Anthropometric Measurements and Frailty in Patients with Liver Diseases
Abstract
1. Introduction
2. Patients and Methods
2.1. Patients
2.2. Statistical Considerations
3. Results
3.1. Baseline Features
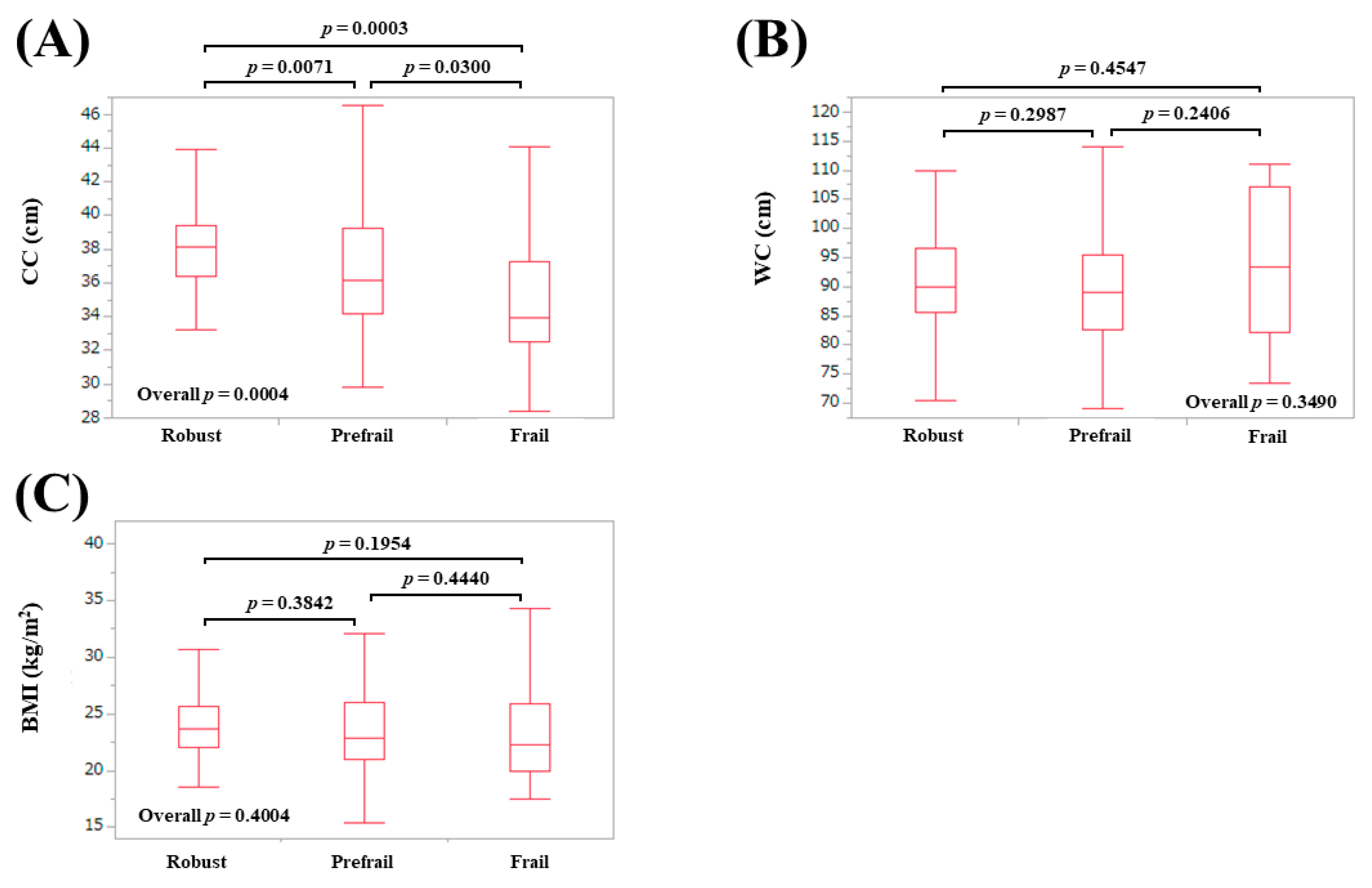
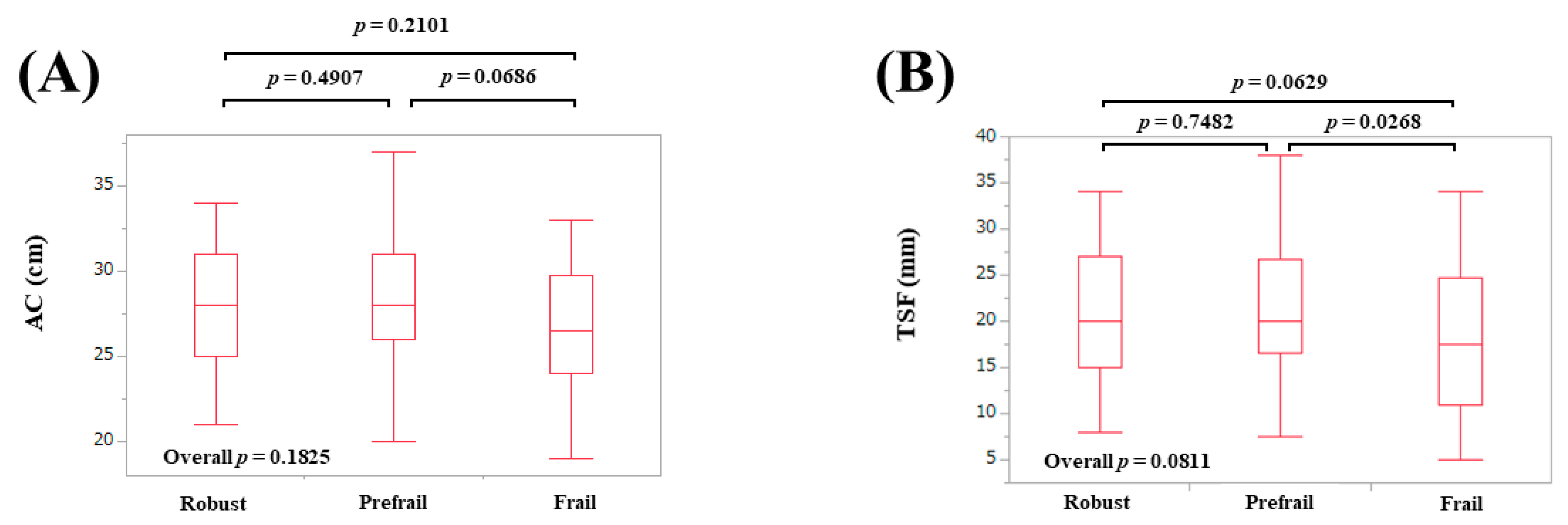
3.2. AMs According to Frailty Status in Males
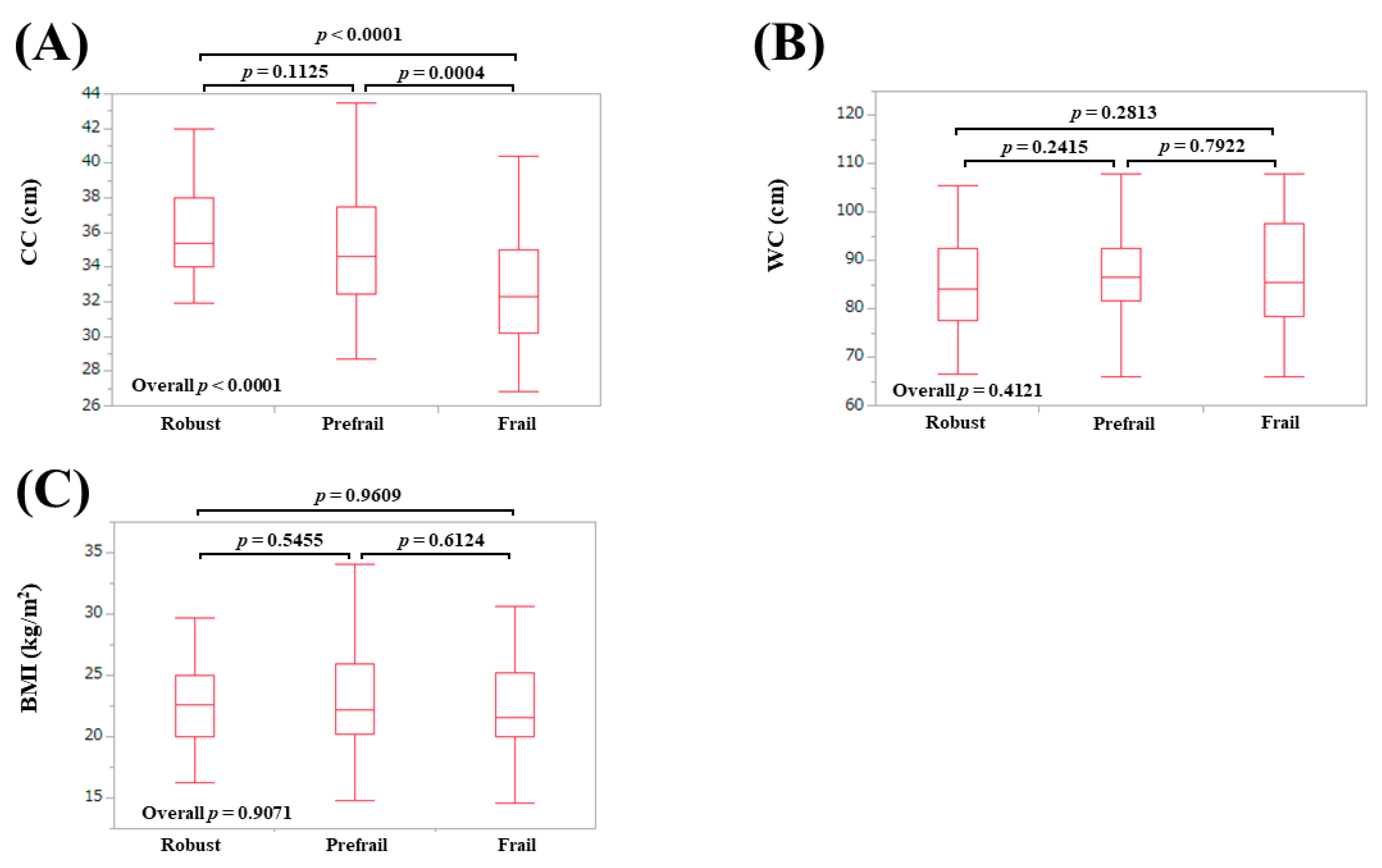
3.3. AMs According to Frailty Status in Females
3.4. AMs According to Frailty Phenotypes in Males
3.5. AMs According to Frailty Phenotypes in Females
3.6. ROC Analysis for the Presence of Frailty in Males
3.7. ROC Analysis for the Presence of Frailty in Females
3.8. Univariate and Multivariate Analyses of Factors Linked to Frailty in Males
3.9. Univariate and Multivariate Analyses of Factors Linked to Frailty in Females
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CLD | chronic liver disease |
| LC | liver cirrhosis |
| AM | anthropometric measurement |
| AC | arm circumference |
| CC | calf circumference |
| BMI | body mass index |
| TSF | triceps skinfold thickness |
| WC | waist circumference |
| AWGS | Asian Working Group for Sarcopenia |
| BW | body weight |
| GS | grip strength |
| WS | walking speed |
| ROC | receiver operating characteristic curve |
| AUC | area under the receiver operating characteristic curve |
| IQR | interquartile range |
| ALBI | albumin-bilirubin |
| OR | odds ratio |
| CI | confidence interval |
References
- Ribeiro, A.R.; Howlett, S.E.; Fernandes, A. Frailty-A promising concept to evaluate disease vulnerability. Mech. Ageing Dev. 2020, 187, 111217. [Google Scholar] [CrossRef]
- Satake, S.; Arai, H. Implications of frailty screening in clinical practice. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 4–10. [Google Scholar] [CrossRef]
- Sewo Sampaio, P.Y.; Sampaio, R.A.; Yamada, M.; Arai, H. Systematic review of the Kihon Checklist: Is it a reliable assessment of frailty? Geriatr. Gerontol. Int. 2016, 16, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Di Sabatino, A.; Lenti, M.V.; Cammalleri, L.; Corazza, G.R.; Pilotto, A. Frailty and the Gut. Dig. Liver Dis. 2018, 50, 533–541. [Google Scholar] [CrossRef]
- Williams, F.R.; Berzigotti, A.; Lord, J.M.; Lai, J.C.; Armstrong, M.J. Review Article: Impact of Exercise on Physical Frailty in Patients with Chronic Liver Disease. Aliment. Pharmacol. Ther. 2019, 50, 988–1000. [Google Scholar] [CrossRef]
- Bunchorntavakul, C.; Reddy, K.R. Review Article: Malnutrition/Sarcopenia and Frailty in Patients with Cirrhosis. Aliment. Pharmacol. Ther. 2020, 51, 64–77. [Google Scholar] [CrossRef]
- Wang, C.W.; Lebsack, A.; Chau, S.; Lai, J.C. The Range and Reproducibility of the Liver Frailty Index. Liver Transplant. 2019, 25, 841–847. [Google Scholar] [CrossRef]
- Laube, R.; Wang, H.; Park, L.; Heyman, J.K.; Vidot, H.; Majumdar, A.; Strasser, S.I.; McCaughan, G.W.; Liu, K. Frailty in Advanced Liver Disease. Liver Int. 2018, 38, 2117–2128. [Google Scholar] [CrossRef]
- Cameron, I.D.; Kurrle, S.E. Frailty and Rehabilitation. Interdiscip. Top. Gerontol. Geriatr. 2015, 41, 137–150. [Google Scholar] [PubMed]
- Vigorito, C.; Abreu, A.; Ambrosetti, M.; Belardinelli, R.; Corrà, U.; Cupples, M.; Davos, C.H.; Hoefer, S.; Iliou, M.C.; Schmid, J.P.; et al. Frailty and Cardiac Rehabilitation: A Call to Action from the EAPC Cardiac Rehabilitation Section. Eur. J. Prev. Cardiol. 2017, 24, 577–590. [Google Scholar] [CrossRef]
- Arjunan, A.; Peel, N.M.; Hubbard, R.E. Feasibility and validity of frailty measurement in geriatric rehabilitation. Australas. J. Ageing 2018, 37, 144–146. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.; Covinsky, K.E.; McCulloch, C.E.; Feng, S. The Liver Frailty Index Improves Mortality Prediction of the Subjective Clinician Assessment in Patients with Cirrhosis. Am. J. Gastroenterol. 2018, 113, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Bhanji, R.A.; Montano-Loza, A.J.; Watt, K.D. Sarcopenia in Cirrhosis: Looking beyond the skeletal muscle loss to see the systemic disease. Hepatology 2019, 70, 2193–2203. [Google Scholar] [CrossRef] [PubMed]
- Bhanji, R.A.; Narayanan, P.; Moynagh, M.R.; Takahashi, N.; Angirekula, M.; Kennedy, C.C.; Mara, K.C.; Dierkhising, R.A.; Watt, K.D. Differing Impact of Sarcopenia and Frailty in Nonalcoholic Steatohepatitis and Alcoholic Liver Disease. Liver Transpl. 2019, 25, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Madden, A.M.; Smith, S. Body composition and morphological assessment of nutritional status in adults: A review of anthropometric variables. J. Hum. Nutr. Diet. 2016, 29, 7–25. [Google Scholar] [CrossRef]
- Tur, J.A.; Bibiloni, M.D.M. Anthropometry, Body Composition and Resting Energy Expenditure in Human. Nutrients 2019, 14, 1891. [Google Scholar] [CrossRef] [PubMed]
- Diana, A.S.; John, A.D.; Catarina, N.M.; Paulo, M.R.; Cláudia, S.M.; David, B.A.; Luís, B.S.; Analiza, M.S. Reference values for body composition and anthropometric measurements in athletes. PLoS ONE 2014, 9, e97846. [Google Scholar]
- Utkualp, N.; Ercan, I. Anthropometric Measurements Usage in Medical Sciences. Biomed. Res. Int. 2015, 2015, 404261. [Google Scholar] [CrossRef]
- Liang-Kung, C.; Jean, W.; Prasert, A.; Tung-Wai, A.; Ming-Yueh, C.; Katsuya, I.; Hak, C.J.; Lin, K.; Miji, K.; Sunyoung, K.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307. [Google Scholar]
- Federico, A.; Caprio, G.G.; Dalise, A.M.; Barbieri, M.; Dallio, M.; Loguercio, C.; Paolisso, G.; Rizzo, M.R. Cirrhosis and Frailty Assessment in Elderly Patients: A Paradoxical Result. Medicine 2020, 99, e18501. [Google Scholar] [CrossRef]
- Hiroshi, F.; Hidetsugu, S.; Yoshiyuki, U.; Hirofumi, U.; Katsutoshi, O.; Isao, S.; Akitaka, S.; Masataka, S.; Sumiko, N.; Makoto, S.; et al. Evidence-based clinical practice guidelines for liver cirrhosis 2015. J. Gastroenterol. 2016, 51, 629–650. [Google Scholar]
- Lurie, Y.; Webb, M.; Cytter-Kuint, R.; Shteingart, S.; Lederkremer, G.Z. Non-invasive diagnosis of liver fibrosis and cirrhosis. World J. Gastroenterol. 2015, 21, 11567–11583. [Google Scholar] [CrossRef]
- Jean-Pierre, Z.; Nathalie, S.; Jérôme, G.; Adeline, P.; Elie-Serge, Z.; Tarik, A.; Renée-Claude, B.; Jean-Luc, B.; Dominique, G.; Jean-Charles, R.; et al. Comparison of nine blood tests and transient elastography for liver fibrosis in chronic hepatitis C: The ANRS HCEP-23 study. J. Hepatol. 2012, 56, 55–62. [Google Scholar]
- Romanelli, R.G.; Stasi, C. Recent Advancements in Diagnosis and Therapy of Liver Cirrhosis. Curr. Drug Targets 2016, 17, 1804–1817. [Google Scholar] [CrossRef]
- Nishikawa, H.; Yoh, K.; Enomoto, H.; Iwata, Y.; Sakai, Y.; Kishino, K.; Shimono, Y.; Ikeda, N.; Takashima, T.; Aizawa, N.; et al. Health-Related Quality of Life and Frailty in Chronic Liver Diseases. Life 2020, 10, 76. [Google Scholar] [CrossRef]
- Satake, S.; Arai, H. Chapter 1 Frailty: Definition, diagnosis, epidemiology. Geriatr. Gerontol. Int. 2020, 20, 7–13. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, H.; Shiraki, M.; Hiramatsu, A.; Moriya, K.; Hino, K.; Nishiguchi, S. Japan Society of Hepatology guidelines for sarcopenia in liver disease (1st edition): Recommendation from the working group for creation of sarcopenia assessment criteria. Hepatol. Res. 2016, 46, 951–963. [Google Scholar] [CrossRef] [PubMed]
- Enomoto, H.; Ueno, Y.; Hiasa, Y.; Nishikawa, H.; Hige, S.; Takikawa, Y.; Taniai, M.; Ishikawa, T.; Yasui, K.; Takaki, A.; et al. Transition in the Etiology of Liver Cirrhosis in Japan: A Nationwide Survey. J. Gastroenterol. 2020, 55, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Osaki, Y.; Nishikawa, H. Treatment for Hepatocellular Carcinoma in Japan Over the Last Three Decades: Our Experience and Published Work Review. Hepatol. Res. 2015, 45, 59–74. [Google Scholar] [CrossRef]
- Puneeta, T.; Navdeep, T.; Lesley, T.; Laura, Z.; Tahira, S.; Michelle, C.; Mang, M.; Robert, J.B.; Saumya, J.; Kelly, W.B.; et al. A rapid bedside screen to predict unplanned hospitalisation and death in outpatients with cirrhosis: A prospective evaluation of the clinical frailty score. Am. J. Gastroenterol. 2016, 111, 1759–1767. [Google Scholar]
- Sinclair, M.; Poltavskiy, E.; Dodge, J.; Lai, J. Frailty is independently associated with increased hospitalisation days in patients on the liver transplant waitlist. World J. Gastroenterol. 2017, 23, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Feng, S.; Terrault, N.; Lizaola, B.; Hayssen, H.; Covinsky, K. Frailty predicts waitlist mortality in liver transplant canddiates. Am. J. Transplant. 2014, 14, 1870–1879. [Google Scholar] [CrossRef] [PubMed]
- Ryoko, K.; Haruka, M.; Kiyoshi, S.; Noriko, T.; Susumu, S.; Izumi, T.; Mitsuru, H.; Motohiko, M. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr. Gerontol. Int. 2015, 15, 969–976. [Google Scholar]
- Nishikawa, H.; Yoh, K.; Enomoto, H.; Iwata, Y.; Sakai, Y.; Kishino, K.; Shimono, Y.; Ikeda, N.; Takashima, T.; Aizawa, N.; et al. Serum Zinc Level Is Associated with Frailty in Chronic Liver Diseases. J. Clin. Med. 2020, 9, 1570. [Google Scholar] [CrossRef] [PubMed]
- Rolland, Y.; Lauwers-Cances, V.; Cournot, M.; Nourhashémi, F.; Reynish, W.; Rivière, D.; Vellas, B.; Grandjean, H. Sarcopenia, calf circumference, and physical function of elderly women: Across-sectional study. J. Am. Geriatr. Soc. 2003, 51, 1120–1124. [Google Scholar] [CrossRef]
- Hawkins, K.L.; Zhang, L.; Ng, D.K.; Althoff, K.N.; Palella, F.J., Jr.; Kingsley, L.A.; Jacobson, L.P.; Margolick, J.B.; Lake, J.E.; Brown, T.T.; et al. Abdominal Obesity, Sarcopenia, and Osteoporosis Are Associated with Frailty in Men Living with and Without HIV. AIDS 2018, 32, 1257–1266. [Google Scholar] [CrossRef]
- Blaum, C.S.; Xue, Q.L.; Michelon, E.; Semba, R.D.; Fried, L.P. The Association Between Obesity and the Frailty Syndrome in Older Women: The Women’s Health and Aging Studies. J. Am. Geriatr. Soc. 2005, 53, 927–934. [Google Scholar] [CrossRef]

| Variables | Male (n = 183) | Female (n = 192) | p Value |
|---|---|---|---|
| Age (years) | 66 (53, 72) | 66 (55, 72.8) | 0.6237 |
| BMI (kg/m2) | 23.2 (21.4, 25.9) | 22.3 (20.1, 25.5) | 0.0136 |
| Etiologies, HBV/HCV/others | 45/72/66 | 22/106/64 | 0.0008 |
| Presence of LC, yes/no | 72/111 | 58/134 | 0.0660 |
| Total bilirubin (mg/dL) | 0.9 (0.6, 1.2) | 0.8 (0.6, 1.0) | 0.7926 |
| Serum albumin (g/dL) | 4.2 (3.9, 4.5) | 4.3 (4.0, 4.5) | 0.1711 |
| ALBI score | −2.86 (−3.1, −2.48) | −2.91 (−3.15, −2.68) | 0.0920 |
| ALBI grade, 1/2/3 | 125/54/4 | 155/33/4 | 0.0177 |
| Prothrombin time (%) | 90.5 (77.9, 100.4) | 93.1 (83.8, 100.1) | 0.0424 |
| Platelet count (× 104/mm3) | 16.5 (11.2, 21.4) | 18.1 (13.7, 22.9) | 0.0130 |
| AST (IU/L) | 26 (20, 36) | 24 (19, 31.8) | 0.2402 |
| ALT (IU/L) | 24 (16, 39) | 17 (13, 26) | 0.0456 |
| GS (kg) | 33.3 (28.0, 39.0) | 21.0 (17.7, 24.5) | <0.0001 |
| WS (m/s) | 1.28 (1.08, 1.44) | 1.32 (1.16, 1.47) | 0.4618 |
| Presence of frailty, yes/no | 22/161 | 28/164 | 0.5439 |
| Arm circumference (cm) | 28 (26, 30) | 28 (25, 30.8) | 0.1688 |
| Triceps skin fold thickness (mm) | 12 (9, 16) | 20 (15, 27) | <0.0001 |
| Calf circumference (cm) | 36.9 (34.4, 39.2) | 34.8 (32.7, 37.4) | <0.0001 |
| Waist circumference (cm) | 89.5 (83.5, 97.0) | 85.8 (80, 92.5) | <0.0001 |
| WS Decrease | WS Non-Decrease | p Value | |
|---|---|---|---|
| AC | 27 (23.5, 29) | 28 (27, 30) | 0.0100 |
| TSF | 1.25 (0.91, 1.58) | 1.15 (0.9, 1.6) | 0.6785 |
| CC | 34.7 (32.9, 38.6) | 37.1 (34.7, 39.4) | 0.0339 |
| WC | 89.9 (81.6, 102.2) | 89.5 (84, 96.5) | 0.5781 |
| BMI | 22.2 (19.9, 25.8) | 23.5 (21.6, 25.9) | 0.2859 |
| GS Decrease | GS Non-Decrease | p Value | |
| AC | 26 (25, 28) | 29 (27, 30.8) | <0.0001 |
| TSF | 1.15 (0.85, 1.5) | 1.2 (0.91, 1.6) | 0.3758 |
| CC | 34.2 (32.9, 36.1) | 37.7 (35.5, 39.6) | <0.0001 |
| WC | 89 (80.6, 96) | 90 (84.2, 97.4) | 0.2324 |
| BMI | 21.8 (19.8, 24.6) | 23.7 (21.7, 26) | 0.0037 |
| Fatigue, Yes | Fatigue, No | p Value | |
| AC | 28 (26, 30) | 28 (27, 30) | 0.1255 |
| TSF | 1.2 (0.9, 1.6) | 1.2 (0.93, 1.6) | 0.7026 |
| CC | 36.1 (33.8, 39.2) | 37.6 (34.7, 39.3) | 0.1705 |
| WC | 89.1 (82.7, 97.8) | 89.8 (84.3, 96.3) | 0.5509 |
| BMI | 22.8 (20.6, 25.9) | 23.6 (21.8, 25.7) | 0.3683 |
| BW Loss, Yes | BW Loss, No | p Value | |
| AC | 27 (23, 29.8) | 29 (27, 30) | 0.1929 |
| TSF | 0.8 (0.65, 1.38) | 1.2 (0.95, 1.6) | 0.2430 |
| CC | 34.5 (32.1, 40.9) | 37.4 (35.5, 39.4) | 0.1738 |
| WC | 89 (82.8, 102.9) | 89.5 (84, 96.5) | 0.8760 |
| BMI | 21.0 (19.2, 26.3) | 23.5 (21.7, 25.7) | 0.1974 |
| PA Decline, Yes | PA Decline, No | p Value | |
| AC | 28 (26, 30) | 28.5 (27, 30) | 0.0278 |
| TSF | 1.1 (0.89, 1.6) | 1.2 (0.95, 1.6) | 0.2382 |
| CC | 36.0 (33.8, 39.1) | 37.4 (35, 39.4) | 0.0224 |
| WC | 92 (82.1, 100.9) | 89 (84, 96.4) | 0.5377 |
| BMI | 23.5 (21.7, 25.8) | 23.5 (21.6, 25.9) | 0.3143 |
| WS Decrease | WS Non-Decrease | p Value | |
|---|---|---|---|
| AC | 27 (25, 29) | 28 (25, 31) | 0.0704 |
| TSF | 1.7 (1.2, 2.4) | 2.0 (1.6, 2.7) | 0.0247 |
| CC | 32.4 (30.8, 34.4) | 35.1 (33.2, 37.5) | 0.0002 |
| WC | 85 (80, 92.5) | 85.9 (80.2, 92.7) | 0.8582 |
| BMI | 22.4 (20.1, 23.8) | 22.2 (20.1, 25.9) | 0.3477 |
| GS Decrease | GS Non-Decrease | p Value | |
| AC | 27 (25, 29.3) | 28 (25, 31) | 0.0536 |
| TSF | 2.0 (1.35, 2.6) | 2.0 (1.6, 2.7) | 0.2259 |
| CC | 33.3 (31.1, 35.8) | 35.1 (33.5, 37.8) | 0.0002 |
| WC | 86 (79.8, 92.1) | 85.5 (80. 93.5) | 0.9234 |
| BMI | 21.7 (20.1, 24.7) | 22.7 (20, 25.8) | 0.6682 |
| Fatigue, Yes | Fatigue, No | p Value | |
| AC | 27 (25, 31) | 28 (26, 30) | 0.5815 |
| TSF | 1.95 (1.4, 2.8) | 2.1 (1.7, 2.6) | 0.2723 |
| CC | 34.5 (31.8, 37.4) | 35.0 (33.5, 37.4) | 0.0718 |
| WC | 86 (78.7, 94) | 85.3 (81.1, 92.3) | 0.7912 |
| BMI | 21.7 (19.8, 26.1) | 22.7 (20.4, 24.8) | 0.7081 |
| BW Loss, Yes | BW Loss, No | p Value | |
| AC | 27 (24, 29) | 28 (25, 31) | 0.2554 |
| TSF | 1.8 (1.2, 2.15) | 2.0 (1.5, 2.7) | 0.0920 |
| CC | 33.1 (31.4, 35.1) | 34.9 (32.9, 37.5) | 0.0637 |
| WC | 89.5 (78, 95) | 85.7 (80, 92.5) | 0.6643 |
| BMI | 23 (20.5, 25.8) | 22.2 (20, 25.5) | 0.9613 |
| PA Decline, Yes | PA Decline, No | p Value | |
| AC | 27.5 (26, 31) | 28 (25, 30) | 0.4672 |
| TSF | 2.15 (1.53, 2.89) | 2.0 (1.5, 2.6) | 0.4689 |
| CC | 34.6 (32.0, 35.9) | 34.9 (33.0, 37.9) | 0.1211 |
| WC | 88 (83.1, 93.3) | 85 (78.5, 92.4) | 0.1304 |
| BMI | 22.9 (20.2, 25.6) | 22.2 (20, 25.4) | 0.5102 |
| Male | AUC | Cutoff | Sensitivity | Specificity |
|---|---|---|---|---|
| AC | 0.676 | 26.4 cm | 0.546 | 0.764 |
| TSF | 0.565 | 7 mm | 0.273 | 0.913 |
| CC | 0.693 | 33.7 cm | 0.500 | 0.663 |
| WC | 0.570 | 95.2 cm | 0.500 | 0.733 |
| BMI | 0.575 | 21.4 kg/m2 | 0.500 | 0.776 |
| Female | AUC | Cutoff | Sensitivity | Specificity |
| AC | 0.599 | 27.6 cm | 0.679 | 0.512 |
| TSF | 0.620 | 12 mm | 0.357 | 0.884 |
| CC | 0.734 | 33.4 cm | 0.714 | 0.750 |
| WC | 0.528 | 98.4 cm | 0.250 | 0.908 |
| BMI | 0.525 | 21.6 kg/m2 | 0.536 | 0.579 |
| Male | Univariate | Multivariate Analysis | ||
|---|---|---|---|---|
| p Value | OR | 95% CI | p Value | |
| Age | 0.0126 | 0.989 | 0.943–1.037 | 0.6389 |
| BMI | 0.3000 | - | - | - |
| Presence of LC | 0.0003 | 0.281 | 0.082–0.962 | 0.0433 |
| Total bilirubin | 0.9262 | - | - | - |
| Serum albumin | <0.0001 | 2.082 | 0.781–5.553 | 0.1428 |
| Prothrombin time | 0.3345 | - | - | - |
| Platelet count | 0.0669 | - | - | - |
| AST | 0.6275 | - | - | - |
| ALT | 0.9838 | - | - | - |
| Arm circumference | 0.0038 | 1.022 | 0.766–1.362 | 0.8835 |
| Triceps skin fold thickness | 0.3222 | - | - | - |
| Calf circumference | 0.0056 | 1.129 | 0.867–1.470 | 0.3675 |
| Waist circumference | 0.2073 | - | - | - |
| Female | Univariate | Multivariate Analysis | ||
| pValue | OR | 95% CI | pValue | |
| Age | 0.0188 | 0.987 | 0.947–1.030 | 0.5514 |
| BMI | 0.7283 | - | - | - |
| Presence of LC | 0.0003 | 0.462 | 0.157–1.361 | 0.1615 |
| Total bilirubin | 0.8808 | - | - | - |
| Serum albumin | 0.0010 | 2.617 | 0.998–6.864 | 0.0444 |
| Prothrombin time | 0.4101 | - | - | - |
| Platelet count | 0.3379 | - | - | - |
| AST | 0.1093 | - | - | - |
| ALT | 0.5371 | - | - | - |
| Arm circumference | 0.0491 | 1.186 | 0.869–1.620 | 0.2793 |
| Triceps skin fold thickness | 0.0263 | 1.004 | 0.883–1.141 | 0.9539 |
| Calf circumference | <0.0001 | 1.524 | 1.172–1.983 | 0.0010 |
| Waist circumference | 0.528 | - | - | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nishikawa, H.; Yoh, K.; Enomoto, H.; Ikeda, N.; Aizawa, N.; Koriyama, T.; Nishimura, T.; Nishiguchi, S.; Iijima, H. Anthropometric Measurements and Frailty in Patients with Liver Diseases. Diagnostics 2020, 10, 433. https://doi.org/10.3390/diagnostics10060433
Nishikawa H, Yoh K, Enomoto H, Ikeda N, Aizawa N, Koriyama T, Nishimura T, Nishiguchi S, Iijima H. Anthropometric Measurements and Frailty in Patients with Liver Diseases. Diagnostics. 2020; 10(6):433. https://doi.org/10.3390/diagnostics10060433
Chicago/Turabian StyleNishikawa, Hiroki, Kazunori Yoh, Hirayuki Enomoto, Naoto Ikeda, Nobuhiro Aizawa, Takashi Koriyama, Takashi Nishimura, Shuhei Nishiguchi, and Hiroko Iijima. 2020. "Anthropometric Measurements and Frailty in Patients with Liver Diseases" Diagnostics 10, no. 6: 433. https://doi.org/10.3390/diagnostics10060433
APA StyleNishikawa, H., Yoh, K., Enomoto, H., Ikeda, N., Aizawa, N., Koriyama, T., Nishimura, T., Nishiguchi, S., & Iijima, H. (2020). Anthropometric Measurements and Frailty in Patients with Liver Diseases. Diagnostics, 10(6), 433. https://doi.org/10.3390/diagnostics10060433




