Single or Double-Lumen Aspiration Needle? Revisiting Choices for In Vitro Fertilization or Intracytoplasmic Sperm Injection—A Critical Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
Quality Assessment of Study Findings
4. Discussion
4.1. Numbers of Retrieved Oocytes
4.2. Number of Mature (MII) Oocytes
4.3. Procedure Duration
4.4. Procedural Complications
4.5. Fertilization Rates and Number of Good Quality Embryos
4.6. Clinical Pregnancy Rate, Ongoing Pregnancy Rate, and Live Birth Rate
4.7. Benefits and Drawbacks of SLN and DLN
4.8. Confounding Factors and Limitations of the Studies
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ART | Assisted reproductive technology |
| SLN | Single-lumen aspiration needle |
| DLN | Double-lumen aspiration needle |
| IVF | In vitro fertilization |
| ICSI | Intracytoplasmic sperm injection |
| PN | Pronuclei |
| COC | Cumulus-oocyte complex |
| MII | Mature oocyte |
| SD | Standard deviation |
| OHSS | Ovarian hyperstimulation syndrome |
References
- Ronchetti, C.; Cirillo, F.; Immediata, V.; Gargasole, C.; Scolaro, V.; Morenghi, E.; Patrizio, P. A Monocentric Randomized Controlled Clinical Trial to Compare Single- and Double-Lumen Needles in Oocyte Retrieval Procedure in Assisted Reproductive Technologies. Reprod. Sci. 2023, 9, 2866–2875. [Google Scholar] [CrossRef]
- De Souza, M.M.; Mancebo, A.C.A.; de Souza, M.D.C.B.; de Azevedo Antunes, R.; Barbeitas, A.L.; de Almeida Raupp, V.; da Silva, L.A.B.D.; Siqueira, F.; de Souza, A.L.B.M. Evaluation of follicular flushing with double lumen needle in patients undergoing assisted reproductive technology treatments. JBRA Assist. Reprod. 2021, 25, 272–275. [Google Scholar] [CrossRef] [PubMed]
- Wallace Single Lumen Oocyte Recovery Systems. Available online: https://www.coopersurgical.com/product/wallace-single-lumen-oocyte-recovery-systems/ (accessed on 7 May 2025).
- Wallace Dual Lumen Oocyte Recovery Systems. Available online: https://www.coopersurgical.com/product/wallace-dual-lumen-oocyte-recovery-systems/ (accessed on 7 May 2025).
- Huang, T.J.; Huang, H.C.; Tsai, H.D.; Kor, C.T.; Yang, C.K.; Wu, H.H. Introduction of the single-lumen oocyte retrieval needle in an assisted reproductive technology center: Propensity score matching analysis of grouping Taiwan. J. Obs. Gynecol. 2025, 64, 105–109. [Google Scholar] [CrossRef]
- Von Horn, K.; Marion, D.; Askan, S.; Georg, G. Randomized, open trial comparing a modified double-lumen needle follicular flushing system with a single-lumen aspiration needle in IVF patients with poor ovarian response. Hum. Reprod. 2017, 32, 832–835. [Google Scholar] [CrossRef]
- Weijie, X.; Jianping, O.; Liuhong, C.; Xin, T. Double-Lumen Needle Follicular Flushing System versus Single-Lumen Aspiration Needle in IVF/ICSI Patients with Poor Ovarian Response: A Meta-Analysis. Adv. Sex. Med. 2017, 7, 167–178. [Google Scholar] [CrossRef]
- Bulent, H.; Tayfun, C.; Esra, B.; Ayse, H.; Erhan, S.; Tayfun, B. In vitro fertilization–intracytoplasmic sperm injection outcomes in single- versus double-lumen oocyte retrieval needles in normally responding patients: A randomized trial. Fertil. Steril. 2011, 95, 812–814. [Google Scholar]
- Hans-Peter, S. Optimizing Technique in Follicular Aspiration and Flushing. In Textbook of Minimal Stimulation IVF-Milder, Mildest or Back to Nature, 1st ed.; Alejandro, C., Gautam, N., Eds.; Jaypee Brothers Medical Pub: New Delhi, India, 2011; pp. 98–102. [Google Scholar]
- Poiseuille’s Law. Available online: https://phys.libretexts.org/@go/page/8532 (accessed on 16 July 2025).
- Robert, H.; Christopher, J.B.; Geoff, R.; Carl, W.; Gabor, T.K. Aspiration of oocytes for in-vitro fertilization. Hum. Reprod. Update 1996, 2, 77–85. [Google Scholar][Green Version]
- Lozano, D.H.; Fanchin, R.; Chevalier, N.; Feyereisen, E.; Hesters, L.; Frydman, N.; Frydman, R. Optimising the semi natural cycle IVF: The importance of follicular flushing. J. Indian Med. Assoc. 2006, 104, 423–427. [Google Scholar]
- Hill, M.J.; Levens, E.D. Is there a benefit in follicular flushing in assisted reproductive technology? Curr. Opin. Obs. Gynecol. 2010, 22, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Mehri, S.; Levi, S.; Setti, P.E.L.; Greco, K.; Sakkas, D.; Martinez, G.; Patrizio, P. Correlation between Follicular Diameters and Flushing versus No Flushing on Oocyte Maturity, Fertilization Rate and Embryo Quality. J. Assist. Reprod. Genet. 2014, 31, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Meixiang, Z.; Hao, S.; Shiqi, Y.; Qian, L.; Yingchun, S.; Guo, Y.; Hu, L.; Sun, J.; Sun, Y.-P. Causes and Effects of Oocyte Retrieval Difficulties: A Retrospective Study of 10,624 Cycles. Front. Endocrinol. 2022, 12, 564344. [Google Scholar] [CrossRef]
- Georgiou, E.X.; Melo, P.; Brown, J.; Granne, I.E. Follicular flushing during oocyte retrieval in assisted reproductive techniques. Cochrane Database Syst. Rev. 2018, 4, CD004634. [Google Scholar] [CrossRef] [PubMed]
- Lainas, G.; Lainas, T.; Kolibianakis, E. The importance of follicular flushing in optimizing oocyte retrieval. Curr. Opin. Obs. Gynecol. 2023, 35, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Rose, B.I. Approaches to oocyte retrieval for advanced reproductive technology cycles planning to utilize in vitro maturation: A review of the many choices to be made. J. Assist. Reprod. Genet. 2014, 31, 1409–1419. [Google Scholar] [CrossRef]
- Matheus, R.; Marcos, S.; Selmo, G.; Marcos, S.; Selmo, G. Follicular flushing during oocyte retrieval: A systematic review and meta-analysis. J. Assist. Reprod. Genet. 2012, 29, 1249–1254. [Google Scholar] [CrossRef]
- Levy, G.; Hill, M.J.; Ramirez, C.I.; Correa, L.; Ryan, M.E.; DeCherney, A.H.; Levens, E.D.; Whitcomb, B.W. The use of follicle flushing during oocyte retrieval in assisted reproductive technologies: A systematic review and meta-analysis. Hum. Reprod. 2012, 27, 2373–2379. [Google Scholar] [CrossRef] [PubMed]
- Mendez, L.D.; Scheffer, J.B.; Frydman, N.; Fay, S.; Fanchin, R.; Frydman, R. Optimal reproductive competence of oocytes retrieved through follicular flushing in minimal stimulation IVF. Reprod. Biomed. Online 2008, 16, 119–123. [Google Scholar] [CrossRef]
- Sesh, K.; Vivian, R.; Nick, R.; Siladitya, B.; Javier, Z.; Arri, C. Association between the number of eggs and live birth in IVF treatment: An analysis of 400 135 treatment cycles. Hum. Reprod. 2011, 26, 1768–1774. [Google Scholar] [CrossRef]
- Oudendijk, J.; Yarde, F.; Eijkemans, M.; Broekmans, F.; Broer, S. The poor responder in IVF: Is the prognosis always poor? A systematic review. Hum. Reprod. Update 2012, 18, 1–11. [Google Scholar] [CrossRef]
- John, J.W.; John, H.P. A prospective study to investigate the value of flushing follicles during transvaginal ultrasound-directed follicle aspiration. Fertil. Steril. 1992, 57, 221–223. [Google Scholar] [CrossRef]
- Seyhan, A.; Ata, B.; Son, W.Y.; Dahan, M.H.; Tan, S.L. Comparison of complication rates and pain scores after transvaginal ultrasound-guided oocyte pickup procedures for in vitro maturation and in vitro fertilization cycles. Fertil. Steril. 2014, 101, 705–709. [Google Scholar] [CrossRef] [PubMed]
- Bagtharia, S.; Haloob, A.R. Is there a benefit from routine follicular flushing for oocyte retrieval? J. Obs. Gynaecol. 2005, 25, 374–376. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, P. The History of Poiseuille’s Law. Annu. Rev. Fluid. Mech. 1993, 25, 1–19. [Google Scholar]
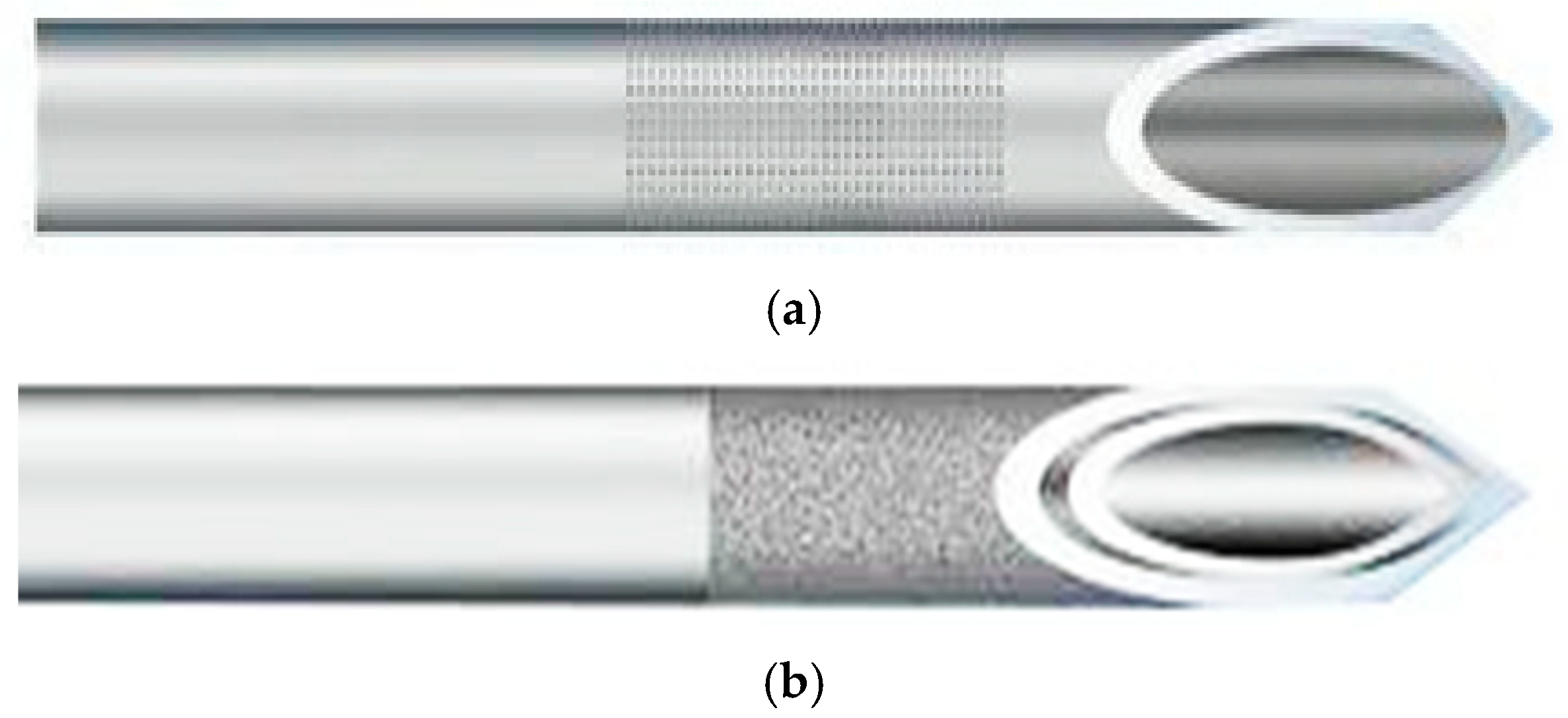

| Needle Types | Single-Lumen Needle | Double-Lumen Needle |
|---|---|---|
| Principal/Function | Has one channel for follicular fluid aspiration | Has two channels: one for aspiration and one for flushing |
| Gauge Range/Options | 16G to 21G | 16G and 17G, commonly used |
| Outer Diameter | 16G: corresponds to 1.6 mm 17G: corresponds to 1.4 mm 18G: corresponds to 1.2 mm 19G: corresponds to 1.1 mm 20G: corresponds to 0.9 mm 21G: corresponds to 0.8 mm | 16G: corresponds to 1.65 mm 17G: corresponds to 1.5 mm |
| Inner Diameter | 16G: corresponds to 1.4 mm 17G: corresponds to 1.2 mm 18G: corresponds to 1.0 mm 19G: corresponds to 0.8 mm 20G: corresponds to 0.6 mm 21G: corresponds to 0.6 mm | 16G: corresponds to 1.0 mm 17G: corresponds to 0.9 mm |
| Needle Length | Commonly around 300–350 mm | Commonly around 300–350 mm |
| Aspiration/Flushing Tubing Length | Typically 900–1000 mm | Typically 900–1000 mm |
| Author and Year | Title of Article/Study Design | Country | Sample Characteristics | Type of Needle/ Flushing Method | Follicle to Oocyte Index | Conclusions |
|---|---|---|---|---|---|---|
| Bulent H et al., 2011 [8] | In vitro fertilization–intracytoplasmic sperm injection outcomes in single versus double-lumen oocyte retrieval needles in normally responding patients: a randomized trial; prospective randomized | Turkey | Age—25 to 35 years SLN, n = 125 DLN, n = 149 Normal responder | SLN—17G Cook DLN—17G Cook DLN-flushing 1 time with 2 mL flushing media | Not mentioned | DLN did not demonstrate beneficial effect compared with SLN in terms of retrieved oocytes, clinical pregnancy rates, and live birth rates. DLN had a statistically longer duration of oocyte retrieval compared to SLN. |
| Camilla R et al., 2023 [1] | A Monocentric Randomized Controlled Clinical Trial to Compare Single and Double- Lumen Needles in Oocyte Retrieval Procedure in Assisted Reproductive Technologies; prospective randomized | Italy | Age—18 to 42 years SLN, n = 100 DLN, n = 100 Type of responder not mentioned | SLN—17G Cook DLN—17G Cook DLN-flushing 2 times, volume of flushing not mentioned | SLN—81% DLN—83% | No significant differences in terms of retrieval efficacy using SLN or DLN. DLN: significant increase in duration of the retrieval procedures. |
| Kyra von H et al., 2017 [6] | Randomized, open trial comparing a modified double-lumen needle follicular flushing system with a single- lumen aspiration needle in IVF patients with poor ovarian response; prospective randomized | Germany | Age—18 to 45 years SLN, n = 40 DLN, n = 40 Poor responder | SLN—17G Gynetics DLN-17G Steiner-Tan Needle flushing system DLN-flushing 3 times with flushing media, volume of flushing not mentioned | SLN—70% DLN—60% | No differences were observed in metaphase II oocytes, two pronuclear oocytes, number of patients having an embryo transfer, and Depression Anxiety and Stress Scale (DASS 21) scores. The procedure duration was significantly increased 2-fold in DLN. |
| Marcelo M et al., 2021 [2] | Evaluation of follicular flushing with double lumen needle in patients undergoing assisted reproductive technology treatments; prospective randomized | Brazil | Age—34 to 42 years SLN, n = 103 DLN, n = 105 Poor responder | SLN—19G Wallace DLN—17G Wallace DLN-flushing 2 times with half buffered medium, volume of flushing not mentioned | SLN—98% DLN—93% | No difference in the oocyte per follicle ratio, follicular flushing with DLN did not increase the number of oocytes recovered from poor responders. Recommended that direct aspiration with an SLN be used as the standard procedure for all patients. |
| Tian-JH et al., 2025 [5] | Introduction of the single- lumen oocyte retrieval needle in an assisted reproductive technology center: Propensity score matching analysis of grouping; retrospective cohort study (age, AMH, and body weight) | Taiwan | Age—31 to 41 years SLN, n = 228 DLN, n = 684 Type of responder not mentioned | SLN—18G KITAZATO DLN—17G Cook DLN-flushing 1–3 times, volume of 1–3 mL flushing media each time | Not mentioned | SLN reduced the procedure duration compared with DLN. SLN also increased the number of oocytes retrieved and the number of normal zygotes (2-PN) compared with DLN. Total number of viable embryos and the pregnancy rate per cycle demonstrates a favorable trend with SLN. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muruti, G.; Ahmad, M.F.; Abu, M.A.; Latif, N.I.A.; Karim, A.K.A. Single or Double-Lumen Aspiration Needle? Revisiting Choices for In Vitro Fertilization or Intracytoplasmic Sperm Injection—A Critical Review. Life 2025, 15, 1334. https://doi.org/10.3390/life15091334
Muruti G, Ahmad MF, Abu MA, Latif NIA, Karim AKA. Single or Double-Lumen Aspiration Needle? Revisiting Choices for In Vitro Fertilization or Intracytoplasmic Sperm Injection—A Critical Review. Life. 2025; 15(9):1334. https://doi.org/10.3390/life15091334
Chicago/Turabian StyleMuruti, Gopinath, Mohd Faizal Ahmad, Muhammad Azrai Abu, Nurul Ilani Abdul Latif, and Abdul Kadir Abdul Karim. 2025. "Single or Double-Lumen Aspiration Needle? Revisiting Choices for In Vitro Fertilization or Intracytoplasmic Sperm Injection—A Critical Review" Life 15, no. 9: 1334. https://doi.org/10.3390/life15091334
APA StyleMuruti, G., Ahmad, M. F., Abu, M. A., Latif, N. I. A., & Karim, A. K. A. (2025). Single or Double-Lumen Aspiration Needle? Revisiting Choices for In Vitro Fertilization or Intracytoplasmic Sperm Injection—A Critical Review. Life, 15(9), 1334. https://doi.org/10.3390/life15091334








