An Advanced Pneumatic Compression Therapy System Improves Leg Volume and Fluid, Adipose Tissue Thickness, Symptoms, and Quality of Life and Reduces Risk of Lymphedema in Women with Lipedema
Abstract
1. Introduction
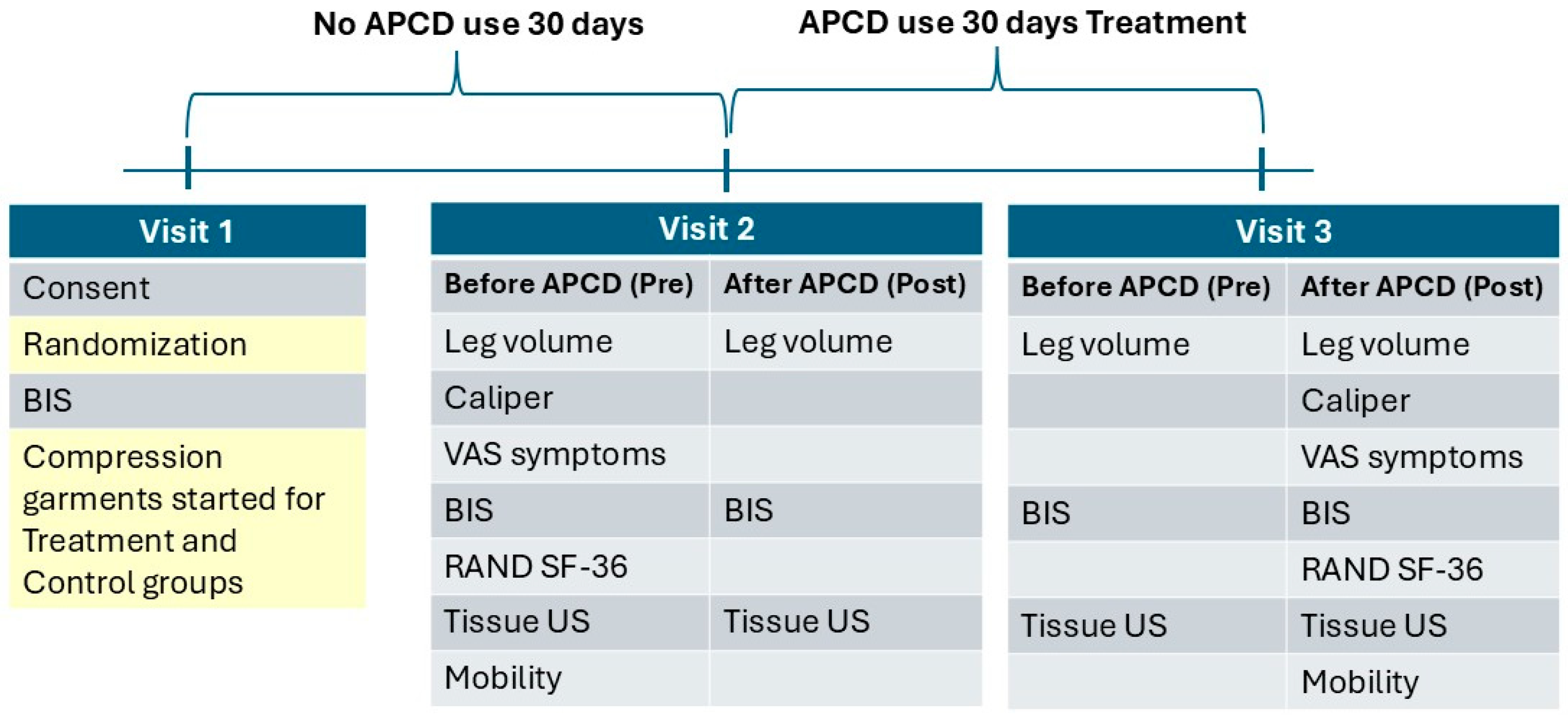
2. Materials and Methods
- Inclusion criteria:
- Ambulatory females, age 18–70 years.
- Stage 2–3, Type II–III lipedema.
- Pain score with or without pressure in any lipedema area of 3 or more on an 11-point Likert visual analog scale.
- Able to maintain a consistent eating plan and exercise regimen for the 60-day study with weight stability (within 4.5 kg or usual weight fluctuation per patient) over three months.
- Willing to wear compression garments during the study.
- Agreement to wash off manual therapy of any kind including massage, physical therapy, occupational therapy, instrument-assisted soft tissue therapy, or other deep tissue therapy and decongestive therapy methods (manual lymph drainage, pneumatic compression use, and compression garments other than the ones provided) over 30 days prior to Visit 2.
- Exclusion criteria:
- Inability to understand the purpose of the study and complete consent.
- Bed bound, preventing assessment of activities of daily living.
- Contraindications to APCD use:
- (a)
- Serious arterial insufficiency measured as a monophasic pulse wave using Doppler (Terason uSmart 3300-15L4 uSmart Linear Array Transducer; Burlington, MA, USA) without arterial disease.
- (b)
- Edema due to decompensated congestive heart failure (CHF), based on history or physical examination.
- (c)
- Active phlebitis, based on physical examination.
- (d)
- Active deep vein thrombosis, based on history or physical examination.
- (e)
- Localized wound infection, based on physical examination.
- (f)
- Cellulitis, based on history or physical examination.
- Positive Stemmer sign on the feet.
- Lymphedema with minimal to no lipedema.
- eight > 170 kg due to weight restriction on bioimpedance spectroscopy device.
- Undergoing surgery during the time of the study.
- Weight loss surgery within the past 18 months.
- Use of diuretic medication.
- Participation in other research at the time of the study.
- Use of immunosuppressant medications including Gleevec, diosmin, methotrexate, corticosteroids, Plaquenil, or other.
- Medical illness deemed significant by the principal investigator.
- Waist to hip ratio > 0.85 suggestive of obesity with lipedema.
- Tape measurement: At V2 and V3, with the back of the leg against a measuring grid. Measurements began at the ankle around the malleoli at 10 cm and continued every 10 cm to the upper thigh (70 cm maximum) with, on average, seven measurements total for the lower and upper leg. The volume of the leg was estimated using the formula for the volume of the frustum of a cone [29]. While consistent measurement by the same research staff at each visit is important, due to staff schedules, subjects were measured by different staff at each visit.
- 3D imaging: Leg volume was measured at V2 and V3 using a 3D imaging system (LymphaTech, Atlanta, GA, USA) [30]. Regarding measurement time, pre was before and post was after treatment (treatment group) or no treatment (control group). The volume of the leg was estimated using the formula for the volume of the frustum of a cone [31].
3. Results
3.1. Compliance
3.2. Demographics
3.3. Quantitative Measures
3.3.1. Leg Volume
Tape Measure
Three-Dimensional Leg Imaging
Weight
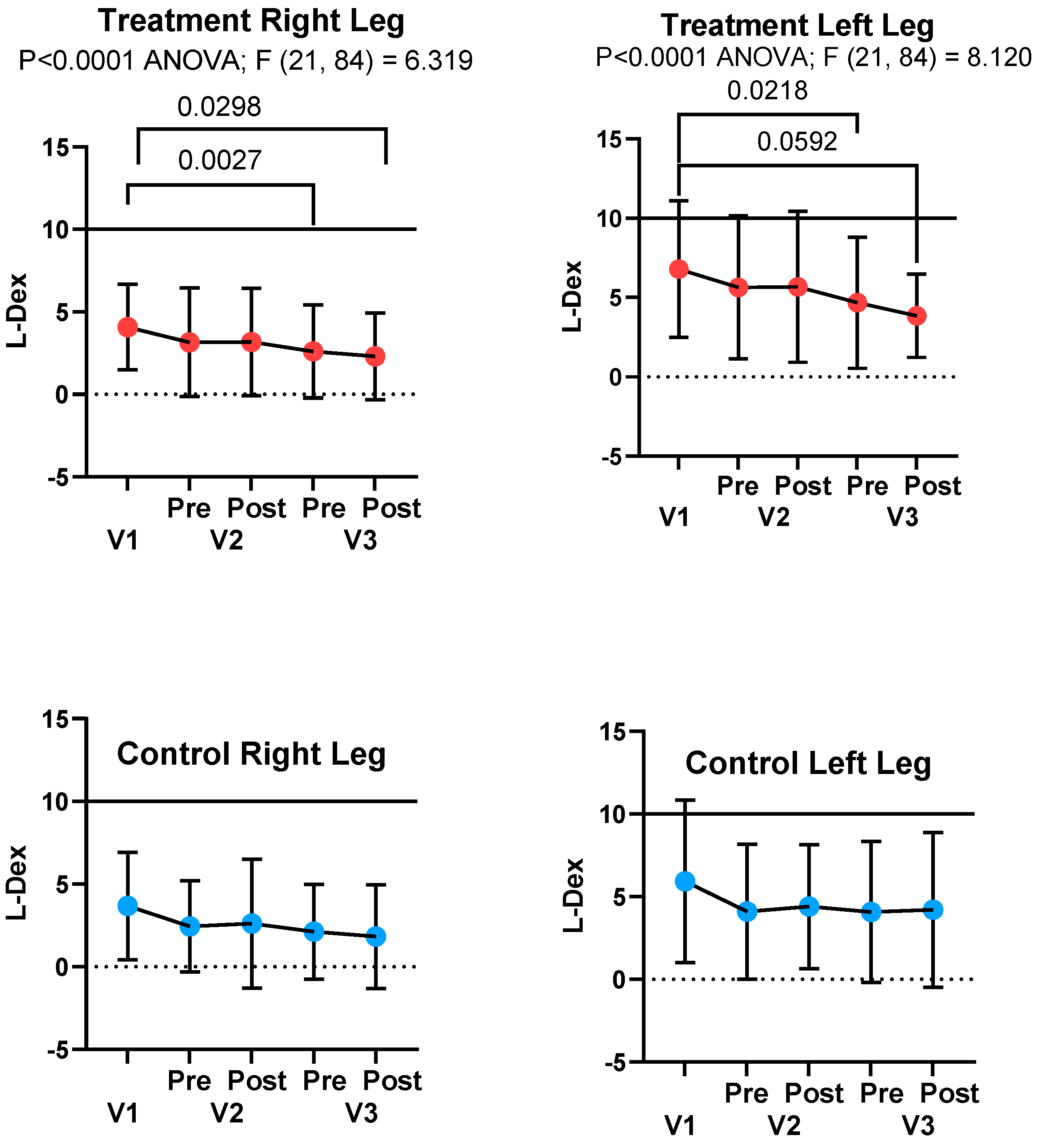
3.3.2. Bioimpedance Spectroscopy
L-Dex Score
Total Body Water
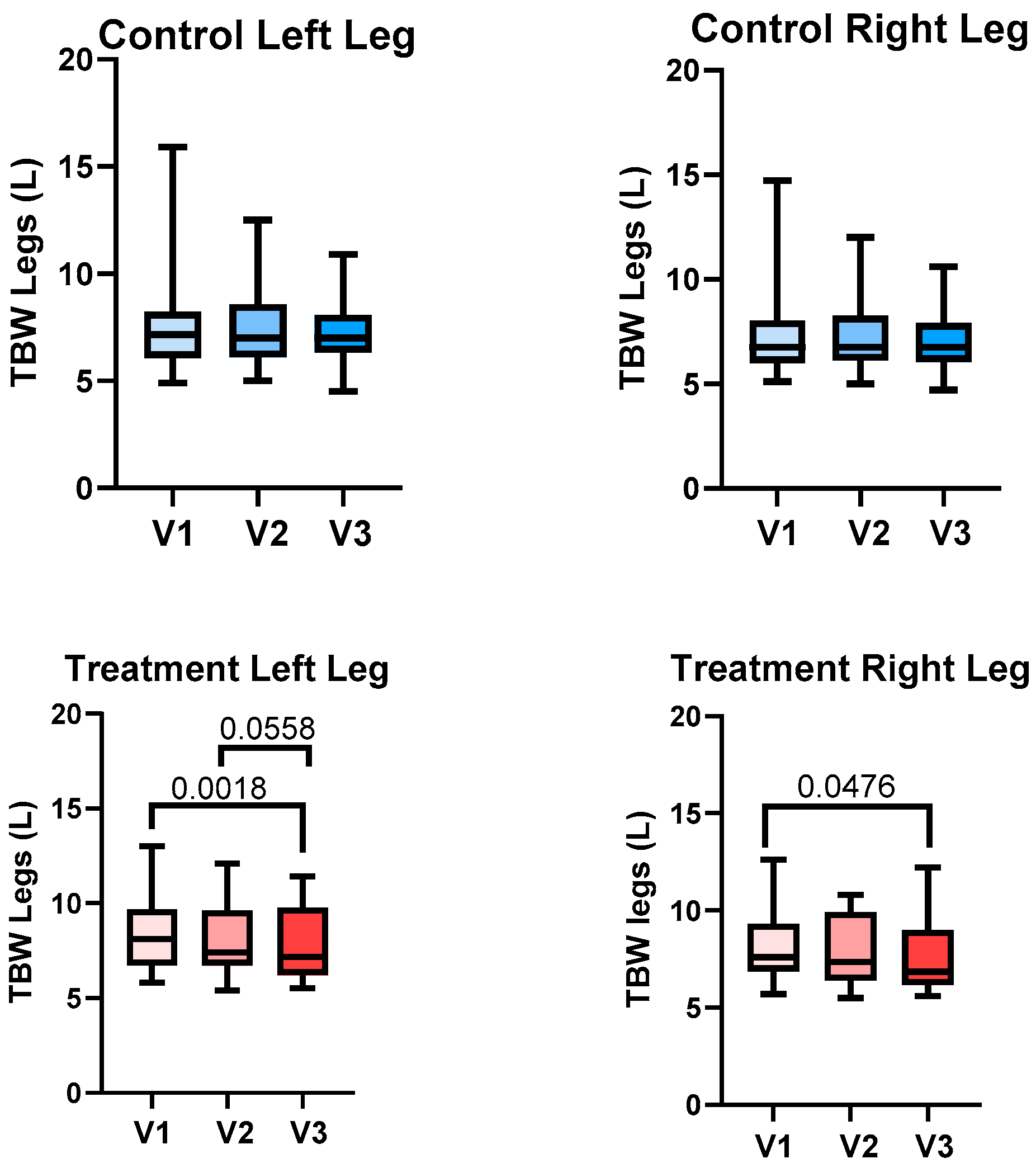
Total Body Water of the Legs
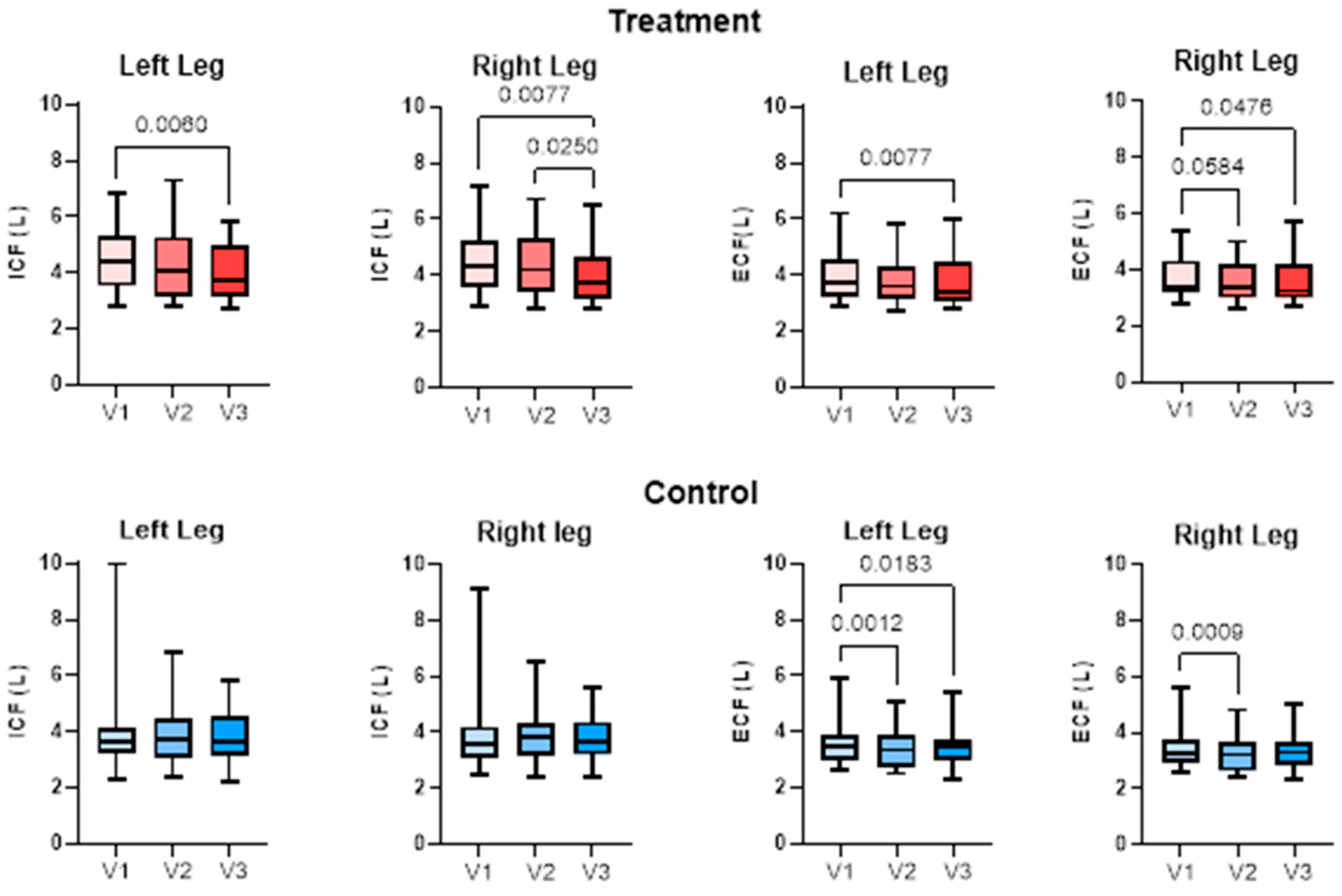
Extracellular and Intracellular Fluid
3.3.3. Caliper
3.3.4. Timed Up and Go
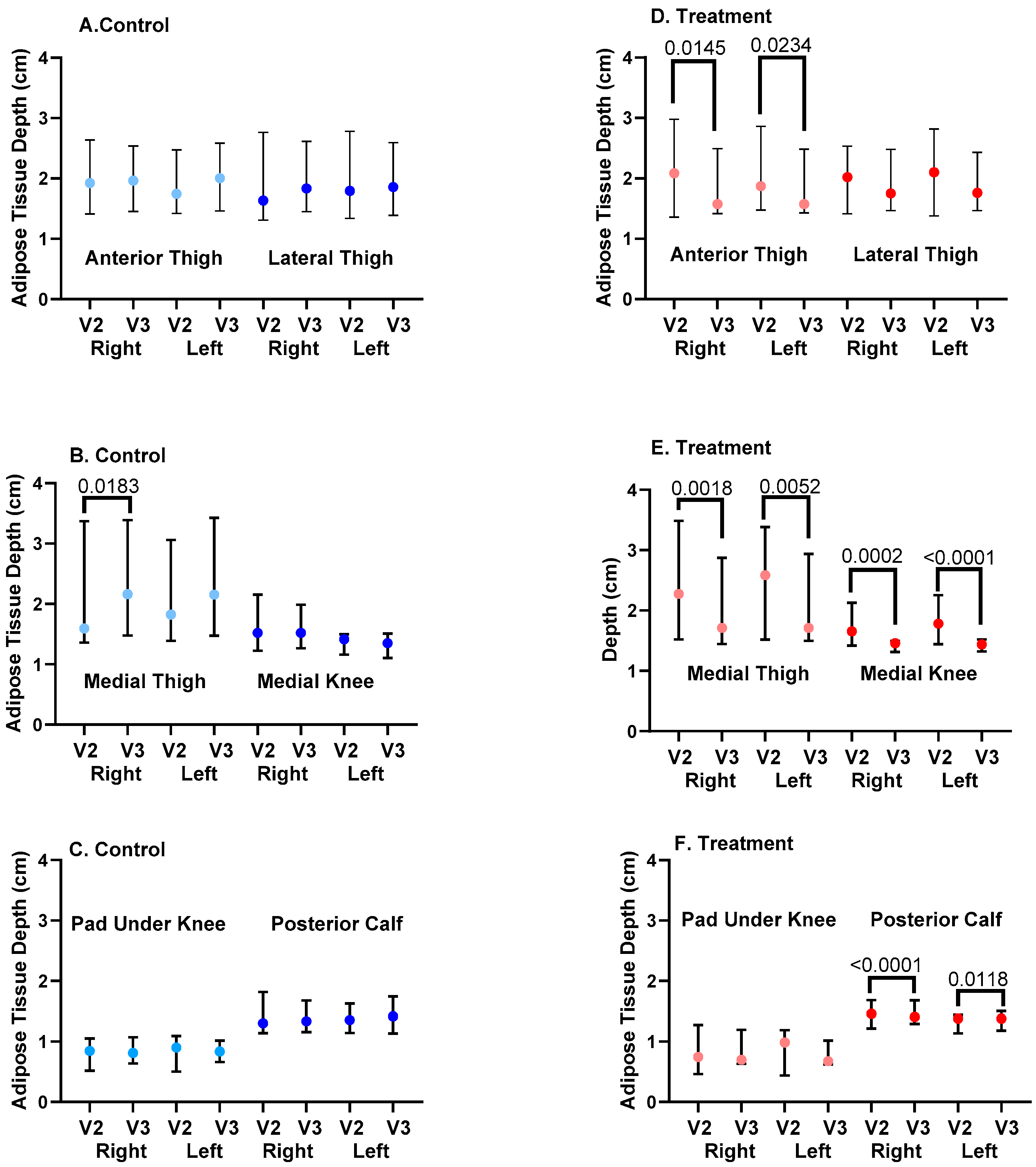
3.3.5. Ultrasound Depth of SAT
Chronic Change in SAT Depth
Acute Changes in SAT Depth
3.4. Qualitative Measures
3.4.1. Visual Analog Scales
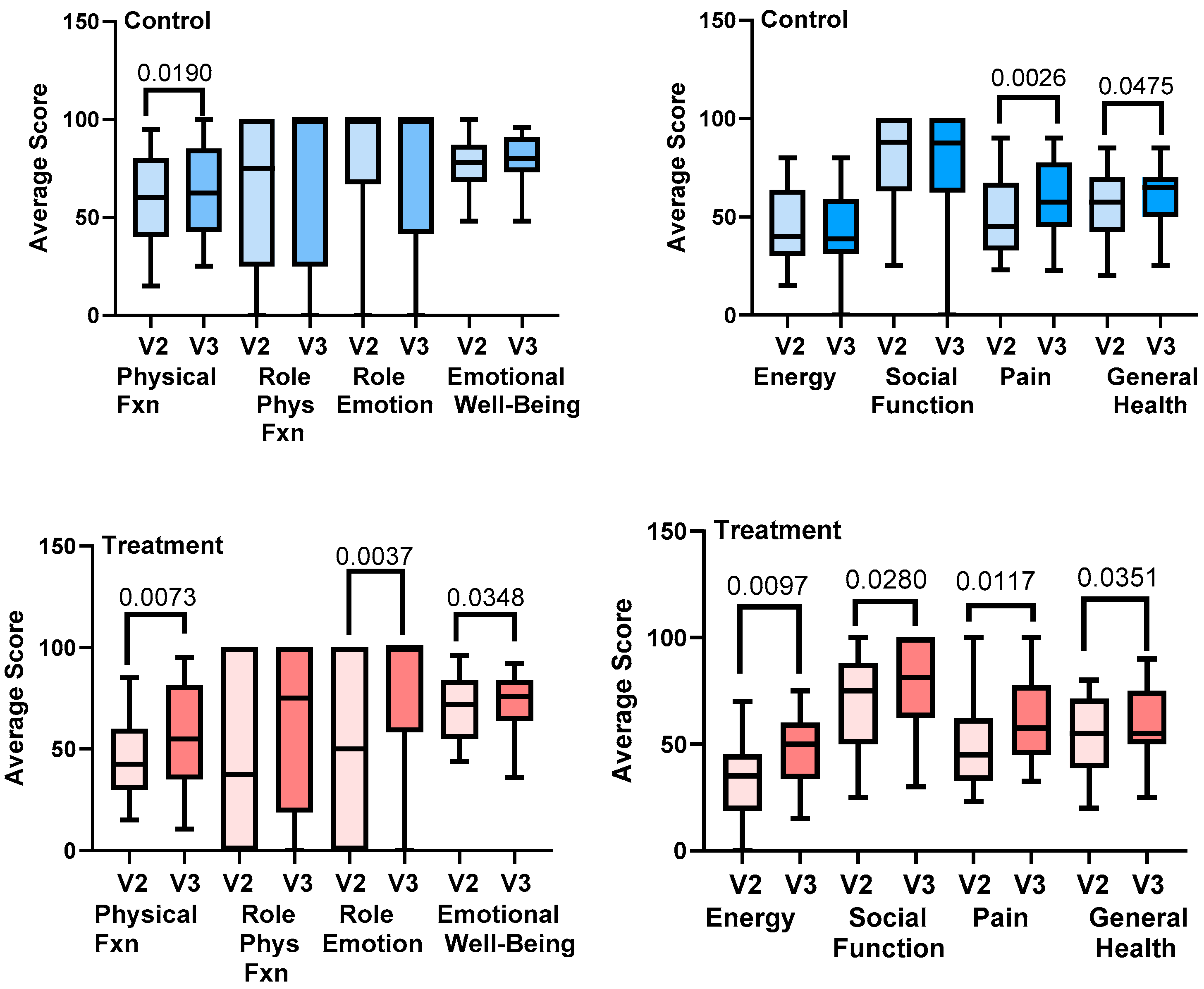
3.4.2. RAND-SF-36
3.4.3. LEFS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| APCD | Intermittent pneumatic compression device |
| BIS | Bioimpedance spectroscopy |
| BMI | Body mass index |
| COPD | Chronic obstructive pulmonary disease |
| CVD | Cardiovascular disease |
| CVI | Chronic venous insufficiency |
| ECF | Extracellular fluid |
| ICF | Intracellular fluid |
| ICG | Indocyanine green |
| HTN | Hypertension |
| MCAS | Mast cell activation syndrome |
| NS | Non-significant |
| PCOS | Polycystic ovarian syndrome |
| POTS | Postural orthostatic tachycardia syndrome |
| SAT | Subcutaneous adipose tissue |
| SF-36 | RAND Short Form 36-Item Survey |
| US | Ultrasound |
| VAS | Visual analog scales |
| WHR | Waist-to-hip ratio |
| WHtR | Waist-to-height ratio |
References
- Jagtman, B.A.; Kuiper, J.P.; Brakkee, A.J. Measurements of skin elasticity in patients with lipedema of the Moncorps “rusticanus” type. Phlebologie 1984, 37, 315–319. [Google Scholar] [PubMed]
- Herbst, K.L.; Kahn, L.A.; Iker, E.; Ehrlich, C.; Wright, T.; McHutchison, L.; Schwartz, J.; Sleigh, M.; Donahue, P.M.; Lisson, K.H.; et al. Standard of care for lipedema in the United States. Phlebology 2021, 36, 779–796. [Google Scholar] [CrossRef] [PubMed]
- Herbst, K.; Mirkovskaya, L.; Bharhagava, A.; Chava, Y.; Te, C.H. Lipedema Fat and Signs and Symptoms of Illness, Increase with Advancing Stage. Arch. Med. 2015, 7, 1–8. [Google Scholar]
- Wright, T.; Babula, M.; Schwartz, J.; Wright, C.; Danesh, N.; Herbst, K. Lipedema Reduction Surgery Improves Pain, Mobility, Physical Function, and Quality of Life: Case Series Report. Plast. Reconstr. Surg. Glob. Open 2023, 11, e5436. [Google Scholar] [CrossRef] [PubMed]
- Bast, J.H.; Ahmed, L.; Engdahl, R. Lipedema in patients after bariatric surgery. Surg. Obes. Relat. Dis. 2016, 12, 1131–1132. [Google Scholar] [CrossRef]
- Pouwels, S.; Huisman, S.; Smelt, H.J.M.; Said, M.; Smulders, J.F. Lipoedema in patients after bariatric surgery: Report of two cases and review of literature. Clin. Obes. 2018, 8, 147–150. [Google Scholar] [CrossRef]
- Pouwels, S.; Smelt, H.J.; Said, M.; Smulders, J.F.; Hoogbergen, M.M. Mobility Problems and Weight Regain by Misdiagnosed Lipoedema After Bariatric Surgery: Illustrating the Medical and Legal Aspects. Cureus 2019, 11, e5388. [Google Scholar] [CrossRef]
- Allen, M.; Schwartz, M.; Herbst, K.L. Interstitial Fluid in Lipedema and Control Skin. Womens Health Rep. 2020, 1, 480–487. [Google Scholar] [CrossRef]
- Strohmeier, K.; Hofmann, M.; Jacak, J.; Narzt, M.-S.; Wahlmueller, M.; Mairhofer, M.; Schaedl, B.; Holnthoner, W.; Barsch, M.; Sandhofer, M.; et al. Multi-Level Analysis of Adipose Tissue Reveals the Relevance of Perivascular Subpopulations and an Increased Endothelial Permeability in Early-Stage Lipedema. Biomedicines 2022, 10, 1163. [Google Scholar] [CrossRef]
- Al-Ghadban, S.; Cromer, W.; Allen, M.; Ussery, C.; Badowski, M.; Harris, D.; Herbst, K.L. Dilated Blood and Lymphatic Microvessels, Angiogenesis, Increased Macrophages, and Adipocyte Hypertrophy in Lipedema Thigh Skin and Fat Tissue. J. Obes. 2019, 2019, 8747461. [Google Scholar] [CrossRef]
- Rasmussen, J.C.; Aldrich, M.B.; Fife, C.E.; Herbst, K.L.; Sevick-Muraca, E.M. Lymphatic function and anatomy in early stages of lipedema. Obesity 2022, 30, 1391–1400. [Google Scholar] [CrossRef] [PubMed]
- Ghods, M.; Georgiou, I.; Schmidt, J.; Kruppa, P. Disease progression and comorbidities in lipedema patients: A 10-year retrospective analysis. Dermatol. Ther. 2020, 33, e14534. [Google Scholar] [CrossRef] [PubMed]
- Amato, A.C.; Amato, J.L.; Benitti, D.A. The Association Between Lipedema and Attention-Deficit/Hyperactivity Disorder. Cureus 2023, 15, e35570. [Google Scholar] [CrossRef]
- Beltran, K.; Herbst, K.L. Differentiating lipedema and Dercum’s disease. Int. J. Obes. 2017, 41, 240–245. [Google Scholar] [CrossRef]
- Luta, X.; Buso, G.; Porceddu, E.; Psychogyiou, R.; Keller, S.; Mazzolai, L. Clinical characteristics, comorbidities, and correlation with advanced lipedema stages: A retrospective study from a Swiss referral centre. PLoS ONE 2025, 20, e0319099. [Google Scholar] [CrossRef]
- Herbst, K.L.; Ussery, C.; Eekema, A. Pilot study: Whole body manual subcutaneous adipose tissue (SAT) therapy improved pain and SAT structure in women with lipedema. Horm. Mol. Biol. Clin. Investig. 2017, 33, 20170035. [Google Scholar] [CrossRef] [PubMed]
- Donahue, P.M.C.; Crescenzi, R.; Petersen, K.J.; Garza, M.; Patel, N.; Lee, C.; Chen, S.C.; Donahue, M.J. Physical Therapy in Women with Early Stage Lipedema: Potential Impact of Multimodal Manual Therapy, Compression, Exercise, and Education Interventions. Lymphat. Res. Biol. 2021, 8, 382–390. [Google Scholar] [CrossRef]
- Szolnoky, G.; Borsos, B.; Barsony, K.; Balogh, M.; Kemeny, L. Complete decongestive physiotherapy with and without pneumatic compression for treatment of lipedema: A pilot study. Lymphology 2008, 41, 40–44. [Google Scholar]
- Szolnoky, G.; Varga, E.; Varga, M.; Tuczai, M.; Dosa-Racz, E.; Kemeny, L. Lymphedema treatment decreases pain intensity in lipedema. Lymphology 2011, 44, 178–182. [Google Scholar]
- Volkan-Yazıcı, M.; Yazici, G.; Esmer, M. The Effects of Complex Decongestive Physiotherapy Applications on Lower Extremity Circumference and Volume in Patients with Lipedema. Lymphat. Res. Biol. 2021, 19, 111–114. [Google Scholar] [CrossRef]
- Volkan-Yazici, M.; Esmer, M. Reducing Circumference and Volume in Upper Extremity Lipedema: The Role of Complex Decongestive Physiotherapy. Lymphat. Res. Biol. 2022, 20, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Atan, T.; Bahar-Özdemir, Y. The Effects of Complete Decongestive Therapy or Intermittent Pneumatic Compression Therapy or Exercise Only in the Treatment of Severe Lipedema: A Randomized Controlled Trial. Lymphat. Res. Biol. 2021, 19, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Wold, L.E.; Hines, E.A., Jr.; Allen, E.V. Lipedema of the legs; a syndrome characterized by fat legs and edema. Ann. Intern. Med. 1951, 34, 1243–1250. [Google Scholar] [CrossRef]
- Urbaniak, G.C.; Plous, S. Research Randomizer; Social Psychology Network: Middletown, CT, USA, 1997. [Google Scholar]
- Forner-Cordero, I.; Perez-Pomares, M.V.; Forner, A.; Ponce-Garrido, A.B.; Munoz-Langa, J. Prevalence of clinical manifestations and orthopedic alterations in patients with lipedema: A prospective cohort study. Lymphology 2021, 54, 170–181. [Google Scholar] [CrossRef]
- Christopher, A.; Kraft, E.; Olenick, H.; Kiesling, R.; Doty, A. The reliability and validity of the Timed Up and Go as a clinical tool in individuals with and without disabilities across a lifespan: A systematic review. Disabil. Rehabil. 2021, 43, 1799–1813. [Google Scholar] [CrossRef]
- Binkley, J.M.; Stratford, P.W.; Lott, S.A.; Riddle, D.L. The Lower Extremity Functional Scale (LEFS): Scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys. Ther. 1999, 79, 371–383. [Google Scholar] [PubMed]
- Ibarra, M.; Eekema, A.; Ussery, C.; Neuhardt, D.; Garby, K.; Herbst, K.L. Subcutaneous adipose tissue therapy reduces fat by dual X-ray absorptiometry scan and improves tissue structure by ultrasound in women with lipoedema and Dercum disease. Clin. Obes. 2018, 8, 398–406. [Google Scholar] [CrossRef]
- Casley-Smith, J.R. Measuring and representing peripheral oedema and its alterations. Lymphology 1994, 27, 56–70. [Google Scholar]
- Yahathugoda, C.; Weiler, M.J.; Rao, R.; De Silva, L.; Dixon, J.B.; Weerasooriya, M.V.; Weil, G.J.; Budge, P.J. Use of a Novel Portable Three-Dimensional Imaging System to Measure Limb Volume and Circumference in Patients with Filarial Lymphedema. Am. J. Trop. Med. Hyg. 2017, 97, 1836–1842. [Google Scholar] [CrossRef]
- Binkley, J.M.; Weiler, M.J.; Frank, N.; Bober, L.; Dixon, J.B.; Stratford, P.W. Assessing Arm Volume in People During and After Treatment for Breast Cancer: Reliability and Convergent Validity of the LymphaTech System. Phys. Ther. 2020, 100, 457–467. [Google Scholar] [CrossRef]
- Ward, L.C.; Gaitatzis, K.; Thompson, B.; Paramanandam, V.S.; Koelmeyer, L.A. Reliability of L-Dex Scores for Assessment of Unilateral Breast Cancer-Related Lymphedema. Eur. J. Breast Health 2024, 20, 251–257. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Duhon, B.H.; Phan, T.T.; Taylor, S.L.; Crescenzi, R.L.; Rutkowski, J.M. Current Mechanistic Understandings of Lymphedema and Lipedema: Tales of Fluid, Fat, and Fibrosis. Int. J. Mol. Sci. 2022, 23, 6621. [Google Scholar] [CrossRef] [PubMed]
- Pereira de Godoy, L.M.; Pereira de Godoy, H.J.; Pereira de Godoy Capeletto, P.; Guerreiro Godoy, M.F.; Pereira de Godoy, J.M. Lipedema and the Evolution to Lymphedema With the Progression of Obesity. Cureus 2020, 12, e11854. [Google Scholar] [CrossRef]
- Coppel, T.; Cunneen, J.; Fetzer, S.; Gordon, K.; Hardy, D.; Jones, J.; McCarroll, A.; O’Neill, C.; Smith, S.; White, C.; et al. Best Practice Guidelines: The Management of Lipoedema; Wounds UK: London, UK, 2017; Volume 13. [Google Scholar]
- Forner-Cordero, I.; Szolnoky, G.; Forner-Cordero, A.; Kemény, L. Lipedema: An overview of its clinical manifestations, diagnosis and treatment of the disproportional fatty deposition syndrome—Systematic review. Clin. Obes. 2012, 2, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Alcolea, J.M.; Alonso Alvarez, B.; Arroyo Bielsa, A.; Domingo, P.; Galindo Garcia, A.; Gracia Graells, M.; Iglesias Urraca, C.; Insua Nipoti, E.; Martin Castillo, E.; Martinez Alvarez, J.R.; et al. Documento de Consenso Lipedema 2018. In Proceedings of the 33rd National Congress of the Spanish Society of Aesthetic Medicine (SEME), Malaga, Spain, 22–24 February 2018. [Google Scholar]
- Sandhofer, M.; Hanke, C.W.; Habbema, L.; Podda, M.; Rapprich, S.; Schmeller, W.; Herbst, K.; Anderhuber, F.; Pilsl, U.; Sattler, G.; et al. Prevention of Progression of Lipedema With Liposuction Using Tumescent Local Anesthesia: Results of an International Consensus Conference. Dermatol. Surg. 2020, 46, 220–228. [Google Scholar] [CrossRef]
- Bertsch, T.; Erbacher, G.; Corda, D.; Damstra, R.J.; van Duinen, K.; Elwell, R.; van Esch-Smeenge, J.; Faerber, G.; Fetzer, S.; Fink, J.; et al. Lipoedema—Myths and facts, Part 5. European Best Practice of Lipoedema—Summary of the European Lipoedema Forum consensus. Phlebologie 2020, 49, 31–49. [Google Scholar]
- Reich-Schupke, S.; Altmeyer, P.; Stücker, M. Thick legs not always lipedema. J. Dtsch. Dermatol. Ges. 2013, 11, 225–233. [Google Scholar] [CrossRef]
- Dean, S.M.; Valenti, E.; Hock, K.; Leffler, J.; Compston, A.; Abraham, W.T. The clinical characteristics of lower extremity lymphedema in 440 patients. J. Vasc. Surg. Venous Lymphat. Disord. 2020, 8, 851–859. [Google Scholar] [CrossRef]
- Russo, S.; Walker, J.L.; Carlson, J.W.; Carter, J.; Ward, L.C.; Covens, A.; Tanner, E.J., 3rd; Armer, J.M.; Ridner, S.; Hayes, S.; et al. Standardization of lower extremity quantitative lymphedema measurements and associated patient-reported outcomes in gynecologic cancers. Gynecol. Oncol. 2021, 160, 625–632. [Google Scholar] [CrossRef]
- Coroneos, C.J.; Wong, F.C.; DeSnyder, S.M.; Shaitelman, S.F.; Schaverien, M.V. Correlation of L-Dex Bioimpedance Spectroscopy with Limb Volume and Lymphatic Function in Lymphedema. Lymphat. Res. Biol. 2019, 17, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Gillham, M.; Sidebotham, D. Chapter 32—Water and Electrolyte Disturbances. In Cardiothoracic Critical Care; Sidebotham, D., McKee, A., Gillham, M., Levy, J.H., Eds.; Butterworth-Heinemann: Philadelphia, PA, USA, 2007; pp. 470–480. [Google Scholar]
- Weiss, L. Histology: Cell and Tissue Biology; Elsevier Biomedical: Amsterdam, The Netherlands, 1983. [Google Scholar]
- Costill, D.L.; Coté, R.; Fink, W. Muscle water and electrolytes following varied levels of dehydration in man. J. Appl. Physiol. 1976, 40, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Durkot, M.J.; Martinez, O.; Brooks-McQuade, D.; Francesconi, R. Simultaneous determination of fluid shifts during thermal stress in a small-animal model. J. Appl. Physiol. 1986, 61, 1031–1034. [Google Scholar] [CrossRef] [PubMed]
- Hvidberg, E. Water-binding by connective tissue and the acid mucopolysaccharides of the ground substance. Acta Pharmacol. Toxicol. 2009, 17, 267–276. [Google Scholar] [CrossRef]
- Comley, K.; Fleck, N. The compressive response of porcine adipose tissue from low to high strain rate. Int. J. Impact Eng. 2012, 46, 1–10. [Google Scholar] [CrossRef]
- Suga, H.; Araki, J.; Aoi, N.; Kato, H.; Higashino, T.; Yoshimura, K. Adipose tissue remodeling in lipedema: Adipocyte death and concurrent regeneration. J. Cutan. Pathol. 2009, 36, 1293–1298. [Google Scholar] [CrossRef]
- Felmerer, G.; Stylianaki, A.; Hägerling, R.; Wang, A.; Ströbel, P.; Hollmén, M.; Lindenblatt, N.; Gousopoulos, E. Adipose Tissue Hypertrophy, An Aberrant Biochemical Profile and Distinct Gene Expression in Lipedema. J. Surg. Res. 2020, 253, 294–303. [Google Scholar] [CrossRef]
- Crescenzi, R.; Donahue, P.M.C.; Petersen, K.J.; Garza, M.; Patel, N.; Lee, C.; Beckman, J.A.; Donahue, M.J. Upper and Lower Extremity Measurement of Tissue Sodium and Fat Content in Patients with Lipedema. Obesity 2020, 28, 907–915. [Google Scholar] [CrossRef]
- Hui, T.H.; Zhou, Z.L.; Qian, J.; Lin, Y.; Ngan, A.H.; Gao, H. Volumetric deformation of live cells induced by pressure-activated cross-membrane ion transport. Phys. Rev. Lett. 2014, 113, 118101. [Google Scholar] [CrossRef]
- Tobias, A.; Ballard, B.D.; Mohiuddin, S.S. Physiology, Water Balance. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- van Esch-Smeenge, J.; Damstra, R.J.; Hendrickx, A.A. Muscle strength and functional exercise capacity in patients with lipoedema and obesity: A comparative study. J. Lymphoedema 2017, 12, 27–31. [Google Scholar]
- Li, Y.; Mao, A.S.; Seo, B.R.; Zhao, X.; Gupta, S.K.; Chen, M.; Han, Y.L.; Shih, T.Y.; Mooney, D.J.; Guo, M. Compression-induced dedifferentiation of adipocytes promotes tumor progression. Sci. Adv. 2020, 6, eaax5611. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, A.; Crescenzi, R.; Usman, T.A.; Reyna, A.J.; Garza, M.E.; Al-Ghadban, S.; Herbst, K.L.; Donahue, P.M.C.; Rutkowski, J.M. Indications of Peripheral Pain, Dermal Hypersensitivity, and Neurogenic Inflammation in Patients with Lipedema. Int. J. Mol. Sci. 2022, 23, 10313. [Google Scholar] [CrossRef]
- Bohannon, R.W. Reference values for the timed up and go test: A descriptive meta-analysis. J. Geriatr. Phys. Ther. 2006, 29, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Benites-Zapata, V.A.; Toro-Huamanchumo, C.J.; Urrunaga-Pastor, D.; Guarnizo-Poma, M.; Lazaro-Alcantara, H.; Paico-Palacios, S.; Pantoja-Torres, B.; Ranilla-Seguin, V.D.C. High waist-to-hip ratio levels are associated with insulin resistance markers in normal-weight women. Diabetes Metab. Syndr. 2019, 13, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Schneider, H.J.; Friedrich, N.; Klotsche, J.; Pieper, L.; Nauck, M.; John, U.; Dörr, M.; Felix, S.; Lehnert, H.; Pittrow, D.; et al. The predictive value of different measures of obesity for incident cardiovascular events and mortality. J. Clin. Endocrinol. Metab. 2010, 95, 1777–1785. [Google Scholar] [CrossRef]
- Brenner, E.; Forner-Cordero, I.; Faerber, G.; Rapprich, S.; Cornely, M. Body mass index vs. waist-to-height-ratio in patients with lipohyperplasia dolorosa (vulgo lipedema). J. Dtsch. Dermatol. Ges. 2023, 21, 1179–1185. [Google Scholar] [CrossRef]
- Bulbena, A.; Gago, J.; Pailhez, G.; Sperry, L.; Fullana, M.A.; Vilarroya, O. Joint hypermobility syndrome is a risk factor trait for anxiety disorders: A 15-year follow-up cohort study. Gen. Hosp. Psychiatry 2011, 33, 363–370. [Google Scholar] [CrossRef]
- Amin, K. The role of mast cells in allergic inflammation. Respir. Med. 2012, 106, 9–14. [Google Scholar] [CrossRef]
- Bonetti, G.; Michelini, S.; Donato, K.; Dhuli, K.; Medori, M.C.; Micheletti, C.; Marceddu, G.; Herbst, K.L.; Cristoni, S.; Fulcheri, E.; et al. Targeting Mast Cells: Sodium Cromoglycate as a Possible Treatment of Lipedema. Clin. Ter. 2023, 174, 256–262. [Google Scholar] [CrossRef]


| Demographic | Group (N) | p-Value * | Total | |
|---|---|---|---|---|
| Control (24) | Treat (22) | |||
| Age | 48.8 ± 8.5 | 52 ± 9.2 | NS | 50.3 ± 8.9 |
| Female/Male | 24/0 | 22/0 | NS | 46 |
| Race: White/Black | 23/2 | 16/5 | NS | 39/7 |
| Systolic BP (mmHg) | 122.5 ± 16 | 124.7 ± 14 | NS | 123.5 ± 15 |
| Diastolic BP (mmHg) | 79.3 ± 8.5 | 80.5 ± 8 | NS | 72.8 ± 9 |
| Heart rate (bpm) | 73.5 ± 8.3 | 72 ± 10.4 | NS | 72.8 ± 9 |
| Height (cm) | 161 ± 7 | 161.6 ± 6.6 | NS | 161.3 ± 6.7 |
| Weight (kg) | 94.9 ± 23 | 104.7 ± 22 | NS | 99.4 ± 22.7 |
| Waist (cm) | 92.4 ± 13 | 98.4 ± 11.4 | NS | 95.2 ± 13 |
| Hips (in) | 121.1 ± 17 | 130.4 ± 15 | NS | 125.3 ± 6.7 |
| WHR | 0.76 ± 0.04 | 0.75 ± 0.05 | NS | 0.76 ± 0.05 |
| WHtR | 0.57 ± 0.08 | 0.61 ± 0.07 | NS | 0.59 ± 0.07 |
| BMI (kg/m2) | 35.3 ± 7 | 38.9 ± 7.5 | NS | 37 ± 7.4 |
| Lipedema Stages | Control (number) | Treatment (number) | ||
| 1 | 0 | 0 | ||
| 2 | 23 | 20 | ||
| 3 | 1 | 2 | ||
| Medical History | Control (%) | Treatment (%) | ||
| Migraine +/− aura | 20/24 | 33/14 | ||
| Depression | 24 | 48 | ||
| Anxiety | 40 | 52 | ||
| Allergies | 100 | 95 | ||
| Hypertension | 8 | 29 | ||
| Prediabetes/Diabetes | 20/12 | 14/9.5 | ||
| Pregnant (ever) | 84 | 86 | ||
| Miscarriage | 32 | 33.3 | ||
| Birth Control | 92 | 90 | ||
| Menopause | 40 | 62 | ||
| Asthma COPD | 16 | 28.5 | ||
| Thyroid Disease | 28 | 38 | ||
| Control (Mean ± SD) | Treatment (Mean ± SD) | |||
| Age 1st menstruation | 12.4 ± 1.9 | 12.2 ± 1.3 | ||
| Times pregnant | 2.3 ± 1.7 | 2.1 ± 2.0 | ||
| Age menopause | 50.2 ± 4.2 | 46.7 ± 7 | ||
| Surgical History | Control (%) | Treatment (%) | ||
| Bariatric | 16 | 33.3 | ||
| Gastrointestinal | 64 | 52 | ||
| Musculoskeletal | 32 | 43 | ||
| Reproductive | 72 | 67 | ||
| Location | Visit 2 | Visit 3 | p-Value |
|---|---|---|---|
| Control Group | |||
| Under Umbilicus | 40.3 ± 17.3 | 40.5 ± 14.8 | NS |
| Right Anterior Thigh | 61.1 ± 6.3 | 62.2 ± 4.8 | NS |
| Right Medial Thigh | 55.2 ± 9.1 | 56.9 ± 7 | NS |
| Left Anterior Thigh | 60.8 ± 6.4 | 62.6 ± 5 | NS |
| Left Medial Thigh | 55.5 ± 9.3 | 57.9 ± 7 | NS |
| Treatment Group | |||
| Under Umbilicus | 45.1 ± 14.3 | 38.9 ± 14.4 | 0.0279 |
| Right Anterior Thigh | 63.8 ± 4.7 | 64.1 ± 4.4 | NS |
| Right Medial Thigh | 57.1 ± 8 | 58.8 ± 7 | NS |
| Left Anterior Thigh | 62.2 ± 6.8 | 64.1 ± 4 | NS |
| Left Medial Thigh | 58.1 ± 7.5 | 59 ± 9 | NS |
| Adipose Tissue Location | Control (n = 24) | |||||
| Visit 2 | p-Value | Visit 3 | p-Value | |||
| Pre | Post | Pre | Post | |||
| Right Leg | ||||||
| Anterior thigh | 2.2 ± 1 | 2.1 ± 1.0 | NS | 2.3 ± 1.0 | 2.3 ± 1.0 | NS |
| Lateral thigh | 2.1 ± 1.1 | 2.1 ± 1.0 | NS | 2.2 ± 0.9 | 2.2 ± 0.9 | NS |
| Medial thigh | 2.3 ± 1.2 | 2.3 ± 1.3 | NS | 2.5 ± 1.1 | 2.5 ± 1.2 | NS |
| Medial knee | 1.9 ± 1.1 | 1.6 ± 0.7 | NS | 1.5 ± 0.5 | 1.4 ± 0.5 | NS |
| Pad under knee | 0.84 ± 0.4 | 0.8 ± 0.4 | NS | 0.94 ± 0.5 | 0.94 ± 0.5 | NS |
| Posterior calf | 1.44 ± 0.5 | 1.4 ± 0.4 | NS | 1.4 ± 0.4 | 1.4 ± 0.4 | NS |
| Left Leg | ||||||
| Anterior thigh | 2.1 ± 0.9 | 2.2 ± 0.9 | NS | 2.2 ± 1.0 | 2.2 ± 1.1 | NS |
| Lateral thigh | 2.1 ± 1.0 | 2.1 ± 0.8 | NS | 2.2 ± 0.9 | 2.2 ± 0.9 | NS |
| Medial thigh | 2.3 ± 1.2 | 2.3 ± 1.2 | NS | 2.5 ± 1.1 | 2.5 ± 1.2 | NS |
| Medial knee | 1.7 ± 0.7 | 1.6 ± 0.7 | NS | 1.4 ± 0.5 | 1.4 ± 0.5 | NS |
| Pad under knee | 0.82 ± 0.4 | 0.89 ± 0.4 | NS | 1.0 ± 0.5 | 0.95 ± 0.5 | NS |
| Posterior calf | 1.5 ± 0.5 | 1.4 ± 0.4 | NS | 1.4 ± 0.4 | 1.5 ± 0.4 | NS |
| Adipose Tissue Location | Treatment (n = 22) | |||||
| Visit 2 | p-Value | Visit 3 | p-Value | |||
| Pre | Post | Pre | Post | |||
| Right Leg | ||||||
| Anterior thigh | 2.3 ± 1.0 | 2.1 ± 0.9 | 0.009 | 2.1 ± 0.8 | 2.0 ± 0.8 | NS |
| Lateral thigh | 2.2 ± 0.9 | 2.1 ± 0.8 | NS | 2.1 ± 0.6 | 2.0 ± 0.6 | NS |
| Medial thigh | 2.6 ± 1.2 | 2.5 ± 0.9 | NS | 2.3 ± 1.0 | 2.2 ± 0.9 | 0.0097 |
| Medial knee | 1.9 ± 0.7 | 1.7 ± 0.5 | NS | 1.5 ± 0.3 | 1.4 ± 0.2 | 0.0097 |
| Pad under knee | 0.86 ± 0.4 | 0.74 ± 0.4 | 0.025 | 0.9 ± 0.4 | 0.9 ± 0.4 | NS |
| Posterior calf | 1.5 ± 0.3 | 1.4 ± 0.3 | 0.036 | 1.4 ± 0.2 | 1.3 ± 0.2 | NS |
| Left Leg | ||||||
| Anterior thigh | 2.2 ± 1.0 | 2.1 ± 0.9 | 0.007 | 2.1 ± 0.8 | 2.0 ± 0.8 | NS |
| Lateral thigh | 2.2 ± 0.8 | 2.0 ± 0.7 | NS | 2.0 ± 0.6 | 1.9 ± 0.6 | NS |
| Medial thigh | 2.6 ± 1.2 | 2.3 ± 1.0 | NS | 2.3 ± 1.0 | 2.2 ± 0.9 | NS |
| Medial knee | 1.9 ± 0.6 | 1.8 ± 0.5 | NS | 1.5 ± 0.2 | 1.5 ± 0.3 | NS |
| Pad under knee | 0.86 ± 0.4 | 0.8 ± 0.4 | NS | 1.0 ± 0.7 | 0.8 ± 0.3 | NS |
| Posterior calf | 1.5 ± 0.3 | 1.4 ± 0.3 | NS | 1.4 ± 0.2 | 1.4 ± 0.5 | NS |
| Location | Control (n = 24) | Treatment (n = 22) | ||||
|---|---|---|---|---|---|---|
| Visit 2 | Visit 3 | p-Value | Visit 2 | Visit 3 | p-Value | |
| Right Leg | ||||||
| Tender | 4.7 ± 2.2 | 3.7 ± 1.9 | NS | 4.6 ± 2.2 | 2.5 ± 1.7 | 0.0003 |
| Ache throb | 4.1 ± 2.3 | 2.9 ± 2.4 | NS | 4.5 ± 2.4 | 1.3 ± 1.8 | <0.0001 |
| Burn Sting | 2.2 ± 2.4 | 1.7 ± 1.9 | NS | 2.6 ± 2.4 | 0.59 ± 1.3 | 0.0016 |
| Tired Heavy | 5.0 ± 2.3 | 4.0 ± 2.5 | NS | 5.5 ± 2.5 | 1.9 ± 1.9 | <0.0001 |
| Swelling Tightness | 4.8 ± 2.5 | 3.7 ± 2.4 | 0.0377 | 4.5 ± 2.6 | 1.5 ± 1.5 | 0.0005 |
| Difficulty Walking | 2.5 ± 2.9 | 1.8 ± 2.0 | NS | 4.1 ± 2.8 | 0.7 ± 1.3 | <0.0001 |
| Easy bruising | 5.9 ± 2.89 | 5.0 ± 2.5 | NS | 5.9 ± 3.0 | 3.3 ± 3.2 | 0.0016 |
| Left Leg | ||||||
| Tender | 4.7 ± 2.2 | 3.7 ± 1.9 | NS | 5.0 ± 2.0 | 2.5 ± 1.7 | <0.0001 |
| Ache Throb | 4.1 ± 2.3 | 2.9 ± 2.4 | NS | 4.8 ± 2.2 | 1.3 ± 1.8 | <0.0001 |
| Burn Sting | 2.2 ± 2.4 | 1.7 ± 1.9 | NS | 2.6 ± 2.4 | 0.59 ± 1.3 | 0.0008 |
| Tired Heavy | 5.0 ± 2.3 | 4.0 ± 2.5 | NS | 5.6 ± 2.4 | 1.9 ± 1.9 | <0.0001 |
| Swelling Tightness | 4.8 ± 2.5 | 3.7 ± 2.4 | NS | 5.1 ± 2.6 | 1.4 ± 1.6 | <0.0001 |
| Difficulty Walking | 2.5 ± 2.9 | 1.8 ± 2.0 | NS | 4.2 ± 2.8 | 0.73 ± 1.3 | <0.0001 |
| Easy Bruising | 5.9 ± 2.9 | 5.0 ± 2.5 | NS | 5.9 ± 3.0 | 3.3 ± 3.2 | 0.0011 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herbst, K.L.; Zelaya, C.; Sommerville, M.; Zimmerman, T.; McHutchison, L. An Advanced Pneumatic Compression Therapy System Improves Leg Volume and Fluid, Adipose Tissue Thickness, Symptoms, and Quality of Life and Reduces Risk of Lymphedema in Women with Lipedema. Life 2025, 15, 725. https://doi.org/10.3390/life15050725
Herbst KL, Zelaya C, Sommerville M, Zimmerman T, McHutchison L. An Advanced Pneumatic Compression Therapy System Improves Leg Volume and Fluid, Adipose Tissue Thickness, Symptoms, and Quality of Life and Reduces Risk of Lymphedema in Women with Lipedema. Life. 2025; 15(5):725. https://doi.org/10.3390/life15050725
Chicago/Turabian StyleHerbst, Karen L., Carlos Zelaya, Marianne Sommerville, Tatiana Zimmerman, and Lindy McHutchison. 2025. "An Advanced Pneumatic Compression Therapy System Improves Leg Volume and Fluid, Adipose Tissue Thickness, Symptoms, and Quality of Life and Reduces Risk of Lymphedema in Women with Lipedema" Life 15, no. 5: 725. https://doi.org/10.3390/life15050725
APA StyleHerbst, K. L., Zelaya, C., Sommerville, M., Zimmerman, T., & McHutchison, L. (2025). An Advanced Pneumatic Compression Therapy System Improves Leg Volume and Fluid, Adipose Tissue Thickness, Symptoms, and Quality of Life and Reduces Risk of Lymphedema in Women with Lipedema. Life, 15(5), 725. https://doi.org/10.3390/life15050725








