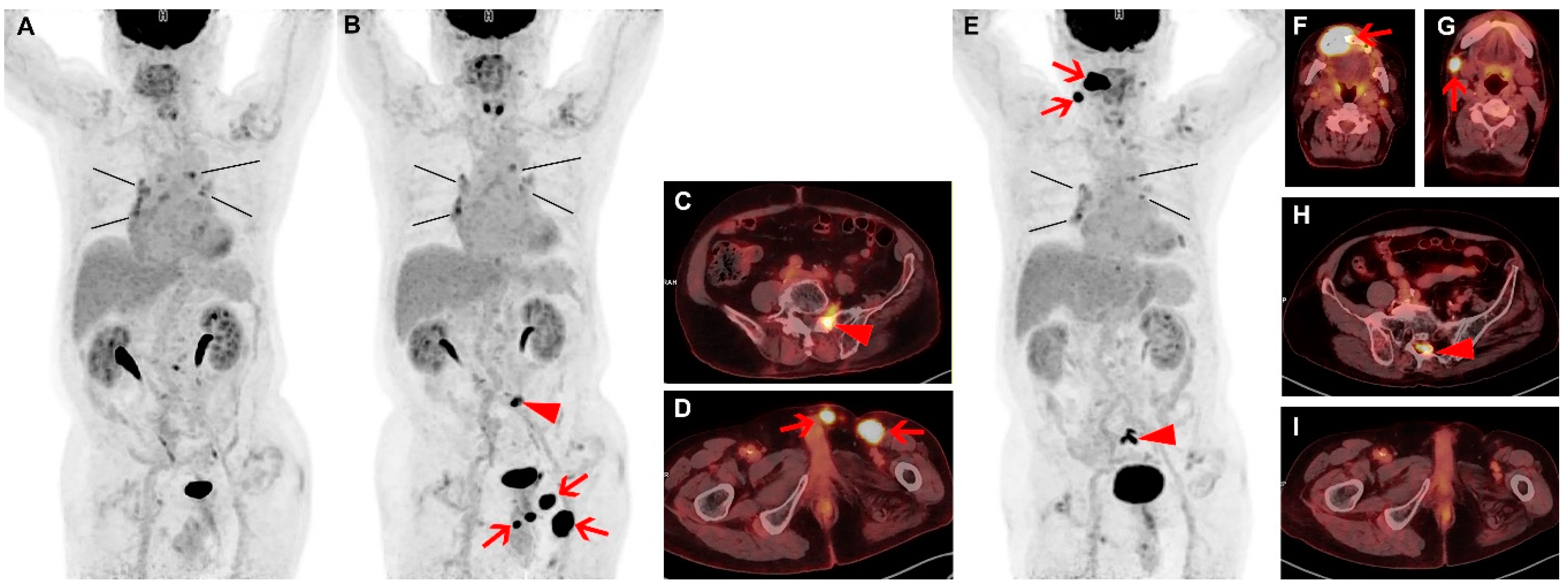
Spontaneous Remission and Concomitant Progression in a Patient with DLBCL
Abstract
:Author Contributions
Funding
Acknowledgements
Conflicts of Interest
References
- Li, S.; Young, K.H.; Medeiros, L.J. Diffuse large B-cell lymphoma. Pathology 2018, 50, 74–87. [Google Scholar] [CrossRef] [PubMed]
- Iacoboni, G.; Zucca, E.; Ghielmini, M.; Stathis, A. Methodology of clinical trials evaluating the incorporation of new drugs in the first-line treatment of patients with diffuse large B-cell lymphoma (DLBCL): A critical review. Ann. Oncol. 2018, 29, 1120–1129. [Google Scholar] [CrossRef] [PubMed]
- Crump, M.; Neelapu, S.S.; Farooq, U.; Van Den Neste, E.; Kuruvilla, J.; Westin, J.; Link, B.K.; Hay, A.; Cerhan, J.R.; Zhu, L.; et al. Outcomes in refractory diffuse large B-cell lymphoma: results from the international SCHOLAR-1 study. Blood 2017, 130, 1800–1808. [Google Scholar] [CrossRef] [PubMed]
- Gattiker, H.H.; Wiltshaw, E.; Galton, D.A. Spontaneous regression in non-Hodgkin’s lymphoma. Cancer 1980, 45, 2627–2632. [Google Scholar] [CrossRef]
- Kumar, R.; Bhargava, P.; Zhuang, H.; Yu, J.Q.; Schuster, S.J.; Alavi, A. Spontaneous regression of follicular, mantle cell, and diffuse large B-cell non-Hodgkin’s lymphomas detected by FDG-PET imaging. Clin. Nucl. Med. 2004, 29, 685–688. [Google Scholar] [CrossRef] [PubMed]
- Kumamoto, M.; Nakamine, H.; Hara, T.; Yokoya, Y.; Kawai, J.; Ito, H.; Nishioka, S.; Takenaka, T.; Wickert, R.S.; Mitchell, D.W. Spontaneous complete regression of high grade non-Hodgkin’s lymphoma. Morphologic, immunohistochemical, and gene amplification analyses. Cancer 1994, 74, 3023–3028. [Google Scholar] [CrossRef]
- Pasvolsky, O.; Berger, T.; Bernstine, H.; Hayman, L.; Raanani, P.; Vidal, L. Spontaneous Regression of Hodgkin Lymphoma: Case Report and Review of the Literature. Acta Haematol. 2019, 141, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Snijder, J.; Mihyawi, N.; Frolov, A.; Ewton, A.; Rivero, G. Spontaneous remission in diffuse large cell lymphoma: a case report. J. Med. Case Rep. 2019, 13, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sasaki, J.; Kurihara, H.; Nakano, Y.; Kotani, K.; Tame, E.; Sasaki, A. Apparent spontaneous regression of malignant neoplasms after radiography: Report of four cases. Int. J. Surg. Case Rep. 2016, 25, 40–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramos, R.; Fernandes, J.S.; Almeida, M.; Almeida, R. A Rare Case of Spontaneous Remission and Relapse of a Primary Central Nervous System Lymphoma. Acta Med. Port. 2018, 31, 777–783. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, E.J.; Kim, J.; Park, S.Y.; O, J.H. Spontaneous Remission and Concomitant Progression in a Patient with DLBCL. Diagnostics 2020, 10, 950. https://doi.org/10.3390/diagnostics10110950
Han EJ, Kim J, Park SY, O JH. Spontaneous Remission and Concomitant Progression in a Patient with DLBCL. Diagnostics. 2020; 10(11):950. https://doi.org/10.3390/diagnostics10110950
Chicago/Turabian StyleHan, Eun Ji, Jihyun Kim, Suk Young Park, and Joo Hyun O. 2020. "Spontaneous Remission and Concomitant Progression in a Patient with DLBCL" Diagnostics 10, no. 11: 950. https://doi.org/10.3390/diagnostics10110950
APA StyleHan, E. J., Kim, J., Park, S. Y., & O, J. H. (2020). Spontaneous Remission and Concomitant Progression in a Patient with DLBCL. Diagnostics, 10(11), 950. https://doi.org/10.3390/diagnostics10110950




