Insights into the Novel Cardiac Biomarker in Acute Heart Failure: Mybp-C
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Study Procedures and Measurements
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Profile of Cardiac Biomarkers
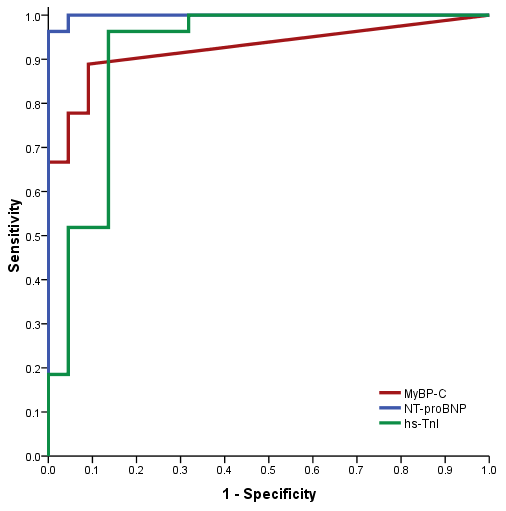
3.3. Diagnostic Performance of MyBP-C
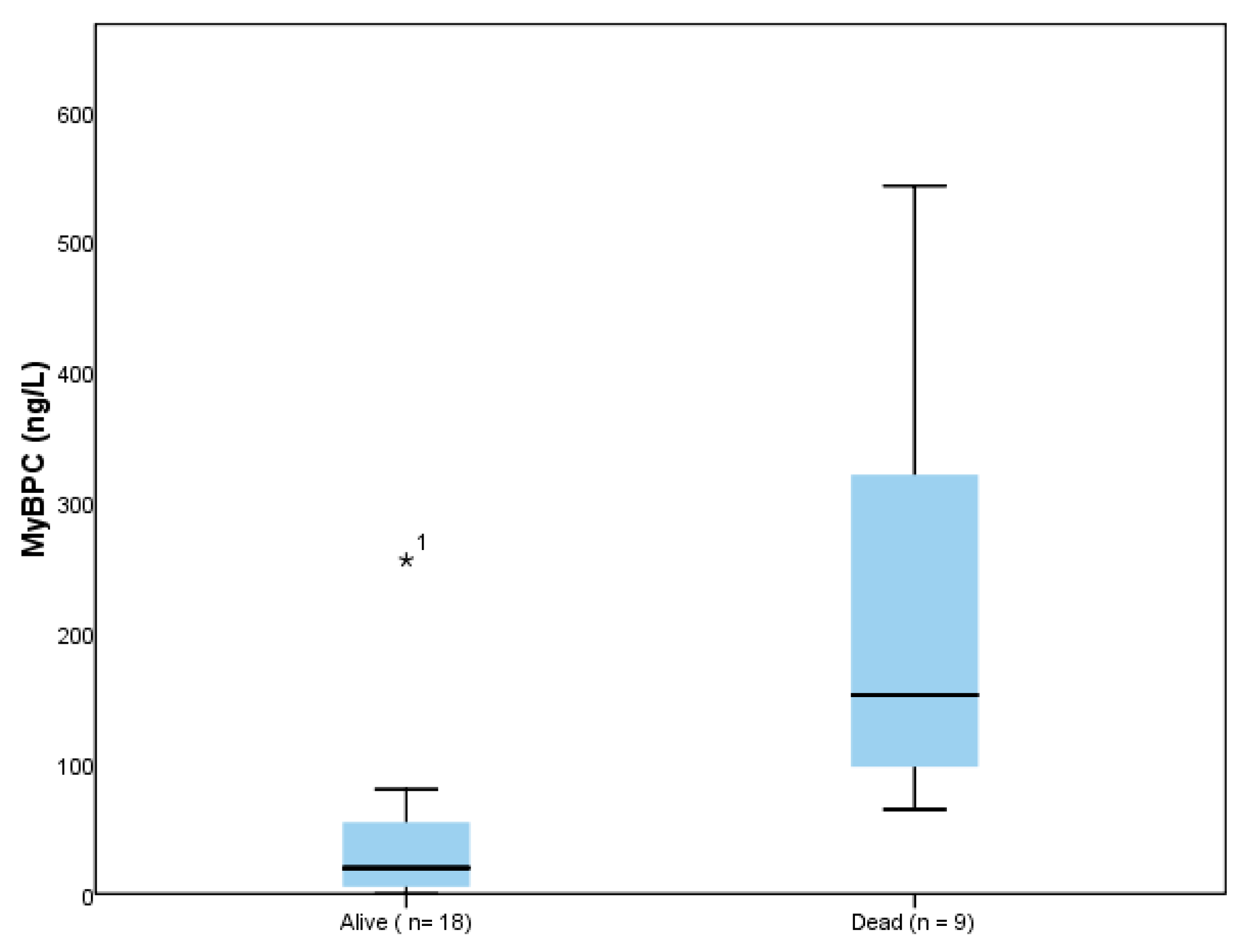
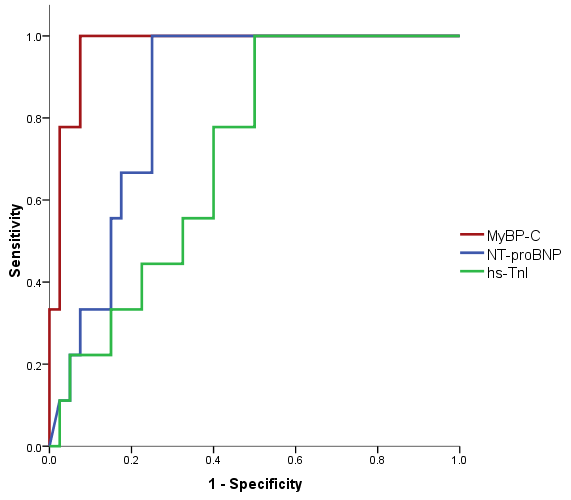
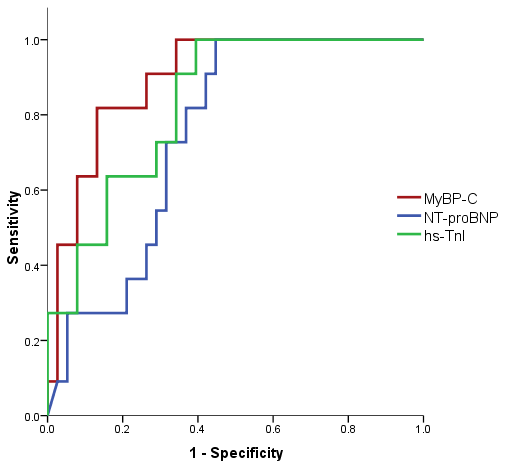
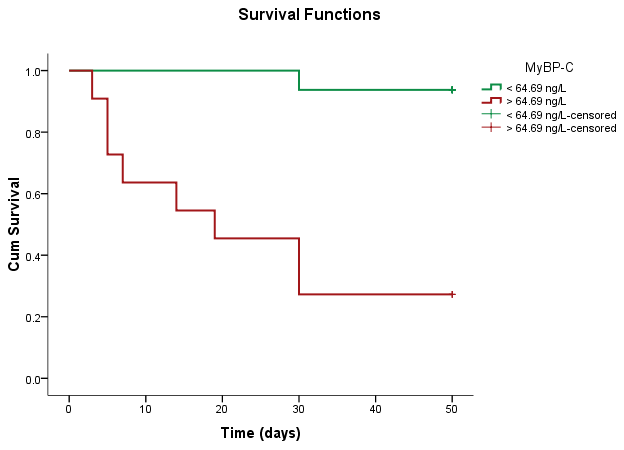
3.4. Prognostic Value of MyBP-C
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ziaeian, B.; Fonarow, G.C. Epidemiology and Aetiology of Heart Failure. Nat. Rev. Cardiol. 2016, 13, 368–378. [Google Scholar] [CrossRef] [PubMed]
- Groenewegen, A.; Rutten, F.H.; Mosterd, A.; Hoes, A.W. Epidemiology of Heart Failure. Eur. J. Heart Fail. 2020, 22, 1342–1356. [Google Scholar] [CrossRef] [PubMed]
- Task Force Members; McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; et al. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure: Developed by the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). With the Special Contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2022, 24, 4–131. [Google Scholar] [CrossRef] [PubMed]
- Writing Committee Members; ACC/AHA Joint Committee Members 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure. J. Card. Fail. 2022, 28, e1–e167. [CrossRef] [PubMed]
- Farmakis, D.; Parissis, J.; Lekakis, J.; Filippatos, G. Acute Heart Failure: Epidemiology, Risk Factors, and Prevention. Rev. Esp. Cardiol. Engl. Ed. 2015, 68, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Arrigo, M.; Jessup, M.; Mullens, W.; Reza, N.; Shah, A.M.; Sliwa, K.; Mebazaa, A. Acute Heart Failure. Nat. Rev. Dis. Primer 2020, 6, 16. [Google Scholar] [CrossRef]
- Wong, C.W.; Tafuro, J.; Azam, Z.; Satchithananda, D.; Duckett, S.; Barker, D.; Patwala, A.; Ahmed, F.Z.; Mallen, C.; Kwok, C.S. Misdiagnosis of Heart Failure: A Systematic Review of the Literature. J. Card. Fail. 2021, 27, 925–933. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Weiß, C.; Hoffmann, U.; Borggrefe, M.; Akin, I.; Behnes, M. Advantages and Limitations of Current Biomarker Research: From Experimental Research to Clinical Application. Curr. Pharm. Biotechnol. 2017, 18, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Gaggin, H.K.; Januzzi, J.L. Biomarkers and Diagnostics in Heart Failure. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2013, 1832, 2442–2450. [Google Scholar] [CrossRef]
- Sarhene, M.; Wang, Y.; Wei, J.; Huang, Y.; Li, M.; Li, L.; Acheampong, E.; Zhengcan, Z.; Xiaoyan, Q.; Yunsheng, X.; et al. Biomarkers in Heart Failure: The Past, Current and Future. Heart Fail. Rev. 2019, 24, 867–903. [Google Scholar] [CrossRef]
- Hill, S.A.; Booth, R.A.; Santaguida, P.L.; Don-Wauchope, A.; Brown, J.A.; Oremus, M.; Ali, U.; Bustamam, A.; Sohel, N.; McKelvie, R.; et al. Use of BNP and NT-proBNP for the diagnosis of heart failure in the emergency department: A systematic review of the evidence. Heart Fail. Rev. 2014, 19, 421–438. [Google Scholar] [CrossRef] [PubMed]
- McKie, P.M.; Burnett, J.C. NT-proBNP. J. Am. Coll. Cardiol. 2016, 68, 2437–2439. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, N.E.; Januzzi, J.L. Established and Emerging Roles of Biomarkers in Heart Failure. Circ. Res. 2018, 123, 614–629. [Google Scholar] [CrossRef] [PubMed]
- Andrijevic, I.; Milutinov, S.; Lozanov Crvenkovic, Z.; Matijasevic, J.; Andrijevic, A.; Kovacevic, T.; Bokan, D.; Zaric, B. N-Terminal Prohormone of Brain Natriuretic Peptide (NT-proBNP) as a Diagnostic Biomarker of Left Ventricular Systolic Dysfunction in Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease (AECOPD). Lung 2018, 196, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L. Natriuretic Peptides as Biomarkers in Heart Failure. J. Investig. Med. 2013, 61, 950–955. [Google Scholar] [CrossRef] [PubMed]
- Maisel, A.S.; Krishnaswamy, P.; Nowak, R.M.; McCord, J.; Hollander, J.E.; Duc, P.; Omland, T.; Storrow, A.B.; Abraham, W.T.; Wu, A.H.B.; et al. Rapid Measurement of B-Type Natriuretic Peptide in the Emergency Diagnosis of Heart Failure. N. Engl. J. Med. 2002, 347, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L.; Camargo, C.A.; Anwaruddin, S.; Baggish, A.L.; Chen, A.A.; Krauser, D.G.; Tung, R.; Cameron, R.; Nagurney, J.T.; Chae, C.U.; et al. The N-Terminal Pro-BNP Investigation of Dyspnea in the Emergency Department (PRIDE) Study. Am. J. Cardiol. 2005, 95, 948–954. [Google Scholar] [CrossRef]
- Mueller, C.; McDonald, K.; de Boer, R.A.; Maisel, A.; Cleland, J.G.F.; Kozhuharov, N.; Coats, A.J.S.; Metra, M.; Mebazaa, A.; Ruschitzka, F.; et al. Heart Failure Association of the European Society of Cardiology Practical Guidance on the Use of Natriuretic Peptide Concentrations. Eur. J. Heart Fail. 2019, 21, 715–731. [Google Scholar] [CrossRef]
- Kociol, R.D.; Pang, P.S.; Gheorghiade, M.; Fonarow, G.C.; O’Connor, C.M.; Felker, G.M. Troponin Elevation in Heart Failure. J. Am. Coll. Cardiol. 2010, 56, 1071–1078. [Google Scholar] [CrossRef]
- Peacock, W.F.; De Marco, T.; Fonarow, G.C.; Diercks, D.; Wynne, J.; Apple, F.S.; Wu, A.H.B. ADHERE Investigators Cardiac Troponin and Outcome in Acute Heart Failure. N. Engl. J. Med. 2008, 358, 2117–2126. [Google Scholar] [CrossRef]
- Arenja, N.; Reichlin, T.; Drexler, B.; Oshima, S.; Denhaerynck, K.; Haaf, P.; Potocki, M.; Breidthardt, T.; Noveanu, M.; Stelzig, C.; et al. Sensitive Cardiac Troponin in the Diagnosis and Risk Stratification of Acute Heart Failure. J. Intern. Med. 2012, 271, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.V.; Januzzi, J.L. ST2: A Novel Remodeling Biomarker in Acute and Chronic Heart Failure. Curr. Heart Fail. Rep. 2010, 7, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L.; Peacock, W.F.; Maisel, A.S.; Chae, C.U.; Jesse, R.L.; Baggish, A.L.; O’Donoghue, M.; Sakhuja, R.; Chen, A.A.; van Kimmenade, R.R.J.; et al. Measurement of the Interleukin Family Member ST2 in Patients with Acute Dyspnea: Results from the PRIDE (Pro-Brain Natriuretic Peptide Investigation of Dyspnea in the Emergency Department) Study. J. Am. Coll. Cardiol. 2007, 50, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L.; Mebazaa, A.; Di Somma, S. ST2 and Prognosis in Acutely Decompensated Heart Failure: The International ST2 Consensus Panel. Am. J. Cardiol. 2015, 115, 26B–31B. [Google Scholar] [CrossRef] [PubMed]
- van Kimmenade, R.R.; Januzzi, J.L.; Ellinor, P.T.; Sharma, U.C.; Bakker, J.A.; Low, A.F.; Martinez, A.; Crijns, H.J.; MacRae, C.A.; Menheere, P.P.; et al. Utility of Amino-Terminal pro-Brain Natriuretic Peptide, Galectin-3, and Apelin for the Evaluation of Patients with Acute Heart Failure. J. Am. Coll. Cardiol. 2006, 48, 1217–1224. [Google Scholar] [CrossRef]
- Khan, S.Q.; Dhillon, O.S.; O’Brien, R.J.; Struck, J.; Quinn, P.A.; Morgenthaler, N.G.; Squire, I.B.; Davies, J.E.; Bergmann, A.; Ng, L.L. C-Terminal Provasopressin (Copeptin) as a Novel and Prognostic Marker in Acute Myocardial Infarction: Leicester Acute Myocardial Infarction Peptide (LAMP) Study. Circulation 2007, 115, 2103–2110. [Google Scholar] [CrossRef]
- Kempf, T.; von Haehling, S.; Peter, T.; Allhoff, T.; Cicoira, M.; Doehner, W.; Ponikowski, P.; Filippatos, G.S.; Rozentryt, P.; Drexler, H.; et al. Prognostic Utility of Growth Differentiation Factor-15 in Patients with Chronic Heart Failure. J. Am. Coll. Cardiol. 2007, 50, 1054–1060. [Google Scholar] [CrossRef]
- de Tombe, P.P. Myosin Binding Protein C in the Heart. Circ. Res. 2006, 98, 1234–1236. [Google Scholar] [CrossRef][Green Version]
- Sadayappan, S.; Gulick, J.; Osinska, H.; Martin, L.A.; Hahn, H.S.; Dorn, G.W.; Klevitsky, R.; Seidman, C.E.; Seidman, J.G.; Robbins, J. Cardiac Myosin-Binding Protein-C Phosphorylation and Cardiac Function. Circ. Res. 2005, 97, 1156–1163. [Google Scholar] [CrossRef]
- Flashman, E.; Redwood, C.; Moolman-Smook, J.; Watkins, H. Cardiac myosin binding protein C: Its role in physiology and disease. Circ. Res. 2004, 94, 1279–1289. [Google Scholar] [CrossRef]
- El-Armouche, A.; Pohlmann, L.; Schlossarek, S.; Starbatty, J.; Yeh, Y.-H.; Nattel, S.; Dobrev, D.; Eschenhagen, T.; Carrier, L. Decreased Phosphorylation Levels of Cardiac Myosin-Binding Protein-C in Human and Experimental Heart Failure. J. Mol. Cell. Cardiol. 2007, 43, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Barefield, D.; Sadayappan, S. Phosphorylation and Function of Cardiac Myosin Binding Protein-C in Health and Disease. J. Mol. Cell. Cardiol. 2010, 48, 866–875. [Google Scholar] [CrossRef] [PubMed]
- Jacques, A.M.; Copeland, O.; Messer, A.E.; Gallon, C.E.; King, K.; McKenna, W.J.; Tsang, V.T.; Marston, S.B. Myosin Binding Protein C Phosphorylation in Normal, Hypertrophic and Failing Human Heart Muscle. J. Mol. Cell. Cardiol. 2008, 45, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Page, S.P.; Kounas, S.; Syrris, P.; Christiansen, M.; Frank-Hansen, R.; Andersen, P.S.; Elliott, P.M.; McKenna, W.J. Cardiac Myosin Binding Protein-C Mutations in Families with Hypertrophic Cardiomyopathy. Circ. Cardiovasc. Genet. 2012, 5, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Kaier, T.E.; Twerenbold, R.; Puelacher, C.; Marjot, J.; Imambaccus, N.; Boeddinghaus, J.; Nestelberger, T.; Badertscher, P.; Sabti, Z.; Giménez, M.R.; et al. Direct Comparison of Cardiac Myosin-Binding Protein C With Cardiac Troponins for the Early Diagnosis of Acute Myocardial Infarction. Circulation 2017, 136, 1495–1508. [Google Scholar] [CrossRef]
- Marjot, J.; Kaier, T.E.; Martin, E.D.; Reji, S.S.; Copeland, O.; Iqbal, M.; Goodson, B.; Hamren, S.; Harding, S.E.; Marber, M.S. Quantifying the Release of Biomarkers of Myocardial Necrosis from Cardiac Myocytes and Intact Myocardium. Clin. Chem. 2017, 63, 990–996. [Google Scholar] [CrossRef] [PubMed]
- Palmer, B.M.; Georgakopoulos, D.; Janssen, P.M.; Wang, Y.; Alpert, N.R.; Belardi, D.F.; Harris, S.P.; Moss, R.L.; Burgon, P.G.; Seidman, C.E.; et al. Role of cardiac myosin binding protein C in sustaining left ventricular systolic stiffening. Circ. Res. 2004, 94, 1249–1255. [Google Scholar] [CrossRef] [PubMed]
- Desjardins, C.L.; Chen, Y.; Coulton, A.T.; Hoit, B.D.; Yu, X.; Stelzer, J.E. Cardiac Myosin Binding Protein C Insufficiency Leads to Early Onset of Mechanical Dysfunction. Circ. Cardiovasc. Imaging 2012, 5, 127–136. [Google Scholar] [CrossRef]
- El Amrousy, D.; Hodeib, H.; Suliman, G.; Hablas, N.; Salama, E.R.; Esam, A. Diagnostic and Prognostic Value of Plasma Levels of Cardiac Myosin Binding Protein-C as a Novel Biomarker in Heart Failure. Pediatr. Cardiol. 2017, 38, 418–424. [Google Scholar] [CrossRef]
- El-Moghazy, E.M.; Morsy, S.M.; Abdallah, S.H.; Ali, M.A. Cardiac Myosin Binding Protein C Plasma Level as a Diagnostic and Prognostic Biomarker in Heart Failure in Children. Egypt. J. Hosp. Med. 2020, 80, 1097–1102. [Google Scholar] [CrossRef]
- Kozhuharov, N.; Wussler, D.; Kaier, T.; Strebel, I.; Shrestha, S.; Flores, D.; Nowak, A.; Sabti, Z.; Nestelberger, T.; Zimmermann, T.; et al. Cardiac Myosin-Binding Protein C in the Diagnosis and Risk Stratification of Acute Heart Failure. Eur. J. Heart Fail. 2021, 23, 716–725. [Google Scholar] [CrossRef]
- Sun, Y.; Dookhun, M.; Zou, H.; Cao, X.; Zhang, Y.; Lu, X. Research Progress of Cardiac Myosin Binding Protein C in Dilated Cardiomyopathy and Other Cardiac Conditions. World J. Cardiovasc. Dis. 2018, 8, 452–461. [Google Scholar] [CrossRef]
- Hou, L.; Kumar, M.; Anand, P.; Chen, Y.; El-Bizri, N.; Pickens, C.J.; Seganish, W.M.; Sadayappan, S.; Swaminath, G. Modulation of Myosin by Cardiac Myosin Binding Protein-C Peptides Improves Cardiac Contractility in Ex-Vivo Experimental Heart Failure Models. Sci. Rep. 2022, 12, 4337. [Google Scholar] [CrossRef] [PubMed]
- McKee, P.A.; Castelli, W.P.; McNamara, P.M.; Kannel, W.B. The Natural History of Congestive Heart Failure: The Framingham Study. N. Engl. J. Med. 1971, 285, 1441–1446. [Google Scholar] [CrossRef]
- Volpicelli, G.; Elbarbary, M.; Blaivas, M.; Lichtenstein, D.A.; Mathis, G.; Kirkpatrick, A.W.; Melniker, L.; Gargani, L.; Noble, V.E.; Via, G.; et al. International Evidence-Based Recommendations for Point-of-Care Lung Ultrasound. Intensive Care Med. 2012, 38, 577–591. [Google Scholar] [CrossRef] [PubMed]
- Platz, E.; Jhund, P.S.; Girerd, N.; Pivetta, E.; McMurray, J.J.V.; Peacock, W.F.; Masip, J.; Martin-Sanchez, F.J.; Miró, Ò.; Price, S.; et al. Expert Consensus Document: Reporting Checklist for Quantification of Pulmonary Congestion by Lung Ultrasound in Heart Failure. Eur. J. Heart Fail. 2019, 21, 844–851. [Google Scholar] [CrossRef] [PubMed]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the Areas under Two or More Correlated Receiver Operating Characteristic Curves: A Nonparametric Approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Iwanaga, Y.; Nishi, I.; Furuichi, S.; Noguchi, T.; Sase, K.; Kihara, Y.; Goto, Y.; Nonogi, H. B-Type Natriuretic Peptide Strongly Reflects Diastolic Wall Stress in Patients with Chronic Heart Failure: Comparison between Systolic and Diastolic Heart Failure. J. Am. Coll. Cardiol. 2006, 47, 742–748. [Google Scholar] [CrossRef]
- Roberts, E.; Ludman, A.J.; Dworzynski, K.; Al-Mohammad, A.; Cowie, M.R.; McMurray, J.J.V.; Mant, J. The Diagnostic Accuracy of the Natriuretic Peptides in Heart Failure: Systematic Review and Diagnostic Meta-Analysis in the Acute Care Setting. BMJ 2015, 350, h910. [Google Scholar] [CrossRef]
- Worster, A.; Balion, C.M.; Hill, S.A.; Santaguida, P.; Ismaila, A.; McKelvie, R.; Reichert, S.M.; McQueen, M.J.; Booker, L.; Raina, P.S. Diagnostic Accuracy of BNP and NT-proBNP in Patients Presenting to Acute Care Settings with Dyspnea: A Systematic Review. Clin. Biochem. 2008, 41, 250–259. [Google Scholar] [CrossRef]
- Hammarsten, O.; Mair, J.; Möckel, M.; Lindahl, B.; Jaffe, A.S. Possible Mechanisms behind Cardiac Troponin Elevations. Biomarkers 2018, 23, 725–734. [Google Scholar] [CrossRef] [PubMed]
- Mueller, C. Risk Stratification in Acute Decompensated Heart Failure: The Role of Cardiac Troponin. Nat. Clin. Pract. Cardiovasc. Med. 2008, 5, 680–681. [Google Scholar] [CrossRef] [PubMed]
- Miftode, R.-S.; Constantinescu, D.; Cianga, C.M.; Petris, A.O.; Timpau, A.-S.; Crisan, A.; Costache, I.-I.; Mitu, O.; Anton-Paduraru, D.-T.; Miftode, I.-L.; et al. A Novel Paradigm Based on ST2 and Its Contribution towards a Multimarker Approach in the Diagnosis and Prognosis of Heart Failure: A Prospective Study during the Pandemic Storm. Life 2021, 11, 1080. [Google Scholar] [CrossRef] [PubMed]
- Villacorta, H.; Maisel, A.S. Soluble ST2 Testing: A Promising Biomarker in the Management of Heart Failure. Arq. Bras. Cardiol. 2016, 106, 145–152. [Google Scholar] [CrossRef]
- Maisel, A.S.; Richards, A.M.; Pascual-Figal, D.; Mueller, C. Serial ST2 Testing in Hospitalized Patients with Acute Heart Failure. Am. J. Cardiol. 2015, 115, 32B–37B. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Pan, X.; Xu, H.; Wu, Y.; Jia, X.; Fang, Y.; Lu, Y.; Xu, Y.; Zhang, J.; Su, Y. Serum Soluble ST2 Is a Valuable Prognostic Biomarker in Patients With Acute Heart Failure. Front. Cardiovasc. Med. 2022, 9, 812654. [Google Scholar] [CrossRef] [PubMed]
- Miftode, R.-S.; Constantinescu, D.; Cianga, C.-M.; Petris, A.-O.; Costache, I.-I.; Mitu, O.; Miftode, I.-L.; Mitu, I.; Timpau, A.-S.; Duca, S.-T.; et al. A Rising Star of the Multimarker Panel: Growth Differentiation Factor-15 Levels Are an Independent Predictor of Mortality in Acute Heart Failure Patients Admitted to an Emergency Clinical Hospital from Eastern Europe. Life 2022, 12, 1948. [Google Scholar] [CrossRef] [PubMed]
- Lourenço, P.; Cunha, F.M.; Ferreira-Coimbra, J.; Barroso, I.; Guimarães, J.-T.; Bettencourt, P. Dynamics of Growth Differentiation Factor 15 in Acute Heart Failure. ESC Heart Fail. 2021, 8, 2527–2534. [Google Scholar] [CrossRef] [PubMed]
- Cotter, G.; Voors, A.A.; Prescott, M.F.; Felker, G.M.; Filippatos, G.; Greenberg, B.H.; Pang, P.S.; Ponikowski, P.; Milo, O.; Hua, T.A.; et al. Growth Differentiation Factor 15 (GDF-15) in Patients Admitted for Acute Heart Failure: Results from the RELAX-AHF Study. Eur. J. Heart Fail. 2015, 17, 1133–1143. [Google Scholar] [CrossRef]
- Kosum, P.; Mattanapojanat, N.; Kongruttanachok, N.; Ariyachaipanich, A. GDF-15: A Novel Biomarker of Heart Failure Predicts 30-Day All-Cause Mortality and 30-Day HF Rehospitalization in Patients with Acute Heart Failure Syndrome. Eur. Heart J. 2022, 43, ehab849.057. [Google Scholar] [CrossRef]
- Chen, H.; Chen, C.; Fang, J.; Wang, R.; Nie, W. Circulating Galectin-3 on Admission and Prognosis in Acute Heart Failure Patients: A Meta-Analysis. Heart Fail. Rev. 2020, 25, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Amin, H.Z.; Amin, L.Z.; Wijaya, I.P. Galectin-3: A Novel Biomarker for the Prognosis of Heart Failure. Clujul Med. 2017, 90, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Zaborska, B.; Sikora-Frąc, M.; Smarż, K.; Pilichowska-Paszkiet, E.; Budaj, A.; Sitkiewicz, D.; Sygitowicz, G. The Role of Galectin-3 in Heart Failure—The Diagnostic, Prognostic and Therapeutic Potential—Where Do We Stand? Int. J. Mol. Sci. 2023, 24, 13111. [Google Scholar] [CrossRef] [PubMed]
- Serraino, G.F.; Jiritano, F.; Costa, D.; Ielapi, N.; Battaglia, D.; Bracale, U.M.; Mastroroberto, P.; Andreucci, M.; Serra, R. Metalloproteinases in Cardiac Surgery: A Systematic Review. Biomolecules 2023, 13, 113. [Google Scholar] [CrossRef] [PubMed]
- Serraino, G.F.; Jiritano, F.; Costa, D.; Ielapi, N.; Napolitano, D.; Mastroroberto, P.; Bracale, U.M.; Andreucci, M.; Serra, R. Metalloproteinases and Hypertrophic Cardiomyopathy: A Systematic Review. Biomolecules 2023, 13, 665. [Google Scholar] [CrossRef] [PubMed]
- Shirakabe, A.; Asai, K.; Hata, N.; Yokoyama, S.; Shinada, T.; Kobayashi, N.; Mizuno, K. Clinical Significance of Matrix Metalloproteinase (MMP)-2 in Patients with Acute Heart Failure. Int. Heart. J. 2010, 51, 404–410. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wagner, D.R.; Delagardelle, C.; Ernens, I.; Rouy, D.; Vaillant, M.; Beissel, J. Matrix Metalloproteinase-9 Is a Marker of Heart Failure after Acute Myocardial Infarction. J. Card. Fail. 2006, 12, 66–72. [Google Scholar] [CrossRef] [PubMed]
- DeLeon-Pennell, K.Y.; Meschiari, C.A.; Jung, M.; Lindsey, M.L. Matrix Metalloproteinases in Myocardial Infarction and Heart Failure. Prog. Mol. Biol. Transl. Sci. 2017, 147, 75–100. [Google Scholar] [CrossRef] [PubMed]
- George, J.; Patal, S.; Wexler, D.; Roth, A.; Sheps, D.; Keren, G. Circulating Matrix Metalloproteinase-2 but Not Matrix Metalloproteinase-3, Matrix Metalloproteinase-9, or Tissue Inhibitor of Metalloproteinase-1 Predicts Outcome in Patients with Congestive Heart Failure. Am. Heart J. 2005, 150, 484–487. [Google Scholar] [CrossRef]
- Yamazaki, T.; Lee, J.-D.; Shimizu, H.; Uzui, H.; Ueda, T. Circulating Matrix Metalloproteinase-2 Is Elevated in Patients with Congestive Heart Failure. Eur. J. Heart Fail. 2004, 6, 41–45. [Google Scholar] [CrossRef]
- Biolo, A.; Fisch, M.; Balog, J.; Chao, T.; Schulze, P.C.; Ooi, H.; Siwik, D.; Colucci, W.S. Episodes of Acute Heart Failure Syndrome Are Associated with Increased Levels of Troponin and Extracellular Matrix Markers. Circ. Heart Fail. 2010, 3, 44–50. [Google Scholar] [CrossRef] [PubMed]
- de Boer, R.A.; Daniels, L.B.; Maisel, A.S.; Januzzi, J.L. State of the Art: Newer biomarkers in heart failure. Eur. J. Heart Fail. 2015, 17, 559–569. [Google Scholar] [CrossRef] [PubMed]
- Dookhun, N.; Zhang, J.-N.; Lu, X.-Z. MyBP-C in Cardiac Conditions and Its Potential Use as Novel Biomarker: A Review. Eur. Acad. Res. 2017, 5, 1352–1368. [Google Scholar]
- Cheng, Y.; Wan, X.; McElfresh, T.A.; Chen, X.; Gresham, K.S.; Rosenbaum, D.S.; Chandler, M.P.; Stelzer, J.E. Impaired contractile function due to decreased cardiac myosin binding protein C content in the sarcomere. Am. J. Physiol. Circ. Physiol. 2013, 305, H52–H65. [Google Scholar] [CrossRef] [PubMed]
- Lowry, M.T.H.; Doudesis, D.; Wereski, R.; Kimenai, D.M.; Tuck, C.; Ferry, A.V.; Bularga, A.; Taggart, C.; Lee, K.K.; Chapman, A.R.; et al. Influence of Age on the Diagnosis of Myocardial Infarction. Circulation 2022, 146, 1135–1148. [Google Scholar] [CrossRef] [PubMed]
- Welsh, P.; Campbell, R.T.; Mooney, L.; Kimenai, D.M.; Hayward, C.; Campbell, A.; Porteous, D.; Mills, N.L.; Lang, N.N.; Petrie, M.C.; et al. Reference Ranges for NT-proBNP (N-Terminal Pro-B-Type Natriuretic Peptide) and Risk Factors for Higher NT-proBNP Concentrations in a Large General Population Cohort. Circ. Heart Fail. 2022, 15, e009427. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.L.; Filippatos, G.; Nieminen, M.; Gheorghiade, M. Troponin Elevation in Patients with Heart Failure: On Behalf of the Third Universal Definition of Myocardial Infarction Global Task Force: Heart Failure Section. Eur. Heart J. 2012, 33, 2265–2271. [Google Scholar] [CrossRef] [PubMed]
- Felker, G.M.; Mentz, R.J.; Teerlink, J.R.; Voors, A.A.; Pang, P.S.; Ponikowski, P.; Greenberg, B.H.; Filippatos, G.; Davison, B.A.; Cotter, G.; et al. Serial high sensitivity cardiac troponin T measurement in acute heart failure: Insights from the RELAX-AHF study. Eur J Heart Fail 2015, 17, 1262–1270. [Google Scholar] [CrossRef] [PubMed]
- Meijers, W.C.; van der Velde, A.R.; de Boer, R.A. Biomarkers in Heart Failure with Preserved Ejection Fraction. Neth. Heart J. 2016, 24, 252–258. [Google Scholar] [CrossRef]
- Ahmed, A.; Aronow, W.S.; Fleg, J.L. Higher New York Heart Association Classes and Increased Mortality and Hospitalization in Patients with Heart Failure and Preserved Left Ventricular Function. Am. Heart J. 2006, 151, 444–450. [Google Scholar] [CrossRef]
- Arnold, J.M.O.; Liu, P.; Howlett, J.; Ignaszewski, A.; Leblanc, M.-H.; Kaan, A.; Pearce, C.; Sinclair, L.; Pearce, S.; Prentice, C. Ten Year Survival by NYHA Functional Class in Heart Failure Outpatients Referred to Specialized Multidisciplinary Heart Failure Clinics 1999 to 2011. Eur. Heart J. 2013, 34, P1505. [Google Scholar] [CrossRef]
- Caraballo, C.; Desai, N.R.; Mulder, H.; Alhanti, B.; Wilson, F.P.; Fiuzat, M.; Felker, G.M.; Piña, I.L.; O’Connor, C.M.; Lindenfeld, J.; et al. Clinical Implications of the New York Heart Association Classification. J. Am. Heart Assoc. 2019, 8, e014240. [Google Scholar] [CrossRef] [PubMed]
- GHERASIM, L. Troponins in Heart Failure—A Perpetual Challenge. Mædica 2019, 14, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Seino, Y.; Ogawa, A.; Yamashita, T.; Fukushima, M.; Ogata, K.; Fukumoto, H.; Takano, T. Application of NT-proBNP and BNP Measurements in Cardiac Care: A More Discerning Marker for the Detection and Evaluation of Heart Failure. Eur. J. Heart Fail. 2004, 6, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Song, B.G.; Jeon, E.S.; Kim, Y.H.; Kang, M.K.; Doh, J.H.; Kim, P.H.; Ahn, S.J.; Oh, H.L.; Kim, H.-J.; Sung, J.D.; et al. Correlation Between Levels of N-Terminal Pro-B-Type Natriuretic Peptide and Degrees of Heart Failure. Korean J. Intern. Med. 2005, 20, 26–32. [Google Scholar] [CrossRef] [PubMed]
- DeFilippi, C.; van Kimmenade, R.R.J.; Pinto, Y.M. Amino-Terminal Pro–B-Type Natriuretic Peptide Testing in Renal Disease. Am. J. Cardiol. 2008, 101, S82–S88. [Google Scholar] [CrossRef] [PubMed]
- Colbert, G.; Jain, N.; de Lemos, J.A.; Hedayati, S.S. Utility of Traditional Circulating and Imaging-Based Cardiac Biomarkers in Patients with Predialysis CKD. Clin. J. Am. Soc. Nephrol. CJASN 2015, 10, 515–529. [Google Scholar] [CrossRef]
- Chouairi, F.; Pacor, J.; Miller, P.E.; Fuery, M.A.; Caraballo, C.; Sen, S.; Leifer, E.S.; Felker, G.M.; Fiuzat, M.; O’Connor, C.M.; et al. Effects of Atrial Fibrillation on Heart Failure Outcomes and NT-proBNP Levels in the GUIDE-IT Trial. Mayo Clin. Proc. Innov. Qual. Outcomes 2021, 5, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Willis, M.S.; Lee, E.S.; Grenache, D.G. Effect of Anemia on Plasma Concentrations of NT-proBNP. Clin. Chim. Acta 2005, 358, 175–181. [Google Scholar] [CrossRef]
- Yap, L.B.; Ashrafian, H.; Mukerjee, D.; Coghlan, J.G.; Timms, P.M. The Natriuretic Peptides and Their Role in Disorders of Right Heart Dysfunction and Pulmonary Hypertension. Clin. Biochem. 2004, 37, 847–856. [Google Scholar] [CrossRef]
- Costabel, J.P.; Burgos, L.M.; Trivi, M. The Significance of Troponin Elevation in Atrial Fibrillation. J. Atr. Fibrillation 2017, 9, 1530. [Google Scholar] [CrossRef] [PubMed]
- Werhahn, S.M.; Becker, C.; Mende, M.; Haarmann, H.; Nolte, K.; Laufs, U.; Zeynalova, S.; Löffler, M.; Dagres, N.; Husser, D.; et al. NT-proBNP as a Marker for Atrial Fibrillation and Heart Failure in Four Observational Outpatient Trials. ESC Heart Fail. 2021, 9, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Jug, B.; Sebestjen, M.; Sabovic, M.; Pohar, M.; Keber, I. Atrial Fibrillation Is an Independent Determinant of Increased NT-proBNP Levels in Outpatients with Signs and Symptoms of Heart Failure. Wien. Klin. Wochenschr. 2009, 121, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Weir, R.A.; McMurray, J.J.; Velazquez, E.J. Epidemiology of heart failure and left ventricular systolic dysfunction after acute myocardial infarction: Prevalence, clinical characteristics, and prognostic importance. Am. J. Cardiol. 2006, 97, 13F–25F. [Google Scholar] [CrossRef] [PubMed]
- Lynch, T.L.; Sadayappan, S. Surviving the Infarct: A Profile of Cardiac Myosin Binding Protein-C Pathogenicity, Diagnostic Utility, and Proteomics in the Ischemic Myocardium. Proteom. Clin. Appl. 2014, 8, 569–577. [Google Scholar] [CrossRef] [PubMed]
- Govindan, S.; McElligott, A.; Muthusamy, S.; Nair, N.; Barefield, D.; Martin, J.L.; Gongora, E.; Greis, K.D.; Luther, P.K.; Winegrad, S.; et al. Cardiac Myosin Binding Protein-C Is a Potential Diagnostic Biomarker for Myocardial Infarction. J. Mol. Cell. Cardiol. 2012, 52, 154–164. [Google Scholar] [CrossRef] [PubMed]
- Lassus, J.; Tarvasmäki, T.; Tolppanen, H. Biomarkers in Cardiogenic Shock. Adv. Clin. Chem. 2022, 109, 31–73. [Google Scholar] [CrossRef] [PubMed]
- Mebazaa, A.; Tolppanen, H.; Mueller, C.; Lassus, J.; DiSomma, S.; Baksyte, G.; Cecconi, M.; Choi, D.J.; Cohen Solal, A.; Christ, M.; et al. Acute Heart Failure and Cardiogenic Shock: A Multidisciplinary Practical Guidance. Intensive Care Med. 2016, 42, 147–163. [Google Scholar] [CrossRef] [PubMed]
- Mitsas, A.C.; Elzawawi, M.; Mavrogeni, S.; Boekels, M.; Khan, A.; Eldawy, M.; Stamatakis, I.; Kouris, D.; Daboul, B.; Gunkel, O.; et al. Heart Failure and Cardiorenal Syndrome: A Narrative Review on Pathophysiology, Diagnostic and Therapeutic Regimens—From a Cardiologist’s View. J. Clin. Med. 2022, 11, 7041. [Google Scholar] [CrossRef]
- Takase, H.; Dohi, Y. Kidney Function Crucially Affects B-Type Natriuretic Peptide (BNP), N-Terminal proBNP and Their Relationship. Eur. J. Clin. Investig. 2014, 44, 303–308. [Google Scholar] [CrossRef]
- Savoj, J.; Becerra, B.; Kim, J.K.; Fusaro, M.; Gallieni, M.; Lombardo, D.; Lau, W.L. Utility of Cardiac Biomarkers in the Setting of Kidney Disease. Nephron 2019, 141, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Freda, B.J.; Tang, W.H.W.; Van Lente, F.; Peacock, W.F.; Francis, G.S. Cardiac Troponins in Renal Insufficiency: Review and Clinical Implications. J. Am. Coll. Cardiol. 2002, 40, 2065–2071. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (n = 49) | AHF (n = 27) | Control Group | p-Value | ||
|---|---|---|---|---|---|---|
| Total Control (n = 22) | No HF (n = 10) | Compensated HF (n = 12) | ||||
| Gender | 0.567 | |||||
| Male, n (%) | 29 (59.2%) | 15 (55.6%) | 14 (63.6%) | 7 (70%) | 7(58.3%) | |
| Female, n (%) | 20 (40.8%) | 12 (44.4%) | 8 (36.4%) | 3 (30%) | 5 (41.7%) | |
| Age, y (mean ± SD) | 67.06 ± 12.33 | 71.48 ± 9.86 | 61.64 ± 13.08 | 59.60 ± 13.83 | 63.33 ± 12.78 | 0.004 |
| Smoking, n (%) | 29 (59.2%) | 17 (63%) | 12 (54.5%) | 6 (60%) | 6 (50%) | 0.551 |
| Alcohol abuse, n (%) | 13 (29.5%) | 8 (29.6%) | 5 (22.7%) | 2 (20%) | 3 (25%) | 0.586 |
| Clinical Parameters | ||||||
| BMI, kg/m2 (mean ± SD) | 28.98 ± 5.35 | 28.73 ± 5.66 | 29.30 ± 5.06 | 29.50 ± 5.41 | 29.13 ± 5.00 | 0.712 |
| Obesity, n (%) | 22 (44.9%) | 11 (40.7%) | 11 (50%) | 5 (50%) | 6 (50%) | 0.517 |
| SBP, mmHg (mean ± SD) | 149.51 ± 37.31 | 160.26 ± 39.68 | 136.32 ± 30.02 | 125.10 ± 22.80 | 145.67 ± 32.95 | 0.024 |
| DBP, mmHg (mean ± SD) | 88.94 ± 21.71 | 91.93 ± 25.37 | 85.27 ± 15.97 | 76.00 ± 9.53 | 93.00 ± 16.41 | 0.291 |
| Heart rate, bpm (mean ± SD) | 98.59 ± 24.40 | 103.48 ± 24.61 | 92.59 ± 23.30 | 82.00 ± 16.12 | 101.42 ± 25.24 | 0.121 |
| Respiratory rate, breaths/min (mean ± SD) | 17.90 ± 3.98 | 19.19 ± 4.38 | 16.32 ± 2.76 | 16.20 ± 1.68 | 16.42 ± 3.50 | 0.011 |
| Oxygen saturation, % (mean ± SD) | 91.35 ± 8.13 | 87.44 ± 9.14 | 96.14 ± 2.03 | 96.90 ± 1.59 | 95.50 ± 2.19 | <0.001 |
| Temperature, °C (mean ± SD) | 36.29 ± 0.46 | 36.43 ± 0.54 | 36.11 ± 0.25 | 36.09 ± 0.26 | 36.13 ± 0.26 | 0.014 |
| Lung congestion, n (%) | 21 (42.9%) | 20 (74.1%) | 1 (4.5%) | 0 (0%) | 1 (8.3%) | <0.001 |
| In-hospital mortality, n (%) | 5 (10.2%) | 5 (18.5%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.033 |
| Inability of self-care, n (%) | 11 (22.4%) | 10 (37%) | 1 (4.5%) | 0 (0%) | 1 (8.3%) | 0.007 |
| Mortality within 30 days, n (%) | 4 (8.2%) | 4 (14.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.060 |
| Rehospitalization within 30 days, n (%) | 11 (22.4%) | 11 (40.7%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.001 |
| Medical History | ||||||
| Hypertension, n (%) | 35 (71.4%) | 23 (85.2%) | 12 (54.5%) | 5 (50%) | 7 (58.3%) | 0.018 |
| Diabetes mellitus, n (%) | 20 (40.8%) | 13 (48.1%) | 7 (31.8%) | 2 (20%) | 5 (41.7%) | 0.247 |
| Dyslipidemia, n (%) | 20 (40.8%) | 13 (48.1%) | 7 (31.8%) | 3 (30%) | 4 (33.3%) | 0.247 |
| CAD, n (%) | 20 (40.8%) | 13 (48.1%) | 7 (31.8%) | 1 (10%) | 6 (50%) | 0.247 |
| Atrial fibrillation, n (%) | 21 (42.9%) | 17 (63%) | 4 (18.2%) | 0 (0%) | 4 (33.3%) | 0.002 |
| CKD, n (%) | 38 (79.2%) | 24 (88.9%) | 14 (66.7%) | 5 (55.6%) | 9 (75%) | 0.060 |
| Stroke, n (%) | 3 (6.1%) | 3 (11.1%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.107 |
| PAD, n (%) | 2 (4.1%) | 2 (7.4%) | 0 (0%) | 0 (0%) | 0 (0%) | 0.192 |
| COPD, n (%) | 7 (14.3%) | 6 (22.2%) | 1 (4.5%) | 0 (0%) | 1 (8.3%) | 0.079 |
| Parameter | Total (n = 49) | AHF (n = 27) | Control Group | p-Value | ||
|---|---|---|---|---|---|---|
| Total Control (n = 22) | No HF (n = 10) | Compensated HF (n = 12) | ||||
| Hemoglobin, g/dL (mean ± SD) | 13.13 ± 2.11 | 12.83 ± 2.44 | 13.5 ± 1.60 | 13.81 ± 1.78 | 13.25 ± 1.47 | 0.271 |
| Hematocrit, % (mean ± SD) | 39.74 ± 5.99 | 39.51 ± 7.06 | 40.02 ± 4.50 | 40.95 ± 4.90 | 39.25 ± 4.18 | 0.770 |
| Serum iron, µg/dL (mean ± SD) | 57.73 ± 37.19 | 46.44 ± 22.82 | 72.24 ± 46.68 | 62.78 ± 26.99 | 79.33 ± 57.49 | 0.015 |
| Ferritin, ng/mL (mean ± SD) | 243.39 ± 335.79 | 280.88 ± 419.11 | 190.47 ± 155.88 | 295.50 ± 169.82 | 133.18 ± 119.28 | 0.403 |
| C-reactive protein, mg/dL (mean ± SD) | 2.42 ± 2.64 | 2.94 ± 2.83 | 1.79 ± 2.28 | 2.29 ± 2.46 | 1.37 ± 2.14 | 0.130 |
| Sodium, mmol/L (mean ± SD) | 138 ± 5.39 | 136.78 ± 6.61 | 139.50 ± 2.84 | 140.20 ± 2.65 | 138.92 ± 2.96 | 0.079 |
| Potassium, mmol/L (mean ± SD) | 4.47 ± 0.54 | 4.58 ± 0.62 | 4.33 ± 0.38 | 4.22 ± 0.27 | 4.42 ± 0.43 | 0.104 |
| Urea, mg/dL (mean ± SD) | 57.86 ± 26.15 | 64.11 ± 28.39 | 50.18 ± 21.30 | 40.80 ± 19.01 | 58.00 ± 20.59 | 0.063 |
| Serum creatinine, mg/dL (mean ± SD) | 1.18 ± 0.52 | 1.33 ± 0.59 | 0.99 ± 0.34 | 0.90 ± 0.36 | 1.07 ± 0.33 | 0.023 |
| ACR, mg/g (mean ± SD) | 168.82 ± 371.98 | 288.27 ± 471.32 | 22.21 ± 19.46 | 10.80 ± 9.99 | 31.72 ± 20.60 | 0.011 |
| UNa+, mmol/L (mean ± SD) | 77.45 ± 47.61 | 60.22 ± 31.29 | 98.59 ± 55.85 | 117.50 ± 52.56 | 82.83 ± 55.67 | 0.004 |
| Serum bicarbonate, mEq/L (mean ± SD) | 23.89 ± 4.46 | 22.58 ± 4.16 | 25.65 ± 4.35 | 24.67 ± 3.62 | 26.35 ± 4.87 | 0.030 |
| eGFR, ml/min/1,73 m2 (mean ± SD) | 65.92 ± 25.95 | 55.30 ± 21.79 | 78.95 ± 25.05 | 87.60 ± 20.23 | 71.75 ± 27.19 | 0.001 |
| Albumin, mg/dL (mean ± SD) | 57.65 ± 5.99 | 56.38 ± 6.64 | 59.20 ± 4.78 | 58.45 ± 3.81 | 59.84 ± 5.55 | 0.102 |
| AST, IU/L (mean ± SD) | 103.67 ± 377.02 | 161.78 ± 498.49 | 28.95 ± 24.11 | 21.67 ± 6.94 | 34.42 ± 30.76 | 0.230 |
| ALT, IU/L (mean ± SD) | 82.33 ± 283.86 | 124.44 ± 375.65 | 28.19 ± 20.913 | 22.56 ± 10.52 | 32.42 ± 25.86 | 0.248 |
| GGT, IU/L (mean ± SD) | 92.60 ± 135.05 | 125.67 ± 169.85 | 50.10 ± 44.54 | 46.89 ± 22.73 | 52.50 ± 56.71 | 0.530 |
| Glycemia, mg/dL (mean ± SD) | 157 ± 85.23 | 175.67 ± 94.70 | 131.80 ± 64.45 | 111.88 ± 29.04 | 145.08 ± 78.47 | 0.810 |
| Uric acid, mg/dL (mean ± SD) | 7.22 ± 2.53 | 8.05 ± 2.52 | 6.16 ± 2.15 | 5.81 ± 1.83 | 6.39 ± 2.39 | 0.010 |
| Total bilirubin, mg/dL (mean ± SD) | 1.01 ± 0.90 | 1.30 ± 1.12 | 0.66 ± 0.27 | 0.64 ± 0.31 | 0.67 ± 0.25 | 0.012 |
| TSH, mIU/L (mean ± SD) | 2.09 ± 1.83 | 2.25 ± 2.22 | 1.89 ± 1.25 | 1.89 ± 1.30 | 1.89 ± 1.26 | 0.501 |
| CK-MB, mg/dL (mean ± SD) | 50.97 ± 105.36 | 69.22 ± 138.59 | 28.57 ± 25.23 | 19.76 ± 10.35 | 35.91 ± 31.59 | 0.182 |
| MyBP-C, ng/L (median, IQR) | 5.23 (0.01–60.73) | 54.88 (9.59–123.87) | 0.01 (0.01–0.01) | 0.01 (0.01–0.01) | 0.01 (0.01–0.01) | <0.001 |
| NT-proBNP, pg/mL (median, IQR) | 3925 (105–15923) | 15783 (7153–21113) | 89.90 (53.75–305.75) | 53.50 (39.73–73.55) | 282.50 (102.50–385.75) | <0.001 |
| hs-cTnI, ng/L (median,IQR) | 42.80 (3.82–510) | 349 (53–3885) | 3.2 (2.08–7.66) | 2.29 (1.33–2.74) | 7.28 (3.66–176.10) | <0.001 |
| Parameter | Total (n = 49) | AHF (n = 27) | Control Group | p-Value | ||
|---|---|---|---|---|---|---|
| Total Control (n = 22) | No HF (n = 10) | Compensated HF (n = 12) | ||||
| LVEDD, mm (mean ± SD) | 54.61 ± 7.78 | 57.11 ± 7.25 | 51.54 ± 7.44 | 48.20 ± 4.56 | 54.33 ± 8.38 | 0.011 |
| LVESD, mm (mean ± SD) | 42.20 ± 9.47 | 44.91 ± 9.88 | 38.78 ± 7.99 | 34.75 ± 3.45 | 41.72 ± 9.04 | 0.034 |
| LVEF, % (mean ± SD) | 37.65 ± 17.45 | 29.81 ± 14.37 | 47.27 ± 16.26 | 59.50 ± 2.83 | 37.08 ± 15.79 | <0.001 |
| LAD, mm (mean ± SD) | 45.73 ± 9.61 | 48.52 ± 10.01 | 42.32 ± 8.07 | 39.70 ± 8.47 | 44.50 ± 7.36 | 0.023 |
| LAA, cm2 (mean ± SD) | 26 ± 7.81 | 28.80 ± 8.45 | 22.57 ± 5.34 | 20.94 ± 3.26 | 23.92 ± 6.42 | 0.004 |
| RVD, mm (mean ± SD) | 33.82 ± 5.99 | 35.15 ± 6.21 | 32.18 ± 5.40 | 31.30 ± 4.47 | 32.92 ± 6.17 | 0.085 |
| sPAP, mmHg (mean ± SD) | 36.08 ± 23.58 | 44.11 ± 22.57 | 26.23 ± 21.35 | 15.40 ± 7.66 | 27 ± 20.42 | 0.007 |
| MAPSE, mm (mean ± SD) | 12.35 ± 3.10 | 11.37 ± 2.84 | 13.55 ± 3.05 | 15.00 ± 1.15 | 12.33 ± 3.62 | 0.013 |
| Moderate/severe MR, n (%) | 28 (57.1%) | 22 (81.4%) | 6 (27.2%) | 0 (0%) | 6 (50%) | 0.002 |
| Moderate/severe TR, n (%) | 28 (57.1%) | 19 (70.4%) | 9 (40.9%) | 1 (10%) | 8 (66.7%) | 0.048 |
| E/e’ >15, n (%) | 15 (32.6%) | 12 (50%) | 3 (13.6%) | 0 (0%) | 3 (25%) | 0.027 |
| Etiology, n (%) | |
| Ischemic disease | 15 (55.6%) |
| Alcoholic DCM | 4 (14.8%) |
| Valvular | 5 (18.5%) |
| Hypertensive heart disease | 3 (11.1%) |
| Ejection fraction, n (%) | |
| HFrEF | 24 (88.9%) |
| HFpEF | 3 (11.1%) |
| HFmrEF | 0 (0%) |
| NYHA Class, n (%) | |
| NYHA I | 0 (0%) |
| NYHA II | 6 (22.2%) |
| NYHA III | 16 (59.3%) |
| NYHA IV | 5 (18.5%) |
| Clinical presentations of AHF, n (%) | |
| Acute decompensated HF | 7 (25.9%) |
| Acute pulmonary oedema | 17 (63%) |
| Cardiogenic shock | 3 (11.1%) |
| Biomarker | Acute Coronary Syndrome n = 8 (29.6%) | Hypertension Emergency n = 6 (22.2%) | Arrhythmia n = 4 (14.8%) | Infection n = 6 (22.2%) | p-Value |
|---|---|---|---|---|---|
| MyBP-C, ng/L (median, IQR) | 68.51 (38.90–448.94) | 4.80 (0.01–93.06) | 81.05 (36.47–153.73) | 52.33 (12.14–173.21) | 0.540 |
| NT-proBNP, pg/mL (median, IQR) | 11,969 (3792.50–16,896) | 16,753.50 (6346–24,999.75) | 8813 (5875.75–15,300.75) | 18,448.50 (6972.50–23,847.25) | 0.456 |
| hs-TnI, ng/L (median, IQR) | 13,918.50 (4000.25–27,812) | 91.15 (48.87–446.50) | 76.75 (23.27–1222.75) | 173 (13.34–661.75) | 0.012 |
| Biomarker | Reduced EF n = 24 (88.9%) | Preserved EF n = 3 (11.1%) | p-Value |
|---|---|---|---|
| MyBP-C, ng/L (median, IQR) | 47.46 (6.43–117.23) | 64.77 (11.26–321.23) | 0.537 |
| NT-proBNP, pg/mL (median, IQR) | 14,357 (7345.25–20,562) | 17,359 (7031–25,600) | 0.643 |
| hs-TnI, ng/L (median, IQR) | 276 (53.12–4230.75) | 370 (6.87–1597) | 0.700 |
| Biomarker | Acute Decompensated HF n = 7 (25.9%) | Acute Pulmonary Edema n = 17 (63%) | Cardiogenic Shock n = 3 (11.1%) | p-Value |
|---|---|---|---|---|
| MyBP-C, ng/L (median, IQR) | 56.84 (5.23–172.54) | 35.76 (7.48–69.02) | 513.30 (318.58–528) | <0.001 |
| NT-proBNP, pg/mL (median, IQR) | 11,268 (8500–29,429) | 15,783 (6914–20,011) | 17,174 (14,090.50–20,218.50) | <0.001 |
| hs-TnI, ng/L (median, IQR) | 349 (19.90–11,841) | 143 (47.90–1117) | 15,996 (8099.50–22,911.50) | <0.001 |
| Biomarker | Without HF n = 10 (20.4%) | Class II NYHA n = 6 (22.2%) | Class III NYHA n = 16 (59.3%) | Class IV NYHA n = 5 (18.5%) | p-Value |
|---|---|---|---|---|---|
| MyBP-C, ng/L (median, IQR) | 0.01 (0.01–0.01) | 0.01 (0.01–50.26) | 27.04 (0.01–68.94) | 97.33 (8.25–431.96) | 0.011 |
| NT-proBNP, pg/mL (median, IQR) | 53.50 (39.73–73.55) | 329 (127.50–9854) | 11,268 (3682.50–19,418.50) | 11,007 (8078.50–27,800) | <0.001 |
| hs-TnI, ng/L (median, IQR) | 2.29 (1.33–2.74) | 53 (3.82–1123.50) | 107 (17.70–2711) | 349 (10.03–15,098.50) | 0.006 |
| Biomarker | AMI n = 9 (33.3%) | Non-AMI n = 18 (66.6%) | p-Value |
|---|---|---|---|
| MyBP-C, ng/L (median, IQR) | 80.18 (44.23–384.58) | 31.40 (4.92–79.29) | 0.046 |
| NT-proBNP, pg/mL (median, IQR) | 12,931 (5169–20,311) | 15,783.50 (7122.50–21,668) | 0.668 |
| hs-TnI, ng/L (median, IQR) | 11,841 (1123.50–25,797) | 87.65 (32.35–364.75) | <0.001 |
| Parameter | My-BPC | NT-proBNP | hs-TnI | |||
|---|---|---|---|---|---|---|
| r | p-Value | r | p-Value | r | p-Value | |
| Age | 0.209 | 0.149 | 0.456 | 0.001 | 0.348 | 0.014 |
| Gender | 0.093 | 0.525 | 0.217 | 0.134 | 0.082 | 0.574 |
| Alcohol abuse | 0.176 | 0.226 | 0.008 | 0.956 | 0.105 | 0.474 |
| Smoking | 0.012 | 0.933 | −0.122 | 0.404 | −0.056 | 0.703 |
| Obesity | −0.028 | 0.851 | −0.218 | 0.133 | −0.070 | 0.634 |
| Dyspnea | 0.707 | <0.001 | 0.837 | <0.001 | 0.644 | <0.001 |
| Pulmonary rales | 0.597 | <0.001 | 0.602 | <0.001 | 0.500 | <0.001 |
| SBP | −0.085 | 0.563 | 0.291 | 0.042 | 0.132 | 0.364 |
| DBP | −0.226 | 0.119 | 0.170 | 0.242 | 0.029 | 0.843 |
| HR | 0.136 | 0.350 | 0.258 | 0.074 | 0.279 | 0.052 |
| Oxygen saturation | −0.487 | <0.001 | −0.618 | <0.001 | −0.623 | <0.001 |
| Lung congestion | 0.681 | <0.001 | 0.612 | <0.001 | 0.539 | <0.001 |
| AMI | 0.535 | <0.001 | 0.332 | 0.020 | 0.607 | <0.001 |
| PE | −0.216 | 0.135 | −0.296 | 0.039 | −0.381 | 0.007 |
| Infection | 0.214 | 0.140 | 0.239 | 0.099 | 0.114 | 0.434 |
| Sepsis | 0.228 | 0.115 | 0.311 | 0.030 | 0.258 | 0.073 |
| Atrial fibrillation | 0.456 | 0.001 | 0.435 | 0.002 | 0.452 | 0.001 |
| Anemia | 0.256 | 0.076 | 0.262 | 0.069 | 0.146 | 0.318 |
| CKD | 0.148 | 0.315 | 0.355 | 0.013 | 0.074 | 0.617 |
| COPD | 0.196 | 0.177 | 0.303 | 0.034 | 0.412 | 0.003 |
| Diabetes mellitus | 0.189 | 0.193 | 0.164 | 0.259 | 0.167 | 0.250 |
| Cardiogenic shock | 0.413 | 0.003 | 0.247 | 0.087 | 0.307 | 0.032 |
| Inotropic support | 0.367 | 0.009 | 0.184 | 0.204 | 0.158 | 0.278 |
| Loop diuretic dose | 0.574 | <0.001 | 0.731 | <0.001 | 0.599 | <0.001 |
| Invasive ventilation | 0.440 | 0.002 | 0.295 | 0.040 | 0.353 | 0.013 |
| Inability of selfcare | −0.274 | 0.057 | −0.446 | 0.001 | −0.190 | 0.190 |
| In-hospital mortality | 0.483 | <0.001 | 0.300 | 0.036 | 0.300 | 0.036 |
| Death within 30 days | 0.412 | 0.003 | 0.329 | 0.021 | 0.074 | 0.614 |
| Length of hospital stay | 0.333 | 0.019 | 0.236 | 0.102 | 0.127 | 0.383 |
| Rehospitalization within 30 days | 0.606 | <0.001 | 0.361 | 0.011 | 0.481 | <0.001 |
| Parameter | My-BPC | NT-proBNP | hs-TnI | |||
|---|---|---|---|---|---|---|
| r | p-Value | r | p-Value | r | p-Value | |
| C-reactive protein | 0.343 | 0.016 | 0.280 | 0.052 | 0.305 | 0.033 |
| Hemoglobin | −0.266 | 0.065 | −0.283 | 0.049 | −0.072 | 0.621 |
| Leucocytes | 0.265 | 0.065 | 0.480 | <0.001 | 0.321 | 0.025 |
| Serum iron | −0.269 | 0.065 | −0.335 | 0.020 | −0.205 | 0.162 |
| Ferritin | 0.105 | 0.515 | −0.032 | 0.843 | −0.079 | 0.623 |
| Serum creatinine | 0.453 | 0.001 | 0.495 | <0.001 | 0.392 | 0.005 |
| eGFR | −0.483 | <0.001 | −0.595 | <0.001 | −0.430 | 0.002 |
| UNa+ | −0.426 | 0.002 | −0.447 | 0.001 | −0.337 | 0.018 |
| ACR | 0.385 | 0.006 | 0.733 | <0.001 | 0.468 | 0.001 |
| Sodium | −0.300 | 0.036 | −0.233 | 0.108 | −0.213 | 0.142 |
| Lactate | 0.132 | 0.465 | 0.014 | 0.939 | 0.438 | 0.011 |
| Serum bicarbonate | −0.489 | 0.001 | −0.202 | 0.211 | −0.198 | 0.221 |
| Albumin | −0.332 | 0.020 | −0.283 | 0.049 | −0.205 | 0.158 |
| Uric acid | 0.449 | 0.002 | 0.453 | 0.002 | 0.158 | 0.293 |
| AST | 0.389 | 0.006 | 0.465 | 0.001 | 0.621 | <0.001 |
| ALT | 0.104 | 0.481 | 0.206 | 0.160 | 0.207 | 0.158 |
| Total bilirubin | 0.239 | 0.098 | 0.213 | 0.143 | 0.183 | 0.208 |
| TSH | 0.028 | 0.850 | 0.068 | 0.647 | 0.033 | 0.824 |
| Total cholesterol | −0.181 | 0.218 | −0.116 | 0.432 | −0.071 | 0.632 |
| Glycemia | 0.047 | 0.753 | 0.174 | 0.242 | 0.255 | 0.083 |
| pH | −0.098 | 0.582 | 0.000 | 0.999 | −0.188 | 0.286 |
| LVEDD | 0.289 | 0.044 | 0.355 | 0.012 | 0.379 | 0.007 |
| LVEF | −0.399 | 0.004 | −0.554 | <0.001 | −0.540 | <0.001 |
| LAA | 0.367 | 0.010 | 0.435 | 0.002 | 0.149 | 0.306 |
| RVD | 0.177 | 0.223 | 0.205 | 0.157 | 0.251 | 0.081 |
| sPAP | 0.449 | 0.001 | 0.582 | <0.001 | 0.413 | 0.003 |
| MAPSE | −0.348 | 0.014 | −0.546 | <0.001 | −0.386 | 0.006 |
| TAPSE | −0.196 | 0.176 | −0.277 | 0.054 | −0.258 | 0.073 |
| E/e′ > 15 | 0.327 | 0.022 | 0.449 | 0.001 | 0.357 | 0.012 |
| LV systolic dysfunction | 0.334 | 0.019 | 0.539 | <0.001 | 0.551 | <0.001 |
| moderate/severe MR | 0.403 | 0.004 | 0.563 | <0.001 | 0.525 | <0.001 |
| moderate/severe TR | 0.277 | 0.054 | 0.429 | 0.002 | 0.315 | 0.028 |
| IVC | 0.355 | 0.012 | 0.425 | 0.002 | 0.386 | 0.006 |
| Parameter | My-BPC | |
|---|---|---|
| r | p-Value | |
| NT-proBNP | 0.727 | <0.001 |
| hs-TnI | 0.604 | <0.001 |
| Biomarker | AUC | Std. Error | Asymptotic 95% Confidence Interval | p-Value | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| MyBP-C (ng/L) | 0.924 | 0.040 | 0.841 | 1.00 | <0.001 |
| NT-proBNP (pg/mL) | 0.998 | 0.003 | 0.000 | 1.00 | <0.001 |
| hs-TnI (ng/L) | 0.912 | 0.047 | 0.813 | 1.00 | <0.001 |
| Characteristic | Mortality (n = 9) | No Mortality (n = 18) | p-Value |
|---|---|---|---|
| Age, y (mean ± SD) | 65.67 ± 8.68 | 74.39 ± 9.29 | 0.027 |
| Male Gender (%) | 4 (44.4%) | 11 (61.1%) | 0.411 |
| Length of hospital stay, days (mean ± SD) | 12.75 ± 5.90 | 10 ± 4.82 | 0.873 |
| SBP, mmHg (mean ± SD) | 170 ± 54.94 | 168.17 ± 36.48 | 0.124 |
| HR, beats/minute (mean ± SD) | 114.25 ± 17.67 | 95.33 ± 23.32 | 0.970 |
| NYHA functional class IV (%) | 3 (33.3%) | 2 (11.1%) | 0.161 |
| Smoking (%) | 3 (33.3%) | 7 (38.9%) | 0.778 |
| Obesity (%) | 4 (44.4%) | 7 (38.9%) | 0.782 |
| Diabetes mellitus (%) | 5 (55.6%) | 8 (44.4%) | 0.586 |
| Arterial hypertension (%) | 7 (77.8%) | 16 (88.9%) | 0.444 |
| Atrial fibrillation (%) | 8 (88.9%) | 9 (50%) | 0.049 |
| Anemia (%) | 4 (44.4%) | 8 (44.4%) | 1 |
| Myocardial infarction (%) | 4 (44.4%) | 5 (27.8%) | 0.756 |
| COPD (%) | 1 (11.1%) | 5 (27.8%) | 0.326 |
| CKD (%) | 9 (100%) | 15 (83.3%) | 0.194 |
| NT-proBNP, pg/mL (median, IQR) | 17,174 (10,066.50–24431.50) | 12,099.50 (6348–19,460) | 0.173 |
| MyBP-C, ng/L (median, IQR) | 152.44 (81.05–417.26) | 19.73 (4.92–55.37) | <0.001 |
| hs-TnI, ng/L (median, IQR) | 203 (34.50–8796.50) | 356 (50.45–4000.25) | 0.797 |
| CRP, mg/dL (mean± SD) | 3.88 ± 3.19 | 2.47 ± 2.60 | 0.229 |
| Creatinine, mg/dL (mean ± SD) | 1.94 ± 1.15 | 1.24 ± 0.37 | 0.155 |
| ACR, mg/g (median, IQR) | 127.95 (59.71–1725.08) | 83.50 (23.01–176.95) | 0.280 |
| UNa+, mEq/L (mean ± SD) | 57.25 ± 43.53 | 69.33 ± 30.09 | 0.129 |
| eGFR, mL/min/1.73 m2 (mean ± SD) | 47.75 ± 32.26 | 61.08 ± 22.94 | 0.093 |
| Uric acid, mg/dL (mean ± SD) | 9.62 ± 0.20 | 7.90 ± 2.41 | 0.029 |
| Serum iron, mcg/dL (mean ± SD) | 46.50 ± 30.88 | 35 ± 13.54 | 0.728 |
| Ferritin, ng/mL (mean ± SD) | 233.25 ± 230.22 | 318.67 ± 567.41 | 0.644 |
| Albumin, g/dL (mean ± SD) | 52.31 ± 6.63 | 58.42 ± 5.79 | 0.021 |
| Lactate, mmol/L (mean ± SD) | 5.02 ± 4.64 | 1.97 ± 0.68 | 0.263 |
| Serum bicarbonate, mEq/L (mean ± SD) | 18.97 ± 3.54 | 21.30 ± 2.24 | 0.042 |
| LVEF, % (mean ± SD) | 30 ± 23.45 | 35 ± 12.79 | 0.927 |
| sPAP, mmHg (mean ± SD) | 34 ± 12.72 | 47.17 ± 20.76 | 0.186 |
| LAA, mm2 (mean ± SD) | 32.66 ± 8.77 | 26.48 ± 5.70 | 0.032 |
| MAPSE, mm (mean ± SD) | 9 ± 3.36 | 12.33 ± 2.74 | 0.239 |
| E/e′ > 15 (%) | 5 (55.6%) | 7 (46.7%) | 0.411 |
| Biomarker | AUC | Std. Error | Asymptotic 95% Confidence Interval | p-Value | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| MyBP-C (ng/L) | 0.972 | 0.021 | 0.000 | 1 | <0.001 |
| NT-proBNP (pg/mL) | 0.849 | 0.054 | 0.742 | 0.955 | 0.001 |
| hs-TnI (ng/L) | 0.714 | 0.078 | 0.560 | 0.868 | 0.047 |
| Biomarker | AUC | Std. Error | Asymptotic 95% Confidence Interval | p-Value | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| MyBP-C (ng/L) | 0.897 | 0.046 | 0.806 | 0.987 | <0.001 |
| NT-proBNP (pg/mL) | 0.750 | 0.070 | 0.614 | 0.886 | 0.012 |
| hs-TnI (ng/L) | 0.833 | 0.060 | 0.715 | 0.950 | 0.001 |
| Chi-Square | df | p-Value | |
|---|---|---|---|
| Log Rank (Mantel–Cox) | 35.191 | 1 | <0.001 |
| Test of equality of survival distributions for the different levels of MyBP-C | |||
| Predictor | Odd Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Death within 30 days | |||
| MyBP-C | 1.08 | 1.0–1.16 | 0.039 |
| NT-proBNP | 1.0 | 1.0–1.0 | 0.49 |
| hs-TnI | 1.0 | 0.99–1.0 | 0.09 |
| Composite of Death/Recurrent HF within 30 days | |||
| MyBP-C | 1.12 | 1.02–1.22 | 0.014 |
| NT-proBNP | 1.0 | 1.0–1.0 | 0.33 |
| hs-TnI | 1.0 | 1.0–1.0 | 0.48 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chetran, A.; Bădescu, M.C.; Şerban, I.L.; Duca, Ş.T.; Afrăsânie, I.; Cepoi, M.-R.; Dmour, B.A.; Matei, I.T.; Haba, M.Ş.C.; Costache, A.D.; et al. Insights into the Novel Cardiac Biomarker in Acute Heart Failure: Mybp-C. Life 2024, 14, 513. https://doi.org/10.3390/life14040513
Chetran A, Bădescu MC, Şerban IL, Duca ŞT, Afrăsânie I, Cepoi M-R, Dmour BA, Matei IT, Haba MŞC, Costache AD, et al. Insights into the Novel Cardiac Biomarker in Acute Heart Failure: Mybp-C. Life. 2024; 14(4):513. https://doi.org/10.3390/life14040513
Chicago/Turabian StyleChetran, Adriana, Minerva Codruţa Bădescu, Ionela Lăcrămioara Şerban, Ştefania Teodora Duca, Irina Afrăsânie, Maria-Ruxandra Cepoi, Bianca Ana Dmour, Iulian Theodor Matei, Mihai Ştefan Cristian Haba, Alexandru Dan Costache, and et al. 2024. "Insights into the Novel Cardiac Biomarker in Acute Heart Failure: Mybp-C" Life 14, no. 4: 513. https://doi.org/10.3390/life14040513
APA StyleChetran, A., Bădescu, M. C., Şerban, I. L., Duca, Ş. T., Afrăsânie, I., Cepoi, M.-R., Dmour, B. A., Matei, I. T., Haba, M. Ş. C., Costache, A. D., Mitu, O., Cianga, C. M., Tuchiluş, C., Constantinescu, D., & Costache-Enache, I. I. (2024). Insights into the Novel Cardiac Biomarker in Acute Heart Failure: Mybp-C. Life, 14(4), 513. https://doi.org/10.3390/life14040513










