; Wright, J. The Association between Socioeconomic Status and Autism Diagnosis in the United Kingdom for Children Aged 5–8 Years of Age: Findings from the Born in Bradford Cohort. Autism 2019, 23, 131–140. [Google Scholar]
- Mazurek, M.O.; Handen, B.L.; Wodka, E.L.; Nowinski, L.; Butter, E.; Engelhardt, C.R. Age at First Autism Spectrum Disorder Diagnosis: The Role of Birth Cohort, Demographic Factors, and Clinical Features. J. Dev. Behav. Pediatr. 2014, 35, 561–569. [Google Scholar]
- Hyman, S.L.; Levy, S.E.; Myers, S.M.; AAP Council on Children with Disabilities, Section on Developmental and Behavioral Pediatrics. Identification, Evaluation, and Management of Children with Autism Spectrum Disorder. Pediatrics 2020, 145, E20193447. [Google Scholar]
- Gulati, S.; Kaushik, J.S.; Saini, L.; Sondhi, V.; Madaan, P.; Arora, N.K.; Pandey, R.M.; Jauhari, P.; Manokaran, R.K.; Sapra, S.; et al. Development and Validation of DSM-5 Based Diagnostic Tool for Children with Autism Spectrum Disorder. PLoS ONE 2019, 14, e0213242. [Google Scholar]
- UNICEF—Bulgaria. Early Childhood Development. Available online: https://www.unicef.bg/mobile/en/themes/view/slug/31 (accessed on 26 August 2020).
- Iskrov, G.; Vasilev, G.; Mitev, M.; Nikolova, R.; Stoykova, M.; Stefanov, R. Practice Patterns for Early Screening and Evaluation for Autism Spectrum Disorder Diagnosis in Bulgaria. J. Autism Dev. Disord. 2019. [Google Scholar] [CrossRef]
- Ivanov, I. Pediatric Examination of Children in Early and Pre-School Age with a Focus on Autism Spectrum Disorder (How to Screen so We Do Not Miss autism?). Pediatrics (Sofia) 2016, 56, 45–49. [Google Scholar]
- Robins, D.; Fein, D.; Barton, M.; Green, J. The Modified Checklist for Autism in Toddlers: An Initial Study Investigating Early Detection of Autism and Pervasive Developmental Disorders. J. Autism Dev. Disord. 2001, 31, 131–144. [Google Scholar]
- Matson, J.L.; Wilkins, J.; Fodstad, J.C. Children with Autism Spectrum Disorders: A Comparison of Those Who Regress vs. Those Who Don’t. Dev. Neurorehabil. 2010, 13, 37–45. [Google Scholar]
- Larsen, K.; Aasland, A.; Diseth, T.H. Identification of Symptoms of Autism Spectrum Disorders in the Second Year of Life at Day-Care Centers by Day-Care Staff: Step One in the Development of a Short Observation List. J. Autism Dev. Disord. 2018, 48, 2267–2277. [Google Scholar]
- Ivanov, I. Pediatric View of Autism: Significance, Frequency, Symptoms, Behavior. In Pediatric Aspects of Autism in the Light of Evidence Based Medicine; Ivanov, I., Pilosof, V., Eds.; Lax Book: Plovdiv, Bulgaria, 2016; pp. 9–38. [Google Scholar]
- Chlebowski, C.; Green, J.A.; Barton, M.L.; Fein, D. Using the Childhood Autism Rating Scale to Diagnose Autism Spectrum Disorders. J. Autism Dev. Disord. 2010, 40, 787–799. [Google Scholar]
- Park, E.-Y.; Kim, J. Factor Structure of the Childhood Autism Rating Scale as per DSM-5. Pediatr. Int. 2015, 58, 139–145. [Google Scholar]
- Adani, S.; Cepanec, M. Sex Differences in Early Communication Development: Behavioral and Neurobiological Indicators of More Vulnerable Communication System Development in Boys. J. Med. Croat. 2019, 60, 141–149. [Google Scholar]
- Steinhausen, H.C.; Jakobsen, H. Incidence Rates of Treated Mental Disorders in Childhood and Adolescence in a Complete Nationwide Birth Cohort. J. Clin. Psychiatry 2019, 80. [Google Scholar] [CrossRef]
- Schuck, R.K.; Flores, R.E.; Fung, L.K. Brief Report: Sex/Gender Differences in Symptomology and Camouflaging in Adults with Autism Spectrum Disorder. J. Autism Dev. Disord. 2019, 49, 2597–2604. [Google Scholar]
- Geelhand, P.; Bernard, P.; Klein, O.; van Tiel, B.; Kissine, M. The Role of Gender in the Perception of Autism Symptom Severity and Future Behavioral Development. Mol. Autism 2019, 10, 16. [Google Scholar]
- Ivanov, I.; Masaldzhieva, R. Structure and Development of Social Cognition: A Look Through the Achievements of Modern Neurosciences. In Abnormal Neuro-Psychic Development. More About Autism; Ivanov, I., Bozhinova, V., Pilosof, V., Eds.; Medical University—Plovdiv: Plovdiv, Bulgaria, 2018; pp. 105–125. [Google Scholar]
- Popov, N. Early Diagnosis of Autism Spectrum Disorder. In Pediatric Aspects of Autism in the Light of Evidence Based Medicine; Ivanov, I., Pilosof, V., Eds.; Lax Book: Plovdiv, Bulgaria, 2016; pp. 144–151. [Google Scholar]
- Bolton, P.F.; Golding, J.; Emond, A.; Steer, C.D. Autism Spectrum Disorder and Autistic Traits in the Avon Alignment Longitudinal Study of Parents and Children: Precursors and Early Signs. J. Am. Acad. Child Adolesc. Psychiatry. 2012, 51, 249–260. [Google Scholar]
- Mitchell, S.; Cardy, J.O.; Zwaigenbaum, L. Differentiating Autism Spectrum Disorder from Other Developmental Delays in the First Two Years of Life. Dev. Disabil. Res. Rev. 2011, 17, 130–140. [Google Scholar]
- National Collaborating Center for Women’s and Children’s Health (UK). Autism: Recognition, Referral and Diagnosis of Children and Young People on the Autism Spectrum; National Institute for Health and Clinical Excellence: Guidance; RCOG Press: London, UK, 2011. [Google Scholar]
- Lo, B.H.; Klopper, F.; Barnes, E.H.; Williams, K. Agreement between Concern about Autism Spectrum Disorder at the Time of Referral and Diagnosis, and Factors Associated with Agreement. J. Paediatr. Child Heal. 2017, 53, 742–748. [Google Scholar]
- Larsen, K. The Early Diagnosis of Preschool Children with Autism Spectrum Disorder in Norway: A Study of Diagnostic Age and Its Associated Factors. Scand. J. Child Adolesc. Psychiatry Psychol. 2015, 3, 136–145. [Google Scholar]
- Lord, C.; Risi, S.; DiLavore, P.S.; Shulman, C.; Thurm, A.; Pickles, A. Autism from 2 to 9 Years of Age. Arch. Gen. Psychiatry 2006, 63, 694–701. [Google Scholar]
- Sacrey, L.-A.R.; Bennett, J.A.; Zwaigenbaum, L. Early Infant Development and Intervention for Autism Spectrum Disorder. J. Child Neurol. 2015, 30, 1921–1929. [Google Scholar]
- Donohue, M.R.; Childs, A.W.; Richards, M.; Robins, D.L. Race Influences Parent Report of Concerns about Symptoms of Autism Spectrum Disorder. Autism 2019, 23, 100–111. [Google Scholar]
| Variable | n | % | |
|---|---|---|---|
| Sex | Male | 149 | 77.6 |
| Female | 43 | 22.4 | |
| Habitation | Urban | 170 | 88.5 |
| Rural | 22 | 11.5 | |
| Etiology | Idiopathic | 153 | 79.7 |
| Syndromic | 39 | 20.3 | |
| Developmental Delay/Intelectial Dysability (DD/ID) | Absent | 34 | 21.9 |
| Mild | 58 | 37.4 | |
| Moderate | 40 | 25.8 | |
| Severe | 16 | 10.3 | |
| Profound | 7 | 4.5 | |
| unmeasurable | 37 | - | |
| Language impairment | Present | 189 | 98.4 |
| Absent | 3 | 1.6 | |
| Epilepsy | Present | 33 | 17.2 |
| Absent | 159 | 82.8 | |
| Cerebral palsy | Present | 5 | 2.6 |
| Absent | 187 | 97.4 |
| ASD signs grouped in domains | n | % |
|---|---|---|
| Impairment of expressive language | 128 | 66.7 |
| language delay | 82 | 42.7 |
| language regression, including in babbling | 35 | 18.2 |
| does not engage in dialogue | 1 | 0.5 |
| idiosyncratic speech | 4 | 2.1 |
| Echolalia | 2 | 1.0 |
| monotonous vocalization or speech | 3 | 1.6 |
| speech stop | 1 | 0.5 |
| Receptive language impairment | 88 | 45.8 |
| does not turn when called by name, or turns rarely | 78 | 40.6 |
| does not execute simple commands | 6 | 3.1 |
| does not pay attention to conversation | 2 | 1.0 |
| late or missing visual search for an asked item | 2 | 1.0 |
| Impairment of non-verbal communication | 72 | 37.5 |
| eye contact—inconsistent, weak or missing | 68 | 35.4 |
| no reciprocal smile | 1 | 0.5 |
| stopped smiling | 1 | 0.5 |
| no facial expression | 1 | 0.5 |
| started waving goodbye late- after 2 years | 1 | 0.5 |
| Behavioral impairment | 53 | 27.6 |
| stereotypical behavior, spins or touched toys, rotates, etc. | 29 | 15.1 |
| episodes of strange behavior | 10 | 5.2 |
| aggressive behavior | 5 | 2.6 |
| affective spells with/without provocation | 5 | 2.6 |
| Hyperactivity | 2 | 1.0 |
| “talk to itself in front of the mirror” | 1 | 0.5 |
| compulsive behavior | 1 | 0.5 |
| Abnormal play | 17 | 8.9 |
| plays alone | 5 | 2.6 |
| does not play with children | 3 | 1.6 |
| monotonous play | 2 | 1.0 |
| licks toys or food | 2 | 1.0 |
| plays mostly with older ones | 1 | 0.5 |
| looks at the angles of objects | 1 | 0.5 |
| prefers playing with small balls | 1 | 0.5 |
| arranges toys in a circle | 1 | 0.5 |
| arranges toys | 1 | 0.5 |
| Restrictive interests | 15 | 7.8 |
| selectivity for food | 11 | 5.7 |
| no interest in new toys | 2 | 1.0 |
| does not want to be photographed | 1 | 0.5 |
| does not want to be touched | 1 | 0.5 |
| Abnormal or delayed communication development | 11 | 5.7 |
| “disturbed communication” | 5 | 2.6 |
| “gets upset when there are many people around” | 1 | 0.5 |
| not interested in children | 1 | 0.5 |
| hugs strangers | 1 | 0.5 |
| “became cool with no emotions” | 1 | 0.5 |
| difficult communication with peers | 1 | 0.5 |
| “impaired social integration” | 1 | 0.5 |
| Impaired joint attention | 4 | 2.1 |
| does not point with a finger | 2 | 1.0 |
| does not look in a pointed direction, or looks briefly | 2 | 1.0 |
| Criteria (A and B), symptoms (1–4) and signs: | n | % |
|---|---|---|
| A. Persistent deficits in social communication and social interaction across multiple contexts currently or by history: | 94 | 100.0 |
| 1 Deficit in socio-emotional reciprocity: | 94 | 100.0 |
| Missing or infrequent spontaneous or reciprocal smile | 89 | 94.7 |
| Lack of sharing emotion, interest or affect | 92 | 97.9 |
| Lack of interaction like give, show, request | 93 | 98.9 |
| Emotionally cool to loved ones | 87 | 92.6 |
| 2. Deficits in nonverbal communicative behaviors used for social interaction: | 94 | 100.0 |
| Abnormal visual contact | 92 | 97.9 |
| Failure to look in the finger-pointed direction | 92 | 97.9 |
| Lack of pointing with a finger to a wanted or interesting item | 91 | 96.8 |
| Poor facial expressions | 87 | 92.6 |
| Deficit in understanding gestures | 90 | 95.7 |
| Deficit in the use of gestures | 90 | 95.7 |
| Violation of privacy | 82 | 87.2 |
| 3. Deficits in developing, maintaining and understanding relationships: | 94 | 100.0 |
| Missing friendships | 84 | 89.4 |
| Lack of interest in peers | 89 | 94.7 |
| Prefers playing with older or younger | 89 | 94.7 |
| Lonely game | 88 | 93.6 |
| Lack of imaginary play (imitation of telephone conversation, driving a car, feeding a doll, etc.) | 90 | 95.7 |
| Lack of social reference (e.g., orientation by mother’s facial expression) | 89 | 94.7 |
| B. Restricted, repetitive patterns of behavior, interests, or activities currently or by history: | n | % |
| 1. Stereotyped or repetitive movements, use of objects, or speech: | 92 | 97.9 |
| Simple motor stereotypes | 90 | 95.7 |
| Arranges toys | 87 | 92.6 |
| Rotates objects | 86 | 91.5 |
| Monotone play | 90 | 95.7 |
| Lack of functional play | 89 | 94.7 |
| Idiosyncratic speech | 90 | 95.7 |
| Echolalia | 89 | 94.7 |
| Perseverations | 80 | 85.1 |
| 2. Insistence on sameness, inflexible adherence to routines, or ritualized patterns of verbal or nonverbal behavior | 89 | 94.7 |
| Prefers the same route when driven by car or walking | 85 | 90.4 |
| Prefers the same food | 87 | 92.6 |
| Extreme distress after small changes | 63 | 67.0 |
| 3. Highly restricted, fixated interests that are abnormal in intensity or focus: | 93 | 98.9 |
| Strong attachment to unusual objects | 83 | 88.3 |
| Lack of interest in reading books or telling stories | 89 | 94.7 |
| Lack or brief interest in new toys | 87 | 92.6 |
| 4. Hyper- or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment: | 89 | 94.7 |
| No response to a call by name | 59 | 62.8 |
| Closure of the ears with the hands in the absence of loud sound | 64 | 68.1 |
| No reaction to pain or fever | 57 | 60.6 |
| Excessive smelling or touching objects | 57 | 60.6 |
| Fascinated by light or movement | 56 | 59.6 |
| Other manifestations | 4 | 4.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ivanov, I.; Pacheva, I.; Timova, E.; Iordanova, R.; Galabova, F.; Gaberova, K.; Petkova, A.; Kotetarov, V.; Panova, M.; Tonchev, N.; et al. The Route to Autism Spectrum Diagnosis in Pediatric Practice in Bulgaria. Diagnostics 2021, 11, 106. https://doi.org/10.3390/diagnostics11010106
Ivanov I, Pacheva I, Timova E, Iordanova R, Galabova F, Gaberova K, Petkova A, Kotetarov V, Panova M, Tonchev N, et al. The Route to Autism Spectrum Diagnosis in Pediatric Practice in Bulgaria. Diagnostics. 2021; 11(1):106. https://doi.org/10.3390/diagnostics11010106
Chicago/Turabian StyleIvanov, Ivan, Iliyana Pacheva, Elena Timova, Ralitsa Iordanova, Fani Galabova, Katerina Gaberova, Aneliya Petkova, Vasil Kotetarov, Margarita Panova, Nikolay Tonchev, and et al. 2021. "The Route to Autism Spectrum Diagnosis in Pediatric Practice in Bulgaria" Diagnostics 11, no. 1: 106. https://doi.org/10.3390/diagnostics11010106
APA StyleIvanov, I., Pacheva, I., Timova, E., Iordanova, R., Galabova, F., Gaberova, K., Petkova, A., Kotetarov, V., Panova, M., Tonchev, N., & Franz, L. (2021). The Route to Autism Spectrum Diagnosis in Pediatric Practice in Bulgaria. Diagnostics, 11(1), 106. https://doi.org/10.3390/diagnostics11010106





