Abstract
Background: Falls are a leading cause of injury, disability, and loss of independence among community-dwelling older adults. Although exercise-based interventions are widely recommended for fall prevention, the comparative effectiveness of different exercise modalities remains insufficiently synthesized. Methods: This systematic review was conducted in accordance with PRISMA 2020 guidelines. Randomized and controlled trials were identified through searches of PubMed, Scopus, Web of Science, and CINAHL, including studies involving adults aged ≥60 years who participated in balance-based, strength-based, multimodal, Tai Ji Quan, Otago Exercise Program, or perturbation-based reactive balance training interventions. Methodological quality was assessed using the Cochrane Risk of Bias 2 (ROB-2) tool. Due to substantial clinical and methodological heterogeneity across interventions and outcome measures, a narrative synthesis was undertaken. Results: Twenty-seven trials met the inclusion criteria. Exercise interventions consistently reduced fall incidence across studies. Tai Ji Quan interventions were associated with approximately 31–58% reductions in falls, the Otago Exercise Program with 23–40% reductions, and multimodal strength–balance training with 20–45% reductions. Perturbation-based reactive balance training demonstrated particularly strong effects on laboratory-induced falls, with reductions ranging from 50–75%. Functional outcomes also improved across intervention types, including faster Timed Up and Go performance, increased gait speed, improvements of approximately 1.2–2.5 points in Short Physical Performance Battery scores, 15–35% gains in lower-limb strength, and enhanced reactive balance responses. Longer-duration interventions (12–24 months) generally demonstrated sustained reductions in fall risk. Conclusions: Evidence from randomized and controlled trials indicates that structured exercise interventions, particularly Tai Ji Quan, the Otago Exercise Program, multimodal strength–balance training, and perturbation-based reactive balance training, are effective in reducing falls and improving balance, mobility, and strength in community-dwelling older adults. These findings support the use of targeted, evidence-based exercise programs as central components of fall-prevention strategies in older populations.
1. Introduction
Falls remain a major threat to the health and independence of older adults, with nearly one in three individuals aged ≥65 years experiencing at least one fall annually. Beyond physical injury, fear of falling is a clinically relevant factor strongly associated with balance impairment, activity restriction, and functional decline. Recent evidence demonstrates significant correlations between fear of falling scores and objective measures of functional balance in community-dwelling older adults, supporting its role as a valid indicator of fall risk [1]. Recent global estimates indicate that falls account for over 684,000 deaths annually worldwide, with adults aged 60 years and older disproportionately affected. The World Health Organization reports that fall constitute the second most common cause of death due to unintentional injuries across the globe, highlighting their significant global impact [2]. Additional epidemiological data suggest that around 40% of community-dwelling adults over 65 years encounter at least one fall each year, often resulting in injury, functional deterioration, and diminished overall well-being [3]. In the European context, fall-related fatalities among older adults are notably high, with approximately 36,000 deaths recorded annually; notably, individuals aged 75 years and older account for the majority of these cases (88%), and women represent a disproportionately affected group (59%) [4]. Collectively, these findings underscore the critical importance of developing and implementing effective fall-prevention strategies for aging populations.
Physical inactivity and reductions in functional capacity, such as weakened lower-limb muscles and compromised balance, are well-established risk factors contributing to falls and fall-related injuries, including head trauma and hip fractures, among older adults [5,6,7,8]. Participating in sports and physical activity not only shapes the human body but also offers a transformative experience that enhances both physical and mental well-being, further reinforcing its value as a preventive health strategy [9,10]. Although these physiological deficits significantly elevate fall vulnerability, they remain highly modifiable through targeted exercise interventions [6,11,12]. Beyond their physical consequences, falls create substantial financial strain due to increased medication use, hospital admissions, and extended rehabilitation services [2,13]. A robust body of evidence supports exercise training as one of the most effective approaches for enhancing functional performance, improving mobility and balance, and ultimately reducing fall risk in older adults [14,15,16]. Additionally, promoting regular physical activity yields considerable economic and public health benefits, contributing positively to national healthcare systems and improving quality of life at both community and individual levels [17].
Given the substantial individual, societal, and economic burden associated with falls, researchers and clinicians have increasingly emphasized the importance of identifying modifiable factors that can effectively mitigate fall risk among older adults [18,19]. A considerable body of scientific literature has demonstrated that deficits in physical fitness, including decreased muscle strength, slower gait speed, impaired balance, and poor postural control, directly contribute to fall likelihood and fall-related injuries [5,6,8]. These impairments tend to worsen progressively with age, particularly in adults over 70 years, as natural age-related declines in neuromuscular function accelerate deterioration in reaction time, proprioception, and coordination. Importantly, these deteriorations are not merely a consequence of aging, but are significantly exacerbated by Sedentary lifestyles and insufficient participation in structured physical activity [7]. Therefore, maintaining adequate levels of physical activity becomes a central component in preventing early functional decline in older populations.
The evidence linking functional decline with fall risk is further reinforced by longitudinal studies indicating that lower-limb strength is one of the strongest predictors of fall likelihood, particularly in tasks requiring rapid balance recovery or directional changes [11]. Weakness in key muscle groups such as the quadriceps, gluteals, and ankle stabilizers reduces the capacity to execute compensatory steps or prevent center-of-mass displacement during unexpected perturbations [20,21]. Similarly, impaired balance abilities, often measured through standardized assessments such as the Timed Up and Go (TUG) or Berg Balance Scale (BBS), are strongly associated with increased fall incidence, highlighting the role of neuromuscular control in stabilizing the body during dynamic tasks [12,16]. Combining these findings, the literature consistently underscores that physical inactivity sets off a cascade of functional deterioration, which in turn contributes to a heightened risk of falls and fall-induced injuries.
In addition to physiological risk factors, several behavioral and environmental contributors have been identified. Poor health behaviors, lack of engagement in wellness-promoting activities, and low adherence to exercise routines all independently elevate fall risk [7]. Environmental hazards such as poor lighting, uneven flooring, and cluttered home environments also contribute, especially among older adults with limited mobility and slower reflexes. Nevertheless, while environmental and behavioral factors play important roles, interventions targeting physical function, particularly those involving structured exercise, remain among the most effective and sustainable strategies for preventing falls. This is supported by systematic reviews showing that exercise-based interventions lead to consistent improvements in muscle strength, functional mobility, balance control, and gait stability, which collectively translate into measurable reductions in fall incidence [14].
From a biomechanical perspective, fall risk in older adults reflects the interaction between lower-limb muscle strength, postural control, and reactive balance capacity. Age-related weakness in key muscle groups and impaired anticipatory control reduce the ability to regulate the center of mass and execute effective balance-recovery responses during daily activities. When unexpected perturbations such as slips or trips occur, insufficient reactive balance further limits compensatory stepping, increasing the likelihood of falls.
The growing emphasis on exercise interventions is further justified by robust economic evidence. Falls are associated with high medical expenditures, including emergency care, orthopedic surgeries, extended hospital stays, and long-term rehabilitation services [13]. At the societal level, these costs place significant pressure on national healthcare systems, particularly in countries with rapidly aging populations. Studies highlight that investments in preventive exercise programs can substantially reduce fall-related healthcare expenses and improve cost-efficiency in the management of older adult health [17]. Moreover, community-level exercise programs support social participation, psychological well-being, and improved quality of life, extending their benefits beyond physical health alone [22,23].
A wide range of exercise modalities has been studied for their potential to reduce fall risk, each focusing on different physiological mechanisms [24]. Strength training programs aim to counteract age-related muscle loss and improve the ability to generate force during daily activities [25]. Balance training interventions target sensory integration, postural alignment, and anticipatory movement adjustments [26]. Multimodal exercise programs incorporate elements of both strength and balance, alongside flexibility, gait training, and functional mobility exercises, thereby addressing multiple determinants of fall risk simultaneously [6,15]. Additionally, Tai Ji Quan has been extensively examined and shown to enhance proprioception, controlled breathing, dynamic balance, and lower-limb coordination, making it particularly effective for older adults with balance limitations [14].
Although this approach is not included as a core reference in your introduction sources, its conceptual relevance is grounded in decades of evidence demonstrating that improved reactive stepping is a critical component of fall prevention [11]. Reactive balance capability represents one of the strongest predictors of fall risk because most real-world falls occur during unexpected perturbations, such as uneven surfaces, sudden turns, or slips during locomotion [27]. Strengthening the neuromuscular responses required to counteract these perturbations aligns with evidence showing that functional and neuromuscular training significantly enhances fall resilience [28].
Despite well-established evidence supporting exercise programs, older adults often face barriers that impede their participation. These include fear of injury, low motivation, limited access to exercise facilities, and the misconception that age restricts the capacity to benefit from physical training [7]. However, research consistently shows that even low- to moderate-intensity exercise can lead to meaningful improvements in physical performance among older adults. Furthermore, community-delivered programs such as Tai Ji Quan classes, supervised balance groups, and home-based strength programs offer scalable, affordable, and culturally adaptable approaches to promoting active aging. These programs provide a structured environment for older adults to engage in safe and effective exercise, with several studies emphasizing their high adherence rates and positive psychological effects [10,14].
Alongside physical benefits, exercise participation contributes to enhanced cognitive and psychological well-being in older adults, supporting a more holistic model of fall prevention. This aligns with contemporary perspectives in physical education and sports science, which view movement not only as a means to enhance physical capacity but also as a transformative experience that shapes mental resilience and promotes emotional stability [10]. Integrating mental and physical benefits of exercise strengthens the rationale for adopting exercise-based approaches as comprehensive fall-prevention strategies.
The compelling evidence supporting exercise interventions has shaped global public health recommendations. Leading organizations, including the World Health Organization, advocate for structured exercise programs emphasizing balance, strength, and mobility training as core components of fall-prevention strategies for community-dwelling older adults [2]. These guidelines stress that such programs should be accessible, evidence-based, and delivered in a manner that considers individual health status, cultural context, and personal preferences. By adopting these recommendations, healthcare systems can proactively address fall risk, reduce long-term healthcare expenditures, and enhance functional independence among older adults.
Despite the growing body of literature supporting exercise-based fall prevention, the current evidence base remains fragmented. Most previous systematic reviews have examined single exercise modalities in isolation, such as strength training, balance training, Tai Ji Quan, or perturbation-based approaches, without providing a unified comparison across these distinct intervention types. As a result, clinicians and policymakers lack an integrated synthesis that contrasts traditional balance- and strength-based programs with emerging reactive balance and perturbation-based training within a single evidence framework. Moreover, the mechanisms through which different exercise modalities reduce fall risk, such as improvements in anticipatory balance, reactive stepping, neuromuscular strength, and long-term adherence, have rarely been examined together. Therefore, this systematic review uniquely addresses this gap by comparatively synthesizing randomized controlled trials investigating Tai Ji Quan, the Otago Exercise Program, multimodal strength–balance training, and perturbation-based reactive balance interventions in community-dwelling older adults, to clarify their relative effectiveness, mechanisms of action, and practical implications for fall prevention. The review was structured according to a PICO framework, comparing different exercise modalities (I) against usual care or alternative exercise (C) in community-dwelling older adults (P), with fall incidence, balance, mobility, and strength as primary outcomes (O).
2. Materials and Methods
2.1. Study Selection Procedures
The review protocol was not preregistered due to the exploratory and integrative nature of the review, which aimed to synthesize diverse and emerging exercise modalities rather than evaluate a narrowly defined intervention. The study selection process followed the PRISMA 2020 Figure 1 (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and PROSPERO guidelines [29] and involved multiple stages to ensure systematic identification and inclusion of relevant studies. The review protocol was not preregistered before conducting the study. The research included studies conducted from 2010 to 2025, covering the last 15 years and ensuring up-to-date findings that reflect current trends in the field. The search was conducted until 15 August 2025, with a final update in September 2025. Across the 2010–2025 period, more than half of the included studies (≈52%) were published between 2015 and 2019, reflecting a surge of high-quality research during this phase. In contrast, early publications from 2010–2014 accounted for only about 7% of the studies, while the remaining 41% were produced between 2020 and 2025, highlighting continued contemporary contributions. The studies were searched through the following electronic databases: PubMed, Scopus, Web of Science, and CINAHL. After completing the initial database search, all retrieved records were imported into reference management software, and duplicate entries were removed. Two independent reviewers (SC and PKC) screened titles and abstracts using predefined eligibility criteria, focusing on exercise-based balance, strength, mobility, and reactive-balance interventions for community-dwelling older adults aged 60 years and above. Studies meeting preliminary criteria underwent full-text screening, where the same reviewers independently assessed methodological relevance, intervention focus, and outcome reporting. Conflicts at any stage were resolved through discussion or consultation with a third reviewer (BK). Only studies that fulfilled all inclusion criteria Table 1 and adhered to intervention relevance for fall prevention were included in the final synthesis.
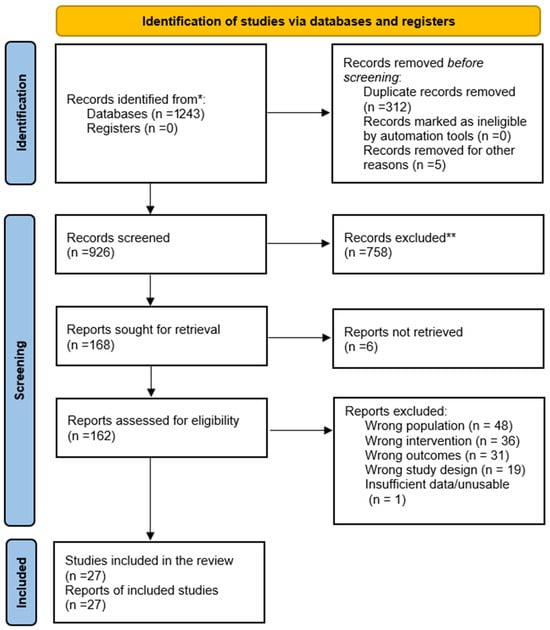
Figure 1.
PRISMA 2020 flow diagram showing the study selection process for the systematic review. * the number of records identified from each database or register, ** indicate how many records were excluded.

Table 1.
Inclusion and Exclusion Criteria.
2.2. Literature Search: Administration and Update
The literature search was conducted systematically across major scholarly databases including PubMed, Scopus, Web of Science, and CINAHL, using a combination of controlled vocabulary and text-based keywords such as “older adults,” “falls,” “balance training,” “strength training,” “Tai Ji Quan,” “Otago Exercise Program,” “perturbation-based balance training,” and “fall prevention exercises.” Boolean operators were applied to refine retrieval, and filters were limited to English-language, peer-reviewed, full-text publications. The search strategy was designed iteratively, and database-specific adjustments were made to maximize sensitivity. To maintain currency, the search was updated before final analysis to capture newly published randomized or controlled trials meeting eligibility criteria, ensuring the dataset reflected the most recent evidence in fall-prevention exercise interventions.
2.3. Data Extraction
Data extraction was performed using a predesigned standardized data extraction protocol [30] to maintain methodological consistency. Extracted information included study identifiers (author, year, country), participant characteristics (sample size, age, eligibility), intervention details (type, frequency, intensity, duration, supervision), comparator groups, outcome variables, measurement instruments, and key findings related to fall incidence, balance performance, mobility, strength, and secondary outcomes. Two independent reviewers conducted the extraction process and cross-checked all entries. Discrepancies were addressed through discussion, and final data were validated before synthesis. When necessary, authors of included trials were contacted for missing or unclear information. When outcome data were missing or unclear, corresponding authors were contacted via email; responses were obtained for a subset of studies, while non-responses were documented and managed conservatively in the synthesis.
2.4. Methodological Quality of the Included Studies
The methodological quality of all included randomized and controlled trials was assessed using the Cochrane Risk of Bias 2 (ROB-2) tool. This assessment evaluated potential sources of bias across five domains: (1) the randomization process, (2) deviations from intended interventions, (3) missing outcome data, (4) measurement of outcomes, and (5) selection of reported results, in accordance with the guidance provided in the Cochrane Handbook for Systematic Reviews of Interventions [31]. Each domain was judged as having “low risk,” “some concerns,” or “high risk” of bias, leading to an overall risk-of-bias judgment for each study based on established criteria [32]. Assessments were conducted independently by two reviewers, with disagreements resolved through discussion and consensus, consistent with recommended best practices for minimizing assessor subjectivity [33]. The ROB-2 evaluations were used to inform confidence in the interpretation of outcomes and to guide the narrative weighting of evidence within the synthesis.
2.5. Summary Measures
Primary summary measures included fall incidence and injurious falls reported as count data, rate ratios, or risk ratios. Continuous outcomes, such as balance scores (BBS, SPPB), mobility performance (TUG, gait speed), and strength measures (Chair Stand Test, dynamometry), were summarized through means, standard deviations, and mean differences where available. Reactive-balance outcomes were extracted as step-recovery responses or lab-induced fall rates. When multiple measures were reported for the same domain, those most widely validated and consistently applied across trials were prioritized to enhance comparability across studies.
2.6. Synthesis of Results
Due to heterogeneity in intervention type, duration, participant characteristics, and outcome assessment methods, a narrative synthesis approach was adopted. Studies were grouped based on intervention modality (e.g., Tai Ji Quan, Otago, multimodal strength-balance training, perturbation-based training), and findings were compared qualitatively across domains of falls, balance, mobility, and strength. Effect direction and consistency were emphasized, and detailed tables were developed to summarize intervention characteristics and outcome results. Where multiple studies reported similar outcomes using comparable tools, patterns of improvement or neutrality were identified to derive cross-study interpretive trends relevant to fall prevention in older adults. Studies reporting laboratory-based biomechanical outcomes, such as slip- or trip-induced balance perturbations and reactive stepping responses, were included alongside community-based fall studies because reactive balance capacity represents a critical mechanistic determinant of fall prevention. Laboratory-based outcomes were analyzed and interpreted separately from community fall incidence, with a clear distinction maintained between mechanistic adaptations (reactive balance and compensatory stepping) and clinical endpoints (actual fall occurrence). This approach allowed biomechanical insights derived from controlled laboratory settings to be contextualized without overextending causal inference to real-world fall reduction.
2.7. Data Synthesis
A quantitative meta-analysis was not conducted due to substantial clinical and methodological heterogeneity across included trials, including differences in intervention modalities, outcome definitions, follow-up durations, and participant risk profiles. Formal statistical heterogeneity indices (e.g., I2 or τ2) were therefore not calculated, as pooling effect estimates under these conditions would risk producing misleading summary effects. Instead, a structured narrative synthesis was undertaken, emphasizing consistency in the direction of effects across studies rather than pooled magnitude estimates. Consistent with PRISMA 2020 guidance, the certainty of evidence was interpreted qualitatively, and a formal GRADE assessment was not applied because no quantitative synthesis was performed.
2.8. Publication Bias
Publication bias was considered by examining the completeness of available data, selective reporting tendencies identified during the risk-of-bias assessment, and the distribution of study outcomes across different intervention modalities. Although formal statistical tests for publication bias (e.g., funnel plots or Egger’s regression) were not feasible due to substantial heterogeneity in measurement scales, intervention types, and study designs, this approach is consistent with PRISMA recommendations for narrative syntheses when meta-analytic pooling is inappropriate [29]. Qualitative assessment methods, supported by guidance from the Cochrane Handbook, allowed for the evaluation of selective reporting patterns and missing data across included trials [31]. Overall, most included studies were published in peer-reviewed journals with transparent reporting practices, reducing but not eliminating the potential for selective publication favoring statistically significant or positive findings, as noted by [32].
2.9. Additional Analyses
Additional analyses included subgroup comparisons based on intervention type (balance-focused, strength-focused, multimodal, perturbation-based), duration (short-term ≤ 12 weeks vs. long-term ≥ 6 months), and delivery mode (home-based vs. supervised group programs). Trends were also evaluated by age range and fall-risk profile to determine differential responsiveness to specific intervention strategies. Sensitivity considerations were applied by giving greater interpretive weight to low-risk-of-bias RCTs while acknowledging outcomes from smaller pilot trials and studies with methodological limitations. These additional analyses supported a more nuanced understanding of which exercise interventions were most effective for reducing falls and improving physical functioning in older adults.
3. Results
A total of 27 studies Table 2 met the eligibility criteria and were included in the final synthesis. These studies varied in intervention type, duration, sample size, and outcome measures, providing a diverse representation of exercise-based strategies for fall prevention among community-dwelling older adults. The selection process is summarized in the PRISMA flow diagram and reflects rigorous screening across multiple databases, removal of duplicates, and detailed full-text evaluation. The included studies comprised randomized controlled trials, cluster RCTs, controlled clinical trials, and pilot interventions, with sample sizes ranging from small feasibility trials to large multi-center investigations. The following subsections present the synthesized results organized by primary and secondary outcome domains, highlighting patterns of effectiveness and variability across intervention types.

Table 2.
Study Characteristics.
Table 3 summarizes the methodological quality of all included trials using the Cochrane ROB-2 tool, illustrating variations in risk of bias across the five assessment domains. Most studies demonstrated low risk in randomization, adherence to interventions, and outcome measurement, although several exhibited “some concerns” due to incomplete follow-up or selective reporting.

Table 3.
Risk of Bias (ROB-2) for Included Studies.
Pilot studies and cluster designs showed slightly higher levels of uncertainty because of small samples, attrition, or limited allocation detail. This table provides a comprehensive evaluation of internal validity across trials and highlights the relative robustness of the evidence base.
Table 4 presents an overview of the intervention characteristics across all included studies, detailing exercise type, frequency, intensity, session duration, total program duration, and delivery format. The interventions varied considerably, ranging from long-term community-based strength-balance programs to short-term perturbation-based reactive balance training.

Table 4.
Summary of Intervention Characteristics Across Included Studies.
3.1. Long-Term Adherence and Sustainability
This variation reflects the diversity of fall-prevention strategies employed in older adult populations. The table provides a clear comparison of intervention structures, enabling an understanding of their scope, intensity, and practical applicability.
Table 5 summarizes the effects of the included interventions on fall incidence and injurious falls, demonstrating that most exercise programs resulted in meaningful reductions in fall frequency compared with control or usual-care groups. The strongest effects were observed in Tai Ji Quan, Otago, multimodal strength-balance programs, and perturbation-based training.

Table 5.
Outcome Summary for Fall Incidence.
3.2. Reactive Balance Improvement
These findings highlight the consistent protective impact of exercise-based interventions on fall risk. The table provides a concise comparison of outcome direction and study-specific observations.
Table 6 outlines the improvements in balance performance across interventions using validated instruments such as the Berg Balance Scale, Timed Up and Go, and post-urography. Most studies reported positive effects, with notable improvements following Tai Ji Quan, Otago, multimodal training, and perturbation-based programs. These findings underscore the importance of targeted balance exercises in enhancing postural control and reactive balance in older adults. The table helps visualize the consistency of balance-related benefits across diverse exercise modalities.

Table 6.
Outcome Summary for Balance Performance.
Table 7 provides a summary of mobility and functional performance outcomes, demonstrating that exercise interventions frequently improved gait speed, TUG performance, and SPPB scores. Programs involving strength-balance combinations, balance circuits, and perturbation training showed particularly strong impacts on functional mobility.

Table 7.
Outcome Summary for Mobility/Functional Performance.
3.3. Strength and Mobility Adaptations
These improvements reflect enhanced physical functioning and reduced fall risk among participants. The table highlights consistent positive effects across a wide range of functional mobility assessments.
Table 8 details the effects of various interventions on lower-limb strength, showing consistent improvements across group exercise programs, balance circuits, multimodal training, and strength-balance combinations. Strength gains were commonly measured using chair stand tests, dynamometry, and force platforms, demonstrating enhanced muscular performance and power.

Table 8.
Outcome Summary for Strength (Lower-Limb Strength).
These findings emphasize the important contribution of strength development to overall fall-prevention effectiveness. The table provides clear evidence of the widespread benefits of strength-oriented interventions.
4. Discussion
The present systematic review synthesized evidence from 27 clinical trials investigating the effects of balance-, strength-, mobility-, and perturbation-based exercise interventions on fall incidence, balance performance, mobility, and lower-limb strength in community-dwelling older adults. Across studies, a consistent pattern emerged demonstrating that structured exercise programs, particularly those emphasizing balance control, reactive stability, and lower-limb strength, produce meaningful improvements in physical function and reduce the risk of falls among older populations. The convergence of evidence from diverse methodologies, ranging from long-term community trials to short-term laboratory-based perturbation training, provides a robust foundation for understanding the multifaceted role of exercise in fall prevention.
The included studies demonstrated substantial clinical and methodological heterogeneity with respect to intervention duration, training intensity, delivery mode, outcome measures, and participant risk profiles. While this variability precluded quantitative meta-analysis, it reflects real-world diversity in fall-prevention practice. Consequently, conclusions should be interpreted as indicative of consistent directional benefits rather than precise effect magnitudes. Importantly, the convergence of positive outcomes across heterogeneous designs strengthens the external validity of exercise-based fall-prevention strategies, although generalizability to very frail or institutionalized populations remains limited.
Our findings demonstrate a consistent improvement in balance performance across multiple interventions included in this review, particularly in studies employing Tai Ji Quan, perturbation-based balance training, and multimodal strength-balance programs [34,38,42,44,46,55,56,57]. These improvements closely mirror the broader evidence base, where Tai Ji Quan has repeatedly been shown to enhance functional balance, postural stability, and reactive control in older adults. In the present review, Tai Ji Quan interventions not only reduced fall incidence but also produced measurable gains in balance function, consistent with the large clinical trials conducted by [42,46]. Mechanistically, these effects may be attributed to Tai Ji Quan’s emphasis on slow, controlled weight shifting, proprioceptive refinement, and continuous center-of-mass regulation, which directly translate into safer movement strategies during daily activities. Similarly, the strong improvements observed in perturbation-based programs [34,44,47] align with previous research showing that repeated exposure to slips, trips, and destabilizing forces enhances reactive stepping, shortens response latency, and strengthens neuromuscular coordination under unexpected loss-of-balance conditions. Together, these patterns indicate that both anticipatory and reactive balance systems adapt robustly to targeted training, offering a strong mechanistic basis for the observed reductions in fall risk across interventions.
In our review, several studies demonstrated clear improvements in balance, mobility, and fall reduction through the Otago Exercise Program (OEP). Specifically, Arkkukangas et al. [49] reported meaningful gains in balance and adherence, Waters et al. [58] documented significant reductions in fall rates among Native American elders, and Cederbom & Arkkukangas [50] showed sustained functional benefits during long-term follow-up. Collectively, these findings highlight OEP’s consistent effectiveness across different populations and study durations.
These results align closely with previous evidence, which shows that structured exercise reduces falls by approximately 15% (rate ratio: 0.85) across large-scale trials [61,62]. Other research has similarly confirmed that balance-strength programs particularly Otago and Tai Ji Quan, enhance lower-limb strength, joint stability, and postural control [63,64].
When viewed together, both our included studies and existing literature suggest that longer, progressively loaded interventions (≥12 months) are associated with even greater reductions in fall risk, reinforcing the importance of sustained engagement for neuromuscular adaptation. Mechanistically, OEP’s effectiveness stems from its progressive lower-limb strengthening and dynamic balance training, which enhance proprioception and functional stability. These adaptations improve anticipatory postural adjustments and gait control, reducing vulnerability to balance disturbances. Such neuromuscular benefits are consistent with prior evidence showing that structured strength-balance programs enhance sensorimotor function and fall resilience in older adults [25,27]. Recent reviews further confirm that home-based, task-specific balance training improves confidence and reduces fear of falling, contributing to lower fall incidence [23,24].
In this systematic review, several included trials demonstrated consistent and meaningful improvements in reactive balance and fall-recovery ability following perturbation-based balance training. Studies such as Mansfield et al. [34], Okubo et al. [47], Allin et al. [51], Aviles et al. [44], and Nørgaard et al. [59] showed that repeated exposure to slips, trips, or rapid postural challenges produced substantial gains in compensatory stepping, reactive stability, and reductions in laboratory-induced falls. Importantly, these benefits emerged even during relatively short intervention periods (4–8 weeks), highlighting the efficiency of perturbation training in eliciting rapid neuromuscular adaptation in older adults. These findings align strongly with previous research demonstrating that high-task-specific perturbation exposure can recalibrate automatic postural responses, accelerate neuromuscular activation, and enhance trunk control during unexpected disturbances. For example, Allin et al. [51] reported significant reductions in both slip- and trip-related falls following treadmill-based perturbations, while Aviles et al. [44] observed superior improvements in reactive balance compared to traditional Tai Ji Quan training. Similarly, the more recent RCT by Nørgaard et al. [59] confirmed that structured perturbation protocols translate into measurable reductions in real-world fall rates, reinforcing the clinical applicability of this approach. Even smaller pilot investigations, such as Okubo et al.’s [48] unpredictability training study, demonstrated that brief exposures can induce meaningful motor learning across both younger and older adults. Taken together, our results support the growing evidence that perturbation-based balance training directly targets the fast, automatic protective responses required to prevent falls. By improving reactive stepping, enhancing proprioceptive sensitivity, and promoting more efficient neuromuscular control, these programs offer a highly potent and time-efficient strategy for fall prevention in community-dwelling older adults.
Beyond falls and reactive balance, many studies reported substantial gains in traditional balance outcomes, such as Berg Balance Scale scores, TUG performance, and posturographic measures. Improvements in these outcomes were observed across diverse interventions, including Tai Ji Quan [42,46], multimodal training [37], Otago [58], balance circuits [56], and strength-balance combinations [38]. These consistent gains suggest that balance-focused exercise induces robust neuromuscular adaptations regardless of specific training modality. Many of these improvements were accompanied by enhancements in mobility, particularly in gait speed, TUG, and SPPB scores. In a study by Liu-Ambrose et al. [45] demonstrated that a home-based strength-balance program yielded meaningful mobility gains alongside reductions in fall incidence, highlighting the interconnectedness of balance and functional mobility in determining overall fall risk.
Another key theme across studies was the improvement of lower-limb muscular strength, which emerged as a crucial mediator of enhanced mobility and balance. LaStayo et al. [52] reported that eccentric resistance training produced greater improvements in lower-limb strength and functional performance than traditional resistance exercise, with no significant differences in fall outcomes. This suggests that eccentric loading enhances neuromuscular and functional capacity, which may indirectly support balance and mobility. Kulkarni et al. [57], Costa et al. [56], and Lacroix et al. [38] all reported significant increases in muscle strength or power following structured exercise interventions. These gains are particularly important given the established relationship between lower-limb weakness and fall risk in older adults. Strength improvements also contributed to better performance on functional tests such as the chair stand and SPPB, demonstrating meaningful carryover from isolated strength adaptations to broader mobility gains. Importantly, strength improvements were not limited to traditional resistance training; even balance-oriented or multimodal programs such as Otago and Stay Balanced produced gains in lower-limb strength, likely due to their emphasis on functional, weight-bearing exercises. Gianoudis et al. [54] showed that a long-term multimodal program with high-velocity resistance and balance training significantly improved strength, power, dynamic balance, and bone density in older adults. However, the absence of a significant reduction in fall incidence underscores the distinction between musculoskeletal gains and direct fall outcomes, highlighting the need for task-specific balance challenges when fall prevention is the primary goal. Importantly, improvements in biomechanical, neuromuscular, or laboratory-based outcomes should be interpreted as indicators of enhanced fall resilience rather than direct proxies for reductions in real-world fall incidence.
Some studies introduced alternative models for fall prevention. The STRIDE trial Bhasin et al. [53] implemented a multifactorial, individualized fall-prevention strategy and found reductions in serious fall injuries through coordinated care, risk assessment, and targeted exercise components. Although not exclusively exercise-based, this trial underscored the importance of integrating exercise within broader fall-prevention frameworks. The ProAct65+ trials Stevens et al. [35]; Gawler et al. [39] highlighted the challenges and benefits of implementing community-based strength-balance programs within primary care settings, demonstrating feasibility and improvements in functional outcomes despite variations in implementation fidelity.
An important observation across studies is that program duration significantly influenced outcomes. Long-term interventions (12–24 months), such as those in Patil et al. [37] and El-Khoury et al. [36], produced sustained reductions in falls and injuries, while shorter interventions (4–12 weeks) tended to yield rapid gains in reactive balance and specific neuromuscular outcomes, as demonstrated by [34,47,60]. This diversity in timelines suggests that fall prevention can be achieved through both long-term conditioning and short-term targeted training, depending on specific outcomes of interest. Long-term multimodal and Otago programs appear particularly effective in reducing fall incidence, while shorter perturbation-based interventions may rapidly enhance reactive balance mechanisms. Subgroup analyses indicate that high-risk populations benefit more from these interventions, with a risk ratio of 0.72 for fall rates [61]. Women show a more pronounced benefit from exercise interventions, particularly in fracture prevention, with a risk ratio of 0.37 [64]. In contrast, while exercise interventions are effective, some studies suggest that multifactorial approaches, which include environmental modifications and education, may offer additional benefits in reducing falls and injuries [62]. This indicates a potential need for integrated strategies in fall prevention. Therefore, Regular participation in physical activity is essential for supporting long-term health, as it helps counteract chronic disease risk, strengthens the musculoskeletal system, improves balance control, and ultimately lowers the probability of experiencing falls among older adults [65,66,67].
This systematic review showed that perturbation-based balance training was one of the most consistently effective strategies for improving reactive stepping, compensatory balance, and laboratory-induced fall recovery. Studies by [47], Allin et al. [51], Aviles et al. [44], and Mansfield et al. [34] demonstrated rapid improvements in reactive balance, even in short interventions lasting 4–8 weeks. These findings are further strengthened by Nørgaard et al. [59], who reported significant real-world fall reductions following treadmill-based perturbation training in older adults. The mechanisms observed in our studies are strongly supported by foundational research showing the importance of “change-in-support” strategies [21] and the role of rapid limb movements in balance recovery [28]. Additionally, systematic reviews emphasize that perturbation-based interventions induce unique neural adaptations that traditional balance training does not elicit [27]. Even short-term pilot studies in our review, Okubo et al. [48], demonstrated improvements in motor learning and response speed, aligning with evidence that repetitive exposure to controlled slips and trips recalibrates neuromuscular timing and trunk control strategies. Together, these results indicate that perturbation-based training offers strong mechanistic and clinical value for fall prevention. Across the studies included in our review, the Otago Exercise Program (OEP) consistently improved balance, strength, and mobility, contributing to meaningful reductions in fall risk. For instance, Arkkukangas et al. [49] and Waters et al. [58] demonstrated significant improvements in functional performance and reductions in fall rates, while long-term effects were observed in the follow-up study by [50]. These findings align with broader evidence supporting the effectiveness of progressive strength-balance training in older adults, including recent analyses by Thomas et al. [61] and Guirguis-Blake et al. [62], which reported significant reductions in fall rates with exercise-based interventions. Mechanistically, these improvements are consistent with established physiological principles: targeted lower-limb resistance training enhances neuromuscular force generation [25], improves stability thresholds, and strengthens compensatory mechanisms required for safe ambulation. The OEP’s home-based format also resonates with evidence from community-based program reviews [22,23], emphasizing accessibility and sustainability as key facilitators of long-term adherence. Thus, our results reinforce OEP as a practical and effective intervention for fall prevention. However, while improvements in reactive balance and laboratory-induced fall recovery are indicative of enhanced neuromuscular preparedness, direct translation to reduced real-world fall incidence should be interpreted cautiously, as relatively few trials have examined long-term community fall outcomes following perturbation-based interventions.
Across all included studies, the overall pattern of findings reflects a compelling body of evidence indicating that exercise, irrespective of specific modality, consistently enhances essential physical attributes linked to fall prevention. Whether through traditional balance exercises, strength conditioning, Tai Ji Quan, or reactive perturbation exposure, older adults demonstrated measurable improvements in functional performance, neuromuscular efficiency, postural control, and fall resilience. The convergence of findings from diverse interventions underscores the adaptability of older adults to structured physical training and confirms that targeted exercise remains a central, evidence-based strategy for reducing fall risk.
4.1. Implications of the Study
The findings of this systematic review hold important implications for clinical practice, community-based health programs, and public health policy. The consistent effectiveness of balance-, strength-, and perturbation-based exercise interventions demonstrates that structured physical training is a powerful and modifiable strategy for reducing fall risk in older adults. Evidence from Tai Ji Quan, Otago, and multimodal programs suggests that exercise can be safely implemented across diverse settings, including home-based programs, community centers, primary care environments, and specialized clinical facilities. These results reinforce the need for integrating exercise prescriptions into routine geriatric care and fall-prevention protocols, emphasizing that even low-intensity, accessible interventions can produce clinically meaningful improvements. The growing evidence supporting perturbation-based training highlights new opportunities for innovation in fall-prevention approaches that target reactive balance mechanisms. Overall, these implications underscore the necessity of prioritizing structured exercise interventions as a foundational element of fall-prevention strategies at individual, clinical, and public health levels. Accordingly, percentage reductions in falls are reported descriptively to illustrate directional trends rather than inferential estimates, and should not be interpreted as pooled or adjusted effect sizes.
4.2. Study Limitations
This review has several limitations that should be acknowledged. First, substantial clinical and methodological heterogeneity existed across studies with respect to intervention type, duration, intensity, outcome measures, and follow-up periods, which limited the feasibility of a pooled meta-analysis and necessitated a narrative synthesis approach. Also, substantial variability existed in the biomechanical and functional assessment tools used across the included studies, including force platforms, wearable sensors, clinical balance scales, and laboratory-based perturbation systems. The lack of standardization in balance and reactive response measurements limits direct comparability across trials and may influence the interpretation of mechanistic findings relative to clinical outcomes.
Second, outcome measures and reporting formats varied widely, with some trials relying on self-reported falls or adherence, potentially introducing measurement bias. Third, several included studies were small pilot or feasibility trials with limited sample sizes, which may reduce the generalizability of findings. Fourth, although comprehensive search strategies were employed, only English-language, peer-reviewed full-text articles were included, which may increase the risk of language or publication bias. Finally, incomplete reporting of allocation concealment, blinding, or long-term follow-up in some studies contributed to “some concerns” ratings in the risk-of-bias assessment and may influence confidence in the strength of the evidence. Accordingly, the findings of this review should be interpreted as evidence of consistent directional benefits of exercise-based interventions rather than definitive comparative or causal conclusions.
4.3. Recommendations for Future Research and Practice
Future research should prioritize the standardization of outcome measures, particularly fall incidence, reactive balance, mobility tests, and lower-limb strength assessments, to enable more robust comparisons and meta-analytic synthesis. Long-term follow-up studies are needed to better understand the sustainability of intervention effects, particularly for perturbation-based and multimodal programs. Researchers should also explore the integration of technology-assisted balance training, such as sensor-based feedback and virtual perturbation systems, which may enhance training specificity and adherence. Greater emphasis should be placed on recruiting more diverse populations, including those over 80 years, individuals with chronic conditions, and underrepresented cultural groups. Clinically, practitioners are encouraged to incorporate structured balance and strength training into routine geriatric care, adapt interventions based on individual risk profiles, and promote adherence through behavioral support strategies. Finally, combining traditional balance and strength programs with perturbation-based training may offer a more comprehensive approach to fall prevention and should be explored in future randomized trials.
5. Conclusions
This systematic review demonstrates that exercise-based interventions targeting balance, lower-limb strength, and reactive postural control are effective in reducing fall risk and improving functional performance in community-dwelling older adults. Strong and consistent evidence supports Tai Ji Quan, the Otago Exercise Program, and multimodal strength–balance training for reducing real-world falls, while perturbation-based balance training shows robust mechanistic benefits by enhancing reactive stepping and fall-recovery responses. From a practical perspective, fall-prevention programs should prioritize structured, progressive balance-strength exercises and, where feasible, incorporate task-specific reactive balance training to address unexpected perturbations encountered in daily life. Future research should focus on standardized outcome measures, longer follow-up periods, and scalable community-based delivery models to strengthen evidence translation into routine geriatric care and public health policy.
Author Contributions
Conceptualization, P.K.C.; data curation, P.K.C., S.C. and İ.İ.; formal analysis, P.K.C. and S.C.; investigation, B.K. and S.S.; methodology, P.K.C. and S.C.; resources, B.K., İ.İ. and G.J.T.; visualization, S.S.; writing—original draft preparation, İ.İ.; writing—review and editing, B.K., S.S. and G.J.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data supporting the findings of this systematic review are derived from previously published studies. No new datasets were generated or analyzed during the current study. The full list of included articles, along with extraction sheets and methodological details, is available from the corresponding author upon reasonable request.
Acknowledgments
The authors express their sincere appreciation to the administrative and technical staff of the Lakshmibai National Institute of Physical Education, Gwalior, for their support throughout the completion of this systematic review. We also thank the Montenegrin Sports Academy for their academic guidance and cooperation during various stages of the study.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| BBS | Berg Balance Scale |
| OEP | Otago Exercise Program |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROSPERO | International Prospective Register for Systematic Reviews |
| RCT | Randomized controlled trial |
| ROB-2 | Cochrane Risk of Bias tool |
| SPPB | Short Physical Performance Battery |
| TUG | Timed Up and Go |
| LiFE | Lifestyle-Integrated Functional Exercise |
| STRIDE | Strategies to Reduce Injuries and Develop Confidence in Elders |
| IMU | Inertial Measurement Unit |
References
- Poncumhak, P.; Srithawong, A.; Namwong, W.; Duangsanjun, W. Ability of a New Fear of Falling Scale in Assessing Fall Risk and Its Correlation with Functional Balance in Community-Dwelling Older Adults. Phys. Act. Health 2025, 9, 124–131. [Google Scholar] [CrossRef]
- Kalache, A.; Fu, D.; Yoshida, S.; Al-Faisal, W.; Beattie, L.; Chodzko-Zajko, W.; Fu, H.; James, K.; Kalula, S.; Krishnaswamy, B.; et al. World Health Organisation Global Report on Falls Prevention in Older Age; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Devassy, S.M.; Scaria, L. Prevalence and risk factors for falls in community-dwelling older population in Kerala; results from a cross sectional survey. Heliyon 2023, 9, e18737. [Google Scholar]
- European Public Health Alliance. Falls in Older Adults in the EU: Factsheet; European Public Health Alliance: Brussels, Belgium, 2016. [Google Scholar]
- Turner, S.; Kisser, R.; Rogmans, W. Fall Among Older Adults in the EU-28. The European Public Health Association. 2015. Available online: https://eupha.org/repository/sections/ipsp/Factsheet_falls_in_older_adults_in_EU.pdf (accessed on 10 March 2021).
- Peeters, G.; van Schoor, N.M.; Lips, P. Fall risk: The clinical relevance of falls and how to integrate fall risk with fracture risk. Best Pract. Res. Clin. Rheumatol. 2009, 23, 797–804. [Google Scholar] [CrossRef]
- Deandrea, S.; Lucenteforte, E.; Bravi, F.; Foschi, R.; La Vecchia, C.; Negri, E. Risk factors for falls in community-dwelling older people: A systematic review and meta-analysis. Epidemiology 2010, 21, 658–668. [Google Scholar] [CrossRef]
- Karinkanta, S.; Piirtola, M.; Sievänen, H.; Uusi-Rasi, K.; Kannus, P. Physical therapy approaches to reduce fall and fracture risk among older adults. Nat. Rev. Endocrinol. 2010, 6, 396–407. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.W.; Ko, I.S.; Lee, K.J. Health promotion behaviors and quality of life among community-dwelling elderly in Korea: A cross-sectional survey. Int. J. Nurs. Stud. 2006, 43, 293–300. [Google Scholar] [CrossRef]
- Uusi-Rasi, K.; Patil, R.; Karinkanta, S.; Kannus, P.; Tokola, K.; Lamberg-Allardt, C.; Sievänen, H. A 2-Year Follow-Up After a 2-Year RCT with Vitamin D and Exercise: Effects on Falls, Injurious Falls and Physical Functioning Among Older Women. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2017, 72, 1239–1245. [Google Scholar] [CrossRef]
- Choudhary, P.K.; Dubey, S.; Rawat, B.; Kumar, S.; Pratap, B.; Bangari, D.; Kumar, S.; Prasad, S.; Kaunteya, D.S. Assessing Strength Effort in Pre-Adolescent Girls: Insights into Effort Accuracy at Different Strength Thresholds. Phys. Educ. Theory Methodol. 2024, 24, 873–880. [Google Scholar] [CrossRef]
- Choudhary, P.K.; Dubey, S. Physiological effects of Zumba exercise on male college students: An intervention study. Phys. Educ. Theory Methodol. 2024, 24, 404–410. [Google Scholar] [CrossRef]
- Benichou, O.; Lord, S.R. Rationale for Strengthening Muscle to Prevent Falls and Fractures: A Review of the Evidence. Calcif. Tissue Int. 2016, 98, 531–545. [Google Scholar] [CrossRef]
- Toraman, A.; Yildirim, N.U. The Falling Risk and Physical Fitness in Older People. Arch. Gerontol. Geriatr. 2010, 51, 222–226. [Google Scholar] [CrossRef]
- Boyé, N.; Van Lieshout, E.M.M.; van Beeck, E.; Hartholt, K.; van der Cammen, T.J.M.; Patka, P. The Impact of Falls in the Elderly. Trauma 2013, 15, 29–35. [Google Scholar] [CrossRef]
- Franco, M.R.; Pereira, L.S.; Ferreira, P.H. Exercise Interventions for Preventing Falls in Older People Living in the Community. Br. J. Sports Med. 2014, 48, 867–868. [Google Scholar] [CrossRef]
- Paterson, D.H.; Warburton, D.E.R. Physical Activity and Functional Limitations in Older Adults: A Systematic Review Related to Canada’s Physical Activity Guidelines. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 38. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.Y.; Wang, Y.L.; Cheng, F.Y.; Chao, Y.H.; Chen, C.L.; Yang, Y.R. Effects of Combined Exercise on Gait Variability in Community-Dwelling Older Adults. Age 2015, 37, 9780. [Google Scholar] [CrossRef] [PubMed]
- Ács, P.; Stocker, M.; Füge, K.; Paár, D.; Oláh, A.; Kovács, A. Economic and Public Health Benefits: The Result of Increased Regular Physical Activity. Eur. J. Integr. Med. 2016, 8, 8–12. [Google Scholar] [CrossRef]
- Severance, J.; Rivera, S.; Cho, J.; Hartos, J.L.; Khan, A.; Knebl, J. A Collaborative Implementation Strategy to Increase Falls Prevention Training Using the Age-Friendly Health Systems Approach. Int. J. Environ. Res. Public Health 2022, 19, 5903. [Google Scholar] [CrossRef]
- Kulkarni, A. Case Report: Multifactorial Intervention for Safe Aging in Place. Geriatrics 2025, 10, 68. [Google Scholar] [CrossRef]
- Granacher, U.; Gollhofer, A.; Hortobágyi, T.; Kressig, R.W.; Muehlbauer, T. The Importance of Trunk Muscle Strength for Balance, Functional Performance, and Fall Prevention in Seniors: A Systematic Review. Sports Med. 2013, 43, 627–641. [Google Scholar] [CrossRef]
- Maki, B.E.; McIlroy, W.E. Control of Rapid Limb Movements for Balance Recovery: Age-Related Changes and Implications for Fall Prevention. Age Ageing 2006, 35, ii12–ii18. [Google Scholar] [CrossRef]
- Avers, D. Community-Based Exercise Programs for Older Adults. Top. Geriatr. Rehabil. 2010, 26, 275–298. [Google Scholar] [CrossRef]
- Fien, S.; Linton, C.; Mitchell, J.S.; Wadsworth, D.P.; Szabo, H.; Askew, C.D.; Schaumberg, M.A. Characteristics of Community-Based Exercise Programs for Community-Dwelling Older Adults in Rural/Regional Areas: A Scoping Review. Aging Clin. Exp. Res. 2022, 34, 1511–1528. [Google Scholar] [CrossRef]
- Sherrington, C.; Fairhall, N.J.; Wallbank, G.K.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S.E. Exercise for Preventing Falls in Older People Living in the Community. Cochrane Database Syst. Rev. 2019, 1, CD012424. [Google Scholar] [CrossRef]
- Peterson, M.D.; Gordon, P.M. Resistance Exercise for the Aging Adult: Clinical Implications and Prescription Guidelines. Am. J. Med. 2011, 124, 194–198. [Google Scholar] [CrossRef]
- Horak, F.B. Postural Orientation and Equilibrium: What Do We Need to Know About Neural Control of Balance to Prevent Falls? Age Ageing 2006, 35, ii7–ii11. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Prictor, M.; Hill, S. Cochrane Consumers and Communication Review Group: Leading the Field on Health Communication Evidence. J. Evid. Based Med. 2013, 6, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 6.2; Cochrane: London, UK, 2020. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomized Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C.; et al. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Mansfield, A.; Peters, A.L.; Liu, B.A.; Maki, B.E. Effect of a Perturbation-Based Balance Training Program on Compensatory Stepping and Grasping Reactions in Older Adults: A Randomized Controlled Trial. Phys. Ther. 2010, 90, 476–491. [Google Scholar] [CrossRef] [PubMed]
- Stevens, Z.; Carpenter, H.; Gawler, S.; Belcher, C.; Haworth, D.; Kendrick, D.; Morris, R.; Masud, T.; Skelton, D.A.; Iliffe, S.; et al. Lessons Learnt During a Complex, Multicentre Cluster Randomized Controlled Trial: The ProAct65+ Trial. Trials 2013, 14, 192. [Google Scholar] [CrossRef]
- El-Khoury, F.; Cassou, B.; Latouche, A.; Aegerter, P.; Charles, M.; Dargent-Molina, P. Effectiveness of a Two-Year Balance-Training Programme on Prevention of Fall-Induced Injuries in At-Risk Women Aged 75–85 Living in the Community: Ossébo Randomized Controlled Trial. BMJ 2015, 351, h3830. [Google Scholar] [CrossRef] [PubMed]
- Patil, R.; Uusi-Rasi, K.; Tokola, K.; Karinkanta, S.; Kannus, P.; Sievänen, H. Effects of a Multimodal Exercise Program on Physical Function, Falls, and Injuries in Older Women: A 2-Year Community-Based Randomized Controlled Trial. J. Am. Geriatr. Soc. 2015, 63, 1306–1313. [Google Scholar] [CrossRef]
- Lacroix, A.; Kressig, R.W.; Muehlbauer, T.; Gschwind, Y.J.; Pfenninger, B.; Bruegger, O.; Granacher, U. Effects of a Supervised Versus an Unsupervised Combined Balance and Strength Training Program on Balance and Muscle Power in Healthy Older Adults: A Randomized Controlled Trial. Gerontology 2016, 62, 275–288. [Google Scholar] [CrossRef]
- Gawler, S.; Skelton, D.A.; Dinan-Young, S.; Masud, T.; Morris, R.W.; Griffin, M.; Kendrick, D.; Iliffe, S.; ProAct65+ Team. Reducing Falls Among Older People in General Practice: The ProAct65+ Exercise Intervention Trial. Arch. Gerontol. Geriatr. 2016, 67, 46–54. [Google Scholar] [CrossRef]
- Trombetti, A.; Hars, M.; Herrmann, F.R.; Kressig, R.W.; Ferrari, S.; Rizzoli, R. Effect of Music-Based Multitask Training on Gait, Balance, and Fall Risk in Elderly People: A Randomized Controlled Trial. Arch. Intern. Med. 2011, 171, 525–533. [Google Scholar] [CrossRef]
- Boongird, C.; Keesukphan, P.; Phiphadthakusolkul, S.; Rattanasiri, S.; Thakkinstian, A. Effects of a Simple Home-Based Exercise Program on Fall Prevention in Older Adults: A 12-Month Primary Care Setting Randomized Controlled Trial. Geriatr. Gerontol. Int. 2017, 17, 2157–2163. [Google Scholar] [CrossRef]
- Li, F.; Harmer, P.; Fitzgerald, K.; Eckstrom, E.; Akers, L.; Chou, L.S.; Pidgeon, D.; Voit, J.; Winters-Stone, K. Effectiveness of a Therapeutic Tai Ji Quan Intervention vs. a Multimodal Exercise Intervention to Prevent Falls Among Older Adults at High Risk of Falling: A Randomized Clinical Trial. JAMA Intern. Med. 2018, 178, 1301–1310. [Google Scholar] [CrossRef]
- Jansen, C.P.; Nerz, C.; Kramer, F.; Labudek, S.; Klenk, J.; Dams, J.; König, H.H.; Clemson, L.; Becker, C.; Schwenk, M. Comparison of a Group-Delivered and Individually Delivered Lifestyle-Integrated Functional Exercise (LiFE) Program in Older Persons: A Randomized Noninferiority Trial. BMC Geriatr. 2018, 18, 267. [Google Scholar] [CrossRef] [PubMed]
- Aviles, J.; Allin, L.J.; Alexander, N.B.; Van Mullekom, J.; Nussbaum, M.A.; Madigan, M.L. Comparison of Treadmill Trip-Like Training Versus Tai Ji Quan to Improve Reactive Balance Among Independent Older Adult Residents of Senior Housing: A Pilot Controlled Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 1497–1503. [Google Scholar] [CrossRef] [PubMed]
- Liu-Ambrose, T.; Davis, J.C.; Best, J.R.; Dian, L.; Madden, K.; Cook, W.; Hsu, C.L.; Khan, K.M. Effect of a Home-Based Exercise Program on Subsequent Falls Among Community-Dwelling High-Risk Older Adults After a Fall: A Randomized Clinical Trial. JAMA 2019, 321, 2092–2100. [Google Scholar] [CrossRef]
- Li, F.; Harmer, P.; Eckstrom, E.; Fitzgerald, K.; Chou, L.S.; Liu, Y. Effectiveness of Tai Ji Quan vs. Multimodal and Stretching Exercise Interventions for Reducing Injurious Falls in Older Adults at High Risk of Falling: Follow-Up Analysis of a Randomized Clinical Trial. JAMA Netw. Open 2019, 2, e188280. [Google Scholar] [CrossRef] [PubMed]
- Okubo, Y.; Sturnieks, D.L.; Brodie, M.A.; Duran, L.; Lord, S.R. Effect of Reactive Balance Training Involving Repeated Slips and Trips on Balance Recovery Among Older Adults: A Blinded Randomized Controlled Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 1489–1496. [Google Scholar] [CrossRef] [PubMed]
- Okubo, Y.; Brodie, M.A.; Sturnieks, D.L.; Hicks, C.; Lord, S.R. A Pilot Study of Reactive Balance Training Using Trips and Slips with Increasing Unpredictability in Young and Older Adults. Clin. Biomech. 2019, 67, 171–179. [Google Scholar] [CrossRef]
- Arkkukangas, M.; Söderlund, A.; Eriksson, S.; Johansson, A.C. Fall Preventive Exercise with or Without Behavior Change Support for Community-Dwelling Older Adults: A Randomized Controlled Trial with Short-Term Follow-Up. J. Geriatr. Phys. Ther. 2019, 42, 9–17. [Google Scholar] [CrossRef]
- Cederbom, S.; Arkkukangas, M. Impact of the Fall Prevention Otago Exercise Programme on Pain Among Community-Dwelling Older Adults: A Short- and Long-Term Follow-Up Study. Clin. Interv. Aging 2019, 14, 721–726. [Google Scholar] [CrossRef]
- Allin, L.J.; Brolinson, P.G.; Beach, B.M.; Kim, S.; Nussbaum, M.A.; Roberto, K.A.; Madigan, M.L. Perturbation-Based Balance Training Targeting Both Slip- and Trip-Induced Falls Among Older Adults: A Randomized Controlled Trial. BMC Geriatr. 2020, 20, 205. [Google Scholar] [CrossRef]
- LaStayo, P.; Marcus, R.; Dibble, L.; Wong, B.; Pepper, G. Eccentric versus traditional resistance exercise for older adult fallers in the community: A randomized trial within a multi-component fall reduction program. BMC Geriatr. 2017, 17, 149. [Google Scholar] [CrossRef]
- Bhasin, S.; Gill, T.M.; Reuben, D.B.; Latham, N.K.; Ganz, D.A.; Greene, E.J.; Dziura, J.; Basaria, S.; Gurwitz, J.H.; Dykes, P.C.; et al. A Randomized Trial of a Multifactorial Strategy to Prevent Serious Fall Injuries. N. Engl. J. Med. 2020, 383, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Gianoudis, J.; Bailey, C.A.; Ebeling, P.R.; Nowson, C.A.; Sanders, K.M.; Hill, K.; Daly, R.M. Effects of a Targeted Multimodal Exercise Program Incorporating High-Speed Power Training on Falls and Fracture Risk Factors in Older Adults: A Community-Based Randomized Controlled Trial. J. Bone Miner. Res. 2013, 29, 182–191. [Google Scholar] [CrossRef]
- Halvarsson, A.; Roaldsen, K.S.; Nilsen, P.; Dohrn, I.-M.; Ståhle, A. StayBalanced: Implementation of Evidence-Based Fall Prevention Balance Training for Older Adults Cluster Randomized Controlled and Hybrid Type 3 Trial. Trials 2021, 22, 166. [Google Scholar] [CrossRef]
- Costa, J.N.A.; Ribeiro, A.L.A.; Ribeiro, D.B.G.; Neri, S.G.R.; Barbosa, D.F.; Avelar, B.P.; Safons, M.P. Balance Exercise Circuit for Fall Prevention in Older Adults: A Randomized Controlled Crossover Trial. J. Frailty Sarcopenia Falls 2022, 7, 60–71. [Google Scholar] [CrossRef]
- Kulkarni, N.; Tsepis, E.; Phalke, V.; Tilekar, S.; Pouliasi, K.; Theodoritzi, M.; Mahajan, A. A Randomized Controlled Trial on Impact of Group Exercise Programme on Fall Risk, Balance, Strength, Fear of Fall and Quality of Life of Older Adults. J. Gerontol. Geriatr. 2022, 71, 47–60. [Google Scholar] [CrossRef]
- Waters, D.L.; Popp, J.; Herman, C.; Ghahate, D.; Bobelu, J.; Pankratz, V.S.; Shah, V.O. The Otago Exercise Program Compared to Falls Prevention Education in Zuni Elders: A Randomized Controlled Trial. BMC Geriatr. 2022, 22, 652. [Google Scholar] [CrossRef] [PubMed]
- Nørgaard, J.E.; Andersen, S.; Ryg, J.; Stevenson, A.J.T.; Andreasen, J.; Oliveira, A.S.; Danielsen, M.B.; Jorgensen, M.G. Effect of Treadmill Perturbation-Based Balance Training on Fall Rates in Community-Dwelling Older Adults: A Randomized Clinical Trial. JAMA Netw. Open 2023, 6, e238422. [Google Scholar] [CrossRef]
- Petrovic, A.; Wirth, R.; Klimek, C.; Lueg, G.; Daubert, D.; Giehl, C.; Trampisch, U.S. Impact of Reactive Balance Training on a Perturbation Treadmill on Physical Performance in Geriatric Patients: Results of a Single-Center Assessor-Blinded Randomized Controlled Trial. J. Clin. Med. 2024, 13, 5790. [Google Scholar] [CrossRef] [PubMed]
- Granacher, U.; Muehlbauer, T.; Gruber, M. A Qualitative Review of Balance and Strength Performance in Healthy Older Adults: Impact for Testing and Training. J. Aging Res. 2012, 2012, 708905. [Google Scholar] [CrossRef]
- Maki, B.E.; McIlroy, W.E. The Role of Limb Movements in Maintaining Upright Stance: The “Change-in-Support” Strategy. Phys. Ther. 1997, 77, 488–507. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.; Kirk, J.; Patel, R.; Fred, M. Standing Strong: A Systematic Review of Multifaceted Fall Prevention in Older Adults. medRxiv 2024. [Google Scholar] [CrossRef]
- Guirguis-Blake, J.; Perdue, L.A.; Coppola, E.L.; Bean, S.I. Interventions to Prevent Falls in Older Adults. JAMA 2024, 332, 58–69. [Google Scholar] [CrossRef]
- de Faria, B.L. Benefits of Physical Activity in Preventing Falls and Improving Functionality in Older Adults. Rev. Fisioter. 2025, 29, 16–17. [Google Scholar] [CrossRef]
- Wong, R.M.Y.; Chong, K.C.; Law, S.-W.; Ho, W.-T.; Li, J.; Chui, C.; Chow, S.K.-H.; Cheung, W.-H. The Effectiveness of Exercises on Fall and Fracture Prevention Amongst Community Elderlies: A Systematic Review and Meta-Analysis. J. Orthop. Transl. 2020, 24, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Sadaqa, M.; Németh, Z.; Makai, A.; Prémusz, V.; Hock, M. Effectiveness of Exercise Interventions on Fall Prevention in Ambulatory Community-Dwelling Older Adults: A Systematic Review with Narrative Synthesis. Front. Public Health 2023, 11, 1209319. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.