Cognitive Slowing, Dysfunction in Verbal Working Memory, Divided Attention and Response Inhibition in Post COVID-19 Condition in Young Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Measurements
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Sample
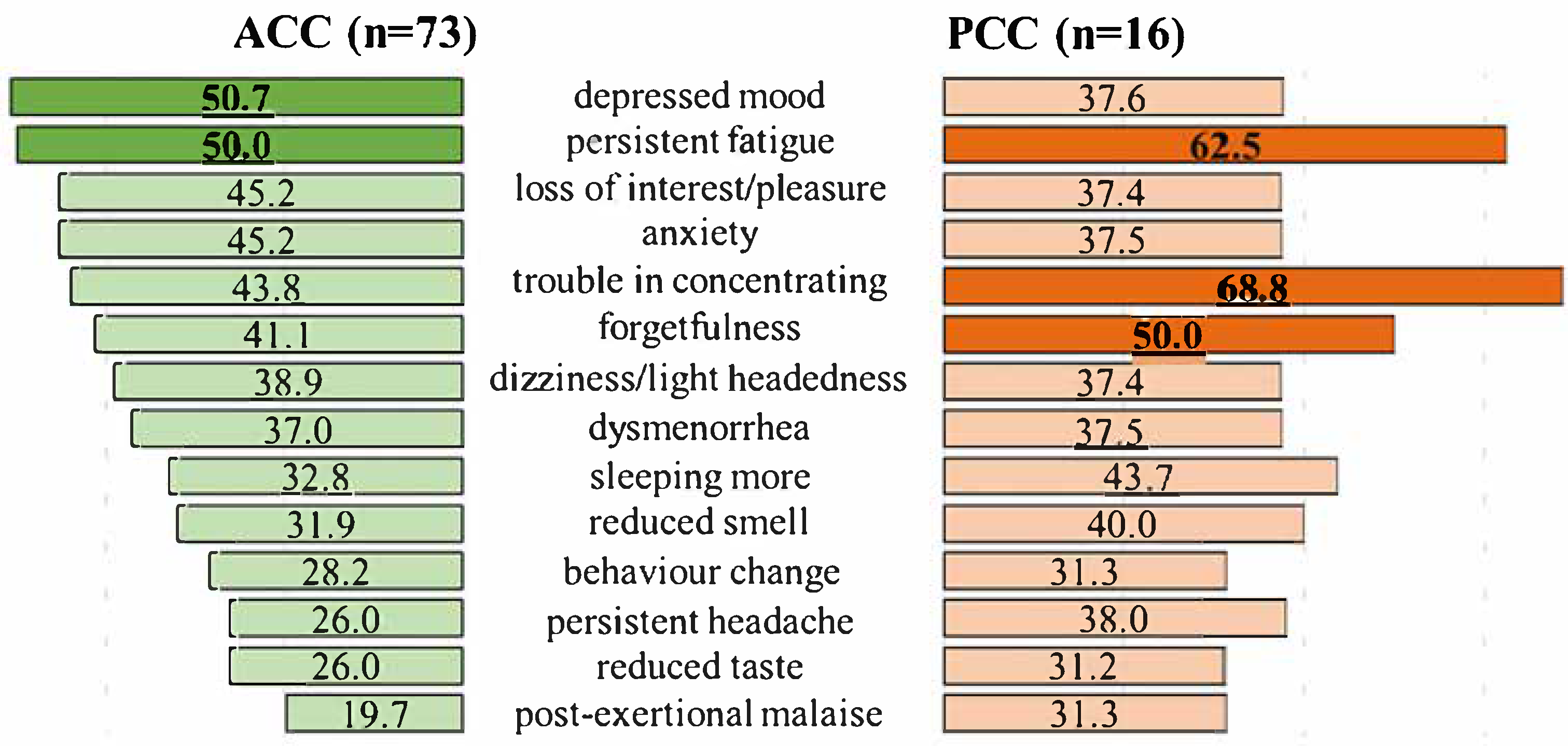
3.2. Symptoms in Acute COVID-19 (ACC) and Post COVID-19 Condition (PCC)
3.3. Results of the Assessment of Cognitive Functions
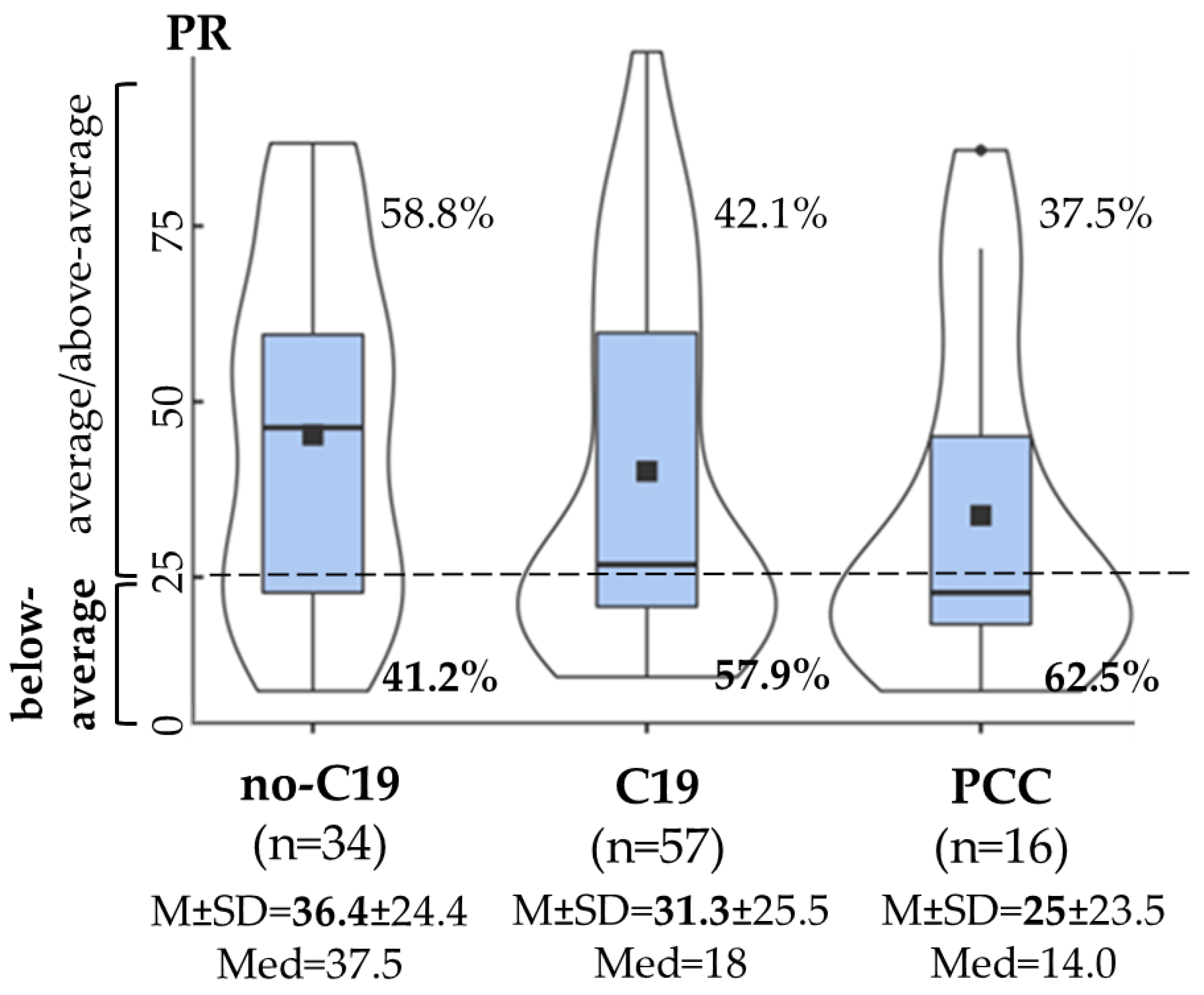
3.3.1. Attention
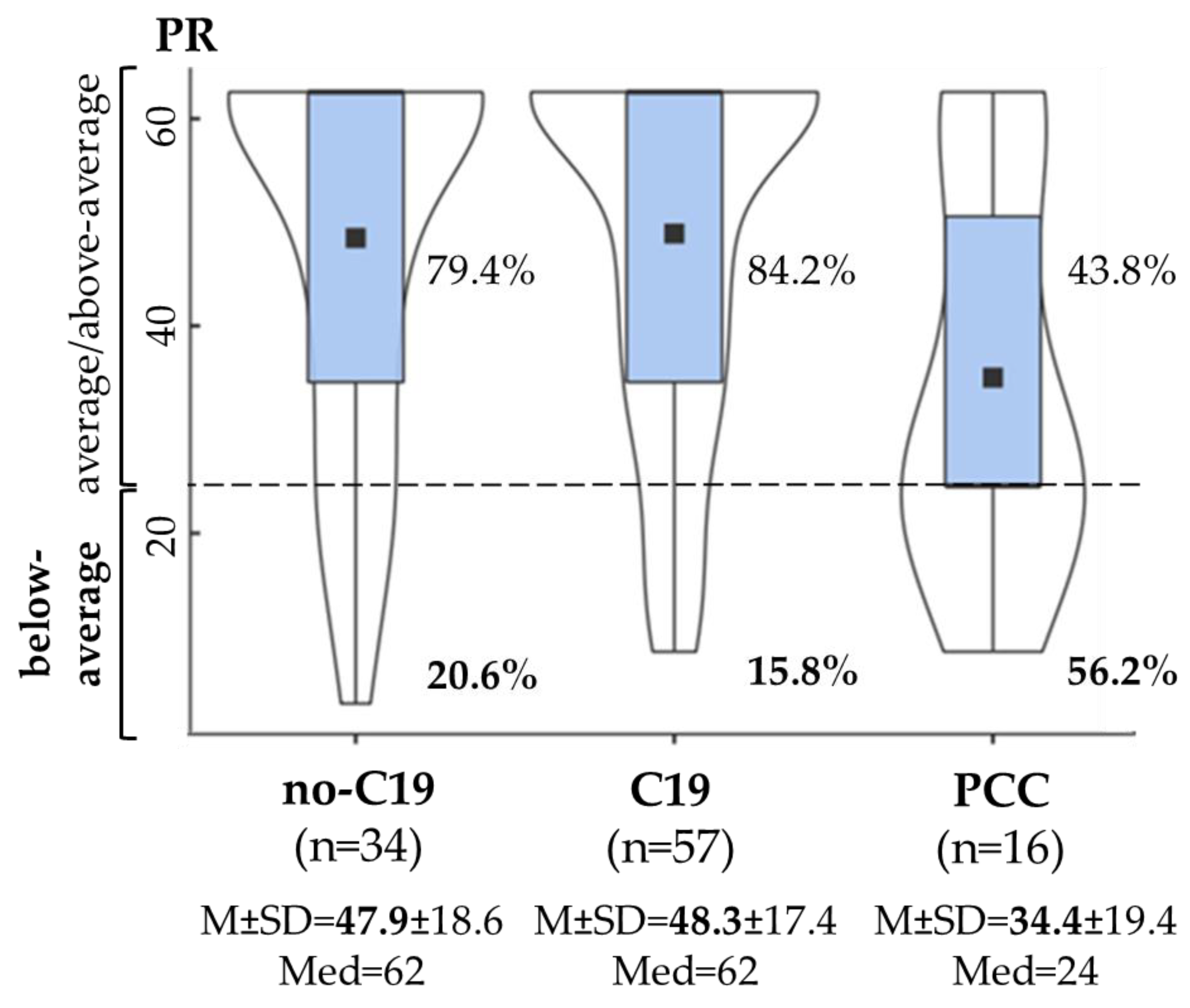
3.3.2. Executive Function
3.3.3. Co-Occurrence of Decreased Cognitive Functions
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 19 September 2023).
- Carfì, A.; Bernabei, R.; Landi, F.; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Amalakanti, S.; Arepalli, K.V.R.; Jillella, J.P. Cognitive Assessment in Asymptomatic COVID-19 Subjects. VirusDisease 2021, 32, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Chopra, V.; Flanders, S.A.; O’Malley, M.; Malani, A.N.; Prescott, H.C. Sixty-Day Outcomes Among Patients Hospitalized With COVID-19. Ann. Intern. Med. 2021, 174, 576–578. [Google Scholar] [CrossRef] [PubMed]
- Negrini, F.; Ferrario, I.; Mazziotti, D.; Berchicci, M.; Bonazzi, M.; de Sire, A.; Negrini, S.; Zapparoli, L. Neuropsychological Features of Severe Hospitalized Coronavirus Disease 2019 Patients at Clinical Stability and Clues for Postacute Rehabilitation. Arch. Phys. Med. Rehabil. 2021, 102, 155–158. [Google Scholar] [CrossRef]
- Whiteside, D.M.; Oleynick, V.; Holker, E.; Waldron, E.J.; Porter, J.; Kasprzak, M. Neurocognitive Deficits in Severe COVID-19 Infection: Case Series and Proposed Model. Clin. Neuropsychol. 2021, 35, 799–818. [Google Scholar] [CrossRef]
- Writing Committee for the COMEBAC Study Group; Morin, L.; Savale, L.; Pham, T.; Colle, R.; Figueiredo, S.; Harrois, A.; Gasnier, M.; Lecoq, A.L.; Meyrignac, O.; et al. Four-Month Clinical Status of a Cohort of Patients After Hospitalization for COVID-19. JAMA 2021, 325, 1525–1534. [Google Scholar] [CrossRef]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-Month Consequences of COVID-19 in Patients Discharged from Hospital: A Cohort Study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Soriano, J.B.; Murthy, S.; Marshall, J.C.; Relan, P.; Diaz, J.V.; WHO Clinical Case Definition Working Group on Post-COVID-19 Condition. A Clinical Case Definition of Post-COVID-19 Condition by a Delphi Consensus. Lancet Infect. Dis. 2022, 22, e102–e107. [Google Scholar] [CrossRef]
- Daugherty, S.E.; Guo, Y.; Heath, K.; Dasmariñas, M.C.; Jubilo, K.G.; Samranvedhya, J.; Lipsitch, M.; Cohen, K. Risk of Clinical Sequelae After the Acute Phase of SARS-CoV-2 Infection: Retrospective Cohort Study. BMJ 2021, 373, n1098. [Google Scholar] [CrossRef]
- Chen, C.; Haupert, S.R.; Zimmermann, L.; Shi, X.; Fritsche, L.G.; Mukherjee, B. Global Prevalence of Post-Coronavirus Disease 2019 (COVID-19) Condition or Long COVID: A Meta-Analysis and Systematic Review. J. Infect. Dis. 2022, 226, 1593–1607. [Google Scholar] [CrossRef]
- Cohen, K.; Ren, S.; Heath, K.; Dasmariñas, M.C.; Jubilo, K.G.; Guo, Y.; Lipsitch, M.; Daugherty, S.E. Risk of Persistent and New Clinical Sequelae Among Adults Aged 65 Years and Older During the Post-Acute Phase of SARS-CoV-2 Infection: Retrospective Cohort Study. BMJ 2022, 376, e068414. [Google Scholar] [CrossRef]
- Carod-Artal, F.J.; García-Moncó, J.C. Epidemiology, Pathophysiology, and Classification of the Neurological Symptoms of Post-COVID-19 Syndrome. Neurol. Perspect. 2021, 1, S5–S15. [Google Scholar] [CrossRef]
- Tenforde, M.W.; Billig Rose, E.; Lindsell, C.J.; Shapiro, N.I.; Files, D.C.; Gibbs, K.W.; Prekker, M.E.; Steingrub, J.S.; Smithline, H.A.; Gong, M.N.; et al. CDC COVID-19 Response Team. Characteristics of Adult Outpatients and Inpatients With COVID-19-11 Academic Medical Centers, United States, March–May 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Logue, J.K.; Franko, N.M.; McCulloch, D.J.; McDonald, D.; Magedson, A.; Wolf, C.R.; Chu, H.Y. Sequelae in Adults at 6 Months After COVID-19 Infection. JAMA Netw. Open 2021, 4, e210830. [Google Scholar] [CrossRef] [PubMed]
- Taquet, M.; Geddes, J.R.; Husain, M.; Luciano, S.; Harrison, P.J. 6-Month Neurological and Psychiatric Outcomes in 236,379 Survivors of COVID-19: A Retrospective Cohort Study Using Electronic Health Records. Lancet Psychiatry 2021, 8, 416–427. [Google Scholar] [CrossRef] [PubMed]
- Ekström, S.; Mogensen, I.; Ödling, M.; Georgelis, A.; Merritt, A.S.; Björkander, S.; Melén, E.; Bergström, A.; Kull, I. Post COVID-19 among young adults- prevalence and associations with general health, stress, and lifestyle factors. BMC Public Health 2025, 25, 1330. [Google Scholar] [CrossRef]
- Mogensen, I.; Ekström, S.; Hallberg, J.; Georgelis, A.; Melén, E.; Bergström, A.; Kull, I. Post COVID-19 symptoms are common, also among young adults in the general population. Sci. Rep. 2023, 13, 11300. [Google Scholar] [CrossRef]
- Rank, A.; Tzortzini, A.; Kling, E.; Schmid, C.; Claus, R.; Löll, E.; Burger, R.; Römmele, C.; Dhillon, C.; Müller, K.; et al. One Year After Mild COVID-19: The Majority of Patients Maintain Specific Immunity, But One in Four Still Suffer from Long-Term Symptoms. J. Clin. Med. 2021, 10, 3305. [Google Scholar] [CrossRef]
- Kim, Y.; Bitna-Ha; Kim, S.W.; Chang, H.H.; Kwon, K.T.; Bae, S.; Hwang, S. Post-Acute COVID-19 Syndrome in Patients After 12 Months From COVID-19 Infection in Korea. BMC Infect. Dis. 2022, 22, 93. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, M.; Penfold, R.S.; Merino, J.; Sudre, C.H.; Molteni, E.; Berry, S.; Canas, L.S.; Graham, M.S.; Klaser, K.; Modat, M.; et al. Risk Factors and Disease Profile of Post-Vaccination SARS-CoV-2 Infection in UK Users of the COVID Symptom Study App: A Prospective, Community-Based, Nested, Case-Control Study. Lancet Infect. Dis. 2022, 22, 43–55. [Google Scholar] [CrossRef]
- Notarte, K.I.; Catahay, J.A.; Velasco, J.V.; Pastrana, A.; Ver, A.T.; Pangilinan, F.C.; Peligro, P.J.; Casimiro, M.; Guerrero, J.J.; Gellaco, M.M.L.; et al. Impact of COVID-19 Vaccination on the Risk of Developing Long-COVID and on Existing Long-COVID Symptoms: A Systematic Review. EClinicalMedicine 2022, 53, 101624. [Google Scholar] [CrossRef]
- Tsampasian, V.; Elghazaly, H.; Chattopadhyay, R.; Debski, M.; Naing, T.K.P.; Garg, P.; Clark, A.; Ntatsaki, E.; Vassiliou, V.S. Risk Factors Associated With Post-COVID-19 Condition: A Systematic Review and Meta-Analysis. JAMA Intern. Med. 2023, 183, 566–580. [Google Scholar] [CrossRef]
- Marshall, M. The Lasting Misery of Coronavirus Long-Haulers. Nature 2020, 585, 339–341. [Google Scholar] [CrossRef] [PubMed]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing Long COVID in an International Cohort: 7 Months of Symptoms and Their Impact. EClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef] [PubMed]
- Hampshire, A.; Trender, W.; Chamberlain, S.R.; Jolly, A.E.; Grant, J.E.; Patrick, F.; Mazibuko, N.; Williams, S.C.; Barnby, J.M.; Hellyer, P.; et al. Cognitive Deficits in People Who Have Recovered From COVID-19. EClinicalMedicine 2021, 39, 101044. [Google Scholar] [CrossRef] [PubMed]
- Seeßle, J.; Waterboer, T.; Hippchen, T.; Simon, J.; Kirchner, M.; Lim, A.; Müller, B.; Merle, U. Persistent Symptoms in Adult Patients 1 Year After Coronavirus Disease 2019 (COVID-19): A Prospective Cohort Study. Clin. Infect. Dis. 2022, 74, 1191–1198. [Google Scholar] [CrossRef]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and Predictors of Long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef]
- Ceban, F.; Ling, S.; Lui, L.M.W.; Lee, Y.; Gill, H.; Teopiz, K.M.; Rodrigues, N.B.; Subramaniapillai, M.; Di Vincenzo, J.D.; Cao, B.; et al. Fatigue and Cognitive Impairment in Post-COVID-19 Syndrome: A Systematic Review and Meta-Analysis. Brain Behav. Immun. 2022, 101, 93–135. [Google Scholar] [CrossRef]
- Guo, P.; Benito Ballesteros, A.; Yeung, S.P.; Liu, R.; Saha, A.; Curtis, L.; Kaser, M.; Haggard, M.P.; Cheke, L.G. COVCOG 2: Cognitive and Memory Deficits in Long COVID: A Second Publication From the COVID and Cognition Study. Front. Aging Neurosci. 2022, 14, 804937. [Google Scholar] [CrossRef]
- Kelly, K.M.; Anghinah, R.; Kullmann, A.; Ashmore, R.C.; Synowiec, A.S.; Gibson, L.C.; Manfrinati, L.; de Araújo, A.; Spera, R.R.; Braverman, A.; et al. Oculomotor, Vestibular, Reaction Time, and Cognitive Tests as Objective Measures of Neural Deficits in Patients Post COVID-19 Infection. Front. Neurol. 2022, 13, 919596. [Google Scholar] [CrossRef]
- Ziauddeen, N.; Gurdasani, D.; O’Hara, M.E.; Hastie, C.; Roderick, P.; Yao, G.; Alwan, N.A. Characteristics and Impact of Long COVID: Findings From an Online Survey. PLoS ONE 2022, 17, e0264331. [Google Scholar] [CrossRef]
- Ding, H.; Yin, S.; Cheng, Y.; Cai, Y.; Huang, W.; Deng, W. Neurologic Manifestations of Nonhospitalized Patients With COVID-19 in Wuhan, China. MedComm 2020, 1, 253–256. [Google Scholar] [CrossRef]
- Boesl, F.; Audebert, H.; Endres, M.; Prüss, H.; Franke, C. A Neurological Outpatient Clinic for Patients With Post-COVID-19 Syndrome—A Report on the Clinical Presentations of the First 100 Patients. Front. Neurol. 2021, 12, 738405. [Google Scholar] [CrossRef] [PubMed]
- Daroische, R.; Hemminghyth, M.S.; Eilertsen, T.H.; Breitve, M.H.; Chwiszczuk, L.J. Cognitive Impairment After COVID-19—A Review on Objective Test Data. Front. Neurol. 2021, 12, 699582. [Google Scholar] [CrossRef]
- Del Brutto, O.H.; Wu, S.; Mera, R.M.; Costa, A.F.; Recalde, B.Y.; Issa, N.P. Cognitive Decline Among Individuals With History of Mild Symptomatic SARS-CoV-2 Infection: A Longitudinal Prospective Study Nested to a Population Cohort. Eur. J. Neurol. 2021, 28, 3245–3253. [Google Scholar] [CrossRef] [PubMed]
- Tavares-Júnior, J.W.L.; de Souza, A.C.C.; Borges, J.W.P.; Oliveira, D.N.; Siqueira-Neto, J.I.; Sobreira-Neto, M.A.; Braga-Neto, P. COVID-19 Associated Cognitive Impairment: A Systematic Review. Cortex 2022, 152, 77–97. [Google Scholar] [CrossRef] [PubMed]
- Crivelli, L.; Palmer, K.; Calandri, I.; Guekht, A.; Beghi, E.; Carroll, W.; Frontera, J.; García-Azorín, D.; Westenberg, E.; Winkler, A.S.; et al. Changes in Cognitive Functioning After COVID-19: A Systematic Review and Meta-Analysis. Alzheimer’s Dement. 2022, 18, 1047–1066. [Google Scholar] [CrossRef]
- Vakani, K.; Ratto, M.; Sandford-James, A.; Antonova, E.; Kumari, V. COVID-19 and Cognitive Function: Evidence for Increased Processing Speed Variability in COVID-19 Survivors and Multifaceted Impairment With Long-COVID Symptoms. Eur. Psychiatry 2023, 66, e43. [Google Scholar] [CrossRef]
- Ariza, M.; Cano, N.; Segura, B.; Adan, A.; Bargalló, N.; Caldú, X.; Campabadal, A.; Jurado, M.A.; Mataró, M.; Pueyo, R.; et al. Neuropsychological Impairment in Post-COVID Condition Individuals With and Without Cognitive Complaints. Front. Aging Neurosci. 2022, 14, 1029842. [Google Scholar] [CrossRef]
- Aschenbrenner, S.; Kaiser, S.; Pfüller, U.; Roesch-Ely, D.; Weisbrod, M. COGBAT—Cognitive Basic Assessment. Schuhfried®, Mödling. 2012. Available online: https://marketplace.schuhfried.com/en/ (accessed on 23 June 2022).
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Woo, M.S.; Malsy, J.; Pöttgen, J.; Seddiq Zai, S.; Ufer, F.; Hadjilaou, A.; Schmiedel, S.; Addo, M.M.; Gerloff, C.; Heesen, C.; et al. Frequent Neurocognitive Deficits After Recovery From Mild COVID-19. Brain Commun. 2020, 2, fcaa205. [Google Scholar] [CrossRef]
- Graham, E.L.; Clark, J.R.; Orban, Z.S.; Lim, P.H.; Szymanski, A.L.; Taylor, C.; DiBiase, R.M.; Jia, D.T.; Balabanov, R.; Ho, S.U.; et al. Persistent Neurologic Symptoms and Cognitive Dysfunction in Non-Hospitalized COVID-19 “Long Haulers”. Ann. Clin. Transl. Neurol. 2021, 8, 1073–1085. [Google Scholar] [CrossRef]
- Hosp, J.A.; Dressing, A.; Blazhenets, G.; Bormann, T.; Rau, A.; Schwabenland, M.; Thurow, J.; Wagner, D.; Waller, C.; Niesen, W.D.; et al. Cognitive Impairment and Altered Cerebral Glucose Metabolism in the Subacute Stage of COVID-19. Brain 2021, 144, 1263–1276. [Google Scholar] [CrossRef]
- Miskowiak, K.W.; Johnsen, S.; Sattler, S.M.; Nielsen, S.; Kunalan, K.; Rungby, J.; Lapperre, T.; Porsberg, C.M. Cognitive Impairments Four Months After COVID-19 Hospital Discharge: Pattern, Severity and Association With Illness Variables. Eur. Neuropsychopharmacol. 2021, 46, 39–48. [Google Scholar] [CrossRef]
- Ortelli, P.; Ferrazzoli, D.; Sebastianelli, L.; Engl, M.; Romanello, R.; Nardone, R.; Bonini, I.; Koch, G.; Saltuari, L.; Quartarone, A.; et al. Neuropsychological and Neurophysiological Correlates of Fatigue in Post-Acute Patients With Neurological Manifestations of COVID-19: Insights Into a Challenging Symptom. J. Neurol. Sci. 2021, 420, 117271. [Google Scholar] [CrossRef] [PubMed]
- Ferrucci, R.; Dini, M.; Groppo, E.; Rosci, C.; Reitano, M.R.; Bai, F.; Poletti, B.; Brugnera, A.; Silani, V.; D’Arminio Monforte, A.; et al. Long-Lasting Cognitive Abnormalities After COVID-19. Brain Sci. 2021, 11, 235. [Google Scholar] [CrossRef]
- Mattioli, F.; Stampatori, C.; Righetti, F.; Sala, E.; Tomasi, C.; De Palma, G. Neurological and Cognitive Sequelae of COVID-19: A Four Month Follow-Up. J. Neurol. 2021, 268, 4422–4428. [Google Scholar] [CrossRef] [PubMed]
- Mazza, M.G.; Palladini, M.; De Lorenzo, R.; Magnaghi, C.; Poletti, S.; Furlan, R.; Ciceri, F.; COVID-19 BioB Outpatient Clinic Study Group; Rovere-Querini, P.; Benedetti, F. Persistent Psychopathology and Neurocognitive Impairment in COVID-19 Survivors: Effect of Inflammatory Biomarkers at Three-Month Follow-Up. Brain Behav. Immun. 2021, 94, 138–147. [Google Scholar] [CrossRef]
- Zhao, S.; Martin, E.M.; Reuken, P.A.; Scholcz, A.; Ganse-Dumrath, A.; Srowig, A.; Utech, I.; Kozik, V.; Radscheidt, M.; Brodoehl, S.; et al. Long COVID Is Associated With Severe Cognitive Slowing: A Multicentre Cross-Sectional Study. EClinicalMedicine 2024, 68, 102434. [Google Scholar] [CrossRef]
- Baseler, H.A.; Aksoy, M.; Salawu, A.; Green, A.; Asghar, A.U.R. The Negative Impact of COVID-19 on Working Memory Revealed Using a Rapid Online Quiz. PLoS ONE 2022, 17, e0269353. [Google Scholar] [CrossRef] [PubMed]
- Bertuccelli, M.; Ciringione, L.; Rubega, M.; Bisiacchi, P.; Masiero, S.; Del Felice, A. Cognitive Impairment in People with Previous COVID-19 Infection: A Scoping Review. Cortex 2022, 154, 212–230. [Google Scholar] [CrossRef]
- Baddeley, A. Working Memory: Looking Back and Looking Forward. Nat. Rev. Neurosci. 2003, 4, 829–839. [Google Scholar] [CrossRef]
- Jonides, J.; Lewis, R.L.; Nee, D.E.; Lustig, C.A.; Berman, M.G.; Moore, K.S. The Mind and Brain of Short-Term Memory. Annu. Rev. Psychol. 2008, 59, 193–224. [Google Scholar] [CrossRef]
- Owen, A.M.; McMillan, K.M.; Laird, A.R.; Bullmore, E. N-Back Working Memory Paradigm: A Meta-Analysis of Normative Functional Neuroimaging Studies. Hum. Brain Mapp. 2005, 25, 46–59. [Google Scholar] [CrossRef] [PubMed]
- Kane, M.J.; Conway, A.R.A.; Miura, T.K.; Colflesh, G.J.H. Working Memory, Attention Control, and the N-Back Task: A Question of Construct Validity. J. Exp. Psychol. Learn. Mem. Cogn. 2007, 33, 615–622. [Google Scholar] [CrossRef]
- Saucier, J.; Jose, C.; Beroual, Z.; Al-Qadi, M.; Chartrand, S.; Libert, E.; Losier, M.C.; Cooling, K.; Girouard, G.; Jbilou, J.; et al. Cognitive Inhibition Deficit in Long COVID-19: An Exploratory Study. Front. Neurol. 2023, 14, 1125574. [Google Scholar] [CrossRef]
- García-Sánchez, C.; Calabria, M.; Grunden, N.; Pons, C.; Arroyo, J.A.; Gómez-Anson, B.; Lleó, A.; Alcolea, D.; Belvís, R.; Morollón, N.; et al. Neuropsychological Deficits in Patients with Cognitive Complaints After COVID-19. Brain Behav. 2022, 12, e2508. [Google Scholar] [CrossRef] [PubMed]
- Bland, A.R.; Barraclough, M.; Trender, W.R.; Mehta, M.A.; Hellyer, P.J.; Hampshire, A.; Penner, I.K.; Elliott, R.; Harenwall, S. Profiles of Objective and Subjective Cognitive Function in Post-COVID Syndrome, COVID-19 Recovered, and COVID-19 Naïve Individuals. Sci. Rep. 2024, 14, 13368. [Google Scholar] [CrossRef]
- Hartung, T.J.; Neumann, C.; Bahmer, T.; Chaplinskaya-Sobol, I.; Endres, M.; Geritz, J.; Haeusler, K.G.; Heuschmann, P.U.; Hildesheim, H.; Hinz, A.; et al. Fatigue and Cognitive Impairment After COVID-19: A Prospective Multicentre Study. EClinicalMedicine 2022, 53, 101651. [Google Scholar] [CrossRef]
- Hartung, T.J.; Bahmer, T.; Chaplinskaya-Sobol, I.; Deckert, J.; Endres, M.; Franzpötter, K.; Geritz, J.; Haeusler, K.G.; Hein, G.; Heuschmann, P.U.; et al. NAPKON Study Group. Predictors of Non-Recovery From Fatigue and Cognitive Deficits After COVID-19: A Prospective, Longitudinal, Population-Based Study. EClinicalMedicine 2024, 69, 102456. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Sun, S.; Xiao, S.; Chen, G.; Chen, P.; Yang, Z.; Tang, X.; Huang, L.; Wang, Y. COVID-19 is associated with changes in brain function and structure: A multimodal meta-analysis of neuroimaging studies. Neurosci. Biobehav. Rev. 2024, 164, 105792. [Google Scholar] [CrossRef] [PubMed]
- Benito-León, J.; Lapeña, J.; García-Vasco, L.; Cuevas, C.; Viloria-Porto, J.; Calvo-Córdoba, A.; Arrieta-Ortubay, E.; Ruiz-Ruigómez, M.; Sánchez-Sánchez, C.; García-Cena, C. Exploring Cognitive Dysfunction in Long COVID Patients: Eye Movement Abnormalities and Frontal-Subcortical Circuits Implications via Eye-Tracking and Machine Learning. Am. J. Med. 2025, 138, 550–559. [Google Scholar] [CrossRef]
- Lin, K.; Gao, Y.; Ji, W.; Li, Y.; Wang, W.; Du, M.; Liu, J.; Hong, Z.; Jiang, T.; Wang, Y. Attentional Impairment and Altered Brain Activity in Healthcare Workers After Mild COVID-19. Brain Imaging Behav. 2024, 18, 566–575. [Google Scholar] [CrossRef] [PubMed]
- Scardua-Silva, L.; Amorim da Costa, B.; Karmann Aventurato, Í.; Batista Joao, R.; Machado de Campos, B.; Rabelo de Brito, M.; Bechelli, J.F.; Santos Silva, L.C.; Ferreira Dos Santos, A.; Koutsodontis Machado Alvim, M.; et al. Microstructural Brain Abnormalities, Fatigue, and Cognitive Dysfunction After Mild COVID-19. Sci. Rep. 2024, 14, 1758. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takács, J.; Deák, D.; Seregély, B.; Koller, A. Cognitive Slowing, Dysfunction in Verbal Working Memory, Divided Attention and Response Inhibition in Post COVID-19 Condition in Young Adults. Life 2025, 15, 821. https://doi.org/10.3390/life15050821
Takács J, Deák D, Seregély B, Koller A. Cognitive Slowing, Dysfunction in Verbal Working Memory, Divided Attention and Response Inhibition in Post COVID-19 Condition in Young Adults. Life. 2025; 15(5):821. https://doi.org/10.3390/life15050821
Chicago/Turabian StyleTakács, Johanna, Darina Deák, Beáta Seregély, and Akos Koller. 2025. "Cognitive Slowing, Dysfunction in Verbal Working Memory, Divided Attention and Response Inhibition in Post COVID-19 Condition in Young Adults" Life 15, no. 5: 821. https://doi.org/10.3390/life15050821
APA StyleTakács, J., Deák, D., Seregély, B., & Koller, A. (2025). Cognitive Slowing, Dysfunction in Verbal Working Memory, Divided Attention and Response Inhibition in Post COVID-19 Condition in Young Adults. Life, 15(5), 821. https://doi.org/10.3390/life15050821





