Feasibility of Strip Meniscometry for Tear Volume Evaluation in Lacrimal Passage Obstruction
Abstract
1. Introduction
2. Materials and Methods
2.1. In Vitro Experiment
= 30 mm × 0.10 mm2 × 1.294
= 3.882 mm3 = 3.882 μL
2.2. Clinical Study
2.2.1. Patients/Subjects
2.2.2. SMTube Measurement
2.2.3. Measurement of Tear Meniscus Using AS-OCT
2.2.4. Subjective Symptoms Questionnaire
2.2.5. Dacryoendoscopic Surgery with Lacrimal Tube Intubation
2.2.6. Dacryocystorhinostomy Technique
2.3. Statistical Analyses
3. Results
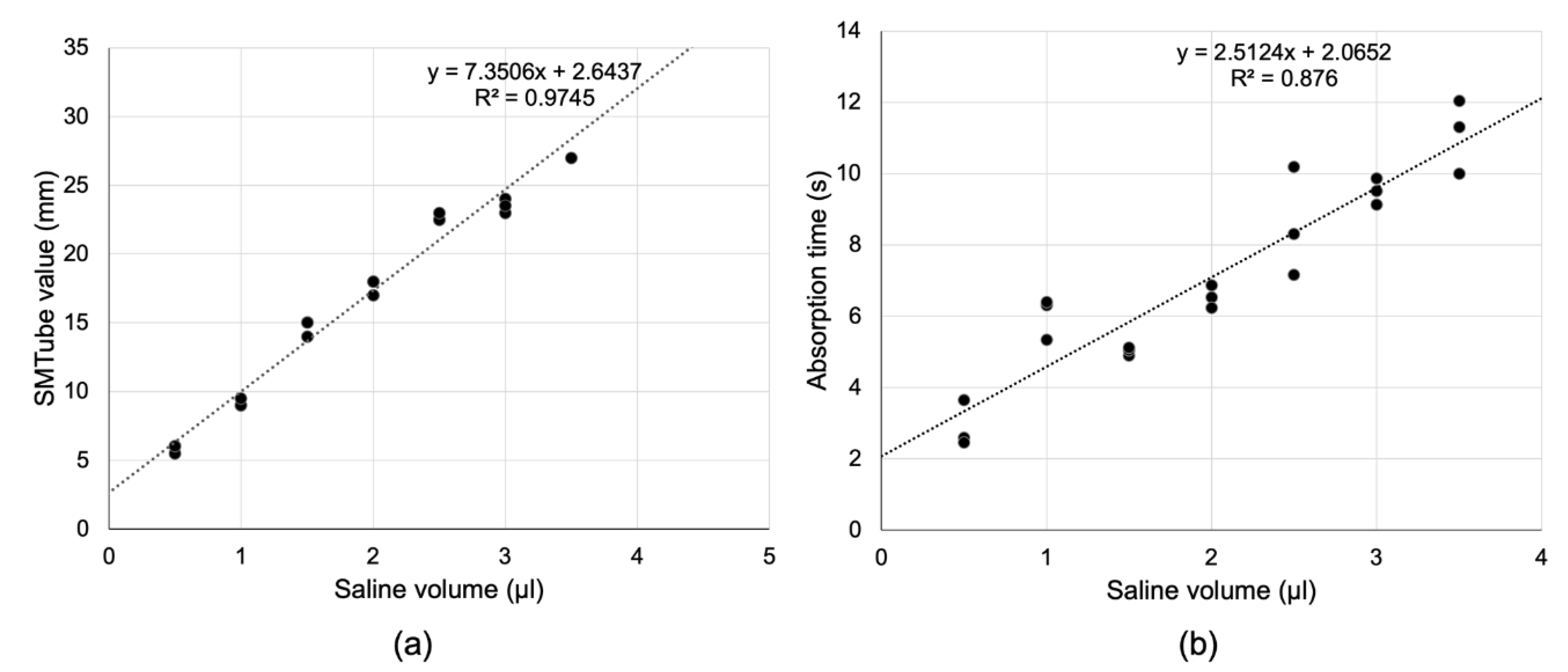
3.1. In Vitro Experiment
3.2. Clinical Study
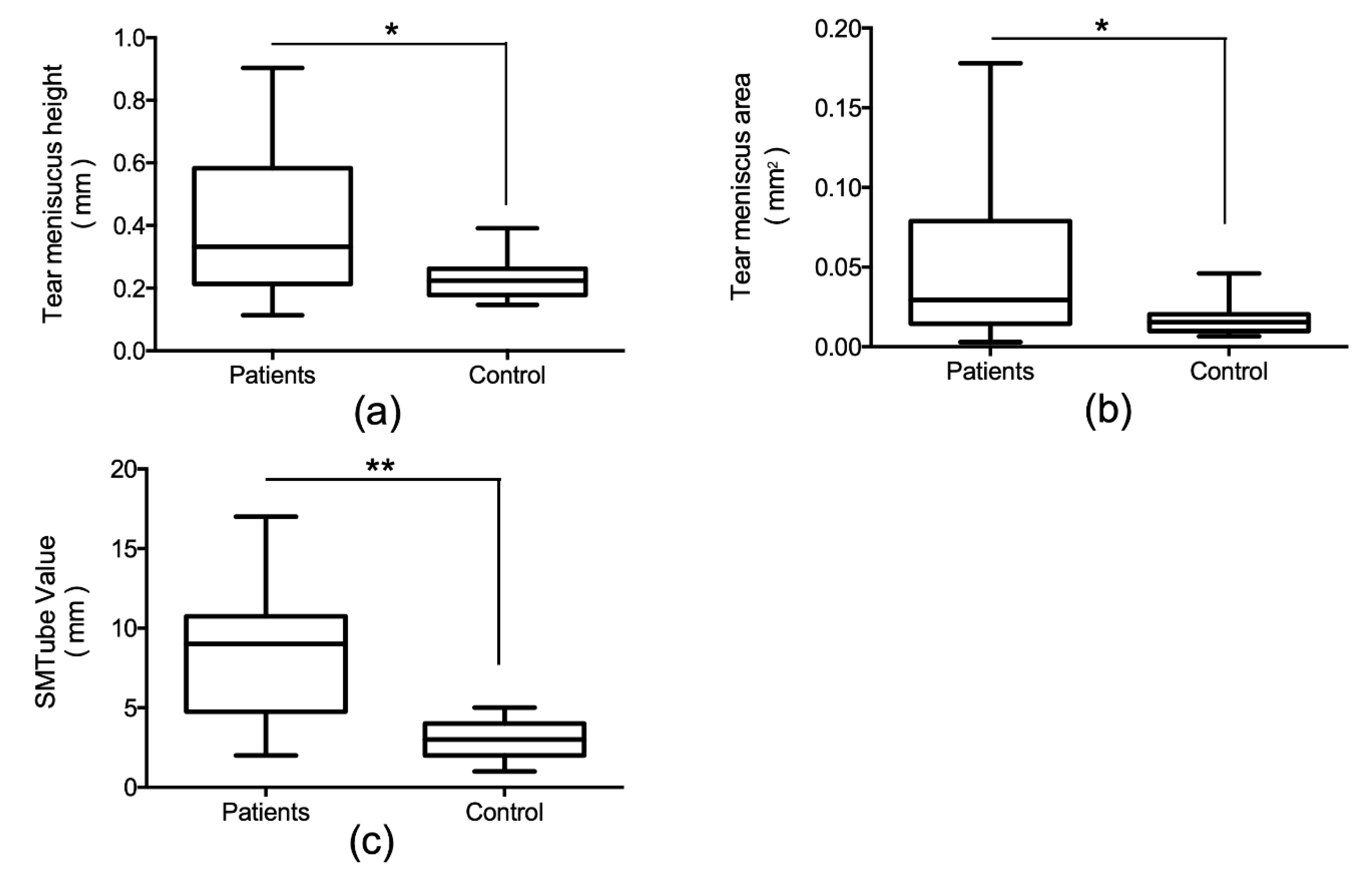
3.2.1. Comparison between Control Subjects and Patients
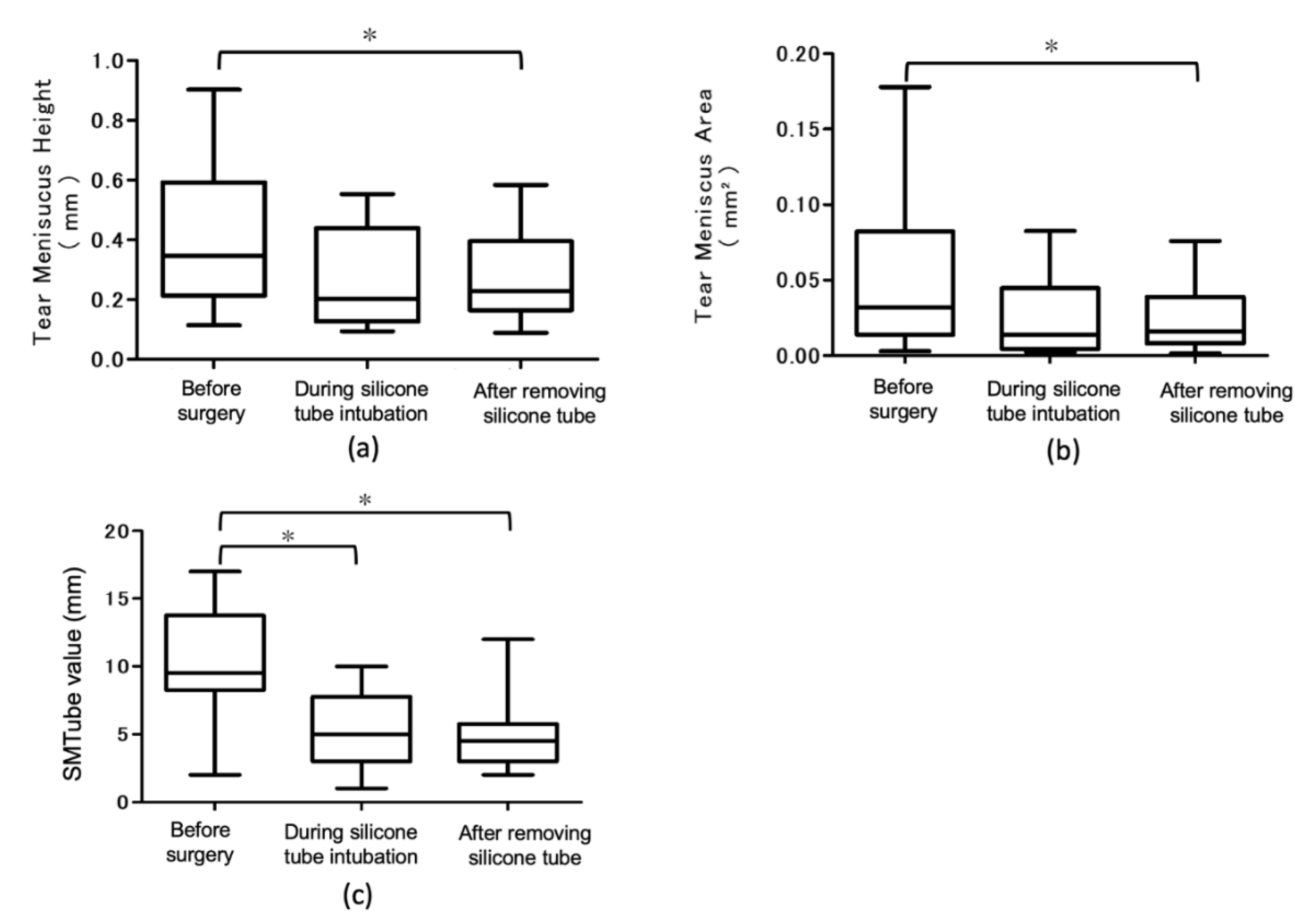
3.2.2. Time-Course Changes of TMH, TMA, and SMTube Values before and after Treatment in Patients with Lacrimal Passage Obstruction
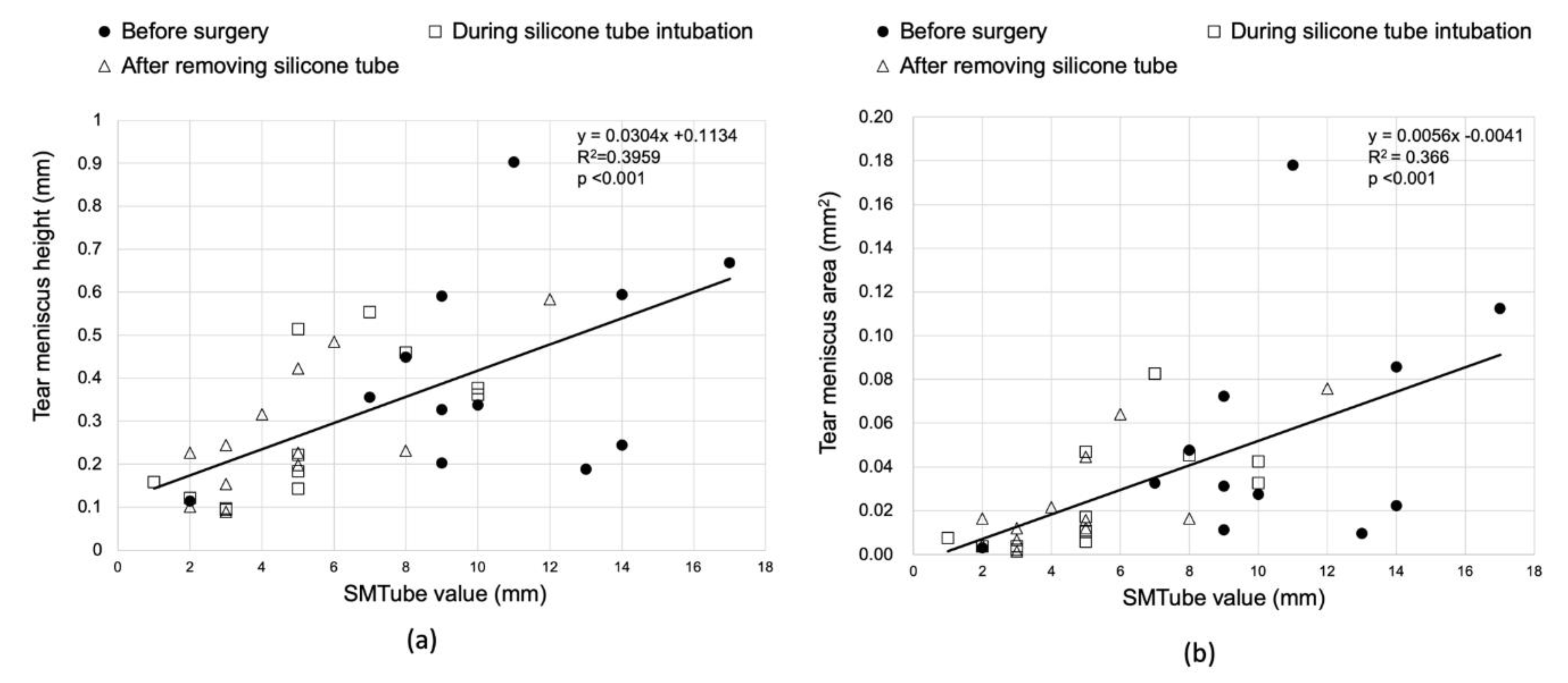
3.2.3. Correlation between the Anterior Segment OCT Parameters and SMTube Values
3.2.4. Correlation between the Patient Questionnaire and Anterior Segment OCT Parameters/SMTube Value
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Koh, S.; Inoue, Y.; Ochi, S.; Takai, Y.; Maeda, N.; Nishida, K. Quality of vision in eyes with epiphora undergoing lacrimal passage intubation. Am. J. Ophthalmol. 2017, 181, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Kabata, Y.; Goto, S.; Takahashi, G.; Tsuneoka, H. Vision-related quality of life in patients undergoing silicone tube intubation for lacrimal passage obstructions. Am. J. Ophthalmol. 2011, 152, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.; Li, J.; Wang, J.; Ma, H.; Cai, C.; Tao, A.; Yuan, Y.; Lu, F. Upper and lower tear menisci in the diagnosis of dry eye. Investig. Ophthalmol. Vis. Sci. 2009, 50, 2722–2726. [Google Scholar] [CrossRef] [PubMed]
- Mainstone, J.C.; Bruce, A.S.; Golding, T.R. Tear meniscus measurement in the diagnosis of dry eye. Curr. Eye Res. 1996, 15, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Holly, F.J. Physical chemistry of the normal and disordered tear film. Trans. Ophthalmol. Soc. UK 1985, 104, 374–380. [Google Scholar] [PubMed]
- Singh, S.; Rajput, A.; Mohamed, A.; Mittal, V. Spectral domain optical coherence tomography for measuring tear film meniscus height and its relationship with epiphora. Indian J. Ophthalmol. 2018, 66, 1592–1594. [Google Scholar] [CrossRef] [PubMed]
- Kojima, T.; Matsumoto, Y.; Ibrahim, O.M.; Wakamatsu, T.H.; Dogru, M.; Tsubota, K. Evaluation of a thermosensitive atelocollagen punctal plug treatment for dry eye disease. Am. J. Ophthalmol. 2014, 157, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, O.M.; Dogru, M.; Ward, S.K.; Matsumoto, Y.; Wakamatsu, T.H.; Ishida, K.; Tsuyama, A.; Kojima, T.; Shimazaki, J.; Tsubota, K. The efficacy, sensitivity, and specificity of strip meniscometry in conjunction with tear function tests in the assessment of tear meniscus. Investig. Ophthalmol. Vis. Sci. 2011, 52, 2194–2198. [Google Scholar] [CrossRef] [PubMed]
- Dogru, M.; Ishida, K.; Matsumoto, Y.; Goto, E.; Ishioka, M.; Kojima, T.; Goto, T.; Saeki, M.; Tsubota, K. Strip meniscometry: A new and simple method of tear meniscus evaluation. Investig. Ophthalmol. Vis. Sci. 2006, 47, 1895–1901. [Google Scholar] [CrossRef] [PubMed]
- Shinzawa, M.; Dogru, M.; Miyasaka, K.; Shimazaki, J.; Sekiryu, T. Application of CASIA SS-1000 optical coherence tomography tear meniscus imaging in testing the efficacy of new strip meniscometry in dry eye diagnosis. Eye Contact Lens 2018, 44, S44–S49. [Google Scholar] [CrossRef] [PubMed]
- Park, D.I.; Lew, H.; Lee, S.Y. Tear meniscus measurement in nasolacrimal duct obstruction patients with Fourier-domain optical coherence tomography: Novel three-point capture method. Acta Ophthalmol. 2012, 90, 783–787. [Google Scholar] [CrossRef] [PubMed]
- Palakuru, J.R.; Wang, J.; Aquavella, J.V. Effect of blinking on tear dynamics. Investig. Ophthalmol. Vis. Sci. 2007, 48, 3032–3037. [Google Scholar] [CrossRef] [PubMed]
- Ueda, K.; Watanabe, A.; Yokoi, N.; Sugimoto, M.; Fukuoka, H.; Shinomiya, K.; Kinoshita, S.; Rajak, S.; Selva, D. Biopsy of recurrent nasolacrimal duct obstruction using sheath-guided dacryoendoscopy. Orbit 2019, 38, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Yokoi, N.; Bron, A.; Tiffany, J.; Brown, N.; Hsuan, J.; Fowler, C. Reflective meniscometry: A non-invasive method to measure tear meniscus curvature. Br. J. Ophthalmol. 1999, 83, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, O.M.; Dogru, M.; Takano, Y.; Satake, Y.; Wakamatsu, T.H.; Fukagawa, K.; Tsubota, K.; Fujishima, H. Application of visante optical coherence tomography tear meniscus height measurement in the diagnosis of dry eye disease. Ophthalmology 2010, 117, 1923–1929. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osawa, I.; Esaka, Y.; Kojima, T.; Simsek, C.; Kudo, H.; Dogru, M. Feasibility of Strip Meniscometry for Tear Volume Evaluation in Lacrimal Passage Obstruction. Diagnostics 2020, 10, 179. https://doi.org/10.3390/diagnostics10040179
Osawa I, Esaka Y, Kojima T, Simsek C, Kudo H, Dogru M. Feasibility of Strip Meniscometry for Tear Volume Evaluation in Lacrimal Passage Obstruction. Diagnostics. 2020; 10(4):179. https://doi.org/10.3390/diagnostics10040179
Chicago/Turabian StyleOsawa, Ikubun, Yuri Esaka, Takashi Kojima, Cem Simsek, Haruka Kudo, and Murat Dogru. 2020. "Feasibility of Strip Meniscometry for Tear Volume Evaluation in Lacrimal Passage Obstruction" Diagnostics 10, no. 4: 179. https://doi.org/10.3390/diagnostics10040179
APA StyleOsawa, I., Esaka, Y., Kojima, T., Simsek, C., Kudo, H., & Dogru, M. (2020). Feasibility of Strip Meniscometry for Tear Volume Evaluation in Lacrimal Passage Obstruction. Diagnostics, 10(4), 179. https://doi.org/10.3390/diagnostics10040179






