Sleep Difficulties in Swiss Elite Athletes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Procedure
2.3. Measures
2.4. Statistics
3. Results
4. Discussion
- 18% of Swiss top athletes have poor sleep health, in line with data from other nations (Canada, USA) tested with the same instrument.
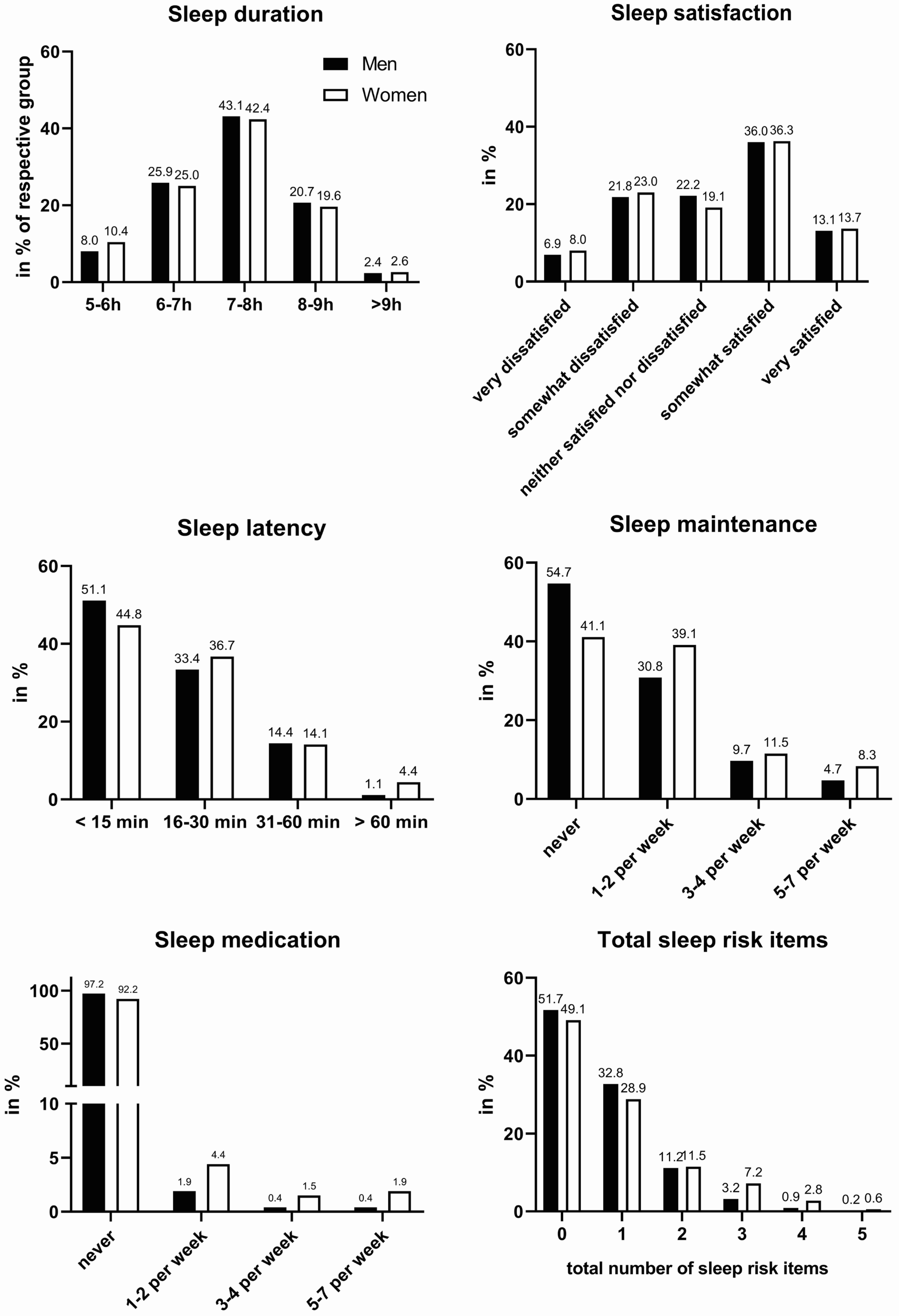
- Female athletes are more prone to sleep problems, reporting a longer duration of falling asleep, more frequent troubles maintaining sleep, and a doubled use of sleep medication.
- Poor sleep health is linked to inferior mental health. Self-reported sleep duration was most sensitively linked to depressive symptoms and symptoms of anxiety disorder.
- Screening and treating sleep disorders might effectively improve mental health, general well-being, as well as performance among athletes around the globe. Effective screening instruments have to be developed.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Watson, A.M. Sleep and Athletic Performance. Curr. Sports Med. Rep. 2017, 16, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Vorster, A.; Erlacher, D.; Barrazoni, F.; Hossner, E.-J.; Bassetti, C. Schlafprobleme im Leistungssport. Swiss Med. Forum 2022, 22, 198–203. [Google Scholar] [CrossRef]
- McMorris, T.; Graydon, J. The effect of exercise on cognitive performance in soccer-specific tests. J. Sports Sci. 1997, 15, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Royal, K.A.; Farrow, D.; Mujika, I.; Halson, S.L.; Pyne, D.; Abernethy, B. The effects of fatigue on decision making and shooting skill performance in water polo players. J. Sports Sci. 2006, 24, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Birrer, D.; Morgan, G. Psychological skills training as a way to enhance an athlete’s performance in high-intensity sports. Scand. J. Med. Sci. Sports 2010, 20, 78–87. [Google Scholar] [CrossRef] [PubMed]
- Skein, M.; Duffield, R.; Edge, J.; Short, M.J.; Mündel, T. Intermittent-Sprint Performance and Muscle Glycogen after 30 h of Sleep Deprivation. Med. Sci. Sports Exerc. 2011, 43, 1301–1311. [Google Scholar] [CrossRef] [PubMed]
- Dáttilo, M.; Antunes, H.K.M.; Galbes, N.M.N.; Mônico-Neto, M.; De Sá Souza, H.; Dos Santos Quaresma, M.V.L.; Lee, K.S.; Ugrinowitsch, C.; Tufik, S.; De Mello, M.T. Effects of Sleep Deprivation on Acute Skeletal Muscle Recovery after Exercise. Med. Sci. Sports Exerc. 2020, 52, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Gupta, L.; Morgan, K.; Gilchrist, S. Does elite sport degrade sleep quality? A systematic review. Sports Med. 2017, 47, 1317–1333. [Google Scholar] [CrossRef] [PubMed]
- Tuomilehto, H.; Vuorinen, V.-P.; Penttilä, E.; Kivimäki, M.; Vuorenmaa, M.; Venojärvi, M.; Airaksinen, O.; Pihlajamäki, J. Sleep of professional athletes: Underexploited potential to improve health and performance. J. Sports Sci. 2017, 35, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Doherty, R.; Madigan, S.M.; Nevill, A.; Warrington, G.; Ellis, J.G. The Sleep and Recovery Practices of Athletes. Nutrients 2021, 13, 1330. [Google Scholar] [CrossRef] [PubMed]
- Walsh, N.P.; Halson, S.L.; Sargent, C.; Roach, G.D.; Nédélec, M.; Gupta, L.; Leeder, J.; Fullagar, H.H.; Coutts, A.J.; Edwards, B.J.; et al. Sleep and the athlete: Narrative review and 2021 expert consensus recommendations. Br. J. Sports Med. 2021, 55, 356–368. [Google Scholar] [CrossRef] [PubMed]
- Birrer, D. Sleep hygiene of Olympic Games participants. In Proceedings of the Sleep-Wake-Epilepsy Days 2022, Bern, Switzerland, 2 November 2022. [Google Scholar]
- Drew, M.; Vlahovich, N.; Hughes, D.; Appaneal, R.; Burke, L.M.; Lundy, B.; Rogers, M.; Toomey, M.; Watts, D.; Lovell, G.; et al. Prevalence of illness, poor mental health and sleep quality and low energy availability prior to the 2016 Summer Olympic Games. Br. J. Sports Med. 2018, 52, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Duffield, R.; Fowler, P. Domestic and International Travel: Implications for performance and recovery in team-sport athletes. In Sport, Recovery, and Performance: Interdisciplinary Insights; Kellmann, M., Beckmann, J., Eds.; Routledge: Abingdon, UK, 2018; pp. 183–197. ISBN 978-1-138-28777-8. [Google Scholar]
- Ehrlenspiel, F.; Erlacher, D.; Ziegler, M. Changes in Subjective Sleep Quality Before a Competition and Their Relation to Competitive Anxiety. Behav. Sleep Med. 2018, 16, 553–568. [Google Scholar] [CrossRef] [PubMed]
- Fullagar, H.H.K.; Skorski, S.; Duffield, R.; Julian, R.; Bartlett, J.; Meyer, T. Impaired sleep and recovery after night matches in elite football players. J. Sports Sci. 2016, 34, 1333–1339. [Google Scholar] [CrossRef] [PubMed]
- Erlacher, D.; Schredl, M.; Lakus, G. Subjective sleep quality prior to home and away games for female volleyball players. Int. J. Dream Res. 2009, 2, 70–72. [Google Scholar]
- Brown, G.A.; Veith, S.; Sampson, J.A.; Whalan, M.; Fullagar, H.H.K. Influence of Training Schedules on Objective Measures of Sleep in Adolescent Academy Football Players. J. Strength Cond. Res. 2020, 34, 2515. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M.; Kellmann, M.; Lang, C.; Brand, S.; Gygax, B.; Ludyga, S.; Müller, C.; Ramseyer, S.; Jakowski, S. Potential Prevalence, Pattern, and Risk Factors of Insomnia Symptoms in Adolescent Elite Athletes. Z. Sportpsychol. 2022, 29, 42–61. [Google Scholar] [CrossRef]
- Dumortier, J.; Mariman, A.; Boone, J.; Delesie, L.; Tobback, E.; Vogelaers, D.; Bourgois, J.G. Sleep, training load and performance in elite female gymnasts. Eur. J. Sport Sci. 2018, 18, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Hausswirth, C.; Louis, J.; Aubry, A.; Bonnet, G.; Duffield, R.; Le Meur, Y. Evidence of Disturbed Sleep and Increased Illness in Overreached Endurance Athletes. Med. Sci. Sports Exerc. 2014, 46, 1036–1045. [Google Scholar] [CrossRef]
- Kellmann, M.; Bertollo, M.; Bosquet, L.; Brink, M.; Coutts, A.J.; Duffield, R.; Erlacher, D.; Halson, S.L.; Hecksteden, A.; Heidari, J.; et al. Recovery and Performance in Sport: Consensus Statement. Int. J. Sports Physiol. Perform. 2018, 13, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Samuels, C.H.; James, L.; Lawson, D.; Meeuwisse, W. The Athlete Sleep Screening Questionnaire: A new tool for assessing and managing sleep in elite athletes. Br. J. Sports Med. 2016, 50, 418. [Google Scholar] [CrossRef] [PubMed]
- Bender, A.M.; Lawson, D.; Werthner, P.; Samuels, C.H. The Clinical Validation of the Athlete Sleep Screening Questionnaire: An Instrument to Identify Athletes that Need Further Sleep Assessment. Sports Med.-Open 2018, 4, 23. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Bender, A.; Tan, X.; Wang, X.; Le, S.; Cheng, S. Assessment of sleep disturbances with the athlete sleep screening questionnaire in Chinese athletes. Sports Med. Health Sci. 2022, 4, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Rabin, J.M.; Mehra, R.; Chen, E.; Ahmadi, R.; Jin, Y.; Day, C. Assessment of sleep health in collegiate athletes using the Athlete Sleep Screening Questionnaire. J. Clin. Sleep Med. 2020, 16, 1349–1356. [Google Scholar] [CrossRef] [PubMed]
- Röthlin, P.; Horvath, S.; Ackeret, N.; Peter, C.; Birrer, D. The Mental Health of Swiss Elite Athletes. Swiss Psychol. Open Off. J. Swiss Psychol. Soc. 2023, 3, 2. [Google Scholar] [CrossRef]
- Torstveit, M.K.; Sundgot-Borgen, J. The Female Athlete Triad: Are Elite Athletes at Increased Risk? Med. Sci. Sports Exerc. 2005, 37, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J. Sleep Health: Can We Define It? Does It Matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Fan, M.; Sun, D.; Zhou, T.; Heianza, Y.; Lv, J.; Li, L.; Qi, L. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: A prospective study of 385 292 UK biobank participants. Eur. Heart J. 2020, 41, 1182–1189. [Google Scholar] [CrossRef] [PubMed]
- Carballeira, Y.; Dumont, P.; Borgacci, S.; Rentsch, D.; de Tonnac, N.; Archinard, M.; Andreoli, A. Criterion validity of the French version of Patient Health Questionnaire (PHQ) in a hospital department of internal medicine. Psychol. Psychother. Theory Res. Pract. 2007, 80, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Gräfe, K.; Zipfel, S.; Herzog, W.; Löwe, B. Screening psychischer Störungen mit dem “Gesundheitsfragebogen für Patienten (PHQ-D)”: Ergebnisse der deutschen Validierungsstudie. [Screening for psychiatric disorders with the Patient Health Questionnaire (PHQ). Results from the German validation study.]. Diagnostica 2004, 50, 171–181. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Hinz, A.; Klein, A.M.; Brähler, E.; Glaesmer, H.; Luck, T.; Riedel-Heller, S.G.; Wirkner, K.; Hilbert, A. Psychometric evaluation of the Generalized Anxiety Disorder Screener GAD-7, based on a large German general population sample. J. Affect. Disord. 2017, 210, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Micoulaud-Franchi, J.-A.; Lagarde, S.; Barkate, G.; Dufournet, B.; Besancon, C.; Trébuchon-Da Fonseca, A.; Gavaret, M.; Bartolomei, F.; Bonini, F.; McGonigal, A. Rapid detection of generalized anxiety disorder and major depression in epilepsy: Validation of the GAD-7 as a complementary tool to the NDDI-E in a French sample. Epilepsy Behav. 2016, 57, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Woodward, M. Epidemiology: Study Design and Data Analysis, 3rd ed.; Chapman and Hall/CRC: New York, NY, USA, 2013; ISBN 978-0-429-19626-3. [Google Scholar]
- Doré, I.; O’Loughlin, J.L.; Sabiston, C.M.; Fournier, L. Psychometric Evaluation of the Mental Health Continuum–Short Form in French Canadian Young Adults. Can. J. Psychiatry 2017, 62, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Lamers, S.M.A.; Westerhof, G.J.; Bohlmeijer, E.T.; ten Klooster, P.M.; Keyes, C.L.M. Evaluating the psychometric properties of the mental health Continuum-Short Form (MHC-SF). J. Clin. Psychol. 2011, 67, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Żemojtel-Piotrowska, M.; Piotrowski, J.P.; Osin, E.N.; Cieciuch, J.; Adams, B.G.; Ardi, R.; Bălţătescu, S.; Bogomaz, S.; Bhomi, A.L.; Clinton, A.; et al. The mental health continuum-short form: The structure and application for cross-cultural studies–A 38 nation study. J. Clin. Psychol. 2018, 74, 1034–1052. [Google Scholar] [CrossRef] [PubMed]
- Baglioni, C.; Nanovska, S.; Regen, W.; Spiegelhalder, K.; Feige, B.; Nissen, C.; Reynolds, C.F.; Riemann, D. Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychol. Bull. 2016, 142, 969–990. [Google Scholar] [CrossRef] [PubMed]
- Schaal, K.; Tafflet, M.; Nassif, H.; Thibault, V.; Pichard, C.; Alcotte, M.; Guillet, T.; Helou, N.E.; Berthelot, G.; Simon, S.; et al. Psychological Balance in High Level Athletes: Gender-Based Differences and Sport-Specific Patterns. PLoS ONE 2011, 6, e19007. [Google Scholar] [CrossRef] [PubMed]
- Kocevska, D.; Lysen, T.S.; Dotinga, A.; Koopman-Verhoeff, M.E.; Luijk, M.P.C.M.; Antypa, N.; Biermasz, N.R.; Blokstra, A.; Brug, J.; Burk, W.J.; et al. Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: A systematic review and meta-analysis. Nat. Hum. Behav. 2021, 5, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Sargent, C.; Lastella, M.; Halson, S.L.; Roach, G.D. How Much Sleep Does an Elite Athlete Need? Int. J. Sports Physiol. Perform. 2021, 16, 1746–1757. [Google Scholar] [CrossRef] [PubMed]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2016, 12, 785–786. [Google Scholar] [CrossRef] [PubMed]
- Whitworth-Turner, C.M.; Di Michele, R.; Muir, I.; Gregson, W.; Drust, B. Training load and schedule are important determinants of sleep behaviours in youth-soccer players. Eur. J. Sport Sci. 2019, 19, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.S.H.; Teo, W.-P.; Aisbett, B.; Warmington, S.A. Extended Sleep Maintains Endurance Performance Better than Normal or Restricted Sleep. Med. Sci. Sports Exerc. 2019, 51, 2516. [Google Scholar] [CrossRef] [PubMed]
- Dekker, K.; Blanken, T.F.; Van Someren, E.J.W. Insomnia and Personality—A Network Approach. Brain Sci. 2017, 7, 28. [Google Scholar] [CrossRef]
- Costa, P.T., Jr.; Terracciano, A.; McCrae, R.R. Gender differences in personality traits across cultures: Robust and surprising findings. J. Personal. Soc. Psychol. 2001, 81, 322–331. [Google Scholar] [CrossRef] [PubMed]
- Kalmbach, D.A.; Cuamatzi-Castelan, A.S.; Tonnu, C.V.; Tran, K.M.; Anderson, J.R.; Roth, T.; Drake, C.L. Hyperarousal and sleep reactivity in insomnia: Current insights. Nat. Sci. Sleep 2018, 10, 193–201. [Google Scholar] [CrossRef]
- Hertenstein, E.; Benz, F.; Schneider, C.L.; Baglioni, C. Insomnia—A risk factor for mental disorders. J. Sleep Res. 2023, 32, e13930. [Google Scholar] [CrossRef]
- Geoffroy, P.A.; Hoertel, N.; Etain, B.; Bellivier, F.; Delorme, R.; Limosin, F.; Peyre, H. Insomnia and hypersomnia in major depressive episode: Prevalence, sociodemographic characteristics and psychiatric comorbidity in a population-based study. J. Affect. Disord. 2018, 226, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Fatima, Y.; Doi, S.A.R.; Najman, J.M.; Al Mamun, A. Continuity of sleep problems from adolescence to young adulthood: Results from a longitudinal study. Sleep Health 2017, 3, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Touchette, E.; Chollet, A.; Galéra, C.; Fombonne, E.; Falissard, B.; Boivin, M.; Melchior, M. Prior sleep problems predict internalising problems later in life. J. Affect. Disord. 2012, 143, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Soh, H.L.; Ho, R.C.; Ho, C.S.; Tam, W.W. Efficacy of digital cognitive behavioural therapy for insomnia: A meta-analysis of randomised controlled trials. Sleep Med. 2020, 75, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Caia, J.; Scott, T.J.; Halson, S.L.; Kelly, V.G. The influence of sleep hygiene education on sleep in professional rugby league athletes. Sleep Health 2018, 4, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Charest, J.; Grandner, M.A. Sleep and Athletic Performance: Impacts on Physical Performance, Mental Performance, Injury Risk and Recovery, and Mental Health. Sleep Med. Clin. 2020, 15, 41–57. [Google Scholar] [CrossRef] [PubMed]
| Sports Group | All | Men | Women | Age |
|---|---|---|---|---|
| N (%) | n (%) | n (%) | M ± SD | |
| Technical (e.g., curling, shooting) | 215 (21.4%) | 94 (43.7%) | 121 (56.3%) | 25.1 ± 10.4 |
| Endurance (e.g., road cycling) | 146 (14.5%) | 75 (51.4%) | 71 (48.6%) | 22.6 ± 7.6 |
| Aesthetic (e.g., synchronized swimming) | 31 (3.1%) | 7 (22.6%) | 24 (77.4%) | 19.4 ± 3.3 |
| Weight-class (e.g., wrestling) | 89 (8.9%) | 49 (55.1%) | 40 (44.9%) | 21.1 ± 4.9 |
| Ball game (e.g., soccer, ice hockey) | 360 (35.9%) | 171 (47.5%) | 189 (52.5%) | 19.7 ± 4.6 |
| Power (e.g., ski alpine) | 74 (7.4%) | 30 (40.5%) | 44 (59.5%) | 21.1 ± 4.1 |
| Antigravitation (e.g., climbing) | 20 (2.0%) | 9 (45.0%) | 11 (55.0%) | 20.7 ± 3.7 |
| Diverse (e.g., track athletics, pentathlon) | 69 (6.9%) | 29 (42.0%) | 40 (58.0%) | 21.3 ± 5.9 |
| Team sport | 380 (37.9%) | 185 (39.9%) | 195 (36.1%) | 20.6 ± 5.7 |
| Individual sport | 624 (62.2%) | 279 (60.1%) | 345 (63.9%) | 22.3 ± 7.7 |
| 16–17 | 328 (32.7%) | 145 (31.2%) | 183 (33.9%) | 16.6 ± 0.5 |
| 18–25 | 487 (48.5%) | 224 (48.3%) | 263 (48.7%) | 20.6 ± 2.3 |
| 26–40 | 161 (16.0%) | 84 (18.1%) | 77 (14.3%) | 29.9 ± 3.7 |
| 41–65 | 28 (2.8%) | 11 (2.4%) | 17 (3.1%) | 50.8 ± 6.0 |
| Total | 1004 (100%) | 464 (46.2%) | 540 (53.8%) | 21.6 ± 7.0 |
| Sleep Duration (ASSQ_v1) | Sleep Satisfaction (ASSQ_v2) | Sleep Latency (ASSQ_v3) | Sleep Maintenance (ASSQ_v4) | Sleep Medication (ASSQ_v5) | |
|---|---|---|---|---|---|
| During the recent past, how many hours of actual sleep did you get at night? | How satisfied/dissatisfied are you with the quality of your sleep? | During the recent past, how long has it usually taken you to fall asleep each night? | How often do you have trouble staying asleep? | During the recent past, how often have you taken medicine to help you sleep (prescribed or over-the-counter)? | |
| High-risk sleep factors (1 pt) | (4) 5 to 6 h | (4) very dissatisfied (3) somewhat dissatisfied | (3) >than 60 min (2) 31 to 60 min | (3) 5 to 7 days/week (2) 3 or 4 times/week | (3) 5 to 7 times/week (2) 3 or 4 times/week (1) 1 or 2 times/week |
| Low-risk sleep factors (0 pt) | (3) 6 to 7 h (2) 7 to 8 h (1) 8 to 9 h (0) >9 h | (2) neither satisfied nor dissatisfied (1) somewhat satisfied (0) very satisfied | (1) 16 to 30 min (0) <15 min | (1) 1 or 2 times/week (0) none | (0) none |
| n | Sleep Duration | Sleep Satisfaction | Sleep Latency | Sleep Efficiency | Sleep Medication | |
|---|---|---|---|---|---|---|
| all | 1004 | 9.3% | 29.9% | 17.1% | 17.3% | 5.5% |
| technical | 215 | 12.6% | 34.0% | 16.7% | 22.3% | 7.9% |
| endurance | 146 | 7.5% | 30.8% | 20.5% | 18.5% | 8.2% |
| aesthetic | 31 | 12.9% | 45.2% | 19.4% | 25.8% | 12.9% |
| weight-class | 89 | 10.1% | 27.0% | 12.4% | 16.9% | 4.5% |
| ball game | 360 | 9.7% | 29.7% | 16.9% | 13.6% | 2.5% |
| power | 74 | 2.7% | 18.9% | 14.9% | 13.5% | 5.4% |
| antigravitation | 20 | 0% | 25.0% | 25.0% | 5.0% | 0% |
| diverse | 69 | 7.2% | 26.1% | 17.4% | 23.2% | 7.2% |
| team | 380 | 9.7% | 27.6% | 17.6% | 13.9% | 2.6% |
| individual | 624 | 9.0% | 31.3% | 16.8% | 19.4% | 7.2% |
| 16–17 | 328 | 9.5% | 29.0% | 19.5% | 9.8% | 4.3% |
| 18–25 | 487 | 8.0% | 29.0% | 15.8% | 19.1% | 5.5% |
| 26–40 | 161 | 9.9% | 36.0% | 17.4% | 21.7% | 6.2% |
| 41–65 | 28 | 25.0% | 21.4% | 10.7% | 50.0% | 14.3% |
| Dependent Variables | Sleep Duration | Sleep Satisfaction | Sleep Latency | Sleep Efficiency | Sleep Medication |
|---|---|---|---|---|---|
| age | −0.037 ** | 0.003 | −0.008 | 0.055 ** | 0.027 |
| Gender (1 = m, 2 = f) | −0.007 | −0.101 | −0.102 | −0.455 ** | −0.966 ** |
| Overall well-being | 0.419 ** | 0.483 ** | −0.479 ** | −0.451 ** | −0.606 ** |
| Training hours (week) | 0.037 ** | −0.008 | 0.009 | 0.020 | 0.033 |
| Competitions | 0.009 * | −0.002 | −0.003 | 0.001 | 0.004 |
| Injuries (0 = n, 1 = y) | −0.072 | −0.227 | −0.202 | −0.199 | −1.078 ** |
| Technical | 0.547 * | 0.241 | 0.006 | 0.355 | 0.121 |
| Endurance | −0.541 | 0.059 | −0.186 | 0.472 | −0.011 |
| Aesthetic | 0.471 | 0.483 | 0.096 | −0.274 | 0.289 |
| Weight-class | 0.474 | 0.211 | 0.332 | 0.410 | 0.801 |
| Ball game | 0.448 | 0.062 | −0.084 | 0.372 | 1.271 * |
| Power | −0.467 | −0.526 | −0.256 | 0.488 | 1.059 |
| Antigravitation | 0.033 | 0.266 | −0.542 | 1.241 * | 16.373 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vorster, A.P.A.; Erlacher, D.; Birrer, D.; Röthlin, P. Sleep Difficulties in Swiss Elite Athletes. Life 2024, 14, 779. https://doi.org/10.3390/life14060779
Vorster APA, Erlacher D, Birrer D, Röthlin P. Sleep Difficulties in Swiss Elite Athletes. Life. 2024; 14(6):779. https://doi.org/10.3390/life14060779
Chicago/Turabian StyleVorster, Albrecht P. A., Daniel Erlacher, Daniel Birrer, and Philipp Röthlin. 2024. "Sleep Difficulties in Swiss Elite Athletes" Life 14, no. 6: 779. https://doi.org/10.3390/life14060779
APA StyleVorster, A. P. A., Erlacher, D., Birrer, D., & Röthlin, P. (2024). Sleep Difficulties in Swiss Elite Athletes. Life, 14(6), 779. https://doi.org/10.3390/life14060779







