How Old Is Too Old? Outcomes of Prolapse Native-Tissue Repair through Uterosacral Suspension in Octogenarians
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weintraub, A.Y.; Glinter, H.; Marcus-Braun, N. Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic organ prolapse. Int. Braz. J. Urol. 2020, 46, 5–14. [Google Scholar] [CrossRef]
- Barber, M.D.; Maher, C. Epidemiology and outcome assessment of pelvic organ prolapse. Int. Urogynecol. J. 2013, 24, 1783–1790. [Google Scholar] [CrossRef]
- Wu, J.M.; Hundley, A.F.; Fulton, R.G.B.; Myers, E.R. Forecasting the Prevalence of Pelvic Floor Disorders in U.S. Women. Obstet. Gynecol. 2009, 114, 1278–1283. [Google Scholar] [CrossRef]
- Santoro, G.A.; Wieczorek, A.P.; Dietz, H.P.; Mellgren, A.; Sultan, A.H.; Shobeiri, S.A.; Stankiewicz, A.; Bartram, C. State of the art: An integrated approach to pelvic floor ultrasonography. Ultrasound Obstet. Gynecol. 2010, 37, 381–396. [Google Scholar] [CrossRef]
- Bump, R.C.; Mattiasson, A.; Bø, K.; Brubaker, L.P.; DeLancey, J.O.; Klarskov, P.; Shull, B.L.; Smith, A.R. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am. J. Obstet. Gynecol. 1996, 175, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Committee on Practice Bulletins—Gynecology and the American Urogynecologic Society. Practice Bulletin No. 176: Pelvic Organ Prolapse. Obstet. Gynecol. 2017, 129, e56–e72. [Google Scholar] [CrossRef] [PubMed]
- Filocamo, M.T.; Serati, M.; Marzi, V.L.; Costantini, E.; Milanesi, M.; Pietropaolo, A.; Polledro, P.; Gentile, B.; Maruccia, S.; Fornia, S.; et al. The Female Sexual Function Index (FSFI): Linguistic Validation of the Italian Version. J. Sex. Med. 2014, 11, 447–453. [Google Scholar] [CrossRef] [PubMed]
- Barba, M.; Cola, A.; Melocchi, T.; Braga, A.; Castronovo, F.; Manodoro, S.; Pennacchio, M.; Munno, G.M.; Ruffolo, A.F.; Degliuomini, R.S.; et al. Italian validation of the Pelvic Floor Distress Inventory (PFDI-20) questionnaire. Int. Urogynecol. J. 2023, 34, 2459–2465. [Google Scholar] [CrossRef] [PubMed]
- Handa, V.L.; Garrett, E.; Hendrix, S.; Gold, E.; Robbins, J. Progression and remission of pelvic organ prolapse: A longitudinal study of menopausal women. Am. J. Obstet. Gynecol. 2004, 190, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Lowder, J.L.; Ghetti, C.; Nikolajski, C.; Oliphant, S.S.; Zyczynski, H.M. Body image perceptions in women with pelvic organ prolapse: A qualitative study. Am. J. Obstet. Gynecol. 2011, 204, 441.e1–441.e5. [Google Scholar] [CrossRef] [PubMed]
- Jelovsek, J.E.; Maher, C.; Barber, M.D. Pelvic organ prolapse. Lancet 2007, 369, 1027–1038. [Google Scholar] [CrossRef] [PubMed]
- Ellerkmann, R.M.; Cundiff, G.W.; Melick, C.F.; Nihira, M.A.; Leffler, K.; Bent, A.E. Correlation of symptoms with location and severity of pelvic organ prolapse. Am. J. Obstet. Gynecol. 2001, 185, 1332–1338. [Google Scholar] [CrossRef]
- Marinkovic, S.P.; Stanton, S.L. Incontinence and Voiding Difficulties Associated With Prolapse. J. Urol. 2004, 171, 1021–1028. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.M.; Dieter, A.A.; Pate, V.; Funk, M.J. Cumulative Incidence of a Subsequent Surgery After Stress Urinary Incontinence and Pelvic Organ Prolapse Procedure. Obstet. Gynecol. 2017, 129, 1124–1130. [Google Scholar] [CrossRef] [PubMed]
- Mouritsen, L.; Larsen, J.P. Symptoms, bother and POPQ in women referred with pelvic organ prolapse. Int. Urogynecol. J. Pelvic. Floor. Dysfunct. 2003, 14, 122–127. [Google Scholar] [CrossRef]
- Elkadry, E.A.; Kenton, K.S.; FitzGerald, M.P.; Shott, S.; Brubaker, L. Patient-selected goals: A new perspective on surgical outcome. Am. J. Obstet. Gynecol. 2003, 189, 1551–1557. [Google Scholar] [CrossRef]
- Hullfish, K.L.; Bovbjerg, V.E.; Steers, W.D. Patient-centered goals for pelvic floor dysfunction surgery: Long-term follow-up. Am. J. Obstet. Gynecol. 2004, 191, 201–205. [Google Scholar] [CrossRef]
- Mahajan, S.T.; Elkadry, E.A.; Kenton, K.S.; Shott, S.; Brubaker, L. Patient-centered surgical outcomes: The impact of goal achievement and urge incontinence on patient satisfaction one year after surgery. Am. J. Obstet. Gynecol. 2006, 194, 722–728. [Google Scholar] [CrossRef]
- Jones, K.A.; Shepherd, J.P.; Oliphant, S.S.; Wang, L.; Bunker, C.H.; Lowder, J.L. Trends in inpatient prolapse procedures in the United States, 1979–2006. Am. J. Obstet. Gynecol. 2010, 202, 501.e1–501.e7. [Google Scholar] [CrossRef]
- Kurkijärvi, K.; Aaltonen, R.; Gissler, M.; Mäkinen, J. Pelvic organ prolapse surgery in Finland from 1987 to 2009: A national register based study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 214, 71–77. [Google Scholar] [CrossRef]
- Asante, A.; Whiteman, M.K.; Kulkarni, A.; Cox, S.; Marchbanks, P.A.; Jamieson, D.J. Elective oophorectomy in the United States: Trends and in-hospital complications, 1998–2006. Obstet. Gynecol. 2010, 116, 1088–1095. [Google Scholar] [CrossRef] [PubMed]
- Thiyagarajan, J.A.; Mikton, C.; Harwood, R.H.; Gichu, M.; Gaigbe-Togbe, V.; Jhamba, T.; Pokorna, D.; Stoevska, V.; Hada, R.; Steffan, G.S.; et al. The UN Decade of healthy ageing: Strengthening measurement for monitoring health and wellbeing of older people. Age Ageing 2022, 51, afac147. [Google Scholar] [CrossRef] [PubMed]
- Chapman, G.C.; Sheyn, D.; Slopnick, E.A.; Hijaz, A.K.; Mahajan, S.T.; Mangel, J.; El-Nashar, S.A. Perioperative Safety of Surgery for Pelvic Organ Prolapse in Elderly and Frail Patients. Obstet. Gynecol. 2020, 135, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Stepp, K.J.; Barber, M.D.; Yoo, E.-H.; Whiteside, J.L.; Paraiso, M.F.R.; Walters, M.D. Incidence of perioperative complications of urogynecologic surgery in elderly women. Am. J. Obstet. Gynecol. 2005, 192, 1630–1636. [Google Scholar] [CrossRef] [PubMed]
- Suskind, A.M.; Jin, C.; Walter, L.C.; Finlayson, E. Frailty and the Role of Obliterative versus Reconstructive Surgery for Pelvic Organ Prolapse: A National Study. J. Urol. 2017, 197, 1502–1506. [Google Scholar] [CrossRef] [PubMed]
- Yadav, G.S.; Chapman, G.C.; Raju, R.; El-Nashar, S.A.; Occhino, J.A. Perioperative outcomes of reconstructive surgery for apical prolapse in the very elderly: A national contemporary analysis. Int. Urogynecol. J. 2021, 32, 1391–1398. [Google Scholar] [CrossRef] [PubMed]
- Haylen, B.T.; de Ridder, D.; Freeman, R.M.; Swift, S.E.; Berghmans, B.; Lee, J.; Monga, A.; Petri, E.; Rizk, D.E.; Sand, P.K.; et al. An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol. Urodyn. 2010, 29, 4–20. [Google Scholar] [CrossRef]
- Spelzini, F.; Frigerio, M.; Manodoro, S.; Interdonato, M.L.; Cesana, M.C.; Verri, D.; Fumagalli, C.; Sicuri, M.; Nicoli, E.; Polizzi, S.; et al. Modified McCall culdoplasty versus Shull suspension in pelvic prolapse primary repair: A retrospective study. Int. Urogynecol. J. 2016, 28, 65–71. [Google Scholar] [CrossRef]
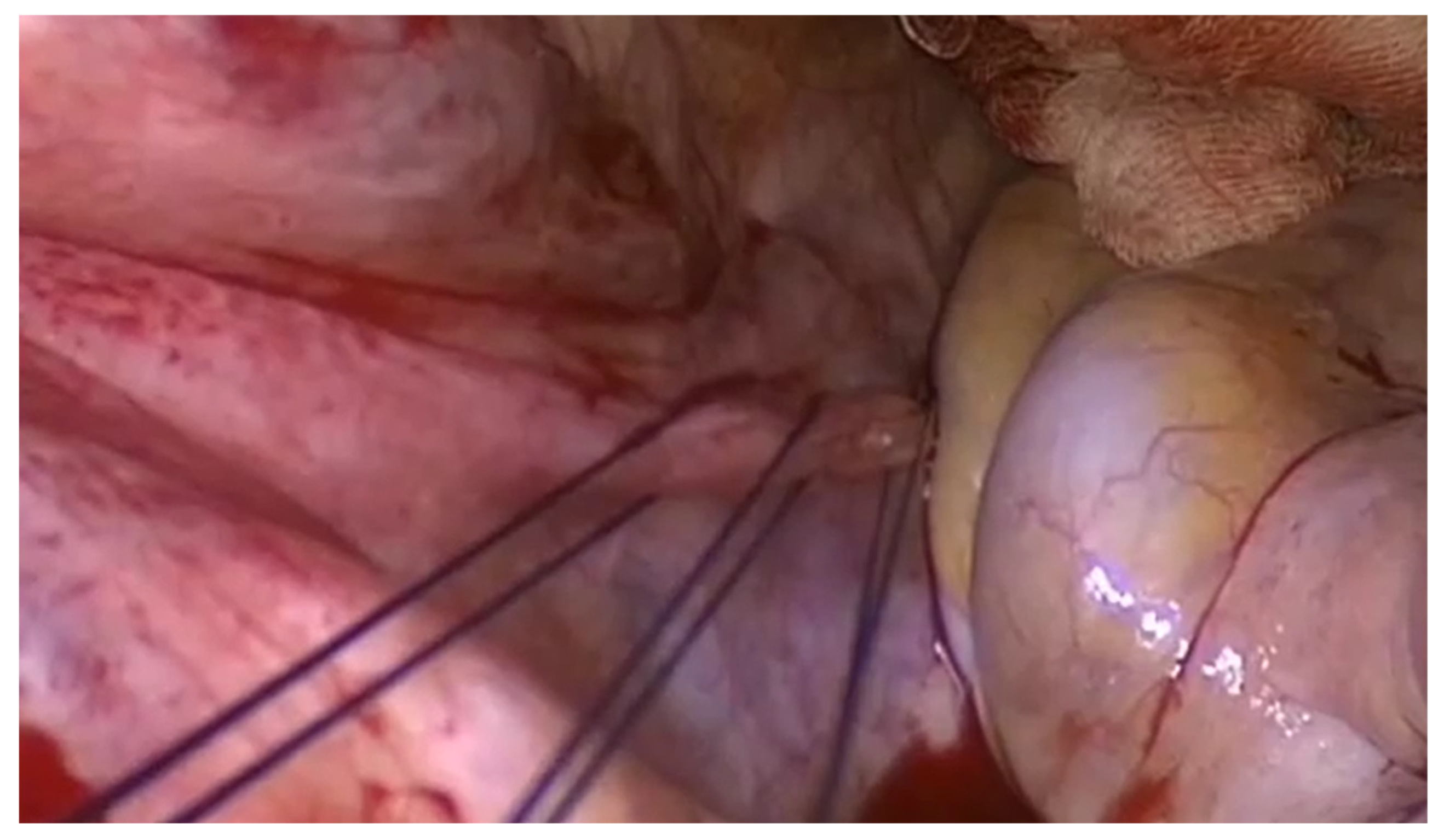
- Manodoro, S.; Frigerio, M.; Milani, R.; Spelzini, F. Tips and tricks for uterosacral ligament suspension: How to avoid ureteral injury. Int. Urogynecol. J. 2017, 29, 161–163. [Google Scholar] [CrossRef]
- Manodoro, S.; Spelzini, F.; Frigerio, M.; Nicoli, E.; Verri, D.; Milani, R. Is Occult Stress Urinary Incontinence a Reliable Predictive Marker? Female Pelvic. Med. Reconstr. Surg. 2016, 22, 280–282. [Google Scholar] [CrossRef]
- Milani, R.; Manodoro, S.; Cola, A.; Palmieri, S.; Frigerio, M. Transvaginal levator myorrhaphy for posthysterectomy vaginal vault prolapse repair. Int. Urogynecol. J. 2017, 29, 913–915. [Google Scholar] [CrossRef] [PubMed]
- Cola, A.; Marino, G.; Milani, R.; Barba, M.; Volontè, S.; Spelzini, F.; Manodoro, S.; Frigerio, M. Native-tissue prolapse repair: Efficacy and adverse effects of uterosacral ligaments suspension at 10-year follow up. Int. J. Gynecol. Obstet. 2022, 159, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Deo, G.; Bernasconi, D.P.; Cola, A.; Palmieri, S.; Spelzini, F.; Milani, R.; Manodoro, S.; Frigerio, M. Long-term outcomes and five-year recurrence-free survival curves after native-tissue prolapse repair. Int. J. Gynecol. Obstet. 2019, 147, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Duan, L.; Lu, Y.X.; Shen, W.J.; Liu, X.; Liu, J.X.; Zhang, Y.H.; Ge, J.; Zhao, Y.; Niu, K.; Wang, W.Y. Long-term effectiveness of transvaginal high uterosacral ligament suspension. Zhonghua Fu Chan Ke Za Zhi 2017, 52, 363–368. (In Chinese) [Google Scholar] [CrossRef] [PubMed]
- Schiavi, M.C.; Savone, D.; Di Mascio, D.; Di Tucci, C.; Perniola, G.; Zullo, M.A.; Muzii, L.; Panici, P.B. Long-term experience of vaginal vault prolapse prevention at hysterectomy time by modified McCall culdoplasty or Shull suspension: Clinical, sexual and quality of life assessment after surgical intervention. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 223, 113–118. [Google Scholar] [CrossRef]
- Doumouchtsis, S.K.; Chrysanthopoulou, E.L. Urogenital consequences in ageing women. Best Pr. Res. Clin. Obstet. Gynaecol. 2013, 27, 699–714. [Google Scholar] [CrossRef]
- Silva, W.A.; Pauls, R.N.; Segal, J.L.; Rooney, C.M.; Kleeman, S.D.; Karram, M.M. Uterosacral ligament vault suspension: Five-year outcomes. Obstet. Gynecol. 2006, 108, 255–263. [Google Scholar] [CrossRef]
- Marino, G.; Frigerio, M.; Barba, M.; Melocchi, T.; De Vicari, D.; Braga, A.; Serati, M.; Maggiore, U.L.R.; Ruffolo, A.F.; Salvatore, S.; et al. Native Tissue Posterior Compartment Repair for Isolated Posterior Vaginal Prolapse: Anatomical and Functional Outcomes. Medicina 2022, 58, 1152. [Google Scholar] [CrossRef]
- Capobianco, G.; Sechi, I.; Muresu, N.; Saderi, L.; Piana, A.; Farina, M.; Dessole, F.; Virdis, G.; De Vita, D.; Madonia, M.; et al. Native tissue repair (NTR) versus transvaginal mesh interventions for the treatment of anterior vaginal prolapse: Systematic review and meta-analysis. Maturitas 2022, 165, 104–112. [Google Scholar] [CrossRef]
- Margulies, R.U.; Rogers, M.A.; Morgan, D.M. Outcomes of transvaginal uterosacral ligament suspension: Systematic review and metaanalysis. Am. J. Obstet. Gynecol. 2010, 202, 124–134. [Google Scholar] [CrossRef]
| Mean age | 81.3 ± 1.9 |
| BMI (kg/m2) | 24.7 ± 3.6 |
| Parity | 2.2 ± 1.0 |
| Maximum child weight (g) | 3637.4 ± 562.1 |
| Menopause | 65 (100%) |
| Mean age of menopause onset | 50.7 ± 3.6 |
| Sexually active | 2 (3.07%) |
| Preoperative | Postoperative | p-Value | |
|---|---|---|---|
| Aa | +1.6 ± 1.3 | −2.3 ± 0.8 | <0.0001 |
| Ba | +1.9 ± 1.4 | −2.4 ± 0.8 | <0.0001 |
| C | +0.9± 2.5 | −6.9 ± 2.0 | <0.0001 |
| Gh | 3.6 ± 0.6 | 3.2 ± 0.7 | 0.0002 |
| Pb | 2.9 ± 0.4 | 2.8 ± 0.4 | 0.1522 |
| Tvl | 9.9 ± 1.2 | 8.4 ± 0.4 | <0.0001 |
| Ap | −1.2 ± 1.6 | −2.7 ± 0.6 | <0.0001 |
| Bp | −1.2± 1.7 | −2.7 ± 0.6 | <0.0001 |
| D | −3.9 ± 2.9 | / | N/A |
| Stress urinary incontinence | 17 (26.1%) | 12 (18.4%) | 0.2786 |
| Overactive bladder syndrome | 21 (32.3%) | 14 (21.5%) | 0.1276 |
| Urge urinary incontinence | 19 (29.2%) | 7 (10.7%) | 0.0094 |
| Voiding symptoms | 38 (58.4%) | 8 (12.3%) | <0.0001 |
| Sexual activity | 2 (3.7%) | 6 (9.2%) | 0.0832 |
| Constipation | 17 (26.1%) | 11 (16.9%) | <0.0001 |
| Bulging symptoms | 65 (100%) | 0 | <0.0001 |
| Vaginal hysterectomy | 65 (100%) |
| Uterosacral ligaments suspension | 65 (100%) |
| Anterior repair | 63 (96.9%) |
| Posterior repair | 44 (67.6%) |
| Mean blood loss | 243.8 ± 149.1 |
| Blood loss ≥ 500 mL | 8 (12.3%) |
| Mean operative time in minutes | 100.8 ± 25.9 |
| Anatomic recurrence | 7 (10.7%) |
| Anterior compartment relapse | 5 (7.7%) |
| Central compartment relapse | 1 (1.5%) |
| Posterior compartment relapse | 3 (4.6%) |
| Mean follow-up time (months) | 23 ± 20 |
| Reoperation | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barba, M.; Cola, A.; De Vicari, D.; Costa, C.; Volontè, S.; Frigerio, M. How Old Is Too Old? Outcomes of Prolapse Native-Tissue Repair through Uterosacral Suspension in Octogenarians. Life 2024, 14, 433. https://doi.org/10.3390/life14040433
Barba M, Cola A, De Vicari D, Costa C, Volontè S, Frigerio M. How Old Is Too Old? Outcomes of Prolapse Native-Tissue Repair through Uterosacral Suspension in Octogenarians. Life. 2024; 14(4):433. https://doi.org/10.3390/life14040433
Chicago/Turabian StyleBarba, Marta, Alice Cola, Desirèe De Vicari, Clarissa Costa, Silvia Volontè, and Matteo Frigerio. 2024. "How Old Is Too Old? Outcomes of Prolapse Native-Tissue Repair through Uterosacral Suspension in Octogenarians" Life 14, no. 4: 433. https://doi.org/10.3390/life14040433
APA StyleBarba, M., Cola, A., De Vicari, D., Costa, C., Volontè, S., & Frigerio, M. (2024). How Old Is Too Old? Outcomes of Prolapse Native-Tissue Repair through Uterosacral Suspension in Octogenarians. Life, 14(4), 433. https://doi.org/10.3390/life14040433









