Congenital Pulmonary Airway Malformation in Preterm Infants: A Case Report and Review of the Literature
Abstract
1. Introduction
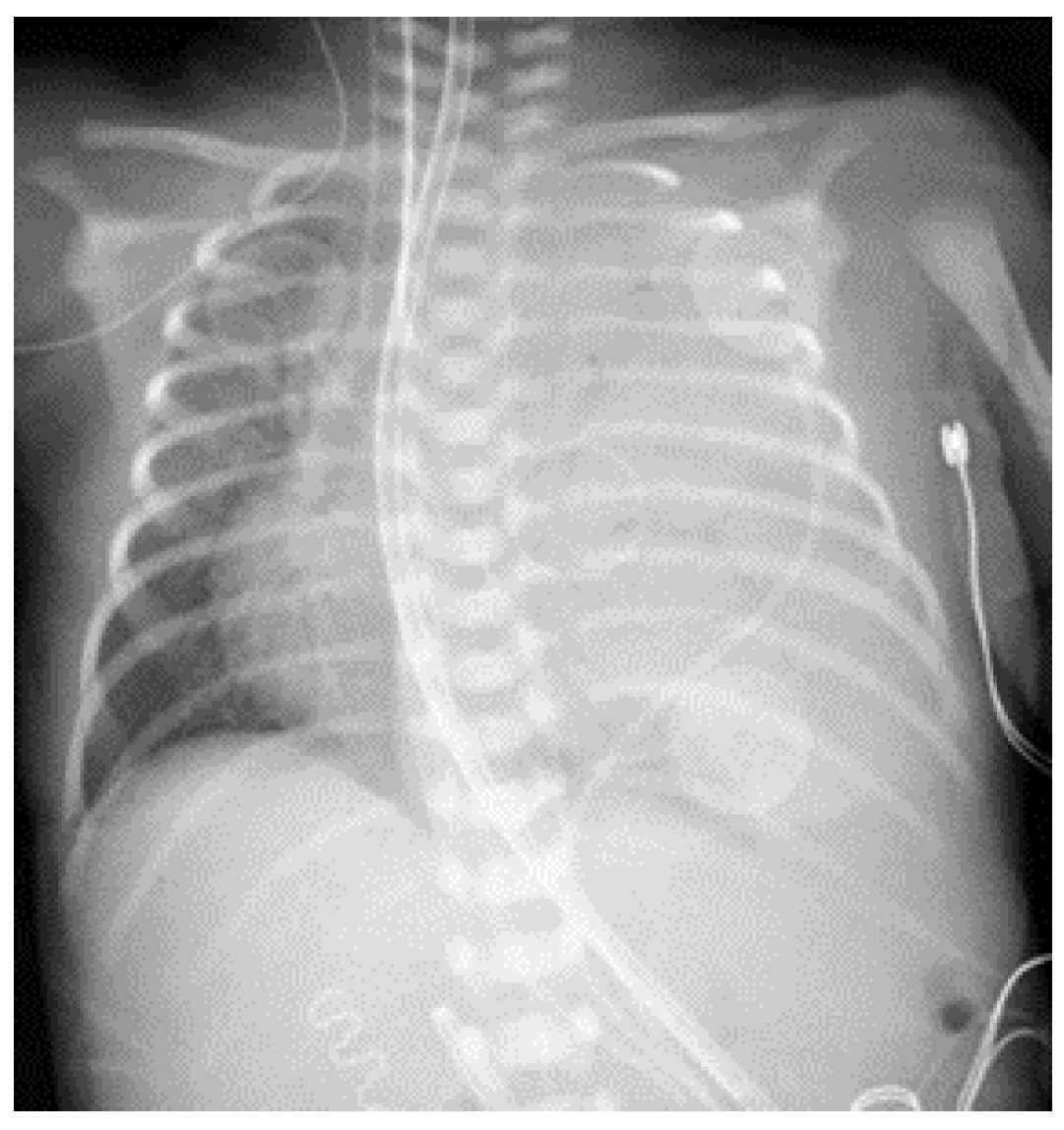
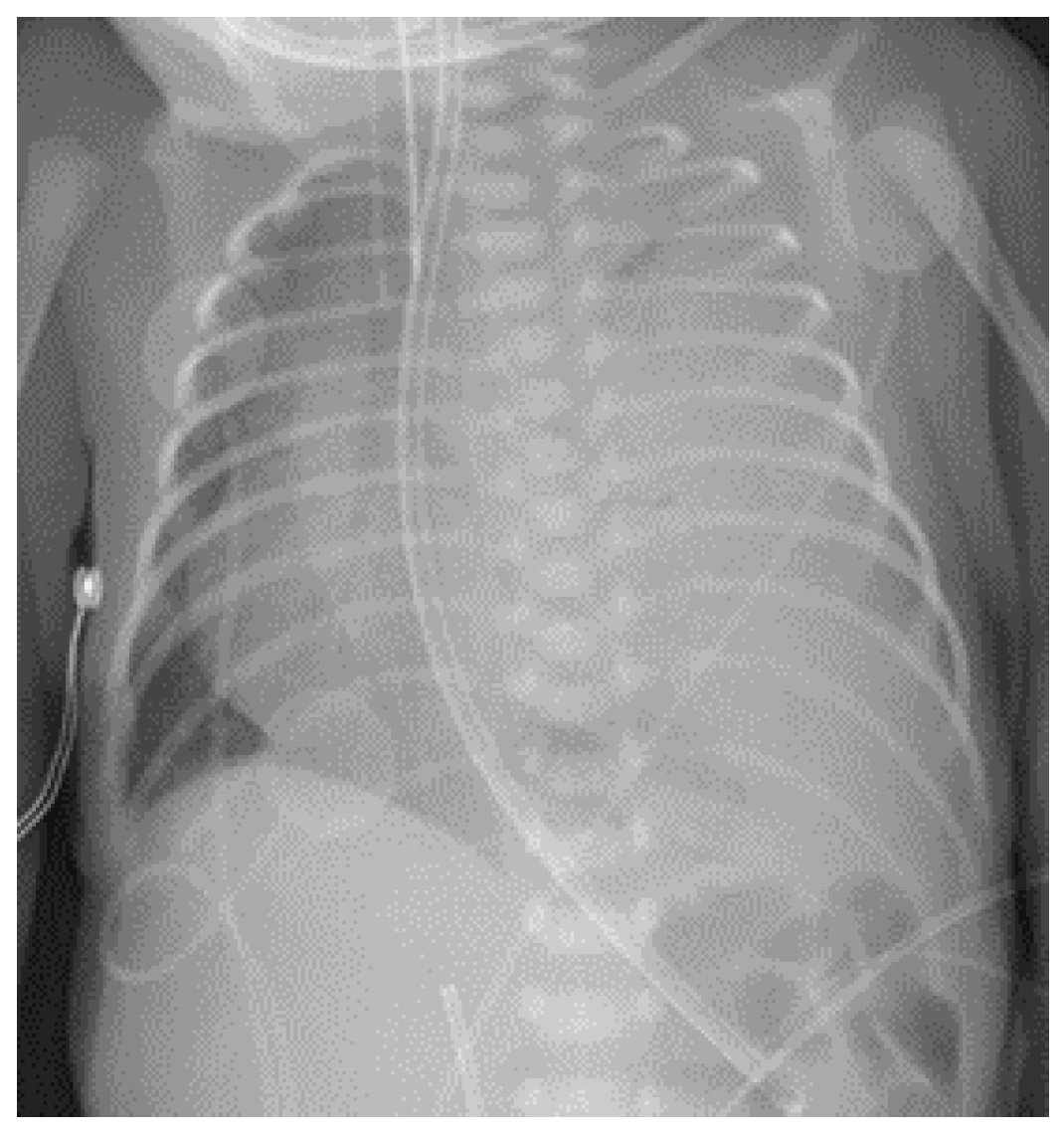
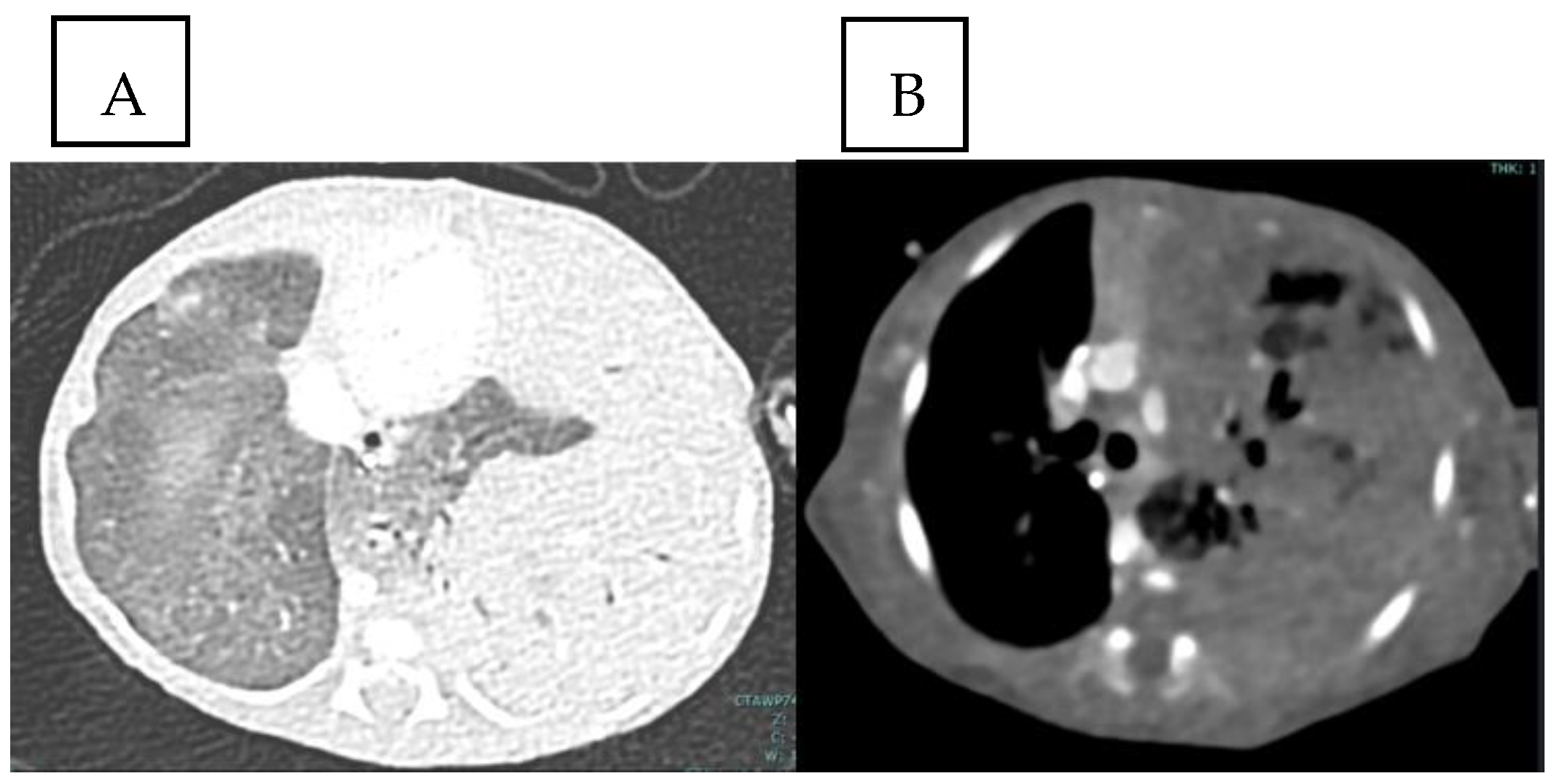
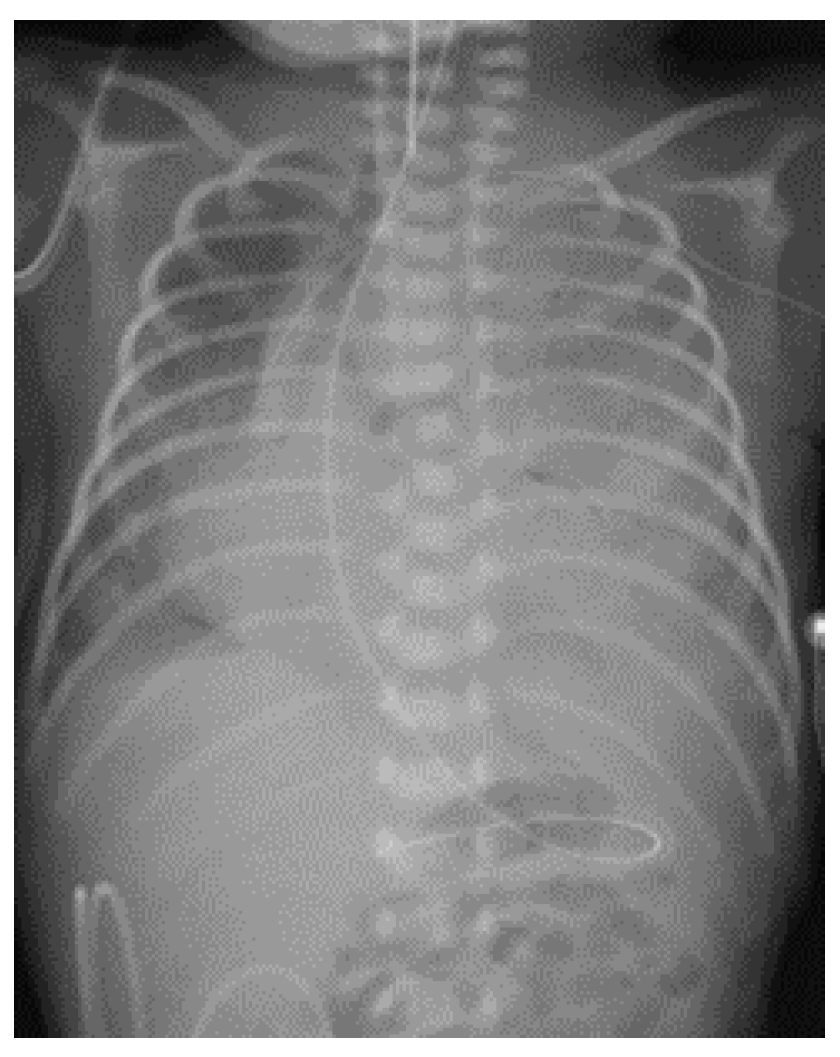
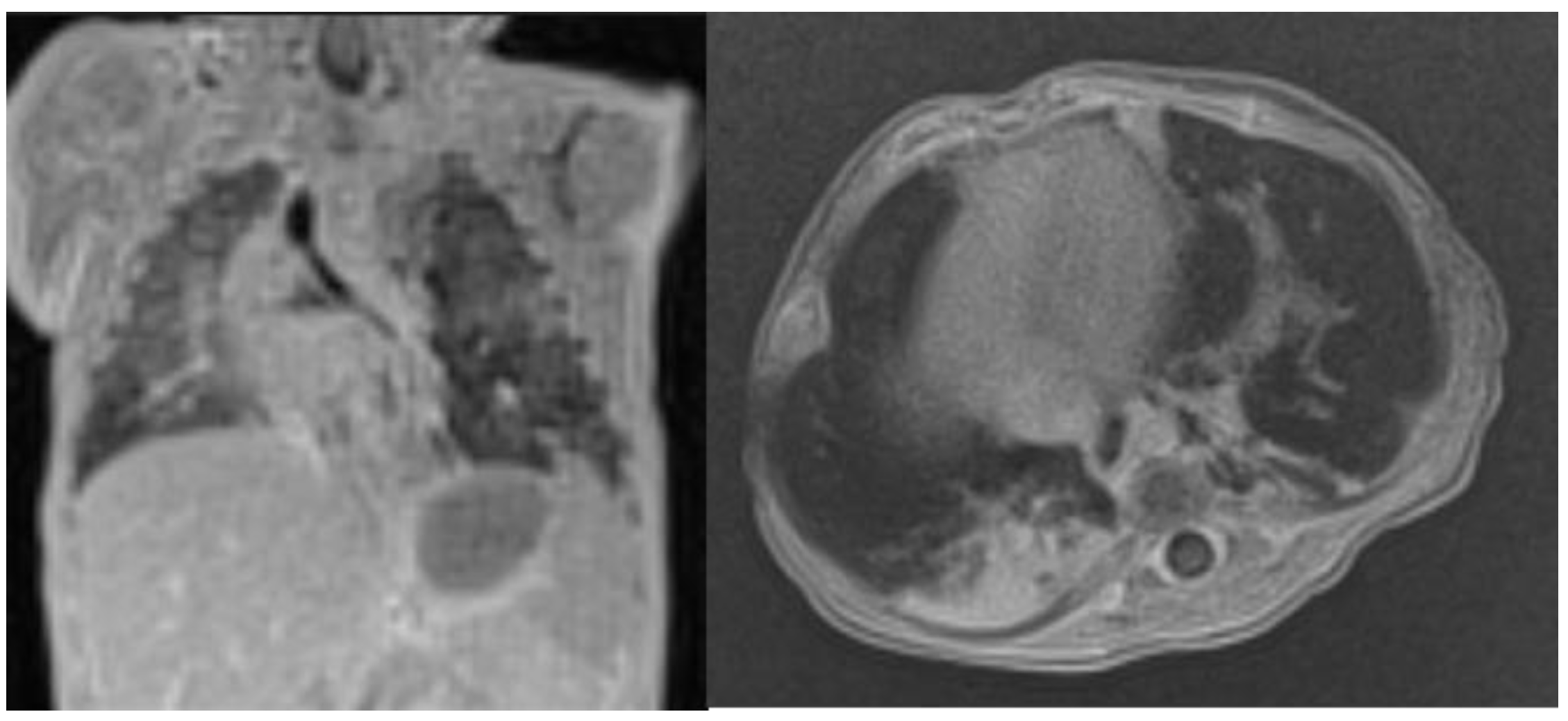
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kunisaki, S.M. Narrative review of congenital lung lesions. Transl. Pediatr. 2021, 10, 1418–1431. [Google Scholar] [CrossRef]
- Kotecha, S.; Barbato, A.; Bush, A.; Claus, F.; Davenport, M.; Delacourt, C.; Deprest, J.; Eber, E.; Frenckner, B.; Greenough, A.; et al. Antenatal and Postnatal Management of Congenital Cystic Adenomatoid Malformation. Paediatr. Respir. Rev. 2012, 13, 162–171. [Google Scholar] [CrossRef]
- Stocker, J.T. Congenital pulmonary airway malformation—A new name for and an expanded classification of congenital cystic adenomatoid malformation of the lung. Histopathology 2002, 41, 424–430. [Google Scholar]
- Ali, M.; Tank, N.; Bawa, M. Antenatally Detected Thoracic Lesions: Prognosis, Management and Outcome. Afr. J. Paediatr. Surg. 2023, 21, 117–122. [Google Scholar] [CrossRef]
- Alamo, L.; Reinberg, O.; Vial, Y.; Gudinchet, F.; Meuli, R. Comparison of foetal US and MRI in the characterisation of congenital lung anomalies. Eur. J. Radiol. 2013, 82, e860–e866. [Google Scholar] [CrossRef]
- Leblanc, C.; Baron, M.; Desselas, E.; Phan, M.H.; Rybak, A.; Thouvenin, G.; Lauby, C.; Irtan, S. Congenital pulmonary airway malformations: State-of-the-art review for pediatrician’s use. Eur. J. Pediatr. 2017, 176, 1559–1571. [Google Scholar] [CrossRef] [PubMed]
- Kersten, C.M.; Hermelijn, S.M.; Mullassery, D.; Muthialu, N.; Cobanoglu, N.; Gartner, S.; Bagolan, P.; Burgos, C.M.; Sgrò, A.; Heyman, S.; et al. The Management of Asymptomatic Congenital Pulmonary Airway Malformation: Results of a European Delphi Survey. Children 2022, 9, 1153. [Google Scholar] [CrossRef] [PubMed]
- Abusalah, Z.G.; Shehab, M.; Abdalla, A.; Nakib, G.N. Postnatally presented and spontaneously resolved congenital pulmonary airway malformation in a preterm baby. BMJ Case Rep. 2019, 12, e229746. [Google Scholar] [CrossRef]
- Ottomeyer, M.; Huddleston, C.; Berkovich, R.M.; Brink, D.S.; Koenig, J.M.; Sobush, K.T. Early resection of a rare congenital pulmonary airway malformation causing severe progressive respiratory distress in a preterm neonate: A case report and review of the literature. BMC Pediatr. 2023, 23, 238. [Google Scholar] [CrossRef]
- Fogarty, M.; Osborn, D.A.; Askie, L.; Seidler, A.L.; Hunter, K.; Lui, K.; Simes, J.; Tarnow-Mordi, W. Delayed vs early umbilical cord clamping for preterm infants: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2018, 218, 1–18. [Google Scholar] [CrossRef]
- Gornall, A.S.; Budd, J.L.S.; Draper, E.S.; Konje, J.C.; Kurinczuk, J.J. Congenital cystic adenomatoid malformation: Accuracy of prenatal diagnosis, prevalence and outcome in a general population. Prenat. Diagn. 2003, 23, 997–1002. [Google Scholar] [CrossRef]
- Ehrenberg-Buchner, S.; Stapf, A.M.; Berman, D.R.; Drongowski, R.A.; Mychaliska, G.B.; Treadwell, M.C.; Kunisaki, S.M. Fetal lung lesions: Can we start to breathe easier? Am. J. Obstet. Gynecol. 2013, 208, 151.e1–151.e7. [Google Scholar] [CrossRef]
- Pederiva, F.; Rothenberg, S.S.; Hall, N.; Ijsselstijn, H.; Wong, K.K.Y.; von der Thüsen, J.; Ciet, P.; Achiron, R.; D’adamo, A.P.; Schnater, J.M. Congenital lung malformations. Nat. Rev. Dis. Prim. 2023, 9, 60. [Google Scholar] [CrossRef]
- Mehl, S.C.; Short, W.D.; Kinley, A.; Olutoye, O.O., II; Lee, T.C.; Keswani, S.G.; King, A. Maternal steroids in high-risk congenital lung malformations. J. Surg. Res. 2022, 280, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Baumgarten, H.D.; Flake, A.W. Fetal Surgery. Pediatr. Clin. N. Am. 2019, 66, 295–308. [Google Scholar] [CrossRef] [PubMed]
- Bose, S.K.; Stratigis, J.D.; Ahn, N.; Pogoriler, J.; Hedrick, H.L.; Rintoul, N.E.; Peranteau, W.H. Prenatally diagnosed large lung lesions: Timing of resection and perinatal outcomes. J. Pediatr. Surg. 2023, 58, 2384–2390. [Google Scholar] [CrossRef]
- Montgomery, A.; Peiffer, S.; Mehl, S.; Lee, T.C.; Keswani, S.G.; King, A. Management and Outcomes of Patients with High-Risk (Congenital Lung Malformation Volume Ratio ≥ 1.6) Congenital Lung Malformations. J. Surg. Res. 2024, 295, 559–566. [Google Scholar] [CrossRef]
- MacGillivray, T.E.; Harrison, M.R.; Goldstein, R.B.; Adzick, N.S. Disappearing fetal lung lesions. J. Pediatr. Surg. 1993, 28, 1321–1325. [Google Scholar] [CrossRef]
- Lima, J.S.; Camargos, P.A.M.; Aguiar, R.A.L.P.; Campos, A.S.; Aguiar, M.J.B. Pre and perinatal aspects of congenital cystic adenomatoid malformation of the lung. J. Matern. Neonatal Med. 2014, 27, 228–232. [Google Scholar] [CrossRef]
- Kunisaki, S.M.; Ehrenberg-Buchner, S.; Dillman, J.R.; Smith, E.A.; Mychaliska, G.B.; Treadwell, M.C. Vanishing fetal lung malformations: Prenatal sonographic characteristics and postnatal outcomes. J. Pediatr. Surg. 2015, 50, 978–982. [Google Scholar] [CrossRef]
- Meizner, I.; Rosenak, D. The vanishing fetal intrathoracic mass: Consider an obstructing mucous plug. Ultrasound Obstet. Gynecol. 1995, 5, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Crombleholme, T.M.; Coleman, B.; Hedrick, H.; Liechty, K.; Howell, L.; Flake, A.W.; Johnson, M.; Adzick, N. Cystic adenomatoid malformation volume ratio predicts outcome in prenatally diagnosed cystic adenomatoid malformation of the lung. J. Pediatr. Surg. 2002, 37, 331–338. [Google Scholar] [CrossRef]
- Pogoriler, J.; Swarr, D.; Kreiger, P.; Adzick, N.S.; Peranteau, W. Congenital Cystic Lung Lesions: Redefining the Natural Distribution of Subtypes and Assessing the Risk of Malignancy. Am. J. Surg. Pathol. 2019, 43, 47–55. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stocker, J.T. Cystic Lung Disease in Infants and Children. Fetal Pediatr. Pathol. 2009, 28, 155–184. [Google Scholar] [CrossRef]
- Lezmi, G.; Hadchouel, A.; Khen-Dunlop, N.; Vibhushan, S.; Benachi, A.; Delacourt, C. Congenital cystic adenomatoid malformations of the lung: Diagnosis, treatment, pathophysiological hypothesis. Rev. Pneumol. Clin. 2013, 69, 190–197. [Google Scholar] [CrossRef]
- Prendergast, B.; Fernando, A.M.R.; Mankad, P.S. Congenital cystic adenoid malformation in a pre-term infant: Management considerations. Pediatr. Surg. Int. 1998, 14, 92–93. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, R.; Ali, H.; Harigopal, S. Persistent pulmonary interstitial emphysema presenting as solitary lung cyst in a preterm infant. BMJ Case Rep. 2012, 2012, bcr2012007516. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Balegar, V.K.K.; Barr, P.A.; McCauley, J.C.; Thomas, G. Selective bronchial intubation in a preterm infant with congenital cystic adenomatoid malformation and pulmonary air leak syndrome. J. Paediatr. Child Health 2013, 49, E93–E96. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, P.; Goergen, S.; Robinson, A.; Moghimi, A.; Malhotra, A. Bilateral congenital pulmonary airway malformation in an extremely preterm infant. BMJ Case Rep. 2021, 14, e242228. [Google Scholar] [CrossRef]

| Referral | Prenatal Findings | GW at Birth | Respiratory Symptoms at Birth | Surgical Neonatal Intervention | Type of Surgery/Histology | Outcome | |
|---|---|---|---|---|---|---|---|
| Case 1 | Prendergast et al., 1998 [26] | No | 29 | Yes | Yes | Pneumonectomy/CCAm type 3 | Alive |
| Case 2 | Srinivasan et al., 2012 [27] | No | 23 + 4, twin | Yes | Yes | Wedge resection/PPIE | Alive |
| Case 3 | Balegar et al., 2012 [28] | Yes | 28 | Yes | Yes | Wedge resection/CCAM type 1 | Alive |
| Case 4 | Abusalah et al., 2019 [8] | No | 28 + 1, twin | Yes | No | − | Alive |
| Case 5 | Chandrasekaran et al., 2021 [29] | Yes | 26 + 1 | Yes | No | CCAM type 3 | Dead |
| Case 6 | Ottomeyer et al., 2023 [9] | No | 28 | Yes | Yes | Lobectomy/CCAM type 3 | Alive |
| Present case | This study | No | 28 + 4 | Yes | No | − | Alive |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertolino, A.; Bertolo, S.; Lago, P.; Midrio, P. Congenital Pulmonary Airway Malformation in Preterm Infants: A Case Report and Review of the Literature. Life 2024, 14, 990. https://doi.org/10.3390/life14080990
Bertolino A, Bertolo S, Lago P, Midrio P. Congenital Pulmonary Airway Malformation in Preterm Infants: A Case Report and Review of the Literature. Life. 2024; 14(8):990. https://doi.org/10.3390/life14080990
Chicago/Turabian StyleBertolino, Alessia, Silvia Bertolo, Paola Lago, and Paola Midrio. 2024. "Congenital Pulmonary Airway Malformation in Preterm Infants: A Case Report and Review of the Literature" Life 14, no. 8: 990. https://doi.org/10.3390/life14080990
APA StyleBertolino, A., Bertolo, S., Lago, P., & Midrio, P. (2024). Congenital Pulmonary Airway Malformation in Preterm Infants: A Case Report and Review of the Literature. Life, 14(8), 990. https://doi.org/10.3390/life14080990









