A Randomized Comparison of Non-Channeled GlidescopeTM Titanium Versus Channeled KingVisionTM Videolaryngoscope for Orotracheal Intubation in Obese Patients with BMI > 35 kg·m−2
Abstract
1. Introduction
2. Materials and Methods
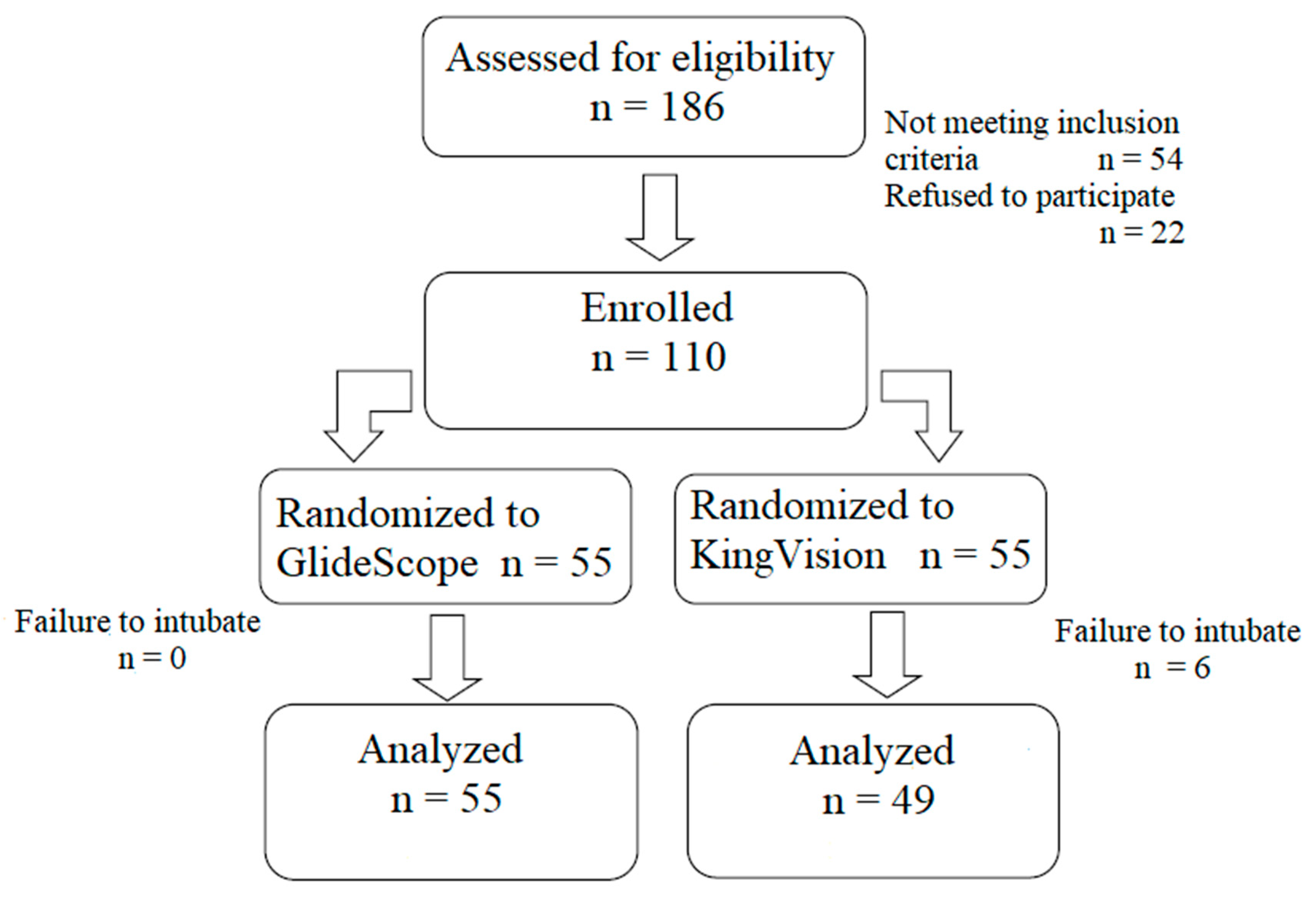
2.1. Study Design
2.2. Study Participants
2.3. Investigators, Their Preparation and Training
2.4. Randomization and Blinding
2.5. Procedures
2.6. Outcome Measures
2.7. Statistical Analysis
3. Results
3.1. Demographic Parameters
3.2. Primary Outcome
3.3. Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity and Severe Obesity among Adults: United States 2017–2018; NCHS Data Brief, no. 360; National Center for Health Statistics: Hyattsville, MD, USA, 2020. [Google Scholar]
- Marques, A.; Peralta, M.; Naia, A.; Loureiro, N.; de Matos, M.G. Prevalence of adult overweight and obesity in 20 European countries, 2014. Eur. J. Public Health 2018, 28, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Abdelaal, M.; le Roux, C.W.; Docherty, N.G. Morbidity and mortality associated with obesity. Ann. Transl. Med. 2017, 5, 161. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.S. Airway management and morbid obesity. Eur. J. Anaesthesiol. 2010, 27, 923–927. [Google Scholar] [CrossRef] [PubMed]
- Juvin, P.; Lavaut, E.; Dupont, H.; Lefevre, P.; Demetriou, M.; Dumoulin, J.L.; Desmonts, J.M. Difficult tracheal intubation is more common in obese than in lean patients. Anesth. Analg. 2003, 97, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Yumul, R.; Elvir-Lazo, O.L.; White, P.F.; Sloninsky, A.; Kaplan, M.; Kariger, R.; Naruse, R.; Parker, N.; Pham, C.; Zhang, X.; et al. Comparison of three video laryngoscopy devices to direct laryngoscopy for intubating obese patients: A randomized controlled trial. J. Clin. Anesth. 2016, 31, 71–77. [Google Scholar] [CrossRef]
- Marrel, J.; Blanc, C.; Frascarolo, P.; Magnusson, I. Videolaryngoscopy improves intubation condition in morbidly obese patients. Eur. J. Anesthesiol. 2007, 24, 1045–1049. [Google Scholar] [CrossRef]
- Andersen, L.H.; Rovsing, L.; Olsen, K.S. GlideScope videolaryngoscope vs. Macintosh direct laryngoscope for intubation of morbidly obese patients: A randomized trial. Acta Anaesthesiol. Scand. 2011, 55, 1090–1097. [Google Scholar] [CrossRef]
- Yousef, G.T.; Abdalgalil, D.A.; Ibrahim, T.H. Orotracheal intubation of morbidly obese patients, comparison of GlideScope video laryngoscope and the LMA CTrach with direct laryngoscopy. Anesth. Essays Res. 2012, 6, 174–179. [Google Scholar] [CrossRef]
- Hoshijima, H.; Denawa, Y.; Tominaga, A.; Nakamura, C.; Shiga, T.; Nagasaka, H. Videolaryngoscope versus Macintosh laryngoscope for tracheal intubation in adults with obesity: A systematic review and meta-analysis. J. Clin. Anesth. 2018, 44, 69–75. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010, 8, 18. [Google Scholar] [CrossRef]
- Piaggio, G.; Elbourne, D.R.; Pocock, S.J.; Evans, S.J.; Altman, D.G.; CONSORT Group. Reporting of noninferiority and equivalence rnadomized trials: Extension of the CONSORT 2010 statement. JAMA 2012, 308, 2594–2604. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, C.E.; Margarson, M.P.; Shearer, E.; Redman, J.W.; Lucas, D.N.; Cousins, J.M.; Fox, W.T.; Kennedy, N.J.; Venn, P.J.; Skues, M.; et al. Peri-operative management of the obese surgical patient 2015. Anaesthesia 2015, 70, 859–876. [Google Scholar] [PubMed]
- Frerk, C.; Mitchell, V.S.; McNarry, A.F.; Mendonca, C.; Bhagrath, R.; Patel, A.; O’Sullivan, E.P.; Woodall, N.M.; Ahmad, I. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br. J. Anaesth. 2015, 115, 827–848. [Google Scholar] [CrossRef] [PubMed]
- Yentis, S.M.; Lee, D.J. Evaluation of an improved scoring system for the grading of direct laryngoscopy. Anaesthesia 1998, 53, 1041–1044. [Google Scholar] [CrossRef] [PubMed]
- Adnet, F.; Borron, S.W.; Racine, S.X.; Clemessy, J.L.; Fournier, J.L.; Plaisance, P.; Lapandry, C. The intubation difficulty scale (IDS). Proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology 1997, 87, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
- Ydemann, M.; Rovsing, L.; Lindekaer, A.L.; Olsen, K.S. Intubation of the morbidly obese patients: GlideScope® vs. FastrachTM. Acta Anaesthesiol. Scand. 2012, 56, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Maassen, R.; Lee, R.; Hermans, B.; Marcus, M.; van Zundert, A. A comparison of three videolaryngoscopes: The Macintosh blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesth. Analg. 2009, 109, 1560–1565. [Google Scholar] [CrossRef]
- Abdelmalak, B.B.; Bernstein, E.; Egan, C.; Abdallah, R.; You, J.; Sessler, D.I.; Doyle, D.J. GlideScope® vs flexible fibreoptic scope for elective intubation in obese patients. Anaesthesia 2011, 66, 550–555. [Google Scholar] [CrossRef]
- Cagnazzi, E.; Mosca, A.; Pe, F.; Togazzari, T.; Manenti, O.; Mittemperger, F.; Raffetti, E.; Donato, F.; Latronico, N. Near-zero difficult tracheal intubation and tracheal intubation failure rate with the “Besta Airway Algorithm” and “Glidescope in morbidly obese” (GLOBE). Minerva Anestesiol. 2016, 82, 966–973. [Google Scholar]
- Ander, F.; Magnuson, A.; Berggren, L.; Ahlstrand, R.; de Leon, A. Time-to-intubation in obese patients. A randomized study comparing direct laryngoscopy and videolaryngoscopy in experienced anesthetists. Minerva Anestesiol. 2017, 83, 906–913. [Google Scholar]
- Sahajanandan, R.; Dhanyee, A.S.; Gautam, A.K. A comparison of King Vision video laryngoscope with CMAC D-blade in obese patients with anticipated difficult airway in tertiary hospital in India—Randomized controlled study. J. Anaesthesiol. Clin. Pharmacol. 2019, 35, 363–367. [Google Scholar] [PubMed]
- Kleine-Brueggeney, M.; Greif, R.; Schoettker, P.; Savoldelli, G.L.; Nabecker, S.; Theiler, L.G. Evaluation of six videolaryngoscopes in 720 patients with a simulated difficult airway: A multicentre randomized controlled trial. Br. J. Anaesth. 2016, 116, 670–679. [Google Scholar] [CrossRef] [PubMed]
- Aziz, M.F.; Brambrink, A.M.; Healy, D.W.; Willett, A.W.; Shanks, A.; Tremper, T.; Jameson, L.; Ragheb, J.; Biggs, D.A.; Paganelli, W.C.; et al. Success of intubation rescue techniques after failed direct laryngoscopy in adults. A retrospective comparative analysis from the multicenter perioperative outcomes group. Anesthesiology 2016, 125, 656–666. [Google Scholar] [CrossRef] [PubMed]
- Aziz, M.F.; Abrons, R.O.; Cattano, D.; Bayman, E.O.; Swanson, D.E.; Hagberg, C.A.; Todd, M.M.; Brambrink, A.M. First-attempt intubation success of video laryngoscopy in patients with anticipated difficult direct laryngoscopy: A multicenter randomized controlled trial comparing the C-MAC D-Blade versus the Glide Scope in a mixed provider and diverse patient population. Anesth. Analg. 2016, 120, 740–750. [Google Scholar]


| Variable | Glidescope Titanium Group | King Vision Group |
|---|---|---|
| (n = 55) | (n = 55) | |
| Sex (males/females) | 32/23 (58%/42%) | 29/26 (53%/47%) |
| Age (years) | 56 [50.5–62] (29–87) | 56 [51–61.2] (28–75) |
| Height (cm) | 175 [172–178] (152–200) | 172 [170–176] (153–195) |
| Weight (kg) | 120 [119–132] (90–205) | 122 [118–130] (89–190) |
| Body mass index (kg∙m−2) | 39.5 [37.9–41.1](35.1–63.2) | 39.2 [37.6–41.7](35.2–57.1) |
| American Society of Anesthesiologists | 1/34/20/0 | 0/45/9/1 |
| Status (1/2/3/4) | (2%/52%/36%/0%) | (0%/82%/16%/2%) |
| Duration of procedure (min) | 116 [98–132] (30–300) | 90 [89–109] (45–220) |
| Mallampati score (1/2/3/4) | 12/24/16/3 | 8/28/17/2 |
| (22%/44%/29%/5%) | (14%/51%/31%/4%) | |
| Mouth opening (cm) | 4.5 [4,5] (2–8) | 4 [4–4.5] (2–7) |
| Thyromental distance (cm) | 7 [6,7] (3–12) | 7 [6.5–7] (4.5–12) |
| Neck circumference (cm) | 49 [47–50] (35–73) | 52 [50–55] (36–66) |
| Limited neck extension (<35°) | 19 (35%) | 8 (15%) |
| Sleep apnea syndrome | 23 (42%) | 21 (38%) |
| Outcome | Glidescope Titanium | King Vision | p |
|---|---|---|---|
| (n = 55) | (n = 55) | ||
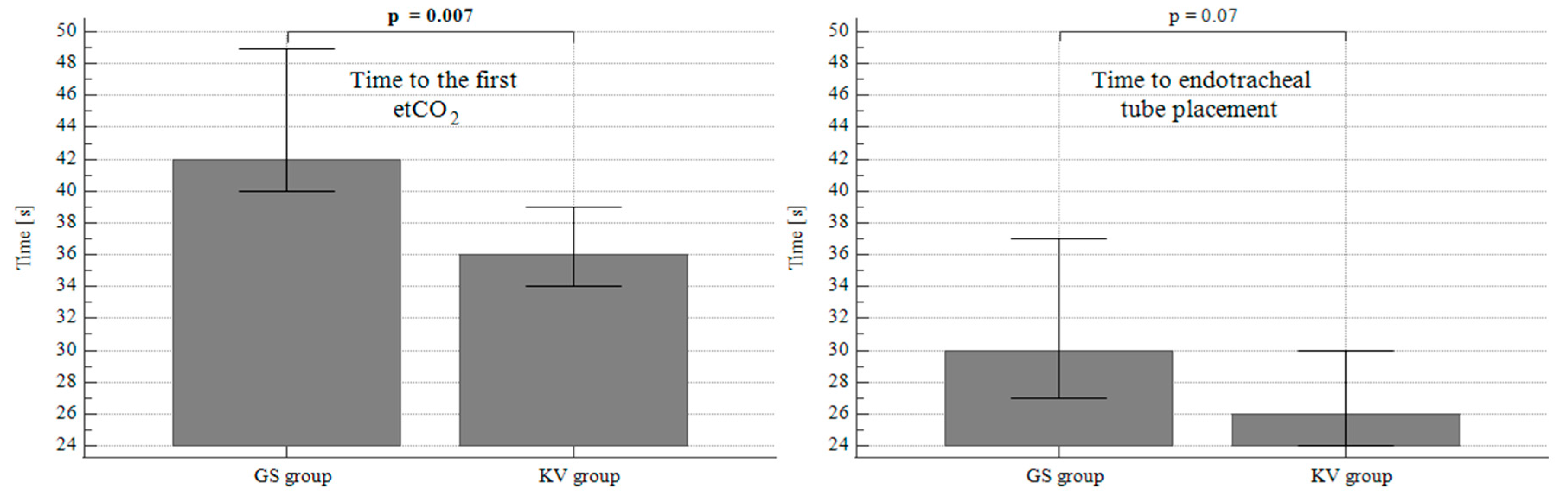
| Duration of intubation (sec) | 42 [40–48.9] (20–147) | 36.0 [34–39] (15–98) | 0.007 * |
| Tracheal tube placement (sec) | 30.0 [27–37] (12–132) | 26.0 [24–30] (10–83) | 0.07 |
| Total success rate (n, %) | 55 (100%) | 49 (89.1%) | 0.03 * |
| First attempt success (n, %) | 49 (89.1%) | 40 (72.7%) | 0.05 |
| Number of attempts 1/2/3 (n) | 49/6/0 | 40/12/3 | 0.05 |
| Cormack–Lehane grade 1/2/3/4 (n) | 39/12/4/0 | 35/16/3/1 | 0.57 |
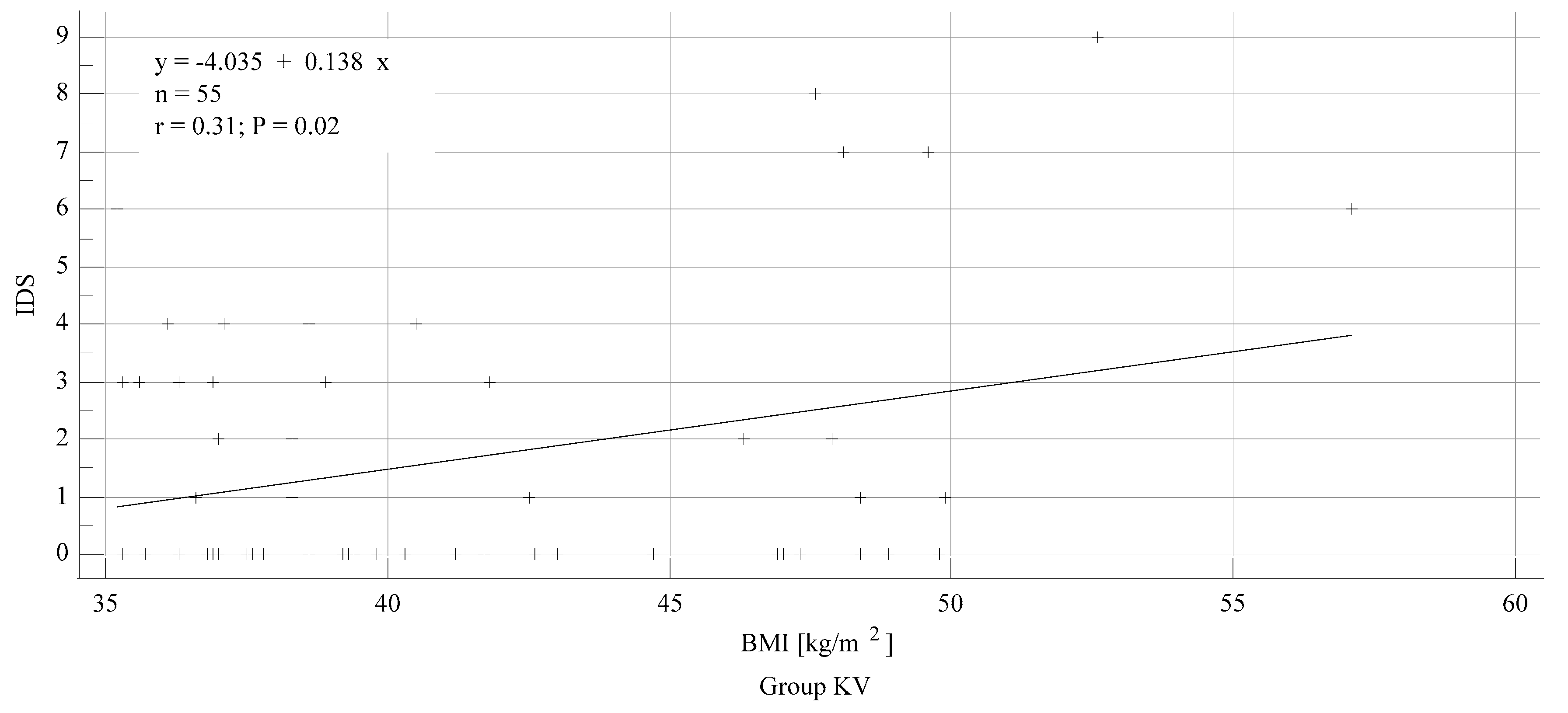
| Intubation Difficulty Scale | 35/16/3/1 | 0 [0–1.2] (0–9) | 0.27 |
| Additional maneuvers (n, %) | 12 (21.8%) | 20 (36.4%) | 0.17 |
| Trauma during intubation (n, %) | 1 (1.8%) | 7 (12.7%) | 0.06 |
| Lowest SpO2 during attempts (%) | 97 [93.4–97] (55–100) | 96 [93.5–96.3] (71–100) | 0.18 |
| Outcome | Glidescope Titanium | King Vision | p |
|---|---|---|---|
| (n = 55) | (n = 55) | ||
| Sore throat (n); none/mild/moderate/severe | 21/31/2/1 | 16/32/6/1 | 0.54 |
| Hoarseness (n); none/mild/moderate/severe | 44/7/4/0 | 41/11/3/0 | 0.29 |
| Pain on swallowing (n); none/mild/moderate/severe | 25/27/3/0 | 29/23/2/1 | 0.75 |
| Cough (n, %) | 5 (9.1%) | 6 (10.9%) | 0.75 |
| Other complaints (n, %) | 1 (1.8%) | 5 (9.1%) | 0.09 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brozek, T.; Bruthans, J.; Porizka, M.; Blaha, J.; Ulrichova, J.; Michalek, P. A Randomized Comparison of Non-Channeled GlidescopeTM Titanium Versus Channeled KingVisionTM Videolaryngoscope for Orotracheal Intubation in Obese Patients with BMI > 35 kg·m−2. Diagnostics 2020, 10, 1024. https://doi.org/10.3390/diagnostics10121024
Brozek T, Bruthans J, Porizka M, Blaha J, Ulrichova J, Michalek P. A Randomized Comparison of Non-Channeled GlidescopeTM Titanium Versus Channeled KingVisionTM Videolaryngoscope for Orotracheal Intubation in Obese Patients with BMI > 35 kg·m−2. Diagnostics. 2020; 10(12):1024. https://doi.org/10.3390/diagnostics10121024
Chicago/Turabian StyleBrozek, Tomas, Jan Bruthans, Michal Porizka, Jan Blaha, Jitka Ulrichova, and Pavel Michalek. 2020. "A Randomized Comparison of Non-Channeled GlidescopeTM Titanium Versus Channeled KingVisionTM Videolaryngoscope for Orotracheal Intubation in Obese Patients with BMI > 35 kg·m−2" Diagnostics 10, no. 12: 1024. https://doi.org/10.3390/diagnostics10121024
APA StyleBrozek, T., Bruthans, J., Porizka, M., Blaha, J., Ulrichova, J., & Michalek, P. (2020). A Randomized Comparison of Non-Channeled GlidescopeTM Titanium Versus Channeled KingVisionTM Videolaryngoscope for Orotracheal Intubation in Obese Patients with BMI > 35 kg·m−2. Diagnostics, 10(12), 1024. https://doi.org/10.3390/diagnostics10121024







