Assessment of Primary Stability and Micromotion of Different Fixation Techniques for Scapular Spine Bone Blocks for the Reconstruction of Critical Bone Loss of the Anterior Glenoid—A Biomechanical Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Implications
2.2. Specimen Preparation
- DSF group: Scapular spine bone block augmentation using double-screw fixation (n = 11)
- SSBBC group: Scapular spine bone block augmentation using single-suture bone block cerclage (n = 10)
- DSBBC group: Scapular spine bone block augmentation using double-suture bone block cerclage (n = 10)
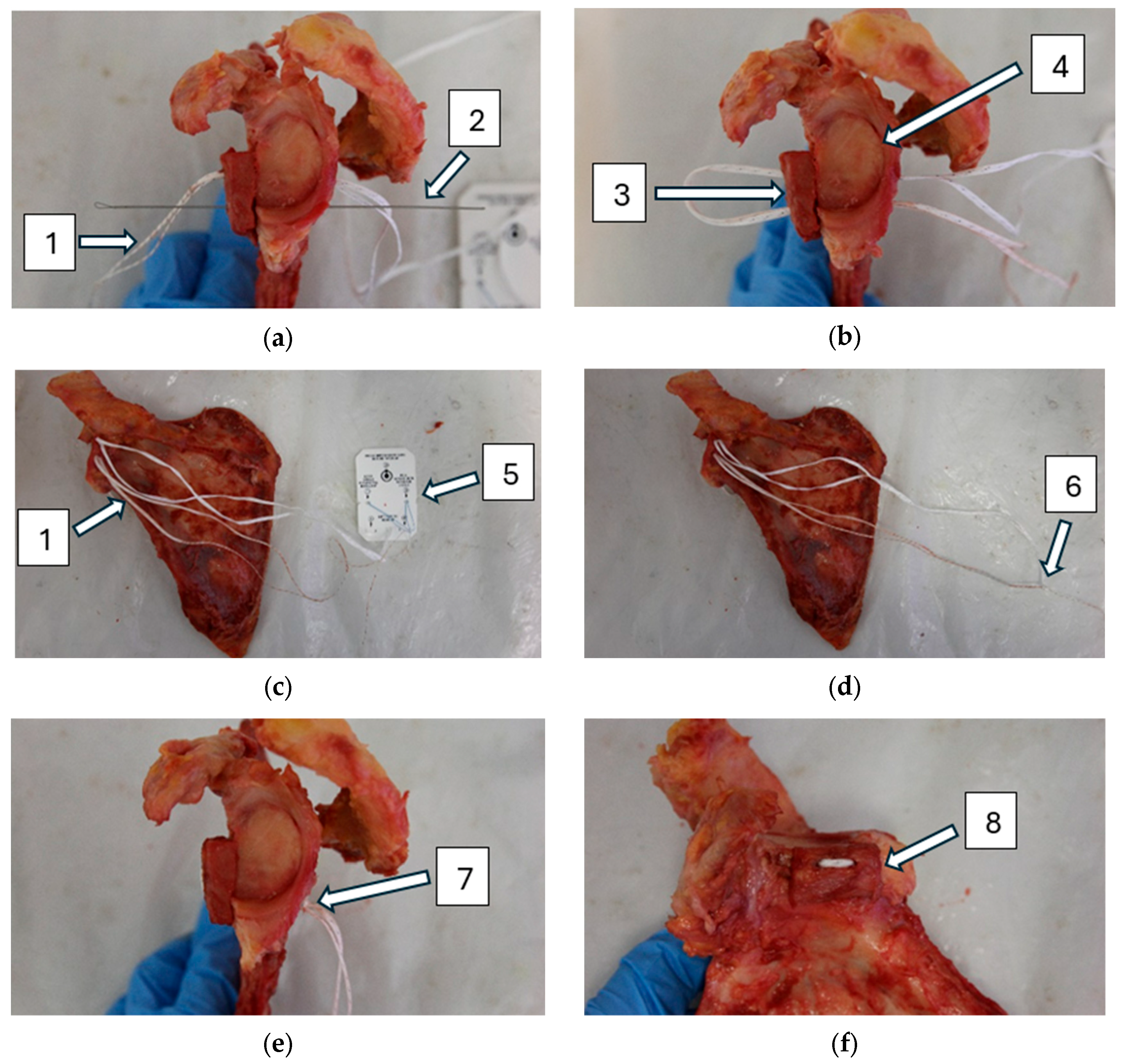
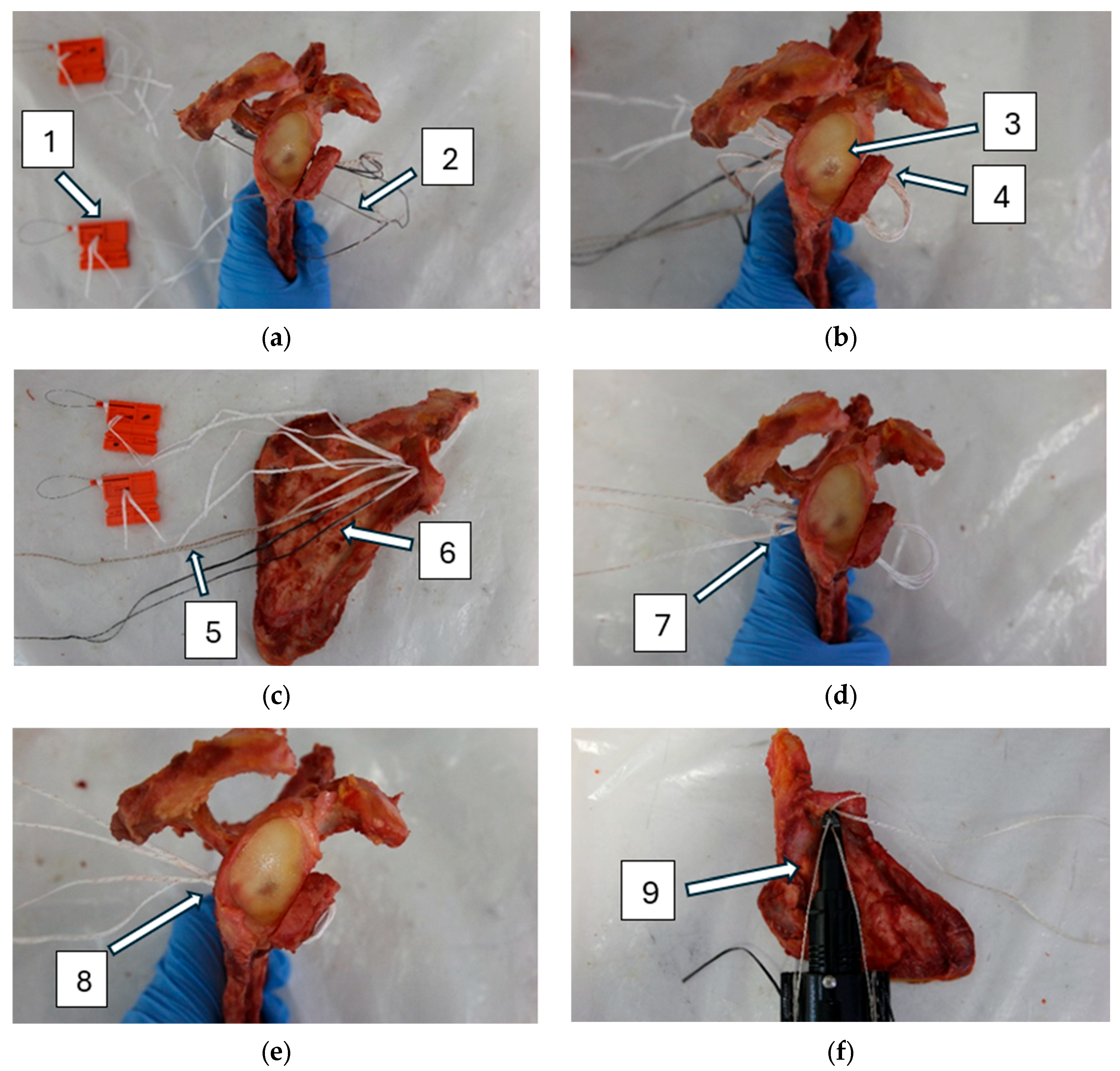
2.3. Glenoid Augmentation Procedure
2.3.1. Double-Screw Fixation
2.3.2. Single-Suture Bone Block Cerclage
2.3.3. Double-Suture Bone Block Cerclage
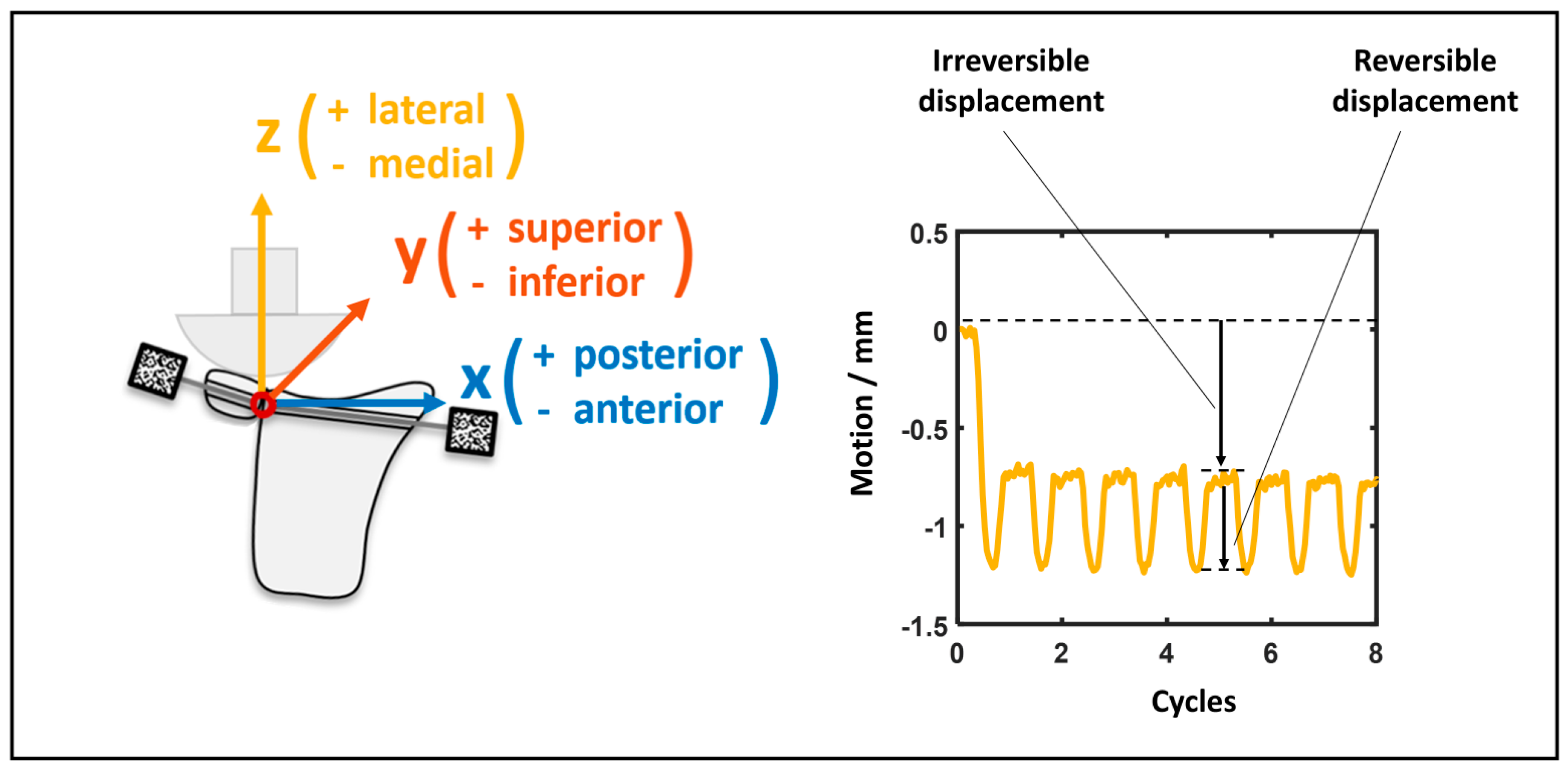
2.4. Biomechanical Testing
2.5. Statistical Analysis
3. Results
3.1. DSF vs. SSBBC
3.2. DSF vs. DSBBC
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DSF | Double-screw fixation |
| SSBBC | Single-suture bone block cerclage |
| DSBBC | Double-suture bone block cerclage |
References
- Zacchilli, M.A.; Owens, B.D. Epidemiology of Shoulder Dislocations Presenting to Emergency Departments in the United States. J. Bone Jt. Surg. 2010, 92, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Midtgaard, K.S.; Bøe, B.; Lundgreen, K.; Wünsche, B.; Moatshe, G. Fremre skulderluksasjon—Utredning og behandling. Tidsskr. Den Nor. Legeforening 2021, 141, 1074–1077. [Google Scholar] [CrossRef] [PubMed]
- Dodson, C.C.; Cordasco, F.A. Anterior Glenohumeral Joint Dislocations. Orthop. Clin. N. Am. 2008, 39, 507–518. [Google Scholar] [CrossRef]
- Owens, B.D.; Duffey, M.L.; Nelson, B.J.; DeBerardino, T.M.; Taylor, D.C.; Mountcastle, S.B. The Incidence and Characteristics of Shoulder Instability at the United States Military Academy. Am. J. Sports Med. 2007, 35, 1168–1173. [Google Scholar] [CrossRef]
- Nazzal, E.M.; Herman, Z.J.; Engler, I.D.; Dalton, J.F.; Freehill, M.T.; Lin, A. First-Time Traumatic Anterior Shoulder Dislocation: Current Concepts. J. ISAKOS 2023, 8, 101–107. [Google Scholar] [CrossRef]
- Wasserstein, D.N.; Sheth, U.; Colbenson, K.; Henry, P.D.G.; Chahal, J.; Dwyer, T.; Kuhn, J.E. The True Recurrence Rate and Factors Predicting Recurrent Instability After Nonsurgical Management of Traumatic Primary Anterior Shoulder Dislocation: A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 2616–2625. [Google Scholar] [CrossRef]
- Murphy, A.I.; Hurley, E.T.; Hurley, D.J.; Pauzenberger, L.; Mullett, H. Long-Term Outcomes of the Arthroscopic Bankart Repair: A Systematic Review of Studies at 10-Year Follow-Up. J. Shoulder Elbow Surg. 2019, 28, 2084–2089. [Google Scholar] [CrossRef]
- Van Der Linde, J.A.; Van Kampen, D.A.; Terwee, C.B.; Dijksman, L.M.; KleinJan, G.; Willems, W.J. Long-Term Results After Arthroscopic Shoulder Stabilization Using Suture Anchors: An 8- to 10-Year Follow-Up. Am. J. Sports Med. 2011, 39, 2396–2403. [Google Scholar] [CrossRef]
- Voos, J.E.; Livermore, R.W.; Feeley, B.T.; Altchek, D.W.; Williams, R.J.; Warren, R.F.; Cordasco, F.A.; Allen, A.A. HSS Sports Medicine Service Prospective Evaluation of Arthroscopic Bankart Repairs for Anterior Instability. Am. J. Sports Med. 2010, 38, 302–307. [Google Scholar] [CrossRef]
- Zimmermann, S.M.; Scheyerer, M.J.; Farshad, M.; Catanzaro, S.; Rahm, S.; Gerber, C. Long-Term Restoration of Anterior Shoulder Stability: A Retrospective Analysis of Arthroscopic Bankart Repair Versus Open Latarjet Procedure. J. Bone Jt. Surg. 2016, 98, 1954–1961. [Google Scholar] [CrossRef]
- Bigliani, L.U.; Newton, P.M.; Steinmann, S.P.; Connor, P.M.; McIlveen, S.J. Glenoid Rim Lesions Associated with Recurrent Anterior Dislocation of the Shoulder. Am. J. Sports Med. 1998, 26, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Min, K.S.; Horng, J.; Cruz, C.; Ahn, H.J.; Patzkowski, J. Glenoid Bone Loss in Recurrent Shoulder Instability After Arthroscopic Bankart Repair: A Systematic Review. J. Bone Jt. Surg. 2023, 105, 1815–1821. [Google Scholar] [CrossRef]
- Shaha, J.S.; Cook, J.B.; Song, D.J.; Rowles, D.J.; Bottoni, C.R.; Shaha, S.H.; Tokish, J.M. Redefining “Critical” Bone Loss in Shoulder Instability: Functional Outcomes Worsen with “Subcritical” Bone Loss. Am. J. Sports Med. 2015, 43, 1719–1725. [Google Scholar] [CrossRef] [PubMed]
- Moroder, P.; Damm, P.; Wierer, G.; Böhm, E.; Minkus, M.; Plachel, F.; Märdian, S.; Scheibel, M.; Khatamirad, M. Challenging the Current Concept of Critical Glenoid Bone Loss in Shoulder Instability: Does the Size Measurement Really Tell It All? Am. J. Sports Med. 2019, 47, 688–694. [Google Scholar] [CrossRef] [PubMed]
- Griffith, J.F.; Antonio, G.E.; Yung, P.S.H.; Wong, E.M.C.; Yu, A.B.; Ahuja, A.T.; Chan, K.M. Prevalence, Pattern, and Spectrum of Glenoid Bone Loss in Anterior Shoulder Dislocation: CT Analysis of 218 Patients. Am. J. Roentgenol. 2008, 190, 1247–1254. [Google Scholar] [CrossRef]
- Gilat, R.; Haunschild, E.D.; Lavoie-Gagne, O.Z.; Tauro, T.M.; Knapik, D.M.; Fu, M.C.; Cole, B.J. Outcomes of the Latarjet Procedure Versus Free Bone Block Procedures for Anterior Shoulder Instability: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2021, 49, 805–816. [Google Scholar] [CrossRef]
- Lunn, J.V.; Castellano-Rosa, J.; Walch, G. Recurrent Anterior Dislocation after the Latarjet Procedure: Outcome after Revision Using a Modified Eden-Hybinette Operation. J. Shoulder Elbow Surg. 2008, 17, 744–750. [Google Scholar] [CrossRef]
- Frank, R.M.; Golijanin, P.; Cole, B.J.; Verma, N.N.; Romeo, A.A.; Provencher, M.T. Clinical and Radiographic Outcomes of Distal Tibia Allograft Reconstruction for Glenoid Bone Defects in Recurrent Anterior Shoulder Instability. J. Shoulder Elbow Surg. 2016, 25, e327. [Google Scholar] [CrossRef]
- Liles, J.L.; Ganokroj, P.; Peebles, A.M.; Mologne, M.S.; Provencher, C.M.T. Primary Distal Tibia Allograft for Restoration of Glenohumeral Stability with Anterior Glenoid Bone Loss. Arthrosc. Tech. 2022, 11, e1039–e1043. [Google Scholar] [CrossRef]
- Williams, H.L.M.; Evans, J.P.; Furness, N.D.; Smith, C.D. It’s Not All About Redislocation: A Systematic Review of Complications After Anterior Shoulder Stabilization Surgery. Am. J. Sports Med. 2019, 47, 3277–3283. [Google Scholar] [CrossRef]
- Longo, U.G.; Loppini, M.; Rizzello, G.; Ciuffreda, M.; Maffulli, N.; Denaro, V. Latarjet, Bristow, and Eden-Hybinette Procedures for Anterior Shoulder Dislocation: Systematic Review and Quantitative Synthesis of the Literature. Arthrosc. J. Arthrosc. Relat. Surg. 2014, 30, 1184–1211. [Google Scholar] [CrossRef]
- Carbone, S.; Moroder, P.; Runer, A.; Resch, H.; Gumina, S.; Hertel, R. Scapular Dyskinesis after Latarjet Procedure. J. Shoulder Elbow Surg. 2016, 25, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Moroder, P.; Kathi, T.; Lacheta, L.; Karpinski, K.; Paksoy, A.; Akgün, D. Arthroscopic Bone Block Cerclage Technique Using a Tricortical Scapular Spine Autograft for Glenoid Reconstruction in Patients with Anterior Shoulder Instability. Arthrosc. Tech. 2022, 11, e379–e383. [Google Scholar] [CrossRef] [PubMed]
- Rohman, E.; Gronbeck, K.; Tompkins, M.; Mittelsteadt, M.; Kirkham, J.A.; Arciero, R.A. Scapular Spine Dimensions and Suitability as a Glenoid Bone Graft Donor Site. Am. J. Sports Med. 2019, 47, 2469–2477. [Google Scholar] [CrossRef] [PubMed]
- Kuan, F.-C.; Hsu, K.-L.; Lin, F.-H.; Hong, C.-K.; Chen, Y.; Shih, C.-A.; Su, W.-R. Morphometric and Biomechanical Comparison of the Scapular Spine and Coracoid Graft in Anterior Shoulder Instability. Am. J. Sports Med. 2022, 50, 3625–3634. [Google Scholar] [CrossRef]
- Youssef, Y.; Heilemann, M.; Melcher, P.; Fischer, J.-P.; Schleifenbaum, S.; Hepp, P.; Theopold, J. Assessment of Micromotion at the Bone-Bone Interface after Coracoid and Scapular-Spine Bone-Block Augmentation for the Reconstruction of Critical Anterior Glenoid Bone Loss—A Biomechanical Cadaver Study. BMC Musculoskelet. Disord. 2023, 24, 790. [Google Scholar] [CrossRef]
- Butt, U.; Charalambous, C.P. Complications Associated with Open Coracoid Transfer Procedures for Shoulder Instability. J. Shoulder Elbow Surg. 2012, 21, 1110–1119. [Google Scholar] [CrossRef]
- Sarna, N.; Dhillon, J.; Maguire, J.A.; Scillia, A.J.; Kraeutler, M.J. Surgical Options and Clinical Outcomes Following a Failed Latarjet Procedure: A Systematic Review. J. Shoulder Elbow Surg. 2024, 33, 2850–2858. [Google Scholar] [CrossRef]
- Lurie, B.M.; Paez, C.J.; Howitt, S.R.; Pennock, A.T. Suture-Button Versus Screw Fixation in Adolescent Syndesmotic Injuries: Functional Outcomes and Maintenance of Reduction. J. Pediatr. Orthop. 2021, 41, e427–e432. [Google Scholar] [CrossRef]
- Peeters, I.; Depover, A.; Van Tongel, A.; De Wilde, L. A Review of Metallic and Non-Metallic Cerclage in Orthopaedic Surgery: Is There Still a Place for Metallic Cerclage? Injury 2019, 50, 1627–1633. [Google Scholar] [CrossRef]
- Rosenow, C.S.; Leland, D.P.; Camp, C.L.; Barlow, J.D. Sutures, Screws, Buttons, and Anchors: A Review of Current Bone Graft Fixation Devices for Glenoid Bone Loss in the Unstable Shoulder. Curr. Rev. Musculoskelet. Med. 2024, 17, 207–221. [Google Scholar] [CrossRef] [PubMed]
- Ye, M.; Chen, J.; Hu, F.; Liu, Y.; Tan, Y. Suture versus Screw Fixation Technique for Tibial Eminence Fracture: A Meta-Analysis of Laboratory Studies. J. Orthop. Surg. 2020, 28, 2309499020907977. [Google Scholar] [CrossRef] [PubMed]
- Bergmann, G.; Graichen, F.; Bender, A.; Rohlmann, A.; Halder, A.; Beier, A.; Westerhoff, P. In Vivo Gleno-Humeral Joint Loads during Forward Flexion and Abduction. J. Biomech. 2011, 44, 1543–1552. [Google Scholar] [CrossRef] [PubMed]
- Pogorzelski, J.; Beitzel, K.; Imhoff, A.B.; Braun, S. Die Mini-open-Latarjet-Technik als Therapie bei rezidivierender vorderer Instabilität des Schultergelenks. Oper. Orthop. Traumatol. 2016, 28, 408–417. [Google Scholar] [CrossRef]
- Martins, R.; Quental, C.; Folgado, J.; Ângelo, A.C.; De Campos Azevedo, C. Influence of Graft Positioning during the Latarjet Procedure on Shoulder Stability and Articular Contact Pressure: Computational Analysis of the Bone Block Effect. Biology 2022, 11, 1783. [Google Scholar] [CrossRef]
- Kenwright, J.; Goodship, A.E.; Kelly, D.J.; Newman, J.H.; Harris, J.D.; Richardson, J.B.; Evans, M.; Spriggins, A.J.; Burrough, S.J.; Rowley, D.I. Effect of Controlled Axial Micromovement on Healing of Tibial Fractures. Lancet 1986, 328, 1185–1187. [Google Scholar] [CrossRef]
- Rechter, G.R.; Anthony, R.T.; Rennard, J.; Kellam, J.F.; Warner, S.J. The Impact of Early Axial Interfragmentary Motion on the Fracture Healing Environment: A Scoping Review. Injury 2024, 55, 111917. [Google Scholar] [CrossRef]
- Ganse, B.; Orth, M.; Roland, M.; Diebels, S.; Motzki, P.; Seelecke, S.; Kirsch, S.-M.; Welsch, F.; Andres, A.; Wickert, K.; et al. Concepts and Clinical Aspects of Active Implants for the Treatment of Bone Fractures. Acta Biomater. 2022, 146, 1–9. [Google Scholar] [CrossRef]
- Yang, Q.; Xu, M.; Fang, H.; Gao, Y.; Zhu, D.; Wang, J.; Chen, Y. Targeting Micromotion for Mimicking Natural Bone Healing by Using NIPAM/Nb2C Hydrogel. Bioact. Mater. 2024, 39, 41–58. [Google Scholar] [CrossRef]
- Ritter, D.; Hachem, A.-I.; Scheibel, M.; Raiss, P.; Denard, P.J.; Campagnoli, A.; Wijdicks, C.A.; Bachmaier, S. Primary Stability and Bone Contact Loading Evaluation of Suture and Screw Based Coracoid Graft Fixation for Anterior Glenoid Bone Loss. Am. J. Sports Med. 2023, 51, 2858–2868. [Google Scholar] [CrossRef]
- Hachem, A.-I.; Del Carmen, M.; Verdalet, I.; Rius, J. Arthroscopic Bone Block Cerclage: A Fixation Method for Glenoid Bone Loss Reconstruction Without Metal Implants. Arthrosc. Tech. 2019, 8, e1591–e1597. [Google Scholar] [CrossRef] [PubMed]
- Kelly, S.R.; Kim, H.M. Arthroscopic Bone Block Cerclage Suture Fixation of Fresh Distal Tibial Allograft for Anterior Glenoid Reconstruction. Arthrosc. Tech. 2023, 12, e1955–e1961. [Google Scholar] [CrossRef] [PubMed]
- Hachem, A.; Diaz-Apablaza, E.; Molina-Creixell, A.; Ruis, X.; Videla, S.; Luis Agulló, J. Clinical Outcomes and Graft Resorption After Metal-Free Bone Block Suture Tape Cerclage Fixation for Recurrent Anterior Shoulder Instability: A Computed Tomography Analysis. Am. J. Sports Med. 2024, 52, 1472–1482. [Google Scholar] [CrossRef] [PubMed]
- Boileau, P.; Saliken, D.; Gendre, P.; Seeto, B.L.; d’Ollonne, T.; Gonzalez, J.-F.; Bronsard, N. Arthroscopic Latarjet: Suture-Button Fixation Is a Safe and Reliable Alternative to Screw Fixation. Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 1050–1061. [Google Scholar] [CrossRef]
- Khiami, F.; Gérometta, A.; Loriaut, P. Management of Recent First-Time Anterior Shoulder Dislocations. Orthop. Traumatol. Surg. Res. 2015, 101, S51–S57. [Google Scholar] [CrossRef]
- Cutts, S.; Prempeh, M.; Drew, S. Anterior Shoulder Dislocation. Ann. R. Coll. Surg. Engl. 2009, 91, 2–7. [Google Scholar] [CrossRef]


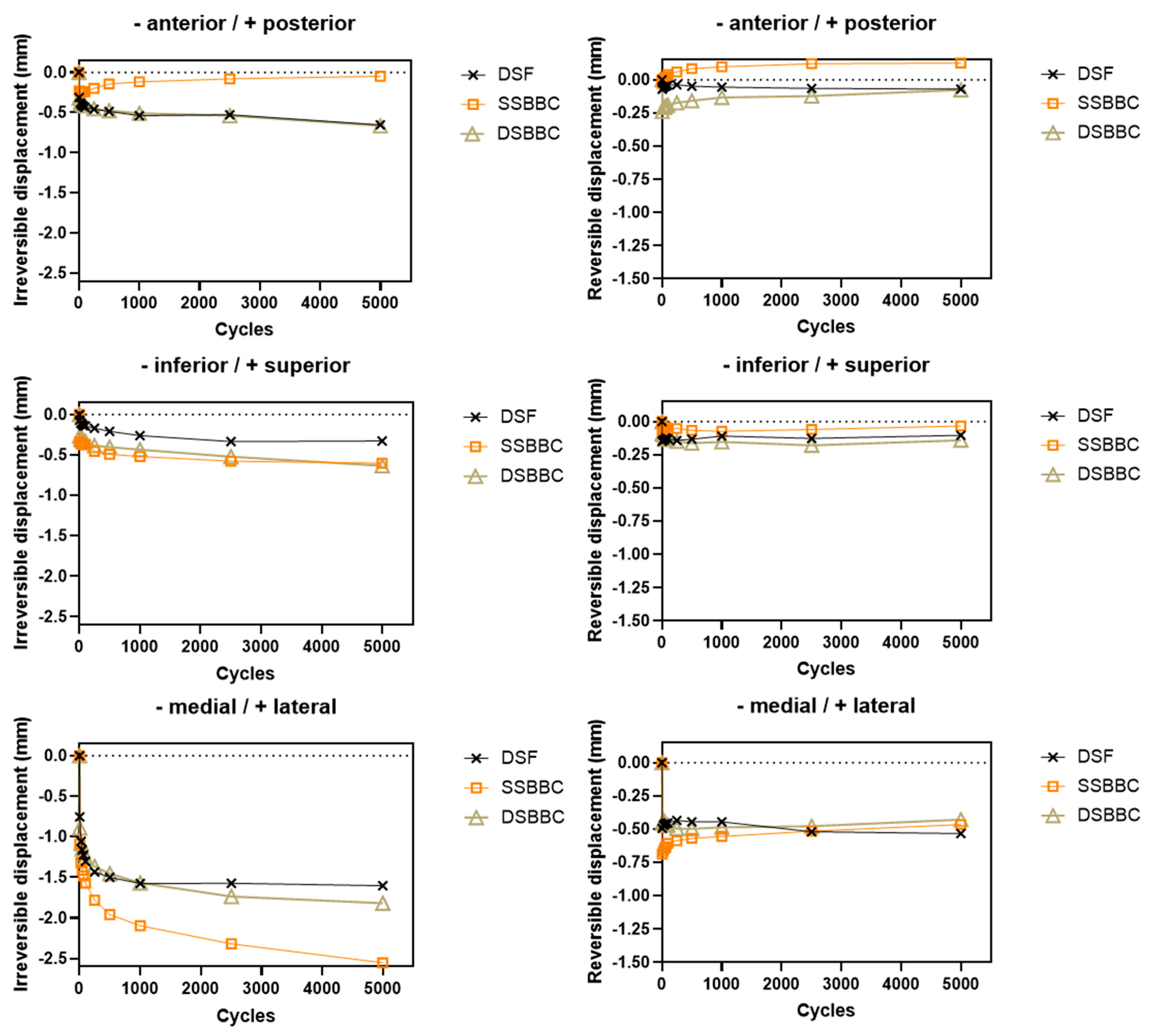
| Procedure | DSF | SSBBC | DSBBC |
|---|---|---|---|
| Irreversible displacement/mm | |||
| x | −0.65 ± 0.92 | −0.05 ± 0.48 | −0.67 ± 0.65 |
| y | −0.33 ± 0.38 | −0.60 ± 0.66 | −0.63 ± 1.10 |
| z | −1.60 ± 0.81 | −2.55 ± 0.47 * | −1.82 ± 0.78 |
| Reversible displacement/mm | |||
| x | −0.07 ± 0.10 | 0.13 ± 0.09 * | −0.08 ± 0.22 |
| y | −0.10 ± 0.13 | −0.03 ± 0.14 | −0.14 ± 0.15 |
| z | −0.53 ± 0.40 | −0.47 ± 0.15 | −0.43 ± 0.32 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brehmer, A.; Youssef, Y.; Heilemann, M.; Wendler, T.; Fischer, J.-P.; Schleifenbaum, S.; Hepp, P.; Theopold, J. Assessment of Primary Stability and Micromotion of Different Fixation Techniques for Scapular Spine Bone Blocks for the Reconstruction of Critical Bone Loss of the Anterior Glenoid—A Biomechanical Study. Life 2025, 15, 658. https://doi.org/10.3390/life15040658
Brehmer A, Youssef Y, Heilemann M, Wendler T, Fischer J-P, Schleifenbaum S, Hepp P, Theopold J. Assessment of Primary Stability and Micromotion of Different Fixation Techniques for Scapular Spine Bone Blocks for the Reconstruction of Critical Bone Loss of the Anterior Glenoid—A Biomechanical Study. Life. 2025; 15(4):658. https://doi.org/10.3390/life15040658
Chicago/Turabian StyleBrehmer, Anton, Yasmin Youssef, Martin Heilemann, Toni Wendler, Jean-Pierre Fischer, Stefan Schleifenbaum, Pierre Hepp, and Jan Theopold. 2025. "Assessment of Primary Stability and Micromotion of Different Fixation Techniques for Scapular Spine Bone Blocks for the Reconstruction of Critical Bone Loss of the Anterior Glenoid—A Biomechanical Study" Life 15, no. 4: 658. https://doi.org/10.3390/life15040658
APA StyleBrehmer, A., Youssef, Y., Heilemann, M., Wendler, T., Fischer, J.-P., Schleifenbaum, S., Hepp, P., & Theopold, J. (2025). Assessment of Primary Stability and Micromotion of Different Fixation Techniques for Scapular Spine Bone Blocks for the Reconstruction of Critical Bone Loss of the Anterior Glenoid—A Biomechanical Study. Life, 15(4), 658. https://doi.org/10.3390/life15040658






