Unveiling Software Limitations in the Assessment of the Minimum Sectional Area and Volume in Cleft LIP and Palate Patients
Abstract
1. Introduction
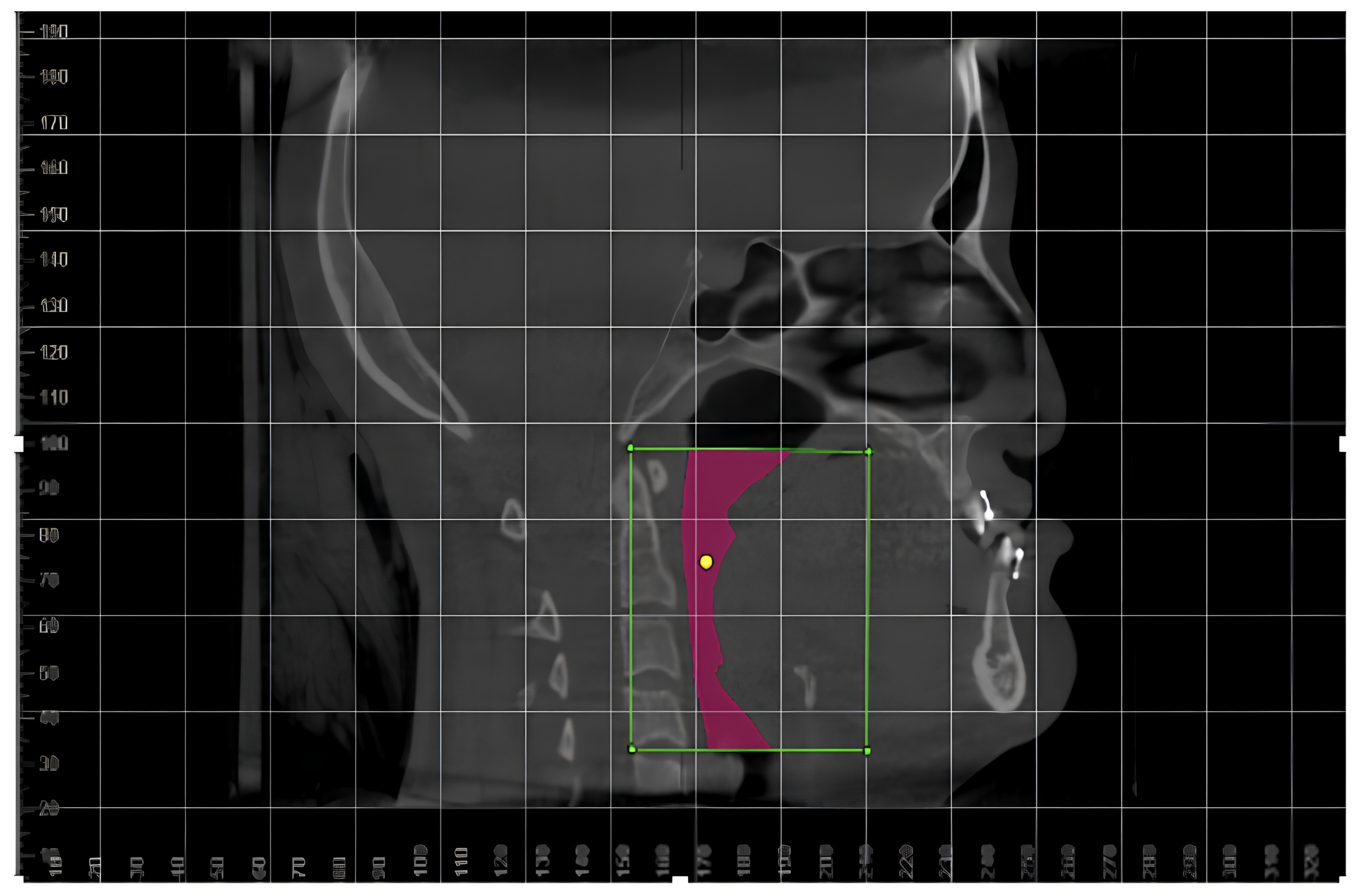
2. Materials and Methods
2.1. Subjects
2.2. Study Protocol
2.3. Error Analysis
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ozawa, T.O.; Shaw, W.C.; Katsaros, C.; Kuijpers-Jagtman, A.M.; Hagberg, C.; Rønning, E.; Semb, G. A New Yardstick for Rating Dental Arch Relationship in Patients with Complete Bilateral Cleft Lip and Palate. Cleft Palate Craniofac. J. 2011, 48, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Bajracharya, M.; Wang, Y.C.; Huang, C.S.; Bhandari, K.; Sinha, S.; Wen-Ching Ko, E. Effects of maxillary advancement on maxillary incisor display in patients with skeletal Class III malocclusion and cleft lip and palate. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 898–906. [Google Scholar] [CrossRef] [PubMed]
- Lacerda, R.H.W.; Ozawa, T.O.; Ramos, T.B.; Furtado, P.G.C.; Oliveira, L.A.D.; Oliveira, A.F.B.D. Facial growth evaluation of complete unilateral cleft lip and palate operated patients: A cleft reference center in Paraíba, Brazil, using the “GOSLON” yardstick. Oral Maxillofac. Surg. 2013, 18, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Posnick, J.C.; Ricalde, P. Cleft-orthognathic surgery. Clin. Plast. Surg. 2004, 31, 315–330. [Google Scholar] [CrossRef] [PubMed]
- McComb, R.W.; Marrinan, E.M.; Nuss, R.C.; Labrie, R.A.; Mulliken, J.B.; Padwa, B.L. Predictors of Velopharyngeal Insufficiency After Le Fort I Maxillary Advancement in Patients with Cleft Palate. J. Oral Maxillofac. Surg. 2011, 69, 2226–2232. [Google Scholar] [CrossRef]
- Trindade-Suedam, I.K.; Lima, T.F.; Campos, L.D.; Yaedú, R.Y.F.; Filho, H.N.; Trindade, I.E.K. Tomographic pharyngeal dimensions in individuals with unilateral cleft lip/palate and class III malocclusion are reduced when compared with controls. Cleft Palate Craniofac. J. 2017, 54, 502–508. [Google Scholar] [PubMed]
- Eslami, N.; Hoseini Zarch, H.; Jahanbin, A.; Darabi, Z.; Moayedi, S. Comparison of Nasopharyngeal Airway Volume in Cleft Lip and Palate Patients with Normal Individuals Using Cone Beam Computed Tomography. J. Craniofac. Surg. 2023, 34, 1111–1114. [Google Scholar] [CrossRef]
- Yatabe-Ioshida, M.S.; Campos, L.D.; Yaedu, R.Y.; Trindade-Suedam, I.K. Upper airway 3D changes of patients with cleft lip and palate after orthognathic surgery. Cleft Palate Craniofac. J. 2019, 56, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Bertier, C.E.; Trindade, I.E.K. Deformidades nasais: Avaliação e tratamento cirúrgico. In Fissuras Labiopalatinas: Uma Abordagem Interdisciplinar; Trindade, I.E.K., Silva-Filho, O.G., Eds.; Editora Santos: São Paulo, Brazil, 2007; pp. 87–107. [Google Scholar]
- Ogawa, T.; Enciso, R.; Shintaku, W.H.; Clark, G.T. Evaluation of cross-section airway configuration of obstructive sleep apnea. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.R.D.R.M.; Pollmann, M.C.F.; Martins, E.J.P. Upper airway dimensions and craniofacial morphology: A correlation study using cone beam computed tomography. Korean J. Orthod. 2024, 54, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Aboudara, C.; Nielsen, I.; Huang, J.C.; Maki, K.; Miller, A.J.; Hatcher, D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 468–479. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-J.; Hong, J.-S.; Hwang, Y.-I.; Park, Y.-H. Three-dimensional analysis of pharyngeal airway in preadolescent children with different anteroposterior skeletal patterns. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 306-e1. [Google Scholar] [CrossRef] [PubMed]
- Schendel, S.A.; Hatcher, D. Automated 3-Dimensional Airway Analysis From Cone-Beam Computed Tomography Data. J. Oral Maxillofac. Surg. 2010, 68, 696–701. [Google Scholar] [CrossRef] [PubMed]
- White, S.M.; Huang, C.J.; Huang, S.C.; Sun, Z.; Eldredge, J.D.; Mallya, S.M. Evaluation of the Upper Airway Morphology: The Role of Cone Beam Computed Tomography. J. Calif. Dent. Assoc. 2015, 43, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Lenza, M.G.; Lenza, M.D.; Dalstra, M.; Melsen, B.; Cattaneo, P.M. An analysis of different approaches to the assessment of upper airway morphology: A CBCT study. Orthod. Craniofac. Res. 2010, 13, 96–105. [Google Scholar] [CrossRef]
- Kim, H.S.; Kim, G.T.; Kim, S.; Lee, J.W.; Kim, E.C.; Kwon, Y.D. Three-dimensional evaluation of the pharyngeal airway using cone-beam computed tomography following bimaxillary orthognathic surgery in skeletal class III patients. Clin. Oral Investig. 2016, 20, 915–922. [Google Scholar] [CrossRef]
- de Torres, H.M.; Evangelista, K.; de Torres, É.M.; Estrela, C.; de Souza Figueiredo, P.T.; Valladares-Neto, J.; Silva, M.A. Comparison of Dimensions of the Nasopharynx and Oropharynx Using Different Anatomical References: Is There Equivalence? J. Oral Maxillofac. Surg. 2019, 77, 2545–2554. [Google Scholar] [CrossRef] [PubMed]
- Guijarro-Martínez, R.; Swennen, G.R. Cone-beam computerized tomography imaging and analysis of the upper airway: A systematic review of the literature. Int. J. Oral Maxillofac. Surg. 2011, 40, 1227–1237. [Google Scholar] [CrossRef] [PubMed]
- El, H.; Palomo, J.M. Measuring the airway in 3 dimensions: A reliability and accuracy study. Am. J. Orthod. Dentofac. Orthop. 2010, 137, S50-e1. [Google Scholar] [CrossRef]
- Weissheimer, A.; Menezes, L.M.D.; Sameshima, G.T.; Enciso, R.; Pham, J.; Grauer, D. Imaging software accuracy for 3-dimensional analysis of the upper airway. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 801–813. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, M.L.; Yatabe, M.; Ioshida, M.; Orlandi, L.; Dumast, P.D.; Trindade-Suedam, I.K. Volumetric reconstruction and determination of minimum crosssectional area of the pharynx in patients with cleft lip and palate: Comparison between two different software. J. Appl. Oral Sci. 2018, 26, e20170282. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, A.; Ronsivalle, V.; Gastaldi, G.; Leonardi, R. Assessment of the accuracy of imaging software for 3D rendering of the upper airway, usable in orthodontic and craniofacial clinical settings. Prog. Orthod. 2022, 23, 22. [Google Scholar] [CrossRef]
- Walter, S.D.; Eliasziw, M.; Donner, A. Sample size and optimal designs for reliability studies. Stat. Med. 1998, 17, 101–110. [Google Scholar] [CrossRef]
- Yushkevich, P.A.; Piven, J.; Hazlett, H.C.; Smith, R.G.; Ho, S.; Gee, J.C.; Gerig, G. User-guided 3D active contour segmentation of anatomical structures: Significantly improved efficiency and reliability. Neuroimage 2006, 31, 1116–1128. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Olszewski, R.; Alexandroni, E.S.; Enciso, R.; Xu, T.; Mah, J.K. The Validity of In Vivo Tooth Volume Determinations From Cone-Beam Computed Tomography. Angle Orthod. 2010, 80, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Alcalde, L.F.A.; Faria, P.E.P.; Nogueira, R.L.M.; Chihara, L.; Sant’Ana, E. Computed tomography visualizing alterations in the upper airway after orthognathic surgery. J. Craniomaxillofac. Surg. 2019, 47, 1041–1045. [Google Scholar] [CrossRef] [PubMed]
- Barrett, J.F.; Keat, N. Artifacts in CT: Recognition and Avoidance. RadioGraphics 2004, 24, 1679–1691. [Google Scholar] [CrossRef] [PubMed]
- Mah, P.; Reeves, T.E.; McDavid, W.D. Deriving Hounsfield units using grey levels in cone beam computed tomography. Dentomaxillofac. Radiol. 2010, 39, 323–335. [Google Scholar] [CrossRef] [PubMed]
- Eguren, M.; Holguin, A.; Diaz, K.; Vidalon, J.; Linan, C.; Pacheco-Pereira, C.; Lagravere Vich, M.O. Can gray values be converted to Hounsfield units? A systematic review. Dentomaxillofac. Radiol. 2022, 51, 20210140. [Google Scholar] [CrossRef]
- Schulze, R.; Heil, U.; Gross, D.; Bruellmann, D.D.; Dranischnikow, E.; Schwanecke, U.; Schoemer, E. Artefacts in CBCT: A review. Dentomaxillofac. Radiol. 2011, 40, 265–273. [Google Scholar] [CrossRef]
- Nackaerts, O.; Maes, F.; Yan, H.; Couto Souza, P.; Pauwels, R.; Jacobs, R. Analysis of intensity variability in multislice and cone beam computed tomography. Clin. Oral Implants Res. 2011, 22, 873–879. [Google Scholar] [CrossRef]
- Silva, I.M.; Freitas, D.Q.; Ambrosano, G.M.; Bóscolo, F.N.; Almeida, S.M. Bone density: Comparative evaluation of Hounsfield units in multislice and cone-beam computed tomography. Braz. Oral Res. 2012, 26, 550–556. [Google Scholar] [CrossRef] [PubMed]

| ICC (Intra) | ||
|---|---|---|
| Software | Minimum Axial Area (mm2) | Vol (cm3) |
| Dolphin | 0.96 | 0.96 |
| InVivo | 1.00 | 0.98 |
| InVesalius | 0.92 | 0.92 |
| ITK-Snap | 0.81 | 0.98 |
| NemoCeph | 1.00 | 0.96 |
| Minimum Axial Area | Volume | |
|---|---|---|
| Comparison | p-Value | p-Value |
| Dolphin vs. InVivo | 6.93 × 10−17 | 7.25 × 10−16 |
| Dolphin vs. InVesalius | 1.20 × 10−15 | 2.74 × 10−11 |
| Dolphin vs. ITK-Snap | 2.26 × 10−12 | 6.63 × 10−15 |
| Dolphin vs. NemoCeph | 2.01 × 10−14 | 6.90 × 10−4 |
| InVivo vs. InVesalius | 4.96 × 10−18 | 6.20 × 10−3 |
| InVivo vs. ITK-Snap | 1.37 × 10−17 | 0.462 |
| InVivo vs. NemoCeph | 5.87 × 10−14 | 7.55 × 10−9 |
| InVesalius vs. ITK-Snap | 5.14 × 10−8 | 1.08 × 10−4 |
| InVesalius vs. NemoCeph | 2.21 × 10−17 | 1.21 × 10−4 |
| ITK-Snap vs. NemoCeph | 4.10 × 10−17 | 5.98 × 10−12 |
| Software | Dolphin3D | InVivoDental | InVesalius | ITK-Snap | NemoFAB |
|---|---|---|---|---|---|
| Files | DICOM | DICOM | DICOM | MULTIPLE | DICOM |
| Segmentation | Quick upper airway segmentation. Good segmentation sensitivity. Segmentation can be checked in 2D slices (axial, coronal, and sagittal). | Quick upper airway segmentation. Threshold interval units (gray levels) compatible with other imaging software. | Segmentation can be checked in 2D slices (axial, coronal, and sagittal). | Segmentation can be checked in 2D slices (axial, coronal, and sagittal). Threshold interval units (gray levels) compatible with other imaging software. | Threshold interval units (gray levels) compatible with other imaging software. |
| Measurements | Automatically calculates volume, area, and mCSA of the segmentation. | Automatically calculates volume, area, and mCSA of the segmentation. | Automatically calculates volume. To determine area and mCSA, it has to export the file to SlicerCMF in order to create a 3D surface model using the SPHARM-PDM module. | Automatically calculates volume. To determine area and mCSA, it has to export the file to SlicerCMF in order to create a 3D surface model using the SPHARM-PDM module. | Automatically calculates volume, area, and mCSA of the segmentation. |
| 3D visualization | Shows an automatic 3D rendering from the CBCT. | Shows an automatic 3D rendering from the CBCT. | Shows volumetric models only from the segmented structures. | Shows volumetric models only from the segmented structures. | Shows an automatic 3D rendering from the CBCT. |
| Saving methods | Saves the volumetric models in the software. Not possible to export data. | Saves the volumetric models in the software. Not possible to export data. | Volumetric models can be saved as independent files and exported to different software. | Volumetric models can be saved as independent files and exported to different software. | Saves the volumetric models in the software. Not possible to export data. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, B.E.; Yaedú, R.Y.F.; Pereira-Silva, M.; Fabris, A.L.d.S.; Garcia-Usó, M.; Magro Filho, O.; Soares, S. Unveiling Software Limitations in the Assessment of the Minimum Sectional Area and Volume in Cleft LIP and Palate Patients. Life 2025, 15, 226. https://doi.org/10.3390/life15020226
Costa BE, Yaedú RYF, Pereira-Silva M, Fabris ALdS, Garcia-Usó M, Magro Filho O, Soares S. Unveiling Software Limitations in the Assessment of the Minimum Sectional Area and Volume in Cleft LIP and Palate Patients. Life. 2025; 15(2):226. https://doi.org/10.3390/life15020226
Chicago/Turabian StyleCosta, Beethoven Estevao, Renato Yassutaka Faria Yaedú, Maísa Pereira-Silva, André Luis da Silva Fabris, Michele Garcia-Usó, Osvaldo Magro Filho, and Simone Soares. 2025. "Unveiling Software Limitations in the Assessment of the Minimum Sectional Area and Volume in Cleft LIP and Palate Patients" Life 15, no. 2: 226. https://doi.org/10.3390/life15020226
APA StyleCosta, B. E., Yaedú, R. Y. F., Pereira-Silva, M., Fabris, A. L. d. S., Garcia-Usó, M., Magro Filho, O., & Soares, S. (2025). Unveiling Software Limitations in the Assessment of the Minimum Sectional Area and Volume in Cleft LIP and Palate Patients. Life, 15(2), 226. https://doi.org/10.3390/life15020226






