B–NHL Cases in a Tertiary Pediatric Hematology—Oncology Department: A 20-Year Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
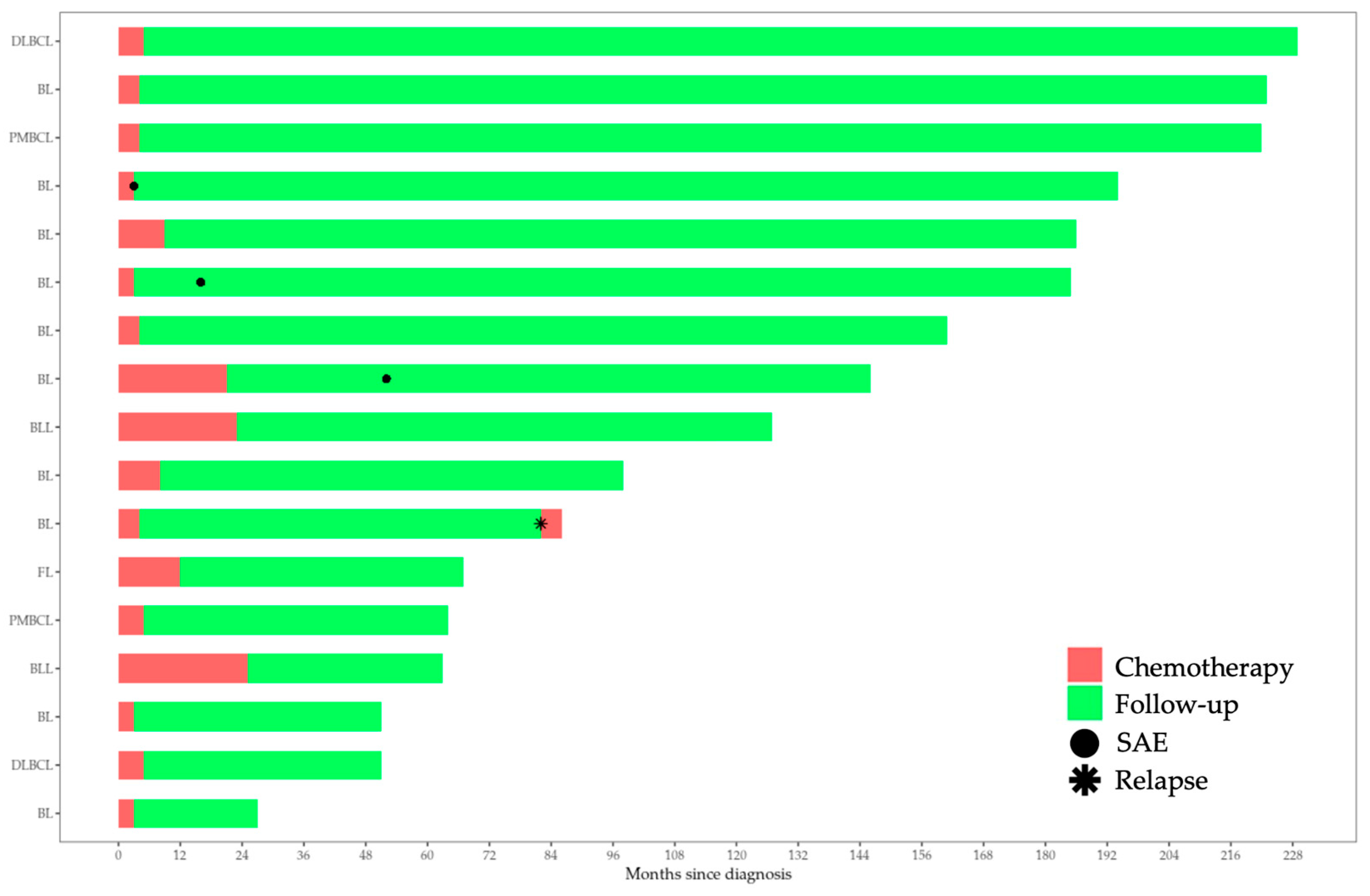
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kaatsch, P. Epidemiology of Childhood Cancer. Cancer Treat. Rev. 2010, 36, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Morton, L.M.; Wang, S.S.; Devesa, S.S.; Hartge, P.; Weisenburger, D.D.; Linet, M.S. Lymphoma Incidence Patterns by WHO Subtype in the United States, 1992–2001. Blood 2006, 107, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Rosolen, A.; Perkins, S.L.; Pinkerton, C.R.; Guillerman, R.P.; Sandlund, J.T.; Patte, C.; Reiter, A.; Cairo, M.S. Revised International Pediatric Non-Hodgkin Lymphoma Staging System. J. Clin. Oncol. 2015, 33, 2112–2118. [Google Scholar] [CrossRef] [PubMed]
- Pfister, S.M.; Reyes-Múgica, M.; Chan, J.K.C.; Hasle, H.; Lazar, A.J.; Rossi, S.; Ferrari, A.; Jarzembowski, J.A.; Pritchard-Jones, K.; Hill, D.A.; et al. A Summary of the Inaugural WHO Classification of Pediatric Tumors: Transitioning from the Optical into the Molecular Era. Cancer Discov. 2022, 12, 331–355. [Google Scholar] [CrossRef] [PubMed]
- Alaggio, R.; Amador, C.; Anagnostopoulos, I.; Attygalle, A.D.; Araujo, I.B.d.O.; Berti, E.; Bhagat, G.; Borges, A.M.; Boyer, D.; Calaminici, M.; et al. The 5th Edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia 2022, 36, 1720–1748. [Google Scholar] [CrossRef]
- Egan, G.; Goldman, S.; Alexander, S. Mature B-NHL in Children, Adolescents and Young Adults: Current Therapeutic Approach and Emerging Treatment Strategies. Br. J. Haematol. 2019, 185, 1071–1085. [Google Scholar] [CrossRef] [PubMed]
- Kyriakidis, I.; Mantadakis, E.; Stiakaki, E.; Groll, A.H.; Tragiannidis, A. Infectious Complications of Targeted Therapies in Children with Leukemias and Lymphomas. Cancers 2022, 14, 5022. [Google Scholar] [CrossRef]
- Xavier, A.C.; Suzuki, R.; Attarbaschi, A. Diagnosis and Management of Rare Paediatric Non-Hodgkin Lymphoma. Best Pract. Res. Clin. Haematol. 2023, 36, 101440. [Google Scholar] [CrossRef]
- Crump, C.; Sundquist, K.; Sieh, W.; Winkleby, M.A.; Sundquist, J. Perinatal and Family Risk Factors for Non-Hodgkin Lymphoma in Early Life: A Swedish National Cohort Study. J. Natl. Cancer Inst. 2012, 104, 923–930. [Google Scholar] [CrossRef]
- Georgakis, M.K.; Karalexi, M.A.; Agius, D.; Antunes, L.; Bastos, J.; Coza, D.; Demetriou, A.; Dimitrova, N.; Eser, S.; Florea, M.; et al. Incidence and Time Trends of Childhood Lymphomas: Findings from 14 Southern and Eastern European Cancer Registries and the Surveillance, Epidemiology and End Results, USA. Cancer Causes Control 2016, 27, 1381–1394. [Google Scholar] [CrossRef]
- SEER*Explorer Application. Available online: https://seer.cancer.gov/statistics-network/explorer/application.html?site=86&data_type=1&graph_type=2&compareBy=sex&chk_sex_1=1&chk_sex_3=3&chk_sex_2=2&rate_type=2&race=1&age_range=15&stage=101&advopt_precision=1&advopt_show_ci=on&hdn_view=1&advopt_show_apc=on&advopt_display=1#resultsRegion1 (accessed on 9 August 2023).
- Chun, G.Y.C.; Sample, J.; Hubbard, A.K.; Spector, L.G.; Williams, L.A. Trends in Pediatric Lymphoma Incidence by Global Region, Age and Sex from 1988-2012. Cancer Epidemiol. 2021, 73, 101965. [Google Scholar] [CrossRef] [PubMed]
- Reedijk, A.M.J.; Beishuizen, A.; Coebergh, J.W.W.; Hoeben, B.A.W.; Kremer, L.C.M.; Hebeda, K.M.; Pieters, R.; Loeffen, J.L.C.; Karim-Kos, H.E. Progress against Non-Hodgkin’s Lymphoma in Children and Young Adolescents in the Netherlands since 1990: Stable Incidence, Improved Survival and Lower Mortality. Eur. J. Cancer 2022, 163, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Abraham, N.; Chitsike, I.; Sylvie, C.G.L.; Kambugu, J.; Stévy, N.M.A.; Pondy, A.H.O.; Renner, L.; Parkin, D.M. Enhancing Information on Stage at Diagnosis for Childhood Cancer in Africa. Pediatr. Blood Cancer 2023, 70, e30555. [Google Scholar] [CrossRef] [PubMed]
- Gaytan-Morales, F.; Alejo-Gonzalez, F.; Reyes-Lopez, A.; Palomo, M.; Rodriguez-Romo, L.; Villareal-Martínez, L.; Sandoval-González, A.; Lopez-Facundo, A.; Tejocote-Romero, I.; Cárdenas-Cardos, R.; et al. Pediatric Mature B-Cell NHL, Early Referral and Supportive Care Problems in a Developing Country. Hematology 2019, 24, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.L.; Hahn, S.M.; Kim, H.S.; Shin, Y.J.; Kim, S.H.; Lee, Y.S.; Lyu, C.J.; Han, J.W. Symptom Interval and Patient Delay Affect Survival Outcomes in Adolescent Cancer Patients. Yonsei Med. J. 2016, 57, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.R.S.; Costa, J.T.; Breviglieri, C.N.M.; Melgares, L.M.P.; Godinho, P.R.; Metzger, M.L. Children and Adolescents with Non-Hodgkin Lymphoma in Brazil: A National Survey Identifies the Challenges Encountered and Documents the Diversity of Care. Hematol. Transfus. Cell Ther. 2023, 45 (Suppl. S2), S36–S42. [Google Scholar] [CrossRef] [PubMed]
- Petridou, E.T.; Dikalioti, S.K.; Skalkidou, A.; Andrie, E.; Dessypris, N.; Trichopoulos, D.; The Childhood Hematology-Oncology Group. Sun Exposure, Birth Weight, and Childhood Lymphomas: A Case Control Study in Greece. Cancer Causes Control 2007, 18, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, C.; Antonopoulos, C.N.; Sergentanis, T.N.; Panagopoulou, P.; Belechri, M.; Petridou, E.T. Is Birth Weight Associated with Childhood Lymphoma? A Meta-Analysis. Int. J. Cancer 2012, 130, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Rahiman, E.A.; Bakhshi, S.; Pushpam, D.; Ramamoorthy, J.; Das, A.; Ghara, N.; Kalra, M.; Kapoor, G.; Meena, J.P.; Siddaigarhi, S.; et al. Outcome and Prognostic Factors in Childhood B Non-Hodgkin Lymphoma from India: Report by the Indian Pediatric Oncology Group (InPOG-NHL-16-01 Study). Pediatr. Hematol. Oncol. 2022, 39, 391–405. [Google Scholar] [CrossRef]
- El-Mallawany, N.K.; Alexander, S.; Fluchel, M.; Hayashi, R.J.; Lowe, E.J.; Giulino-Roth, L.; Wistinghausen, B.; Hermiston, M.; Allen, C.E.; The COG NHL Committee. Children’s Oncology Group’s 2023 Blueprint for Research: Non-Hodgkin Lymphoma. Pediatr. Blood Cancer 2023, 70 (Suppl. S6), e30565. [Google Scholar] [CrossRef]
- Wang, X.-L.; Wang, X.-L.; He, S.; Zhai, H.-L. Association of Β2-Microglobulin with the Prognosis of Non-Hodgkin’s Lymphoma: A Meta Analysis. Int. J. Clin. Exp. Med. 2015, 8, 3992–3999. [Google Scholar]
- Ramadan, S.M.; Ceparano, G.; Cignetti, A.; Sammassimo, S.; Bagnardi, V.; Pagan, E.; Gottardi, D.; Fiori, S.; Passerini, R.; Radice, T.; et al. Prognostic Impact of the Baseline Immunologic Profile in Patients with Aggressive B Non-Hodgkin Lymphomas. Blood 2019, 134, 1522. [Google Scholar] [CrossRef]
- Lin, Y.; Gustafson, M.P.; Bulur, P.A.; Gastineau, D.A.; Witzig, T.E.; Dietz, A.B. Immunosuppressive CD14+HLA-DRlow/− Monocytes in B-Cell Non-Hodgkin Lymphoma. Blood 2011, 117, 872–881. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Wu, X.; Liu, X.; Yang, P.; Xu, J.; Chai, Y.; Guo, Q.; Wang, Z.; Zhang, L. Prognostic Significance of Monocytes and Monocytic Myeloid-Derived Suppressor Cells in Diffuse Large B-Cell Lymphoma Treated with R-CHOP. Cell Physiol. Biochem. 2016, 39, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Cheng, L.; Yang, S.; Liu, Y.; Zhu, Z. iTRAQ-Based Proteomic Analysis Reveals Potential Serum Biomarkers for Pediatric Non-Hodgkin’s Lymphoma. Front. Oncol. 2022, 12, 848286. [Google Scholar] [CrossRef] [PubMed]
- Valkovic, T.; Gasic, V.; Nacinovic-Duletic, A. Multiple Myeloma Index for Risk of Infection. J. Cancer 2018, 9, 2211–2214. [Google Scholar] [CrossRef] [PubMed]
- Planinc-Peraica, A.; Kolonić, S.O.; Radić-Kristo, D.; Dominis, M.; Jaksić, B. Serum Immunoglobulins in Non-Hodgkin’s Lymphoma Patients. Coll. Antropol. 2010, 34, 407–411. [Google Scholar] [PubMed]
- Haddouche, M.; Meziane, W.; Hadjidj, Z.; Mesli, N.; Aribi, M. Clinical Association of Baseline Levels of Conjugated Dienes in Low-Density Lipoprotein and Nitric Oxide with Aggressive B-Cell Non-Hodgkin Lymphoma and Their Relationship with Immunoglobulins and Th1-to-Th2 Ratio. J. Blood Med. 2016, 7, 111–119. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Roy Moulik, N.; Singh Arora, R. Immunisation in Children with Cancer Treated with Standard Dose Chemotherapy- Review of Evidence. Pediatr. Hematol. Oncol. J. 2020, 5, 89–95. [Google Scholar] [CrossRef]
- Kyriakidis, I.; Vasileiou, E.; Rossig, C.; Roilides, E.; Groll, A.H.; Tragiannidis, A. Invasive Fungal Diseases in Children with Hematological Malignancies Treated with Therapies That Target Cell Surface Antigens: Monoclonal Antibodies, Immune Checkpoint Inhibitors and CAR T-Cell Therapies. J. Fungi 2021, 7, 186. [Google Scholar] [CrossRef]
- Samochatova, E.V.; Maschan, A.A.; Shelikhova, L.N.; Myakova, N.V.; Belogurova, M.B.; Khlebnikova, O.P.; Shamardina, A.V.; Ryskal, O.V.; Roumiantseva, J.V.; Konovalov, D.M.; et al. Therapy of Advanced-Stage Mature B-Cell Lymphoma and Leukemia in Children and Adolescents with Rituximab and Reduced Intensity Induction Chemotherapy (B-NHL 2004M Protocol): The Results of a Multicenter Study. J. Pediatr. Hematol. Oncol. 2014, 36, 395–401. [Google Scholar] [CrossRef]
- Hlavackova, E.; Krenova, Z.; Kerekes, A.; Slanina, P.; Vlkova, M. B Cell Subsets Reconstitution and Immunoglobulin Levels in Children and Adolescents with B Non-Hodgkin Lymphoma after Treatment with Single Anti CD20 Agent Dose Included in Chemotherapeutic Protocols: Single Center Experience and Review of the Literature. Biomed. Pap. [CrossRef]
- Alexander, S.; Aupérin, A.; Bomken, S.; Csóka, M.; Kazanowska, B.; Chiang, A.K.; Andres, M.; Uyttebroeck, A.; Burke, G.A.A.; Zsiros, J.; et al. Effect of Rituximab on Immune Status in Children with Mature B-Cell Non-Hodgkin Lymphoma: A Prespecified Secondary Analysis of the Inter-B-NHL Ritux 2010 Trial. Lancet Haematol. 2023, 10, e445–e457. [Google Scholar] [CrossRef] [PubMed]
- Moser, O.; Zimmermann, M.; Meyer, U.; Klapper, W.; Oschlies, I.; Schrappe, M.; Attarbaschi, A.; Mann, G.; Niggli, F.; Spix, C.; et al. Second Malignancies after Treatment of Childhood Non-Hodgkin Lymphoma—A Report of the Berlin-Frankfurt-Muenster Study Group. Haematologica 2020, 106, 1390–1400. [Google Scholar] [CrossRef]
- Ehrhardt, M.J.; Sandlund, J.T.; Zhang, N.; Liu, W.; Ness, K.K.; Bhakta, N.; Chemaitilly, W.; Krull, K.R.; Brinkman, T.M.; Crom, D.B.; et al. Late Outcomes of Adult Survivors of Childhood Non-Hodgkin Lymphoma: A Report from the St. Jude Lifetime Cohort Study. Pediatr. Blood Cancer 2017, 64, e26338. [Google Scholar] [CrossRef]
- Ehrhardt, M.J.; Dixon, S.B.; Belsky, J.; Hochberg, J. Late Effects and Frontline Treatment Selection for Children with Non-Hodgkin Lymphoma. Best Pract. Res. Clin. Haematol. 2023, 36, 101443. [Google Scholar] [CrossRef]
- Moosmann, J.; Krusemark, A.; Dittrich, S.; Ammer, T.; Rauh, M.; Woelfle, J.; Metzler, M.; Zierk, J. Age-and sex-specific pediatric reference intervals for neutrophil-to-lymphocyte ratio, lymphocyte-to-monocyte ratio, and platelet-to-lymphocyte ratio. Int. J. Lab. Hematol. 2022, 44, 296–301. [Google Scholar] [CrossRef] [PubMed]
| n = 17 | Sex (M:F) | Median Age at Diagnosis (Range) | |
|---|---|---|---|
| B-NHL classification | |||
| BL | 10 (58.8%) | 10:0 | 7.7 (4.3–10.4) |
| PMBCL | 2 (11.8%) | 1:1 | 17.6 (12.8–22.3) |
| DLBCL | 2 (11.8%) | 1:1 | 12.5 (9.2–15.8) |
| BLL | 2 (11.8%) | 1:1 | 4.9 (4.7–5) |
| FL | 1 (5.9%) | 0:1 | 14.1 |
| Murphy staging | |||
| Stage I | 6% | ||
| Stage II | 12% | ||
| Stage III | 53% | ||
| Stage IV | 29% | ||
| FAB/LMB risk stratification | |||
| A | - | ||
| B | 87% | ||
| C | 13% | ||
| BFM risk stratification | |||
| R1 | - | ||
| R2 | 53% | ||
| R3 | 20% | ||
| R4 | 27% |
| Work-Up | Median | Range | % of Cohort with Abnormal Values for Age |
|---|---|---|---|
| WBC (/μL) | 8500 | 3800 to 62,500 | 12% |
| Lymphocytes (/μL) | 2204 | 531 to 13,750 | 20% |
| Lymphocyte proportion † (%) | 27.5 ± 13.3 | 20.2 to 34.9 | 12% |
| Relative neutrophil count † (%) | 60.3 ± 15.2 | 51.8 to 68.7 | 18% |
| Relative mononuclear cell population † (%) | 9.5 ± 4 | 7.3 to 11.7 | 41% |
| Percentage of eosinophils † (%) | 2.3 ± 2 | 1.2 to 3.7 | None |
| Hemoglobin † (g/dL) | 11.6 ± 1.4 | 10.9 to 12.4 | 6% |
| Platelet count † (/μL) | 330,060 ± 117,736 | 265,400 to 395,800 | 6% |
| Platelet-to-lymphocyte ratio | 152.6 | 2.8 to 580 | 60% |
| Lymphocyte-to-monocyte ratio | 3.5 ± 2.5 | 2.1 to 4.9 | 53% |
| LDH (U/L) | 397 | 194 to 14,640 | 73% |
| ESR (mm/1 h) | 26 | 10 to 110 | 93% |
| CRP (mg/dL) | 0.67 | 0.03 to 5.5 | 54% |
| AST (U/L) | 30 | 18 to 281 | 40% |
| ALT (U/L) | 18 | 9 to 67 | 20% |
| GGT (U/L) | 14 | 8 to 110 | 33% |
| Albumin † (g/dL) | 3.9 ± 0.5 | 3.6 to 4.2 | 33% |
| Creatinine (mg/dL) | 0.56 | 0.4 to 1.2 | 13% |
| C3 (mg/dL) | 128.5 | 119 to 184 | 17% |
| Cystatin-C (mg/L) | 0.62 | 0.54 to 1.04 | 0 |
| Ig | Levels at Diagnosis | Levels at the End of Chemotherapy | Days to Recover at Normal Levels |
|---|---|---|---|
| IgA (mg/dL) | 158.7 (±108.1) | 106.5 (±59.5) | 0 (0 to 3530) |
| IgM (mg/dL) | 112.5 (±48.8) | 39.6 (15.6 to 195) | 359 (0 to 3530) |
| IgG (mg/dL) | 1110.8 (±431.4) | 766.7 (±257.8) | 0 (0 to 1483) |
| IgG1 (mg/dL) | 563.8 (±258) | 620.7 (±298.9) | NA |
| IgG2 (mg/dL) | 168.8 (±81.1) | 270.3 (±129.4) | NA |
| IgG3 (mg/dL) | 32.2 (±17.7) | 34.1 (±21.9) | NA |
| IgG4 (mg/dL) | 11.4 (±9.3) | 19.1 (±14) | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kyriakidis, I.; Pelagiadis, I.; Stratigaki, M.; Katzilakis, N.; Stiakaki, E. B–NHL Cases in a Tertiary Pediatric Hematology—Oncology Department: A 20-Year Retrospective Cohort Study. Life 2024, 14, 633. https://doi.org/10.3390/life14050633
Kyriakidis I, Pelagiadis I, Stratigaki M, Katzilakis N, Stiakaki E. B–NHL Cases in a Tertiary Pediatric Hematology—Oncology Department: A 20-Year Retrospective Cohort Study. Life. 2024; 14(5):633. https://doi.org/10.3390/life14050633
Chicago/Turabian StyleKyriakidis, Ioannis, Iordanis Pelagiadis, Maria Stratigaki, Nikolaos Katzilakis, and Eftichia Stiakaki. 2024. "B–NHL Cases in a Tertiary Pediatric Hematology—Oncology Department: A 20-Year Retrospective Cohort Study" Life 14, no. 5: 633. https://doi.org/10.3390/life14050633
APA StyleKyriakidis, I., Pelagiadis, I., Stratigaki, M., Katzilakis, N., & Stiakaki, E. (2024). B–NHL Cases in a Tertiary Pediatric Hematology—Oncology Department: A 20-Year Retrospective Cohort Study. Life, 14(5), 633. https://doi.org/10.3390/life14050633








