The Efficacy of Early Rehabilitation Combined with Virtual Reality Training in Patients with First-Time Acute Stroke: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
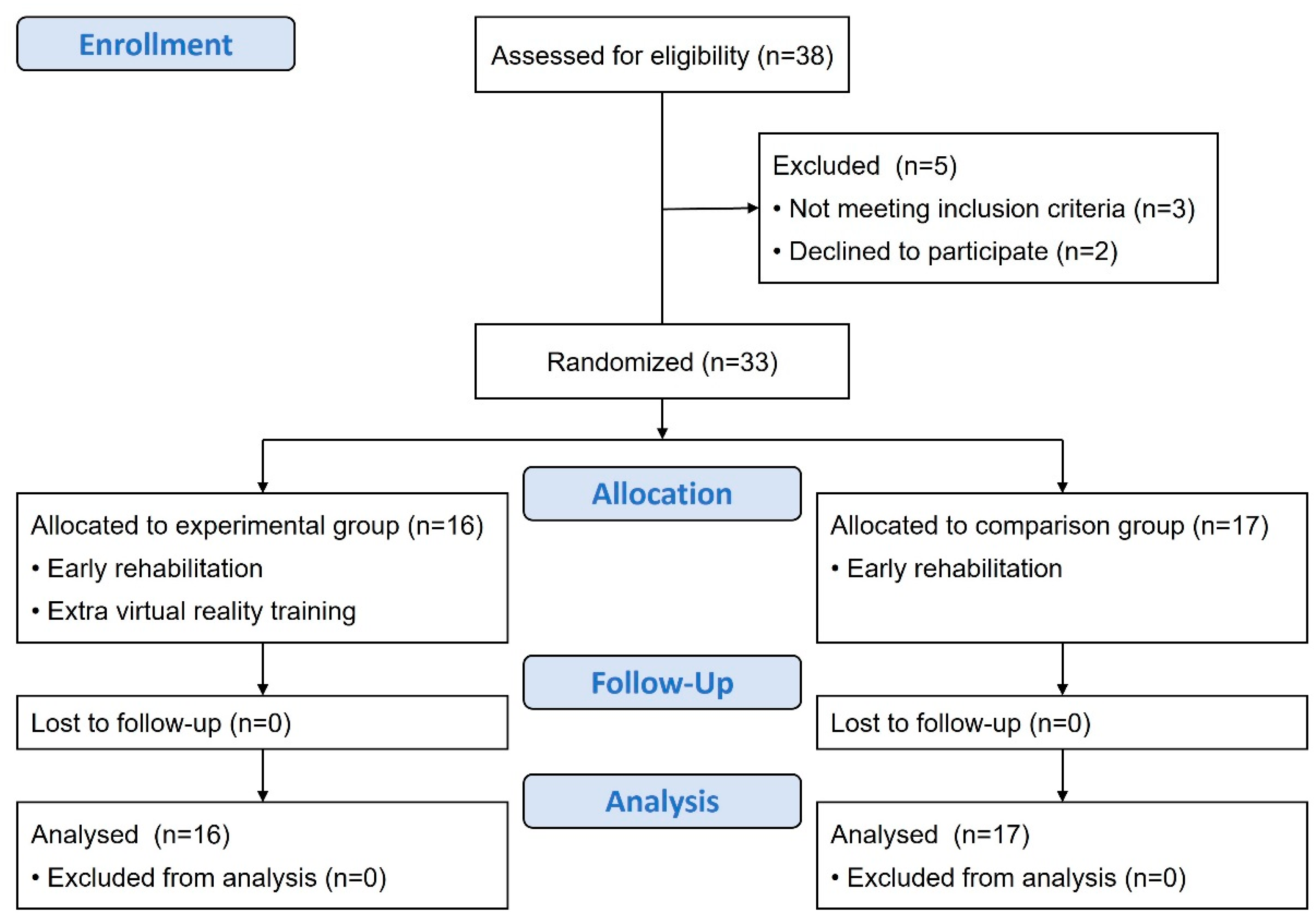
2.1. Study Design
2.2. Participants
2.3. Study Cohorts and Interventions
2.4. Measures
2.4.1. Muscle Strength
2.4.2. Functional Recovery
2.4.3. Psychological Health
2.5. Data Analysis
3. Results
3.1. Baseline Characteristics of Participants
3.2. Outcome Evaluation
3.2.1. Muscle Strength
3.2.2. Functional Recovery
3.2.3. Psychological Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Saini, V.; Guada, L.; Yavagal, D.R. Global Epidemiology of Stroke and Access to Acute Ischemic Stroke Interventions. Neurology 2021, 97, S6–S16. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, F.-I.; Chiou, H.-Y. Stroke: Morbidity, risk factors, and care in Taiwan. J. Stroke 2014, 16, 59. [Google Scholar] [CrossRef] [PubMed]
- Menon, B.; Salini, P.; Habeeba, K.; Conjeevaram, J.; Munisusmitha, K. Female caregivers and stroke severity determines caregiver stress in stroke patients. Ann. Indian Acad. Neurol. 2017, 20, 418. [Google Scholar] [CrossRef] [PubMed]
- Schöttke, H.; Giabbiconi, C.-M. Post-stroke depression and post-stroke anxiety: Prevalence and predictors. Int. Psychogeriatr. 2015, 27, 1805–1812. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Wang, C.-X.; Zhang, N.; Xiang, Y.-T.; Yang, Y.; Shi, Y.-Z.; Deng, Y.-M.; Zhu, M.-F.; Liu, F.; Yu, P. The association between post-stroke depression, aphasia, and physical independence in stroke patients at 3-month follow-up. Front. Psychiatry 2018, 9, 374. [Google Scholar] [CrossRef] [PubMed]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef]
- Jun, E.M.; Roh, Y.H.; Kim, M.J. The effect of music-movement therapy on physical and psychological states of stroke patients. J. Clin. Nurs. 2013, 22, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.-L. Efficacy of early rehabilitation therapy on movement ability of hemiplegic lower extremity in patients with acute cerebrovascular accident. Medicine 2018, 97, e9544. [Google Scholar] [CrossRef] [PubMed]
- Rethnam, V.; Langhorne, P.; Churilov, L.; Hayward, K.S.; Herisson, F.; Poletto, S.R.; Tong, Y.; Bernhardt, J. Early Mobilisation Post-Stroke: A Systematic Review and Meta-Analysis of Individual Participant Data. Disabil. Rehabil. 2022, 44, 1156–1163. [Google Scholar] [CrossRef]
- Askim, T.; Bernhardt, J.; Salvesen, Ø.; Indredavik, B. Physical activity early after stroke and its association to functional outcome 3 months later. J. Stroke. Cerebrovasc. Dis. 2014, 23, e305–e312. [Google Scholar] [CrossRef]
- Fernandes, J.B.; Fernandes, S.; Domingos, J.; Castro, C.; Romão, A.; Graúdo, S.; Rosa, G.; Franco, T.; Ferreira, A.P.; Chambino, C.; et al. Motivational strategies used by health care professionals in stroke survivors in rehabilitation: A scoping review of experimental studies. Front. Med. 2024, 11, 1384414. [Google Scholar] [CrossRef]
- Held, J.P.; Ferrer, B.; Mainetti, R.; Steblin, A.; Hertler, B.; Moreno-Conde, A.; Dueñas, A.; Pajaro, M.; Vargiu, E.; Zarco, M.J.; et al. Autonomous rehabilitation at stroke patients home for balance and gait: Safety, usability and compliance of a virtual reality system. Eur. J. Phys. Rehabil. Med. 2018, 54, 545–553. [Google Scholar] [CrossRef]
- Laver, K.E.; Lang, E.B.; George, S.; Deutsch, J.E.; Saposnik, G.; Crotty, M. Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev. 2017, 11, CD008349. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Li, D.; Liu, Y.; Wang, J.; Xiao, Q. Virtual reality for limb motor function, balance, gait, cognition and daily function of stroke patients: A systematic review and meta-analysis. J. Adv. Nurs. 2021, 77, 3255–3273. [Google Scholar] [CrossRef]
- de Rooij, I.J.; van de Port, I.G.; Punt, M.; Abbink-van Moorsel, P.J.; Kortsmit, M.; van Eijk, R.P.; Visser-Meily, J.M.; Meijer, J.-W.G. Effect of virtual reality gait training on participation in survivors of subacute stroke: A randomized controlled trial. Phys. Ther. 2021, 101, pzab051. [Google Scholar] [CrossRef]
- Corbetta, D.; Imeri, F.; Gatti, R. Rehabilitation that incorporates virtual reality is more effective than standard rehabilitation for improving walking speed, balance and mobility after stroke: A systematic review. J. Physiother. 2015, 61, 117–124. [Google Scholar] [CrossRef]
- Hao, J.; Yao, Z.; Harp, K.; Gwon, D.Y.; Chen, Z.; Siu, K.-C. Effects of virtual reality in the early-stage stroke rehabilitation: A systematic review and meta-analysis of randomized controlled trials. Physiother. Theory Pract. 2023, 39, 2569–2588. [Google Scholar] [CrossRef] [PubMed]
- Tynterova, A.; Shusharina, N.; Barantsevich, E.; Khoymov, M.; Rozhdestvensky, A. Virtual reality technology in personalized rehabilitation of patients with acute ischemic stroke. Eur. Phys. J. Spec. Top. 2024, 233, 723–731. [Google Scholar] [CrossRef]
- Lin, R.C.; Chiang, S.L.; Heitkemper, M.M.; Weng, S.M.; Lin, C.F.; Yang, F.C.; Lin, C.H. Effectiveness of early rehabilitation combined with virtual reality training on muscle strength, mood state, and functional status in patients with acute stroke: A randomized controlled trial. Worldviews Evid. Based Nurs. 2020, 17, 158–167. [Google Scholar] [CrossRef]
- Lanzoni, D.; Vitali, A.; Regazzoni, D.; Rizzi, C. Design of customized virtual reality serious games for the cognitive rehabilitation of retrograde amnesia after brain stroke. J. Comput. Inf. Sci. Eng. 2022, 22, 031009. [Google Scholar] [CrossRef]
- Castillo, J.F.V.; Vega, M.F.M.; Cardona, J.E.M.; Lopez, D.; Quiñones, L.; Gallo, O.A.H.; Lopez, J.F. Design of Virtual Reality Exergames for Upper Limb Stroke Rehabilitation Following Iterative Design Methods: Usability Study. JMIR Serious Games 2024, 12, e48900. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J. Pharmacol. Pharmacother. 2010, 1, 100–110. [Google Scholar] [CrossRef] [PubMed]
- Banks, J.L.; Marotta, C.A. Outcomes validity and reliability of the modified Rankin scale: Implications for stroke clinical trials: A literature review and synthesis. Stroke 2007, 38, 1091–1096. [Google Scholar] [CrossRef]
- Florence, J.M.; Pandya, S.; King, W.M.; Robison, J.D.; Baty, J.; Miller, J.P.; Schierbecker, J.; Signore, L.C. Intrarater reliability of manual muscle test (Medical Research Council scale) grades in Duchenne’s muscular dystrophy. Phys. Ther. 1992, 72, 115–122. [Google Scholar] [CrossRef]
- Benaim, C.; Pérennou, D.A.; Villy, J.; Rousseaux, M.; Pelissier, J.Y. Validation of a standardized assessment of postural control in stroke patients: The Postural Assessment Scale for Stroke Patients (PASS). Stroke 1999, 30, 1862–1868. [Google Scholar] [CrossRef]
- Kidd, D.; Stewart, G.; Baldry, J.; Johnson, J.; Rossiter, D.; Petruckevitch, A.; Thompson, A.J. The Functional Independence Measure: A comparative validity and reliability study. Disabil. Rehabil. 1995, 17, 10–14. [Google Scholar] [CrossRef]
- Quinn, T.J.; Langhorne, P.; Stott, D.J. Barthel index for stroke trials: Development, properties, and application. Stroke 2011, 42, 1146–1151. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Zeger, S.L.; Liang, K.-Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics 1986, 42, 121–130. [Google Scholar] [CrossRef]
- Chen, L.; Lo, W.L.; Mao, Y.R.; Ding, M.H.; Lin, Q.; Li, H.; Zhao, J.L.; Xu, Z.Q.; Bian, R.H.; Huang, D.F. Effect of Virtual Reality on Postural and Balance Control in Patients with Stroke: A Systematic Literature Review. BioMed. Res. Int. 2016, 2016, 7309272. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; Chen, Z.; Remis, A.; He, Z. Virtual Reality-Based Rehabilitation to Restore Motor Function in People with Amputation: A Systematic Literature Review. Am. J. Phys. Med. Rehabil. 2023, 102, 468–474. [Google Scholar] [CrossRef] [PubMed]
- Kiper, P.; Przysiężna, E.; Cieślik, B.; Broniec-Siekaniec, K.; Kucińska, A.; Szczygieł, J.; Turek, K.; Gajda, R.; Szczepańska-Gieracha, J. Effects of immersive virtual therapy as a method supporting recovery of depressive symptoms in post-stroke rehabilitation: Randomized controlled trial. Clin. Interv. Aging 2022, 17, 1673–1685. [Google Scholar] [CrossRef] [PubMed]
- Winter, C.; Kern, F.; Gall, D.; Latoschik, M.E.; Pauli, P.; Käthner, I. Immersive virtual reality during gait rehabilitation increases walking speed and motivation: A usability evaluation with healthy participants and patients with multiple sclerosis and stroke. J. Neuroeng. Rehabil. 2021, 18, 68. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.-S.; Cho, S.; Ku, J.; Kim, Y.; Lee, K.; Hwang, H.-J.; Paik, N.-J. Clinical Application of Virtual Reality for Upper Limb Motor Rehabilitation in Stroke: Review of Technologies and Clinical Evidence. J. Clin. Med. 2020, 9, 3369. [Google Scholar] [CrossRef] [PubMed]
- Meng, J.; Yan, Z.; Gu, F.; Tao, X.; Xue, T.; Liu, D.; Wang, Z. Transcranial direct current stimulation with virtual reality versus virtual reality alone for upper extremity rehabilitation in stroke: A meta-analysis. Heliyon 2023, 9, e12695. [Google Scholar] [CrossRef] [PubMed]
- da Silva Cameirão, M.; Bermúdez i Badia, S.; Duarte, E.; Verschure, P.F. Virtual reality based rehabilitation speeds up functional recovery of the upper extremities after stroke: A randomized controlled pilot study in the acute phase of stroke using the rehabilitation gaming system. Restor. Neurol. Neurosci. 2011, 29, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.-H.; Ryu, H.; Jang, S.H. A task-specific interactive game-based virtual reality rehabilitation system for patients with stroke: A usability test and two clinical experiments. J. NeuroEngineering Rehabil. 2014, 11, 32. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Podlasek, A.; Somaa, F. Virtual reality in post-stroke neurorehabilitation–a systematic review and meta-analysis. Top. Stroke Rehabil. 2023, 30, 53–72. [Google Scholar] [CrossRef]
- Foldvari, M.; Clark, M.; Laviolette, L.C.; Bernstein, M.A.; Kaliton, D.; Castaneda, C.; Pu, C.T.; Hausdorff, J.M.; Fielding, R.A.; Singh, M.A.F. Association of muscle power with functional status in community-dwelling elderly women. J. Gerontol. A Biol. Sci. Med. Sci. 2000, 55, M192–M199. [Google Scholar] [CrossRef]
- Chen, Y.; Niu, M.; Zhang, X.; Qian, H.; Xie, A.; Wang, X. Effects of home-based lower limb resistance training on muscle strength and functional status in stable Chronic obstructive pulmonary disease patients. J. Clin. Nurs. 2018, 27, e1022–e1037. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.; Zhu, G.; Zhang, M.; Xie, S.Q. Reviewing clinical effectiveness of active training strategies of platform-based ankle rehabilitation robots. J. Healthc. Eng. 2018, 2018, 2858294. [Google Scholar] [CrossRef]
- Lee, H.S.; Park, Y.J.; Park, S.W. The effects of virtual reality training on function in chronic stroke patients: A systematic review and meta-analysis. Biomed. Res. Int. 2019, 2019, 7595639. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, E.; Radford, K.; Grant, M.; Terry, J. Developing stroke-specific vocational rehabilitation: A soft systems analysis of current service provision. Disabil. Rehabil. 2014, 36, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Zeng, A.; Chen, Z.; Wei, Y.; Huang, K.; Chen, J.; Ren, Z. Effects of virtual reality training on upper limb function and balance in stroke patients: Systematic review and meta-meta-analysis. J. Med. Internet. Res. 2021, 23, e31051. [Google Scholar] [CrossRef] [PubMed]
- Checa, D.; Saucedo-Dorantes, J.J.; Osornio-Rios, R.A.; Antonino-Daviu, J.A.; Bustillo, A. Virtual Reality Training Application for the Condition-Based Maintenance of Induction Motors. Appl. Sci. 2022, 12, 414. [Google Scholar] [CrossRef]
- Melo, M. Virtual reality for medical training: Notes on opportunities and challenges. PsychTech Health J. 2023, 6, 1–2. [Google Scholar] [CrossRef]
| All Participants | Experimental Group (EG) | Comparison Group (CG) | t/x2 | p | |
|---|---|---|---|---|---|
| n = 33 | n = 16 | n = 17 | |||
| Age (years) | 61.5 ± 11.1 | 59.9 ± 12.8 | 63.1 ± 9.3 | 0.676 | 0.417 |
| Sex (male) | 25 (75.8) | 13 (81.2) | 12 (70.6) | 0.51 | 0.475 |
| Body mass index (kg/m2) | 25.6 ± 4.7 | 26.2 ± 4.8 | 24.9 ± 4.7 | 0.563 | 0.459 |
| Education | 3.735 | 0.443 | |||
| Under elementary school | 1 (3.0) | 0 (0) | 1 (5.9) | ||
| Elementary school | 7 (21.2) | 4 (25.0) | 3 (17.6) | ||
| Junior high school | 6 (18.2) | 3 (18.8) | 3 (17.6) | ||
| Senior high school | 7 (21.2) | 5 (31.2) | 2 (11.8) | ||
| College and above | 12 (36.4) | 4 (25.0) | 8 (47.1) | ||
| Marital status | 0.279 | 0.870 | |||
| Unmarried | 7 (21.2) | 4 (25.0) | 3 (17.6) | ||
| Married | 24 (72.7) | 11 (68.8) | 13 (76.5) | ||
| Widowed | 2 (6.1) | 1 (6.2) | 1 (5.9) | ||
| Caregiver | 6.686 | 0.153 | |||
| None | 2 (6.1) | 2 (12.5) | 0 (0) | ||
| Family members | 24 (72.7) | 12 (75.0) | 12 (70.6) | ||
| Foreigner maid | 1 (3.0) | 1 (6.2) | 0 (0) | ||
| Professional caregiver | 6 (18.2) | 1 (6.2) | 5 (29.4) | ||
| Paraside/Affected side (Right) | 19 (57.6) | 7 (43.8) | 12 (70.6) | 2.431 | 0.166 |
| Duration of stay | 17.8 ± 6.6 | 17.8 ± 6.6 | 17.9 ± 6.8 | 0.003 | 0.955 |
| Comorbidities | |||||
| Hypertension | 23 (69.7) | 11 (68.8) | 12 (70.6) | 0.013 | 1.000 |
| Type 2 diabetes | 7 (21.2) | 5 (31.2) | 2 (11.8) | 1.873 | 0.225 |
| Heart disease | 9 (27.3) | 5 (31.2) | 4 (23.5) | 0.248 | 0.708 |
| Hyperlipidemia | 23 (69.7) | 11 (68.8) | 12 (70.6) | 0.013 | 1.000 |
| Metabolic syndrome | 6 (18.2) | 4 (25.0) | 2 (11.8) | 0.971 | 0.398 |
| Discharge destination | 1.873 | 0.225 | |||
| Home | 26 (78.8) | 11 (68.8) | 15 (88.2) | ||
| Post-acute care units/Nursing home | 7 (21.2) | 5 (31.2) | 2 (11.8) |
| All (n = 33) | EG (n = 16) | CG (n = 17) | Baseline | Post-Intervention | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Baseline | After | p | Baseline | After | p | EG vs. CG | EG vs. CG | |||
| t | p | t | p | ||||||||
| Muscle strength | |||||||||||
| Affected side | |||||||||||
| Upper extremity | 3.5 ± 1.2 | 3.4 ± 1.3 | 4.3 ± 1.3 | 0.082 | 3.5 ± 1.2 | 4.1 ± 1.6 | 0.192 | 0.01 | 0.940 | 0.07 | 0.794 |
| Lower extremity | 3.8 ± 0.8 | 3.7 ± 0.6 | 4.6 ± 0.8 | 0.001 | 3.8 ± 0.9 | 4.5 ± 0.9 | 0.047 | 0.26 | 0.611 | 0.25 | 0.618 |
| Unaffected side | |||||||||||
| Upper extremity | 4.7 ± 0.5 | 4.6 ± 0.6 | 4.9 ± 0.3 | 0.034 | 4.8 ± 0.4 | 5.0 ± 0.0 | 0.073 | 2.07 | 0.160 | 1.07 | 0.310 |
| Lower extremity | 4.5 ± 0.8 | 4.5 ± 0.8 | 4.9 ± 0.5 | 0.128 | 4.5 ± 0.7 | 4.8 ± 0.4 | 0.085 | 0.01 | 0.913 | 0.11 | 0.744 |
| NHISS | 1.6 ± 1.0 | 1.7 ± 1.3 | 1.9 ± 2.2 | 0.775 | 1.5 ± 0.5 | 1.4 ± 0.5 | 0.315 | 0.22 | 0.646 | 0.88 | 0.357 |
| Depression | 10.2 ± 4.5 | 12.1 ± 1.4 | 9.2 ± 2.2 | <0.001 | 8.5 ± 5.8 | 9.2 ± 5.6 | 0.719 | 5.83 | 0.022 | 0.00 | 0.994 |
| Anxiety | 10.9 ± 5.2 | 12.5 ± 2.4 | 11.0 ± 2.3 | 0.090 | 9.4 ± 6.6 | 8.9 ± 5.8 | 0.827 | 3.20 | 0.083 | 1.83 | 0.186 |
| mRS | 3.5 ± 0.9 | 3.3 ± 0.9 | 2.7 ± 1.2 | 0.112 | 3.7 ± 0.8 | 2.5 ± 1.1 | 0.001 | 1.23 | 0.277 | 0.16 | 0.691 |
| PASS | 20.6 ± 12.0 | 21.0 ± 12.3 | 30.0 ± 8.0 | 0.020 | 20.1 ± 12.1 | 24.2 ± 12.5 | 0.336 | 0.04 | 0.837 | 2.45 | 0.128 |
| FIM | 88.2 ± 28.0 | 95.4 ± 23.5 | 108.3 ± 17.5 | 0.088 | 81.4 ± 30.9 | 94.9 ± 34.2 | 0.235 | 2.11 | 0.156 | 1.95 | 0.173 |
| Barthel Index | 46.7 ± 24.2 | 52.5 ± 23.0 | 57.2 ± 27.6 | 0.605 | 41.2 ± 24.7 | 53.5 ± 29.5 | 0.195 | 1.85 | 0.183 | 0.14 | 0.716 |
| Within Group | Between Group | Interaction Group (EG) × Time | Interaction a Group (EG) × Time | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ref: Baseline | CG vs. EG | Reference Group (CG) × Time | Reference Group (CG) × Time | |||||||||
| ß | p | ß | p | ß | 95% C.I. | p | ß | 95% C.I. | p-Adjusted a | |||
| Lower | Upper | Lower | Upper | |||||||||
| Muscle strength | ||||||||||||
| Affected side | ||||||||||||
| Upper extremity | 0.81 | 0.063 | 0.03 | 0.937 | −0.17 | −1.42 | 1.09 | 0.797 | −0.29 | −1.12 | 0.55 | 0.500 |
| Lower extremity | 0.94 | <0.001 | 0.14 | 0.592 | −0.29 | −1.05 | 0.47 | 0.456 | −0.33 | −0.88 | 0.21 | 0.232 |
| Unaffected side | ||||||||||||
| Upper extremity | 0.38 | 0.022 | 0.26 | 0.143 | −0.20 | −0.57 | 0.17 | 0.291 | −0.24 | −0.53 | 0.05 | 0.107 |
| Lower extremity | 0.38 | 0.106 | −0.03 | 0.910 | −0.02 | −0.61 | 0.57 | 0.942 | −0.09 | −0.46 | 0.29 | 0.642 |
| NHISS | 0.19 | 0.766 | −0.16 | 0.640 | −0.36 | −1.64 | 0.91 | 0.576 | −0.47 | −1.34 | 0.39 | 0.286 |
| Depression | −2.88 | <0.001 | −3.59 | 0.01 | 3.58 | −0.32 | 7.48 | 0.072 | 3.77 | 0.87 | 6.67 | 0.011 |
| Anxiety | −1.50 | 0.070 | −3.15 | 0.059 | 1.03 | −3.35 | 5.41 | 0.645 | 1.03 | −1.72 | 3.78 | 0.463 |
| mRS | −0.63 | 0.090 | 0.34 | 0.256 | −0.49 | −1.44 | 0.45 | 0.308 | −0.50 | −1.09 | 0.10 | 0.100 |
| PASS | 9.00 | 0.011 | −0.88 | 0.830 | −4.88 | −15.50 | 5.74 | 0.367 | −4.62 | −11.2 | 1.93 | 0.167 |
| FIM | 12.9 | 0.069 | −14.0 | 0.130 | 0.65 | −24.7 | 26.0 | 0.960 | −0.91 | −15.5 | 13.7 | 0.903 |
| Barthel Index | 4.7 | 0.590 | −11.3 | 0.159 | 7.67 | −16.9 | 32.3 | 0.541 | 8.52 | −10.3 | 27.3 | 0.374 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chao, T.-C.; Lin, C.-H.; Lee, M.-S.; Chang, C.-C.; Lai, C.-Y.; Huang, C.-Y.; Chang, W.-Y.; Chiang, S.-L. The Efficacy of Early Rehabilitation Combined with Virtual Reality Training in Patients with First-Time Acute Stroke: A Randomized Controlled Trial. Life 2024, 14, 847. https://doi.org/10.3390/life14070847
Chao T-C, Lin C-H, Lee M-S, Chang C-C, Lai C-Y, Huang C-Y, Chang W-Y, Chiang S-L. The Efficacy of Early Rehabilitation Combined with Virtual Reality Training in Patients with First-Time Acute Stroke: A Randomized Controlled Trial. Life. 2024; 14(7):847. https://doi.org/10.3390/life14070847
Chicago/Turabian StyleChao, Ta-Chung, Chia-Huei Lin, Meei-Shyuan Lee, Cheng-Chiang Chang, Chia-Ying Lai, Chien-Yao Huang, Wen-Yuan Chang, and Shang-Lin Chiang. 2024. "The Efficacy of Early Rehabilitation Combined with Virtual Reality Training in Patients with First-Time Acute Stroke: A Randomized Controlled Trial" Life 14, no. 7: 847. https://doi.org/10.3390/life14070847
APA StyleChao, T.-C., Lin, C.-H., Lee, M.-S., Chang, C.-C., Lai, C.-Y., Huang, C.-Y., Chang, W.-Y., & Chiang, S.-L. (2024). The Efficacy of Early Rehabilitation Combined with Virtual Reality Training in Patients with First-Time Acute Stroke: A Randomized Controlled Trial. Life, 14(7), 847. https://doi.org/10.3390/life14070847









