What Is New about the Semimembranosus Distal Tendon? Ultrasound, Anatomical, and Histological Study with Clinical and Therapeutic Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Samples
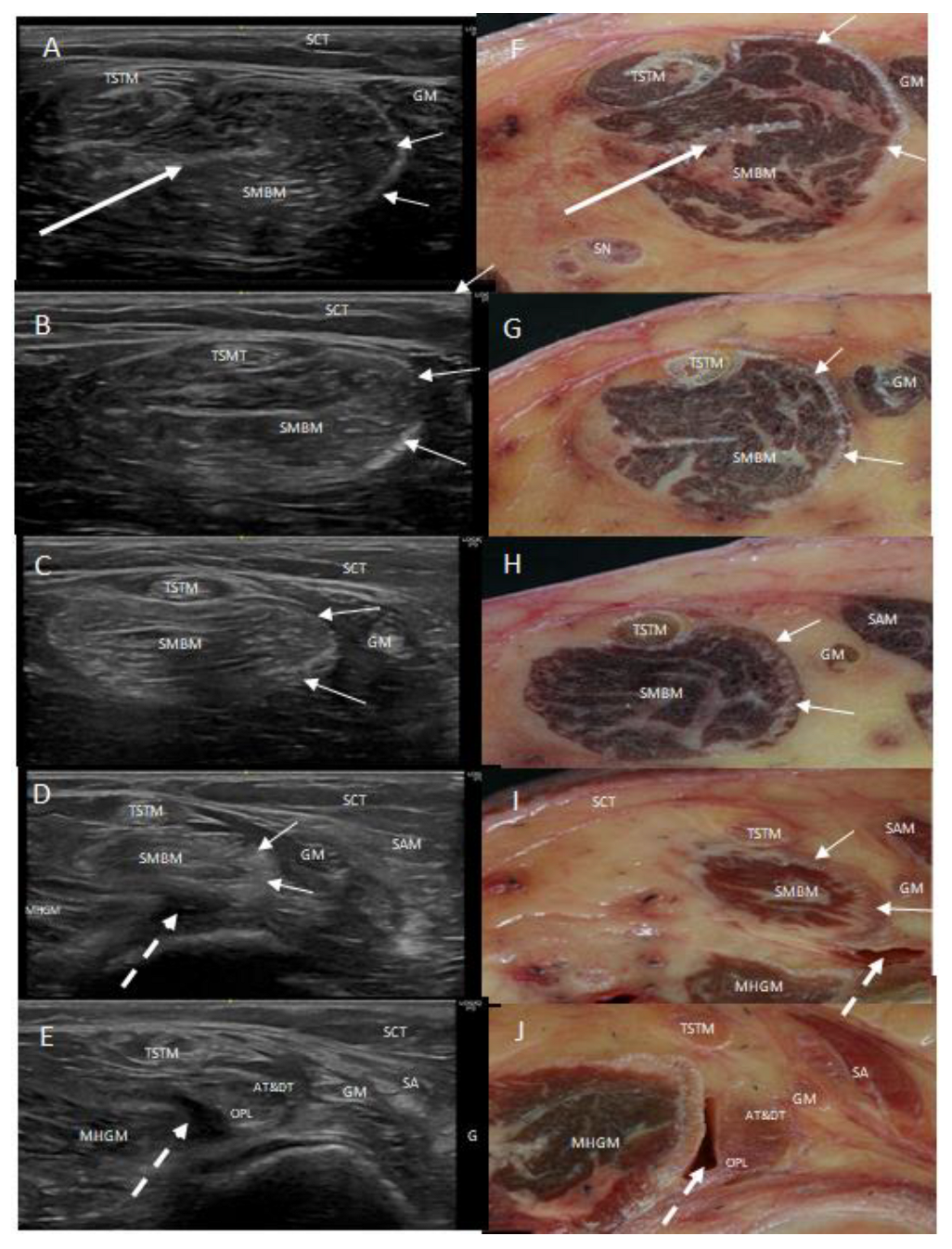
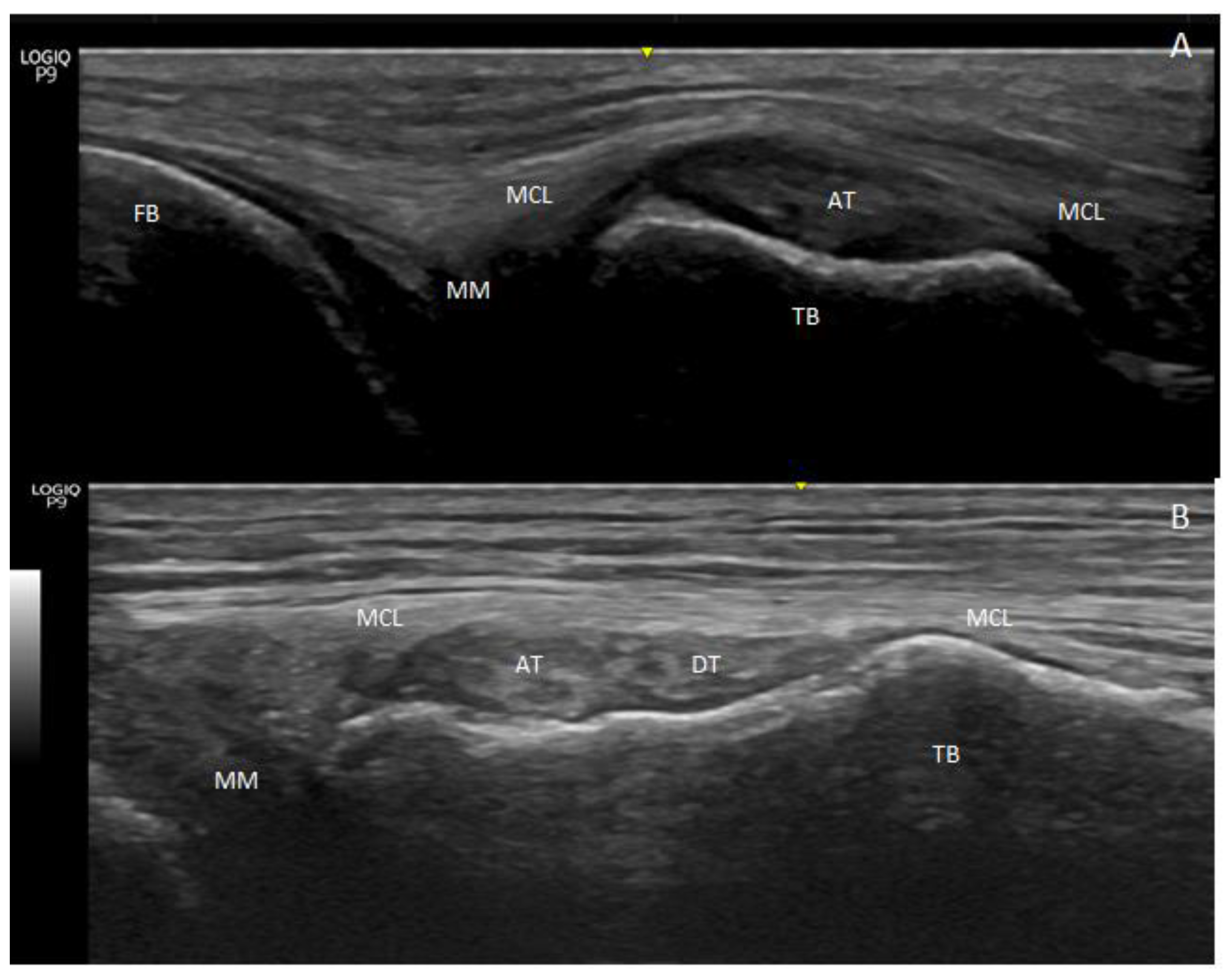
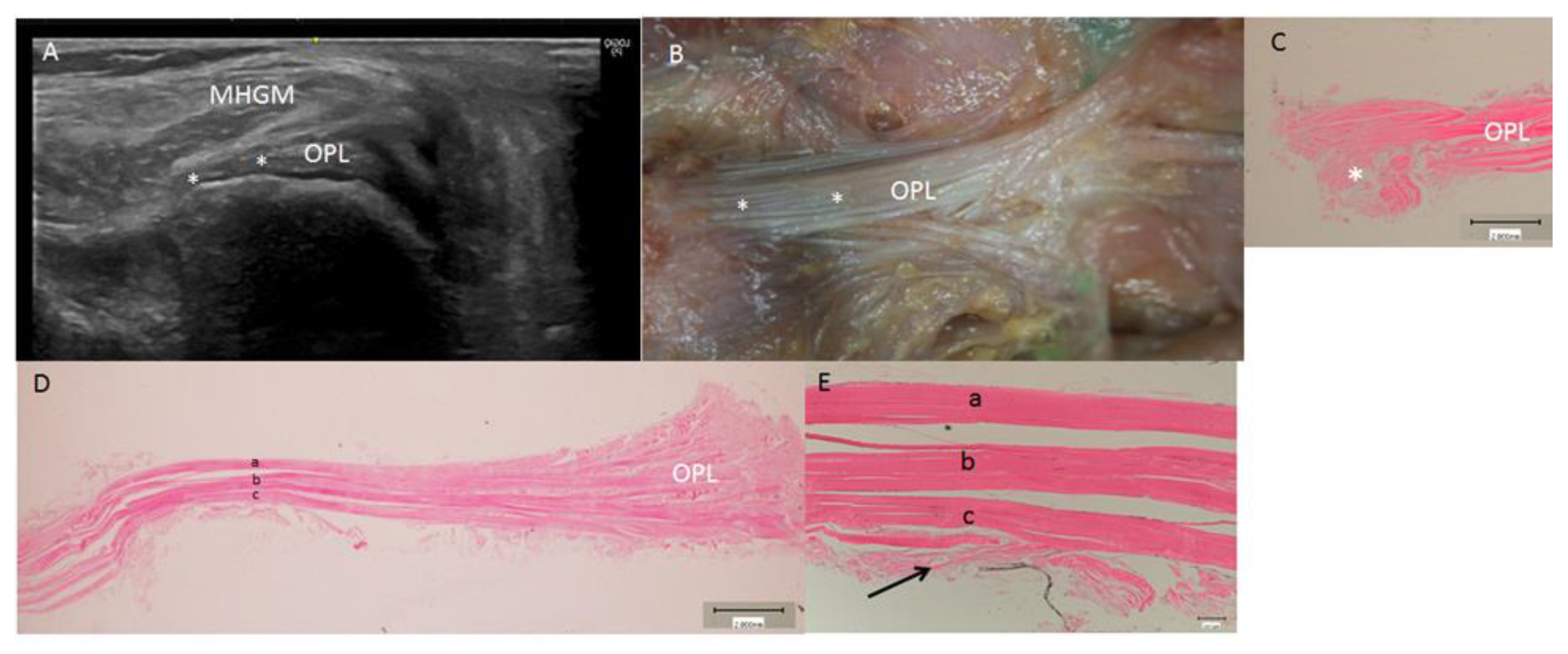
2.2. Ultrasound Study
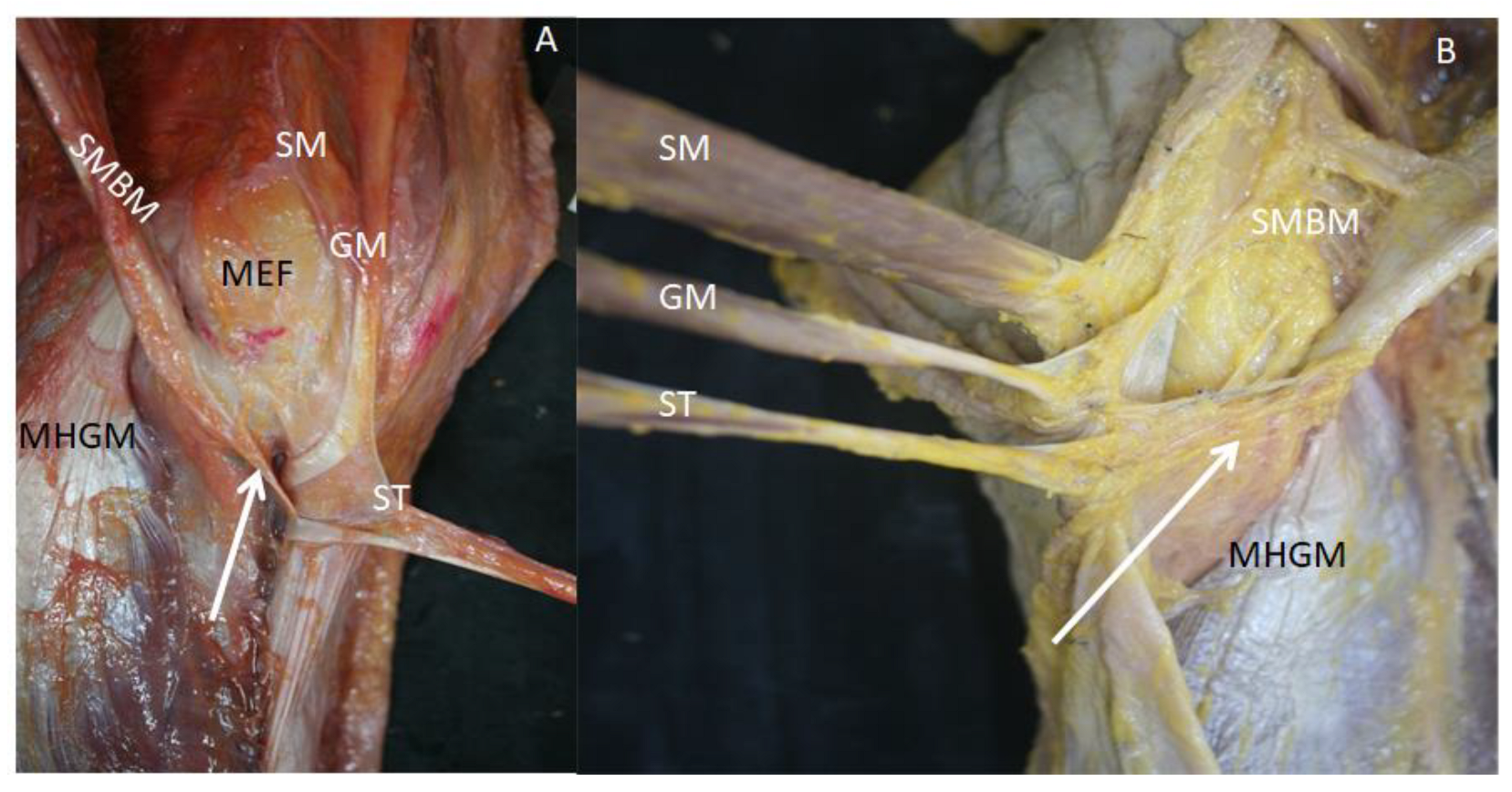
2.3. Anatomical Study
2.3.1. Dissection Procedure
2.3.2. Sectional Study
2.4. Histological Study
2.5. Statistical Analysis
3. Results
3.1. Ultrasound Study
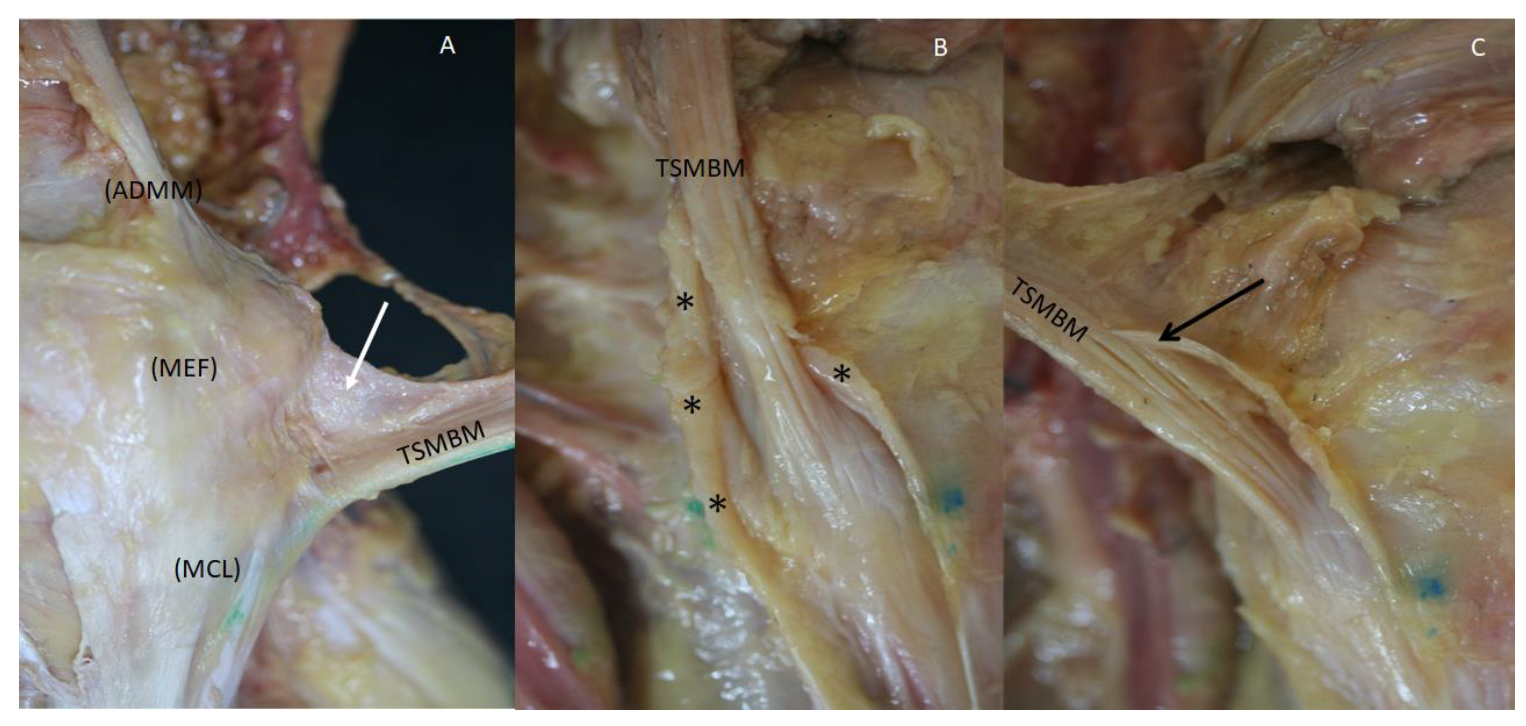
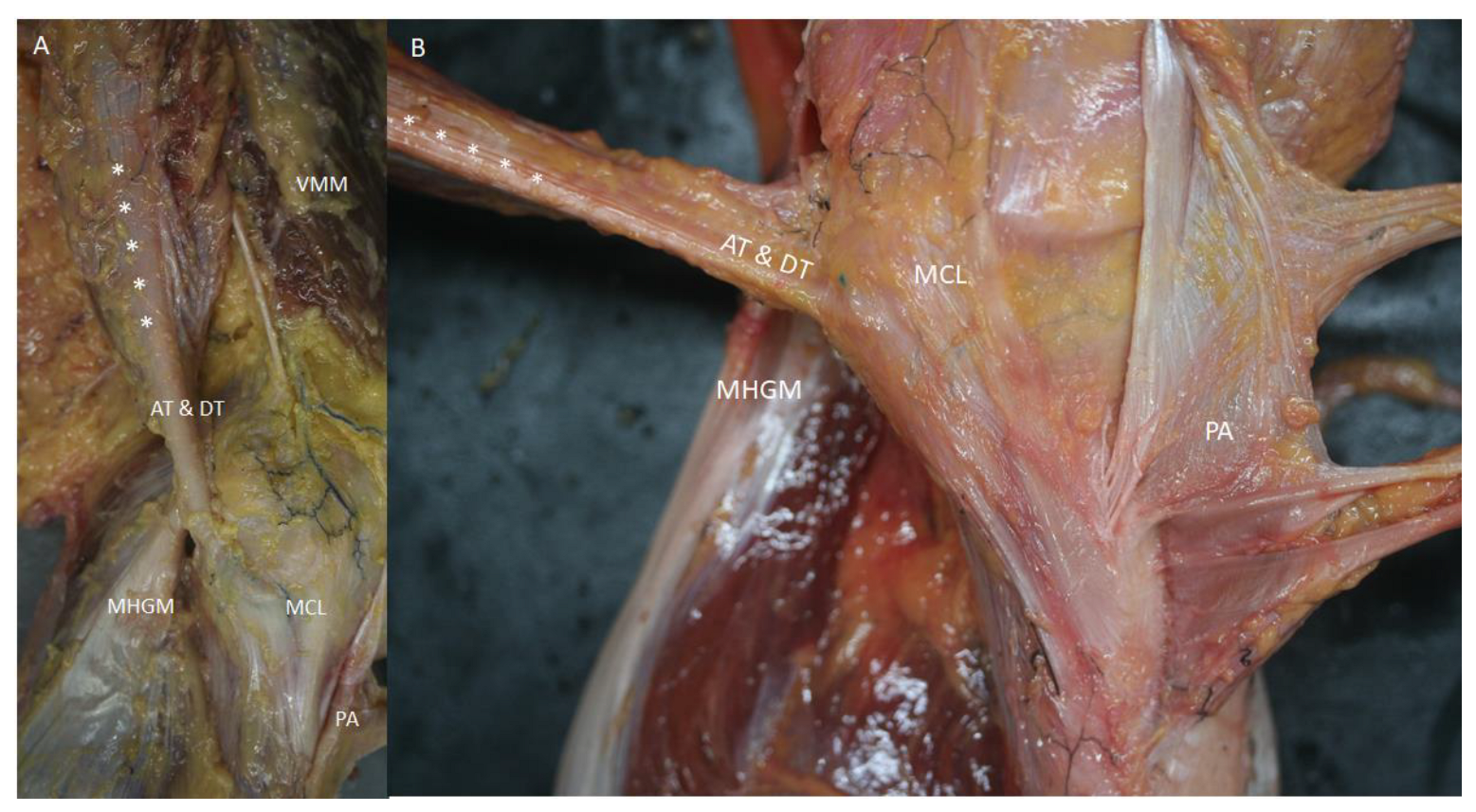
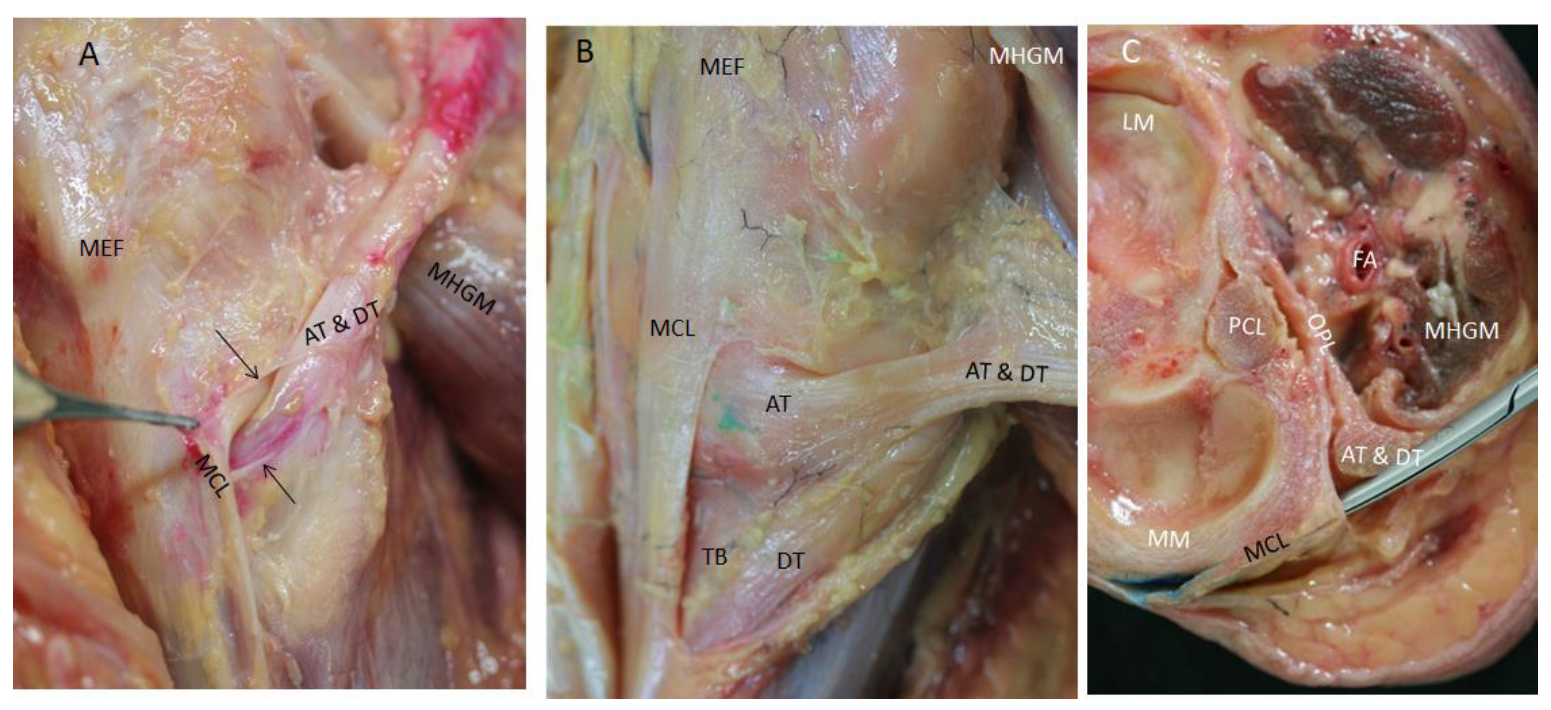
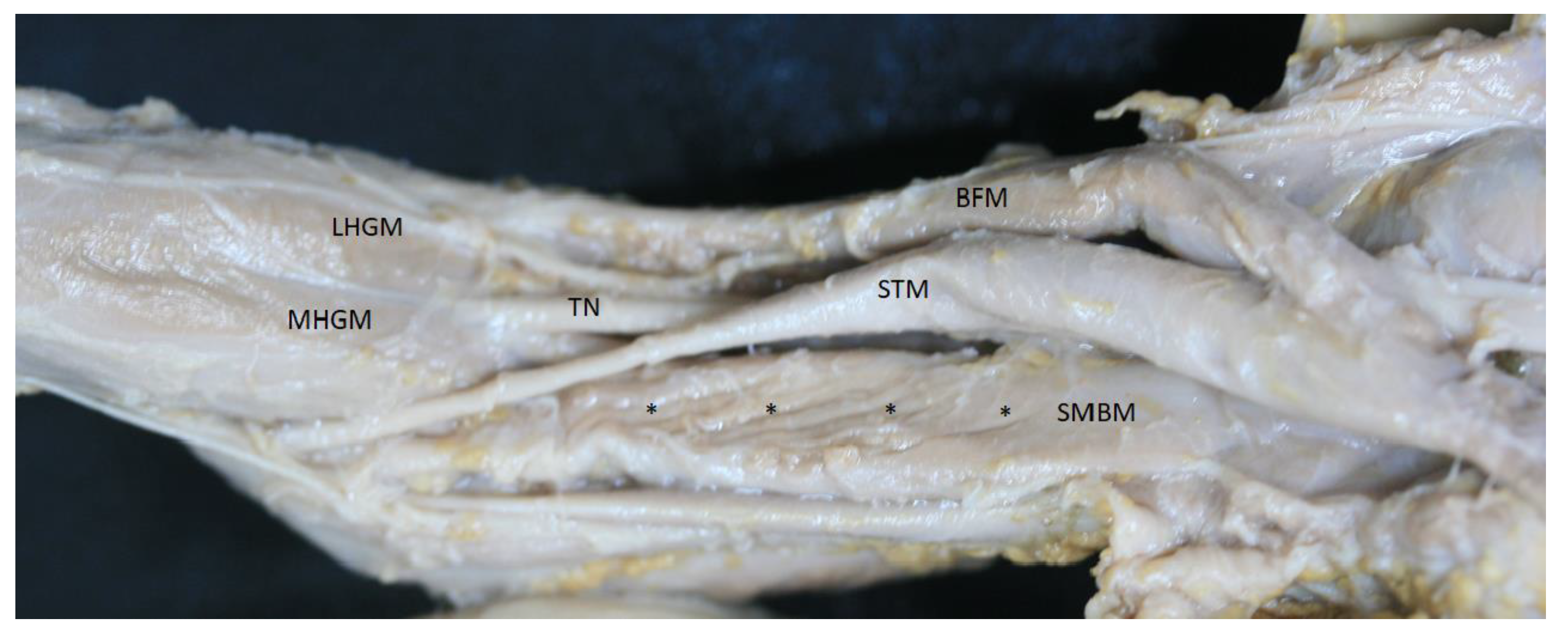
3.2. Anatomical Study
3.3. Histological Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Llusá, M.; Merí, À.; Ruano, D. Manual y Atlas Fotográfico de Anatomía del Aparato Locomotor, 1st ed.; Médica Panamericana: Madrid, Spain, 2004; 358p. [Google Scholar]
- Zhong, S.; Wu, B.; Wang, M.; Wang, X.; Yan, Q.; Fan, X.; Hu, Y.; Han, Y.; Li, Y. The anatomical and imaging study of pes anserinus and its clinical application. Medicine 2018, 97, e0352. [Google Scholar] [CrossRef] [PubMed]
- Olewnik, Ł.; Gonera, B.; Podgórski, M.; Polguj, M.; Jezierski, H.; Topol, M. A proposal for a new classification of pes anserinus morphology. Knee Surg. Sport Traumatol. Arthrosc. 2019, 27, 2984–2993. [Google Scholar] [CrossRef] [PubMed]
- Beltran, J.; Matityahu, A.; Hwang, K.; Jbara, M.; Maimon, R.; Padron, M.; Mota, J.; Beltran, L.; Sundaram, M. The distal semimembranosus complex: Normal MR anatomy, variants, biomechanics and pathology. Skelet. Radiol. 2003, 32, 435–445. [Google Scholar]
- Benninger, B.; Delamarter, T. Distal semimembranosus muscle-tendon-unit review: Morphology, accurate terminology, and clinical relevance. Folia Morphol. 2013, 72, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, R.R. The Medial and Posteromedial Ligamentous and Capsular Structures of the Knee: Review of Anatomy and Relevant Imaging Findings. Semin. Musculoskelet Radiol. 2016, 20, 12–25. [Google Scholar] [CrossRef] [PubMed]
- Vieira, T.D.; Pioger, C.; Frank, F.; Saithna, A.; Cavaignac, E.; Thaunat, M.; Cottet, B. Arthroscopic Dissection of the Distal Semimembranosus Tendon: An Anatomical Perspective on Posteromedial Instability and Ramp Lesions. Arthrosc Tech. 2019, 8, e987–e991. [Google Scholar] [CrossRef]
- Sims, W.F.; Jacobson, K.E. The Posteromedial Corner of the Knee: Medial-Sided Injury Patterns Revisited. Am. J. Sports Med. 2004, 32, 337–345. [Google Scholar] [CrossRef]
- De Maeseneer, M.; Shahabpour, M.; Lenchik, L.; Milants, A.; De Ridder, F.; De Mey, J.; Cattrysse, E. Distal insertions of the semimembranosus tendon: MR imaging with anatomic correlation. Skelet. Radiol. 2014, 43, 781–791. [Google Scholar] [CrossRef]
- Kim, Y.C.; Yoo, W.K.; Chung, I.H.; Seo, J.S.; Tanaka, S. Tendinous insertion of semimembranosus muscle into the lateral meniscus. Surg. Radiol. Anat. 1998, 19, 365–369. [Google Scholar] [CrossRef]
- LaPrade, R.F.; Morgan, P.M.; Wentorf, F.A.; Johansen, S.; Engebretsen, L. The anatomy of the posterior aspect of the knee: An anatomic study. J. Bone Jt. Surg. Ser. A. 2007, 89, 758–764. [Google Scholar] [CrossRef]
- Cavaignac, E.; Sylvie, R.; Teulières, M.; Fernandez, A.; Frosch, K.H.; Gomez-Brouchet, A.; Sonnery-Cottet, B. What Is the Relationship Between the Distal Semimembranosus Tendon and the Medial Meniscus? A Gross and Microscopic Analysis from the SANTI Study Group. Am. J. Sports Med. 2021, 49, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Benninger, B.; Delamarter, T. The “Oblique Popliteal Ligament”: A Macro- and Microanalysis to Determine If It Is a Ligament or a Tendon. Anat. Res. Int. 2012, 2012, 151342. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Suzuki, D.; Murakami, G.; Cho, B.H.; Fujimiya, M.; Kozuka, N. Human fetal anatomy of the posterior semimembranosus complex at the knee with special reference to the gastrocnemio-semimembranosus bursa. Knee 2011, 18, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.W.; Abe, H.; Jin, Y.; Shibata, S.; Murakami, G.; Rodríguez-Vázquez, J.F. Positional changes in tendon insertions from bone to fascia: Development of the pes anserinus and semimembranosus muscle insertion in human foetuses. Folia Morphol. 2016, 75, 503–511. [Google Scholar] [CrossRef]
- Balius, R.; Pedret, C.; Iriarte, I.; Sáiz, R.; Cerezal, L. Sonographic landmarks in hamstring muscles. Skelet. Radiol. 2019, 48, 1675–1683. [Google Scholar] [CrossRef] [PubMed]
- De Maeseneer, M.; Marcelis, S.; Boulet, C.; Kichouh, M.; Shahabpour, M.; De Mey, J.; Cattrysse, E. Ultrasound of the knee with emphasis on the detailed anatomy of anterior, medial, and lateral structures. Skelet. Radiol. 2014, 43, 1025–1039. [Google Scholar] [CrossRef]
- Laprade, M.D.; Kennedy, M.I.; Wijdicks, C.A.; Laprade, R.F. Anatomy and biomechanics of the medial side of the knee and their surgical implications. Sports Med. Arthrosc. 2015, 23, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Saygi, B.; Yildirim, Y.; Berker, N.; Ofluoglu, D.; Karadag-Saygi, E.; Karahan, M. Evaluation of the neurosensory function of the medial meniscus in humans. Arthrosc. J. Arthrosc. Relat. Surg. 2005, 21, 1468–1472. [Google Scholar] [CrossRef] [PubMed]
- Khoshnoodi, P.; Tehranzadeh, A.D.; Dunn, J.M.; Tehranzadeh, J. Semimembranosus tendon avulsion fracture of the posteromedial tibial plateau associated with posterior cruciate ligament tear and capsular rupture. Skelet. Radiol. 2014, 43, 239–242. [Google Scholar] [CrossRef]
- Bylund, W.E.; de Weber, K. Semimembranosus tendinopathy: One cause of chronic posteromedial knee pain. Sports Health 2010, 2, 380–384. [Google Scholar] [CrossRef]
- Lundquist, R.B.; Matcuk, G.R.; Schein, A.J.; Skalski, M.R.; White, E.A.; Forrester, D.M.; Patel, D.B. Posteromedial corner of the knee: The neglected corner. Radiographics 2015, 35, 1123–1137. [Google Scholar] [CrossRef] [PubMed]
- Rothstein, C.P.; Laorr, A.; Helms, C.A.; Tirman, P.F.J. Semimembranosus-tibial collateral ligament bursitis: MR imaging findings. Am. J. Roentgenol. 1996, 166, 875–877. [Google Scholar] [CrossRef] [PubMed]
- Beltran, L.; Ghazikhanian, V.; Padron, M.; Beltran, J. The proximal hamstring muscle-tendon-bone unit: A review of the normal anatomy, biomechanics, and pathophysiology. Eur. J. Radiol. 2012, 81, 3772–3779. [Google Scholar] [CrossRef] [PubMed]
- Yoon, M.A.; Choi, J.Y.; Lim, H.K.; Yoo, H.J.; Hong, S.H.; Choi, J.A.; Kang, H.S. High prevalence of abnormal MR findings of the distal semimembranosus tendon: Contributing factors based on demographic, radiographic, and MR features. Am. J. Roentgenol. 2014, 202, 1087–1093. [Google Scholar] [CrossRef] [PubMed]
- Chahal, J.; Al-Taki, M.; Pearce, D.; Leibenberg, A.; Whelan, D.B. Injury patterns to the posteromedial corner of the knee in high-grade multiligament knee injuries: A MRI study. Knee Surg. Sport Traumatol Arthrosc. 2010, 18, 1098–1104. [Google Scholar] [CrossRef] [PubMed]
- Haberfehlner, H.; Maas, H.; Harlaar, J.; Becher, J.G.; Buizer, A.I.; Jaspers, R.T. Freehand three-dimensional ultrasound to assess semitendinosus muscle morphology. J. Anat. 2016, 229, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Nimura, A.; Yamaguchi, K.; Akita, K. Anatomical study of the proximal origin of hamstring muscles. J. Orthop. Sci. 2012, 17, 614–618. [Google Scholar] [CrossRef] [PubMed]
- Julie, M.; Fritz, J.J.; Irrgang, C.D.H. Rehabilitation Following Allograft Meniscal Transplantation. J. Orthop. Sport Phys. Ther. 1996, 24, 98. [Google Scholar]
- Dean, R.S.; DePhillipo, N.N.; Monson, J.K.; LaPrade, R.F. Peripheral Stabilization Suture to Address Meniscal Extrusion in a Revision Meniscal Root Repair: Surgical Technique and Rehabilitation Protocol. Arthrosc. Tech. 2020, 9, e1211–e1218. [Google Scholar] [CrossRef]
- Bizzini, M.; Gorelick, M.; Drobny, T. Lateral meniscus repair in a professional ice Hockey goaltender: A case report with a 5-year follow-up. J. Orthop. Sports Phys. Ther. 2006, 36, 89–100. [Google Scholar] [CrossRef][Green Version]
- Cavanaugh, J.T.; Killian, S.E. Rehabilitation following meniscal repair. Curr. Rev. Musculoskelet Med. 2012, 5, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Perkins, B.; Gronbeck, K.R.; Yue, R.A.; Tompkins, M.A. Similar failure rate in immediate post-operative weight bearing versus protected weight bearing following meniscal repair on peripheral, vertical meniscal tears. Knee Surg. Sport Traumatol. Arthrosc. 2018, 26, 2245–2250. [Google Scholar] [CrossRef] [PubMed]
- Mackey, A.L.; Heinemeier, K.M.; Koskinen, S.O.A.; Kjaer, M. Dynamic adaptation of tendon and muscle connective tissue to mechanical loading. Connect. Tissue Res. 2008, 49, 165–168. [Google Scholar] [CrossRef] [PubMed]
- Rot-Nikcevic, I.; Reddy, T.; Downing, K.J.; Belliveau, A.C.; Hallgrímsson, B.; Hall, B.K.; Kablar, R. Myf5−/−: MyoD−/− amyogenic fetuses reveal the importance of early contraction and static loading by striated muscle in mouse skeletogenesis. Dev. Genes Evol. 2006, 216, 1–9. [Google Scholar] [CrossRef]
- Yamaguchi, Y.; Kodama, R.; Yamada, S. Morphogenetic progression of thigh and lower leg muscles during human embryonic development. Anat. Rec. 2023, 306, 2072–2080. [Google Scholar] [CrossRef]


| TENDON (mm) | MUSCLE (mm) | |||||
|---|---|---|---|---|---|---|
| Width | Thickness | Diameter | Width | Thickness | Diameter | |
| Average (SD) | 11.8 (1.43) | 4.69 (0.72) | 38.44 (2.93) | 38.29 (4.33) | 14.36 (3.23) | 112.64 (10.74) |
| 95% CI | 11.30–12.32 | 4.43–4.95 | 37.38–39.50 | 36.73–39.85 | 14.36–13.2 | 108.77–116.51 |
| Median (IQR) | 12.21 (2) | 4.65 (0.96) | 38.77 (2.5) | 39 (5.08) | 13.1 (4.43) | 109.8 (22.42) |
| Test Shapiro–Wilk (p) | 0.86 (0.000) | 0.961 (0.20) | 0.879 (0.14) | 0.940 (0.07) | 0.85 (0.001) | 0.894 (0.004) |
| Measures Distribution of Tendon and Muscle According to the Sex (1) | SEX | Test U Mann–Whitney | ||
|---|---|---|---|---|
| Man | Woman | |||
| TENDON (mm) | width | 11.70 (1.48) 10.96–12.3 | 11.96 (1.39) 11.15–12.76 | 140.5 (0.582) |
| thickness | 4.91 (0.59) 4.61–5.20 | 4.41 (0.78) 3.95–4.86 | 80.0 (0.081) | |
| diameter | 38.41 (3.28) 36.78–40.0 | 38.47 (2.53) 37–39.9 | 130.0 (0.879) | |
| MUSCLE (mm) | width | 38.5 (4.23) 36.4–36.44 | 37.9 (4.59) 12.38–15.1 | 101.0 (0.342) |
| thickness | 14.85 (2.35) 12.97–16.7 | 13.74 (2.33) 12.38–15.1 | 110.0 (0.558) | |
| diameter | 111.2 (10.1) 106.2–116.2 | 114.5 (11.7) 107.8–121.3 | 147.0 (0.425) | |
| Measures distribution of tendon and muscle according to the side (1) | SIDE | |||
| Right | Left | |||
| TENDON (mm) | width | 11.83 (1.34) 11.23–12.44 | 11.76 (1.65) 10.66–12.87 | 126.0 (0.696) |
| thickness | 4.69 (0.68) 4.39–501 | 4.67 (0.82) 4.13–5.23 | 117.5 (0.938) | |
| diameter | 38.57 (3.12) 37.15–39.99 | 38.19 (2.66) 36.40–39.97 | 103.0 (0.639) | |
| MUSCLE (mm) | width | 37.85 (4.52) 35.80–39.91 | 39.12 (3.99) 36.44–41.81 | 129.0 (0.611) |
| thick | 14.49 (3.59) 12.85–16.12 | 14.13 (2.54) 12.42–15.83 | 115.0 (1.0) | |
| diameter | 111.38 (10.87) 107.96–122.16 | 115.1 (10.57) 107.96–122.16 | 145.0 (0.254) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iglesias-Chamorro, P.; Pérez-Bellmunt, A.; Ortiz-Miguel, S.; Möller, I.; Blasi, J.; Ortiz-Sagristà, J.; Martinoli, C.; Sanjuan, X.; Miguel-Pérez, M. What Is New about the Semimembranosus Distal Tendon? Ultrasound, Anatomical, and Histological Study with Clinical and Therapeutic Application. Life 2024, 14, 631. https://doi.org/10.3390/life14050631
Iglesias-Chamorro P, Pérez-Bellmunt A, Ortiz-Miguel S, Möller I, Blasi J, Ortiz-Sagristà J, Martinoli C, Sanjuan X, Miguel-Pérez M. What Is New about the Semimembranosus Distal Tendon? Ultrasound, Anatomical, and Histological Study with Clinical and Therapeutic Application. Life. 2024; 14(5):631. https://doi.org/10.3390/life14050631
Chicago/Turabian StyleIglesias-Chamorro, Pere, Albert Pérez-Bellmunt, Sara Ortiz-Miguel, Ingrid Möller, Juan Blasi, Juan Ortiz-Sagristà, Carlo Martinoli, Xavier Sanjuan, and Maribel Miguel-Pérez. 2024. "What Is New about the Semimembranosus Distal Tendon? Ultrasound, Anatomical, and Histological Study with Clinical and Therapeutic Application" Life 14, no. 5: 631. https://doi.org/10.3390/life14050631
APA StyleIglesias-Chamorro, P., Pérez-Bellmunt, A., Ortiz-Miguel, S., Möller, I., Blasi, J., Ortiz-Sagristà, J., Martinoli, C., Sanjuan, X., & Miguel-Pérez, M. (2024). What Is New about the Semimembranosus Distal Tendon? Ultrasound, Anatomical, and Histological Study with Clinical and Therapeutic Application. Life, 14(5), 631. https://doi.org/10.3390/life14050631







