Endoscopic Foraminotomy for the Treatment of Lumbar Neuro-Foramen Stenosis: Role of CT in Treatment Planning and Post-Operative Assessment
Abstract
1. Introduction
2. Methods
2.1. Study Sample
2.2. Clinical Evaluation
2.3. CT Protocol
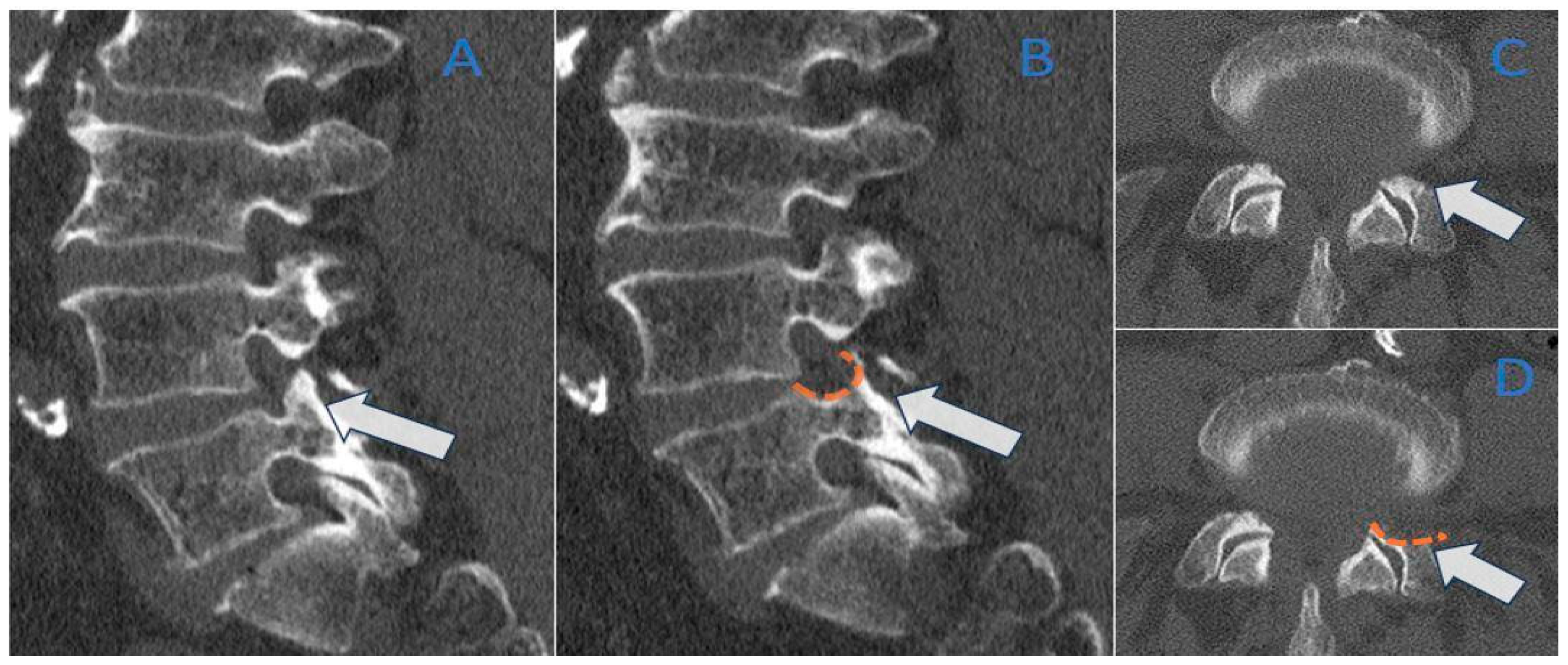
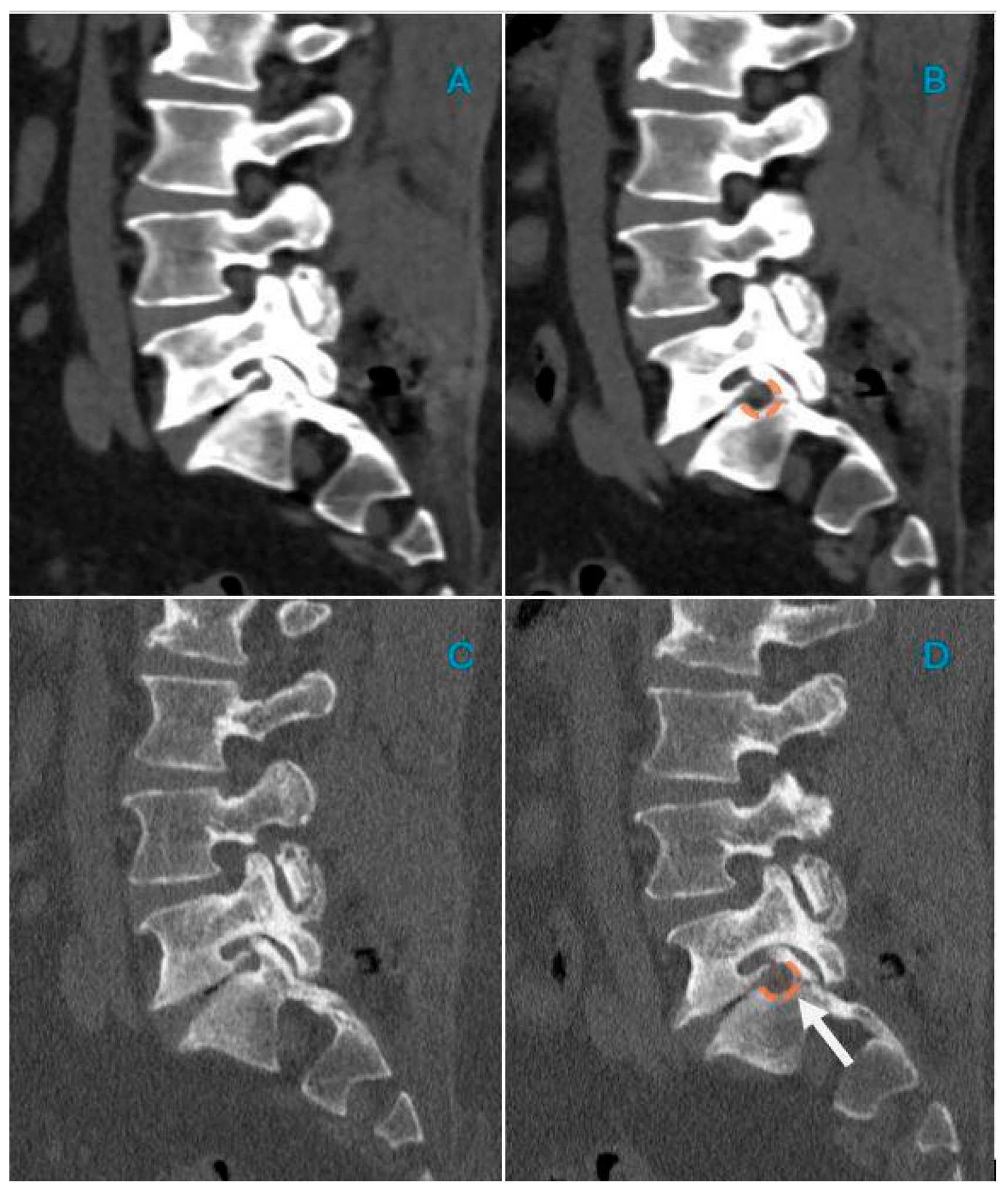
2.4. CT Post-Processing
2.5. Image Analysis
2.6. Statistical Analysis
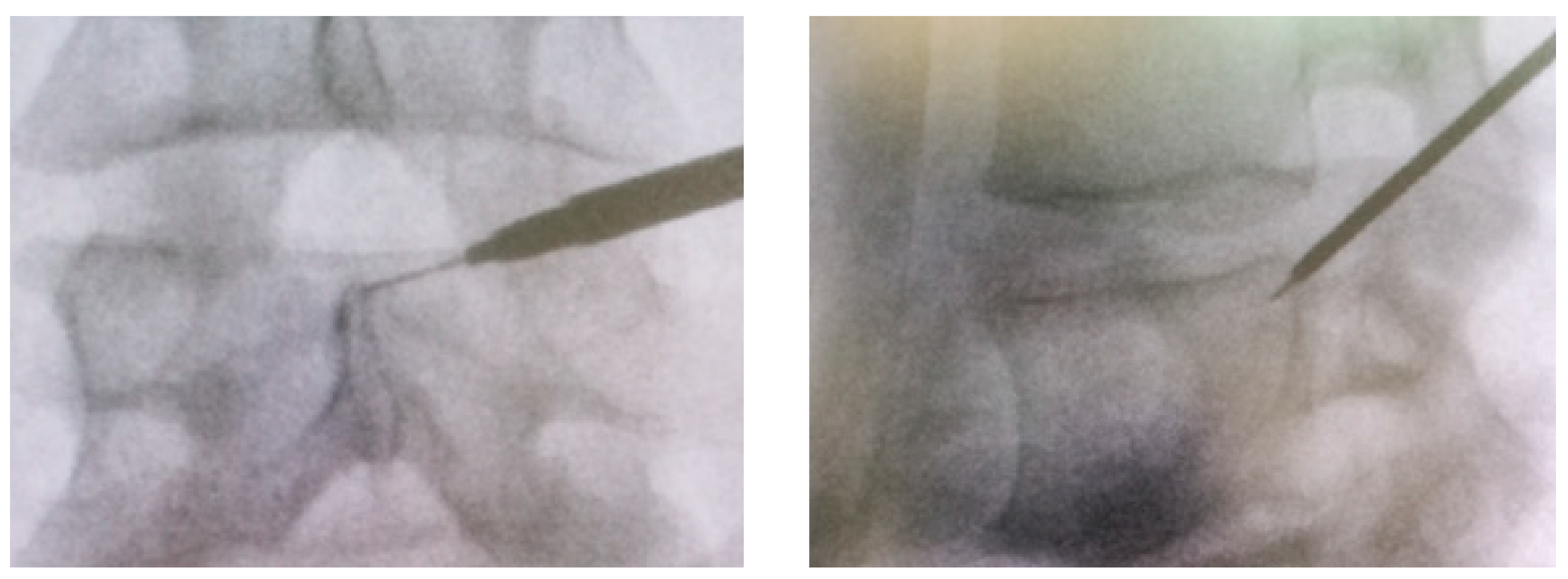
2.7. Foraminotomy Surgery
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shiri, R.; Falah-Hassani, K.; Heliövaara, M.; Solovieva, S.; Amiri, S.; Lallukka, T.; Burdorf, A.; Husgafvel-Pursiainen, K.; Viikari-Juntura, E. Risk Factors for Low Back Pain: A Population-Based Longitudinal Study. Arthritis Care Res. 2019, 71, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Heliövaara, M.; Knekt, P.; Aromaa, A. Incidence and risk factors of herniated lumbar intervertebral disc or sciatica leading to hospitalization. J. Chronic Dis. 1987, 40, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Frymoyer, J.W. Lumbar disk disease: Epidemiology. Instr. Course Lect. 1992, 41, 217–223. [Google Scholar] [PubMed]
- Kabeer, A.S.; Osmani, H.T.; Patel, J.; Robinson, P.; Ahmed, N. The adult with low back pain: Causes, diagnosis, imaging features and management. Br. J. Hosp. Med. 2023, 84, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Casser, H.R.; Seddigh, S.; Rauschmann, M. Acute Lumbar Back Pain. Dtsch. Ärzteblatt Int. 2016, 113, 223–234. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, A.S.; Xu, A.; Ansari, K.; Hardacker, K.; Anderson, G.; Alsoof, D.; Daniels, A.H. Lumbar Disc Herniation: Diagnosis and Management. Am. J. Med. 2023, 136, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Delgado-López, P.D.; Rodríguez-Salazar, A.; Martín-Alonso, J.; Martín-Velasco, V. Hernia discal lumbar: Historia natural, papel de la exploración, timing de la cirugía, opciones de tratamiento y conflicto de intereses [Lumbar disc herniation: Natural history, role of physical examination, timing of surgery, treatment options and conflicts of interests]. Neurocirugia 2017, 28, 124–134. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Hoy, D.; Brooks, P.; Blyth, F.; Buchbinder, R. The Epidemiology of low back pain. Best Pract. Res. Clin. Rheumatol. 2010, 24, 769–781. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef] [PubMed]
- Özer, A.F.; Akyoldaş, G.; Çevik, O.M.; Aydın, A.L.; Hekimoğlu, M.; Sasani, M.; Öktenoğlu, T.; Çerezci, Ö.; Süzer, T. Lumbar Foraminal Stenosis Classification That Guides Surgical Treatment. Int. J. Spine Surg. 2022, 16, 666–673. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, S.; Lee, J.W.; Yeom, J.S.; Kim, K.J.; Kim, H.J.; Chung, S.K.; Kang, H.S. A practical MRI grading system for lumbar foraminal stenosis. AJR Am. J. Roentgenol. 2010, 194, 1095–1098. [Google Scholar] [CrossRef] [PubMed]
- Orita, S.; Inage, K.; Eguchi, Y.; Kubota, G.; Aoki, Y.; Nakamura, J.; Matsuura, Y.; Furuya, T.; Koda, M.; Ohtori, S. Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Gaggiano, C.; Avramovič, M.Z.; Vitale, A.; Emeršič, N.; Sota, J.; Toplak, N.; Gentileschi, S.; Caggiano, V.; Tarsia, M.; Markelj, G.; et al. Systemic auto-inflammatory manifestations in patients with spondyloarthritis. Jt. Bone Spine 2024, 91, 105772. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Munakomi, S.; Cruz, R. Lumbar Spinal Stenosis; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar] [PubMed]
- Heard, J.C.; Lee, Y.; Ezeonu, T.; Lambrechts, M.J.; Issa, T.Z.; Yalla, G.R.; Tran, K.; Singh, A.; Purtill, C.; Somers, S.; et al. Does the Severity of Foraminal Stenosis Impact Outcomes of Lumbar Decompression Surgery? World Neurosurg. 2023, 179, e296–e304. [Google Scholar] [CrossRef] [PubMed]
- Mataki, K.; Koda, M.; Shibao, Y.; Kumagai, H.; Nagashima, K.; Miura, K.; Noguchi, H.; Funayama, T.; Abe, T.; Yamazaki, M. New methods for diagnosing lumbar foraminal stenosis using dynamic digital tomosynthesis radiculography. J. Clin. Neurosci. 2020, 77, 106–109. [Google Scholar] [CrossRef] [PubMed]
- Du, R.; Xu, G.; Bai, X.; Li, Z. Facet Joint Syndrome: Pathophysiology, Diagnosis, and Treatment. J. Pain Res. 2022, 15, 3689–3710. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sivakanthan, S.; Hasan, S.; Hofstetter, C. Full-Endoscopic Lumbar Discectomy. Neurosurg. Clin. N. Am. 2020, 31, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Pan, M.; Li, Q.; Li, S.; Mao, H.; Meng, B.; Zhou, F.; Yang, H. Percutaneous Endoscopic Lumbar Discectomy: Indications and Complications. Pain Physician 2020, 23, 49–56. [Google Scholar] [PubMed]
- Rhee, D.Y.; Ahn, Y. Full-Endoscopic Lumbar Foraminotomy for Foraminal Stenosis in Spondylolisthesis: Two-Year Follow-Up Results. Diagnostics 2022, 12, 3152. [Google Scholar] [CrossRef] [PubMed]
- Malik, K.N.; Giberson, C.; Ballard, M.; Camp, N.; Chan, J. Pain Management Interventions in Lumbar Spinal Stenosis: A Literature Review. Cureus 2023, 15, e44116. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ahn, Y.; Park, H.B.; Yoo, B.R.; Jeong, T.S. Endoscopic lumbar foraminotomy for foraminal stenosis in stable spondylolisthesis. Front. Surg. 2022, 9, 1042184. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giordan, E.; Billeci, D.; Del Verme, J.; Varrassi, G.; Coluzzi, F. Endoscopic Transforaminal Lumbar Foraminotomy: A Systematic Review and Meta-Analysis. Pain Ther. 2021, 10, 1481–1495. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Song, Q.P.; Hai, B.; Zhao, W.K.; Huang, X.; Liu, K.X.; Zhu, B.; Liu, X.G. Full-Endoscopic Foraminotomy with a Novel Large Endoscopic Trephine for Severe Degenerative Lumbar Foraminal Stenosis at L5S1 Level: An Advanced Surgical Technique. Orthop. Surg. 2021, 13, 659–668. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ahn, Y.; Park, H.B. Transforaminal Endoscopic Lumbar Foraminotomy for Juxta-Fusional Foraminal Stenosis. J. Clin. Med. 2023, 12, 5745. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Dong, H.; Tan, H.; Xie, X.; Liu, N.; Zhang, G.; Li, X.; Yang, Y.; Zhu, B. Uniportal Full-endoscopic Foraminotomy for Lumbar Foraminal Stenosis: Clinical Characteristics and Functional Outcomes. Orthop. Surg. 2024, 16, 1861–1870. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shen, S.C.; Chen, H.C.; Tsou, H.K.; Lin, R.H.; Shih, Y.T.; Huang, C.W.; Tang, C.L.; Chen, H.T.; Chang, C.C.; Tzeng, C.Y. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation based on image analysis and clinical findings: A retrospective review of 345 cases. Medicine 2023, 102, e32832. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Evins, A.I.; Banu, M.A.; Njoku, I., Jr.; Elowitz, E.H.; Härtl, R.; Bernado, A.; Hofstetter, C.P. Endoscopic lumbar foraminotomy. J. Clin. Neurosci. 2015, 22, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Jeong, T.S.; Ahn, Y.; Lee, S.G.; Kim, W.K.; Son, S.; Kwon, J.H. Correlation between MRI Grading System and Surgical Findings for Lumbar Foraminal Stenosis. J. Korean Neurosurg. Soc. 2017, 60, 465–470. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jeong, J.; Ham, S.; Shim, E.; Kim, B.H.; Kang, W.Y.; Kang, C.H.; Ahn, K.S.; Lee, K.C.; Choi, H. Electron density dual-energy CT can improve the detection of lumbar disc herniation with higher image quality than standard and virtual non-calcium images. Eur. Radiol. 2024, 34, 7334–7346. [Google Scholar] [CrossRef] [PubMed]
- Foti, G.; Longo, C.; Oliboni, E.; Faccioli, N.; Sanfilippo, L.; Guerriero, M.; Augelli, R.; Motta, L.; Marocco, S. Spondylodiscitis of the thoraco-lumbar spine: Diagnostic performance of dual-energy CT vs. MRI. Eur Radiol. 2025, 35, 1647–1657. [Google Scholar] [CrossRef] [PubMed]
- Murata, S.; Minamide, A.; Iwasaki, H.; Nakagawa, Y.; Hashizume, H.; Yukawa, Y.; Tsutsui, S.; Takami, M.; Okada, M.; Nagata, K.; et al. Microendoscopic decompression for lumbosacral foraminal stenosis: A novel surgical strategy based on anatomical considerations using 3D image fusion with MRI/CT. J. Neurosurg. Spine 2020, 33, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Heller, G.Z.; Manuguerra, M.; Chow, R. How to analyze the Visual Analogue Scale: Myths, truths and clinical relevance. Scand. J. Pain 2016, 13, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Masala, S.; Cesaroni, A.; Sergiacomi, G.; Fiori, R.; Massari, F.; Manenti, G.; Nardi, P.; Simonetti, G. Percutaneous kyphoplasty: New treatment for painful vertebral body fractures. In Vivo 2004, 18, 149–153. [Google Scholar] [PubMed]


| Characteristic | Total |
|---|---|
| Sex | |
| Male | 27 |
| Female | 20 |
| Mean Age (Range) years | 71 (50–91) |
| Operative Level Left | |
| L3–L4 | 1 |
| L4–L5 | 19 |
| L5–S1 | 2 |
| Operative Level Right | |
| L3–L4 | 11 |
| L4–L5 | 17 |
| L5–S1 | 3 |
| Evaluation time | Vas value, mean (SD) |
| Presurgica | 9.17 (0.58) |
| 1 Week | 1.96 (1.09) |
| 1 Month | 0.66 (0.71) |
| Levels | R1 Overall | R1 Symptoms | R1 Not-Symptoms | R1 p-Value | R2 Overall | R2 Symptoms | R2 Not-Symptoms | R2 p-Value |
|---|---|---|---|---|---|---|---|---|
| Left | ||||||||
| L3–L4 (n = 1) | ||||||||
| * cc | 0.55 (2.15) | 4.00 (0.0) | 0.48 (2.12) | 0.069 | 0.02 (1.13) | 4.00 (0.0) | 0.10 (1.00) | 0.001 |
| * tr | 0.08 (1.09) | 0.00 (0.0) | 0.08 (1.10) | >0.9 | 0.15 (1.76) | 0.00 (0.0) | 0.15 (1.78) | >0.9 |
| ** area | 3.96 (14.2) | 30.00 (0.0) | 3.46 (13.9) | 0.064 | 2.38 (10.7) | 40.00 (0.0) | 1.65 (9.43) | 0.043 |
| L4–L5 (n = 19) | ||||||||
| cc | 1.30 (2.36) | 3.11 (1.49) | 0.29 (2.15) | <0.001 | 1.21 (2.09) | 2.89 (2.21) | 0.26 (1.29) | <0.001 |
| tr | 1.25 (1.69) | 2.26 (1.48) | 0.69 (1.55) | <0.001 | 1.28 (1.82) | 2.26 (2.08) | 0.74 (1.42) | 0.006 |
| area | 22.04 (31.4) | 48.47 (24.6) | 7.26 (24.5) | <0.001 | 15.81 (18.6) | 29.9 (16.4) | 7.94 (14.8) | <0.001 |
| L5–S1(n = 2) | ||||||||
| cc | 0.30 (0.87) | 2.00 (0.00) | 0.24 (0.81) | <0.001 | 0.21 (0.74) | 1.50 (0.71) | 0.16 (0.70) | 0.002 |
| tr | 0.68 (2.35) | 5.00 (0.00) | 0.51 (2.23) | <0.001 | 0.62 (1.97) | 1.50 (4.95) | 0.59 (1.88) | >0.9 |
| area | 8.23 (16.9) | 56.00 (24.0) | 6.35 (13.80) | <0.001 | 5.58 (16.4) | 40.0 (46.6) | 4.24 (13.6) | 0.006 |
| Right | ||||||||
| L3–L4 (n = 11) | ||||||||
| cc | 0.66 (1.3) | 2.09 (1.58) | 0.29 (1.02) | <0.001 | 0.66 (2.13) | 2.91 (4.01) | 0.07 (0.34) | <0.001 |
| tr | 0.51 (1.9) | 2.64 (1.43) | 0.05 (1.68) | <0.001 | 0.75 (1.30) | 2.73 (1.42) | 0.24 (0.58) | <0.001 |
| area | 10.96 (21.3) | 35.73 (19.8) | 4.48 (16.6) | <0.001 | 10.6 (21.6) | 34.8 (23.1) | 3.57 (15.9) | <0.001 |
| L4–L5 (n = 17) | ||||||||
| cc | 1.72 (2.03) | 3.29 (1.99) | 0.97 (1.59) | <0.001 | 2.40 (2.96) | 4.24 (2.68) | 1.53 (2.71) | 0.001 |
| tr | 1.57 (2.05) | 3.12 (1.54) | 0.83 (1.86) | <0.001 | 1.17 (1.92) | 2.35 (2.37) | 0.61 (1.38) | 0.001 |
| area | 25.06 (24.2) | 43.24 (11.4) | 16.47 (24.0) | 0.001 | 22.1 (24.80) | 39.3 (20.6) | 14.06 (22.5) | <0.001 |
| L5–S1 (n = 3) | ||||||||
| cc | 0.09 (0.97) | 1.33 (3.51) | 0.02 (0.62) | 0.15 | 0.04 (1.45) | 2.00 (5.29) | 0.16 (0.91) | 0.2 |
| tr | 0.06 (0.60) | 0.67 (1.15) | 0.02 (0.55) | 0.2 | 0.09 (0.65) | 1.33 (1.53) | 0.02 (0.50) | 0.019 |
| area | 2.26 (11.50) | 24.33 (18.0) | 0.94 (9.77) | 0.003 | 0.96 (11.9) | 29.3 (31.3) | 0.74 (7.71) | 0.001 |
| L3 L4 DX | L4 L5 DX | L5 S1 DX | L3 L4 SX | L4 L5 SX | L5 S1 SX | ||
|---|---|---|---|---|---|---|---|
| Pre-treatment | CC | 0.749 (0.586–0.851) | 0.633 (0.419–0.776) | 0.769 (0.631–0.859) | 0.900 (0.834–0.941) | 0.471 (0.237–0.655) | 0.851 (0.754–0.912) |
| TR | 0.300 (0.032–0.527) | 0.630 (0.434–0.769) | 0.332 (0.065–0.554) | 0.730 (0.528–0.845) | 0.503 (0.273–0.679) | 0.460 (0.179–0.662) | |
| AREA | 0.905 (0.841–0.944) | 0.595 (0.387–0.745) | 0.889 (0.792–0.939) | 0.509 (0.281–0.683) | 0.667 (0.488–0.793) | 0.807 (0.554–0.906) | |
| Post-treatment | CC | 0.733 (0.551–0.844) | 0.890 (0.817–0.935) | 0.772 (0.636–0.861) | 0.631 (0.439–0.768) | 0.859 (0.745–0.920) | 0.848 (0.751–0.909) |
| TR | 0.094 (-0.183–0.357) | 0.550 (0.332–0.712) | 0.401 (0.121–0.615) | 0.427 (0.180–0.623) | 0.490 (0.257–0.670) | 0.678 (0.408–0.823) | |
| AREA | 0.849 (0.752–0.910) | 0.680 (0.504–0.802) | 0.817 (0.700–0.890) | 0.402 (0.154–0.603) | 0.847 (0.750–0.909) | 0.847 (0.700–0.918) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foti, G.; Tripodi, G.; Ocello, G.; Manenti, G.; Merci, G.; Mignolli, T.; Sanfilippo, L.; Guerriero, M.; Serra, G. Endoscopic Foraminotomy for the Treatment of Lumbar Neuro-Foramen Stenosis: Role of CT in Treatment Planning and Post-Operative Assessment. Life 2025, 15, 615. https://doi.org/10.3390/life15040615
Foti G, Tripodi G, Ocello G, Manenti G, Merci G, Mignolli T, Sanfilippo L, Guerriero M, Serra G. Endoscopic Foraminotomy for the Treatment of Lumbar Neuro-Foramen Stenosis: Role of CT in Treatment Planning and Post-Operative Assessment. Life. 2025; 15(4):615. https://doi.org/10.3390/life15040615
Chicago/Turabian StyleFoti, Giovanni, Gianluca Tripodi, Giuseppe Ocello, Guglielmo Manenti, Giorgio Merci, Thomas Mignolli, Lorenza Sanfilippo, Massimo Guerriero, and Gerardo Serra. 2025. "Endoscopic Foraminotomy for the Treatment of Lumbar Neuro-Foramen Stenosis: Role of CT in Treatment Planning and Post-Operative Assessment" Life 15, no. 4: 615. https://doi.org/10.3390/life15040615
APA StyleFoti, G., Tripodi, G., Ocello, G., Manenti, G., Merci, G., Mignolli, T., Sanfilippo, L., Guerriero, M., & Serra, G. (2025). Endoscopic Foraminotomy for the Treatment of Lumbar Neuro-Foramen Stenosis: Role of CT in Treatment Planning and Post-Operative Assessment. Life, 15(4), 615. https://doi.org/10.3390/life15040615







