Arthrocentesis of Temporomandibular Joints—A Clinical Comparative Study
Abstract
1. Introduction
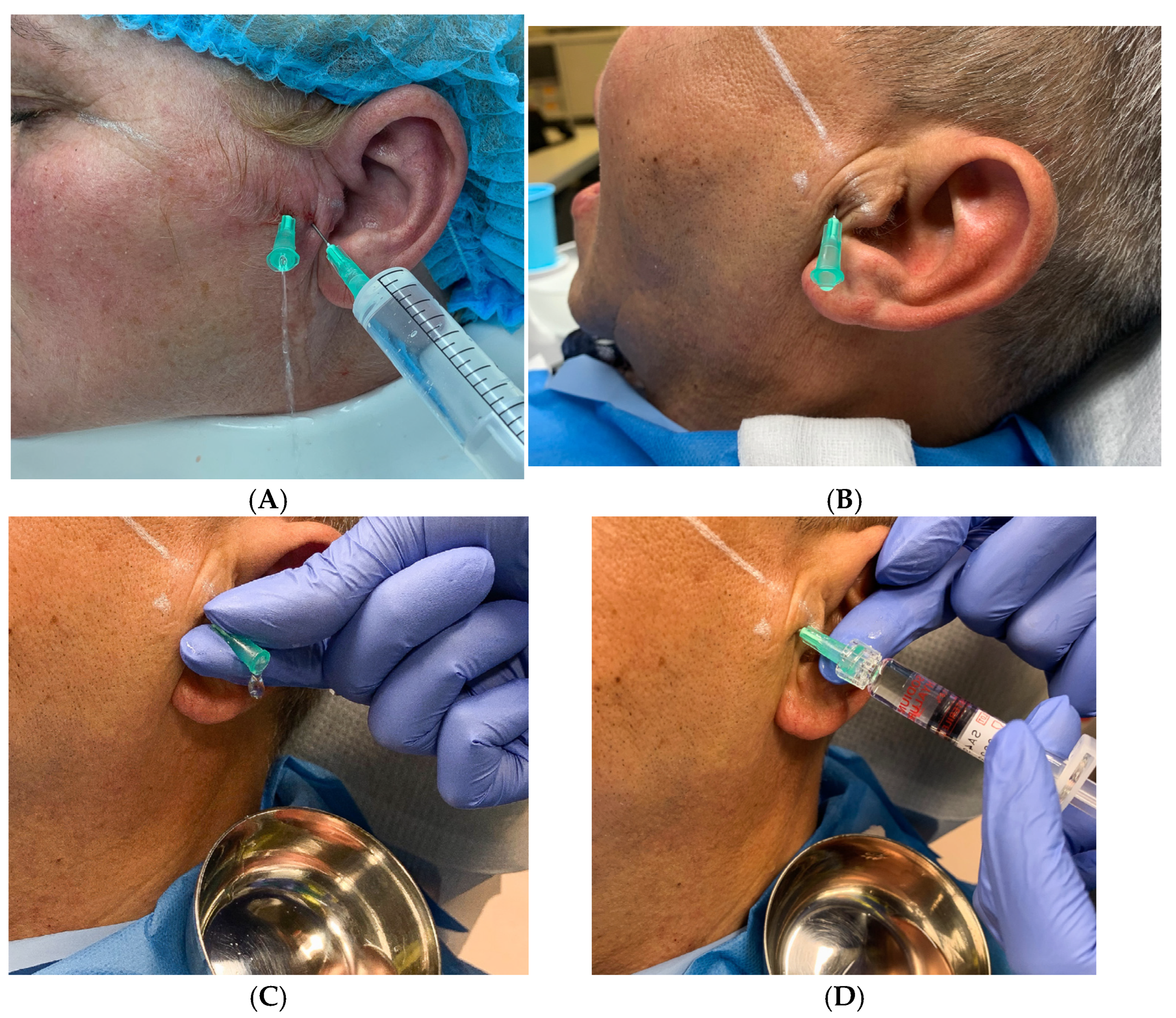
2. Materials and Methods
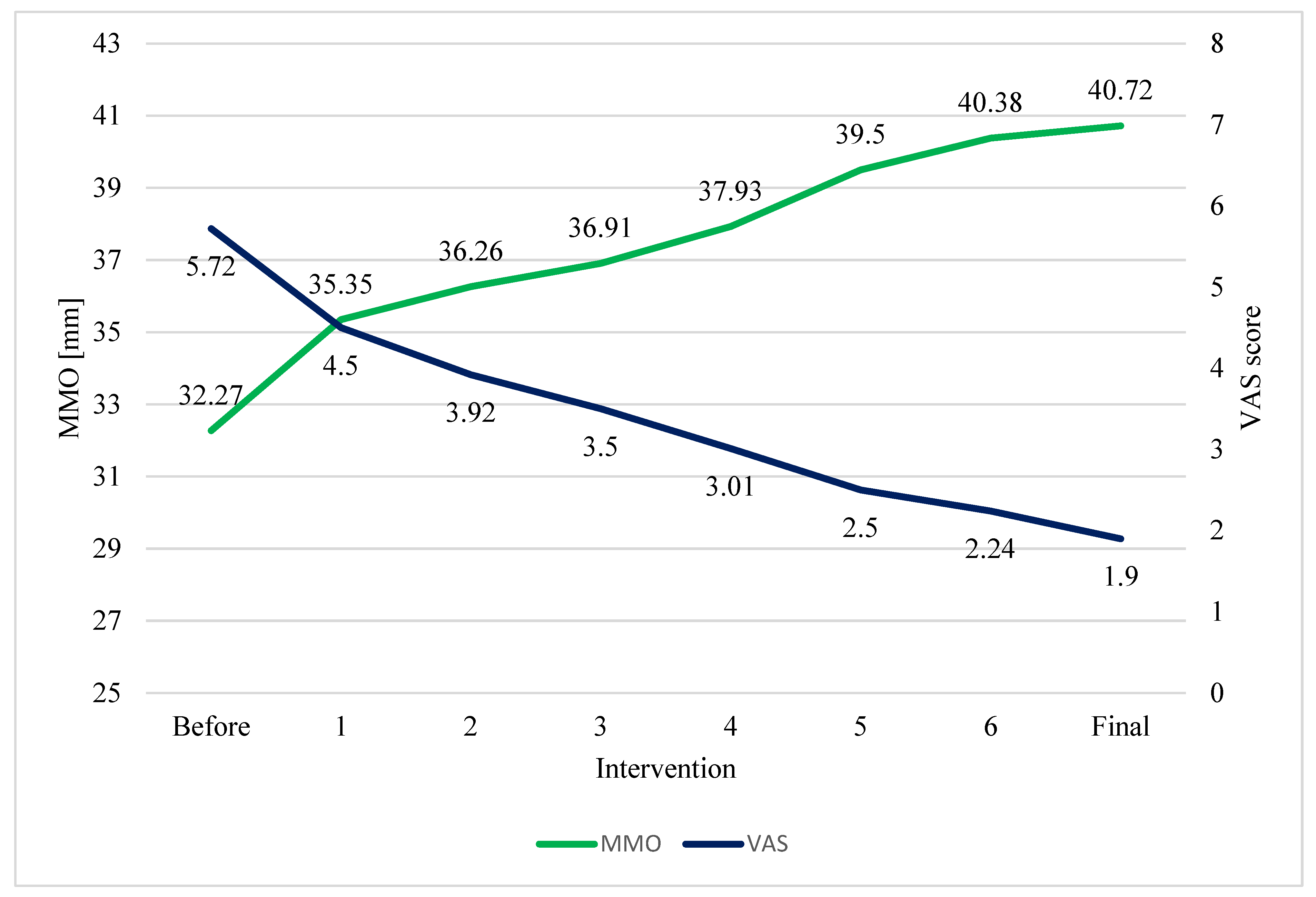
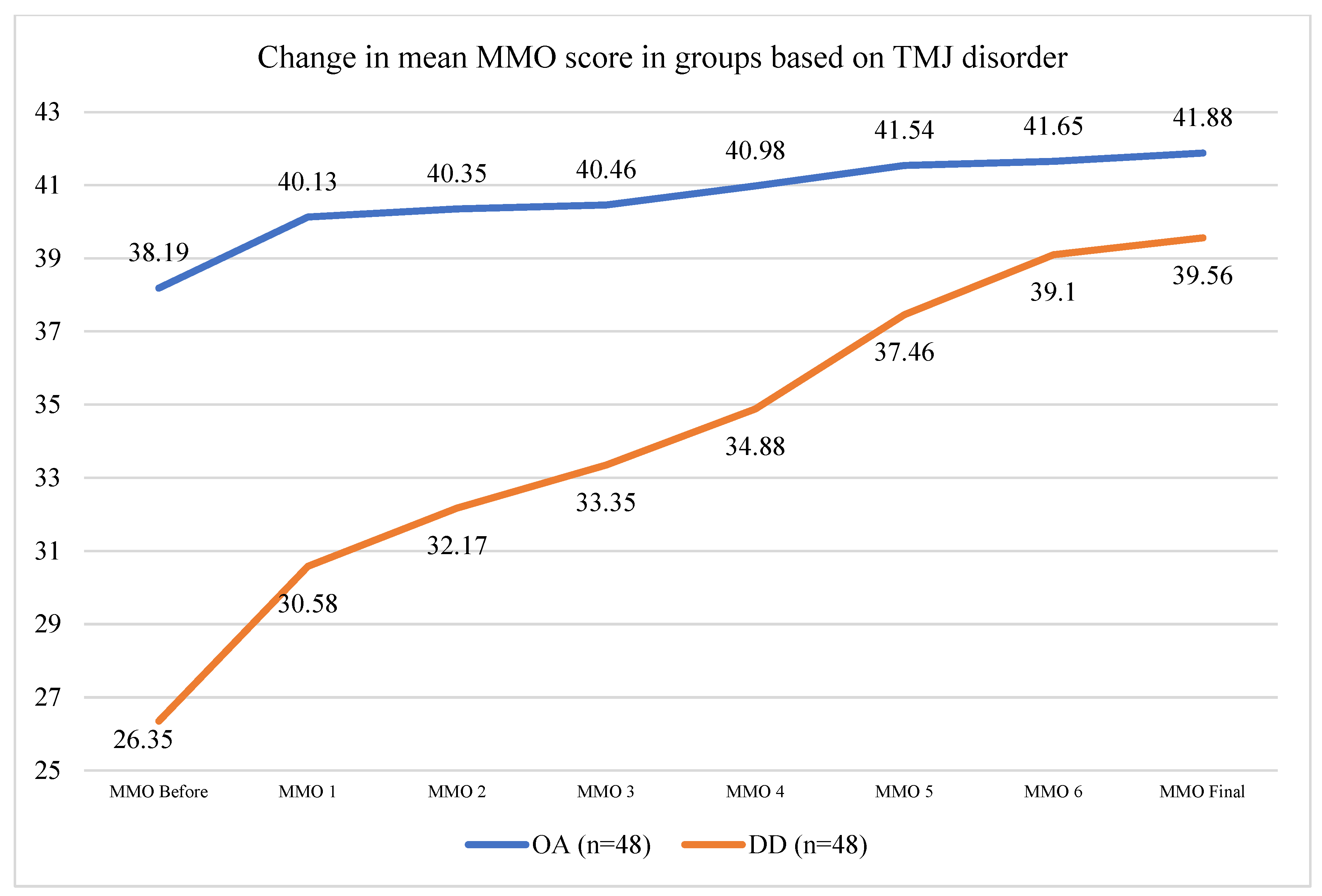
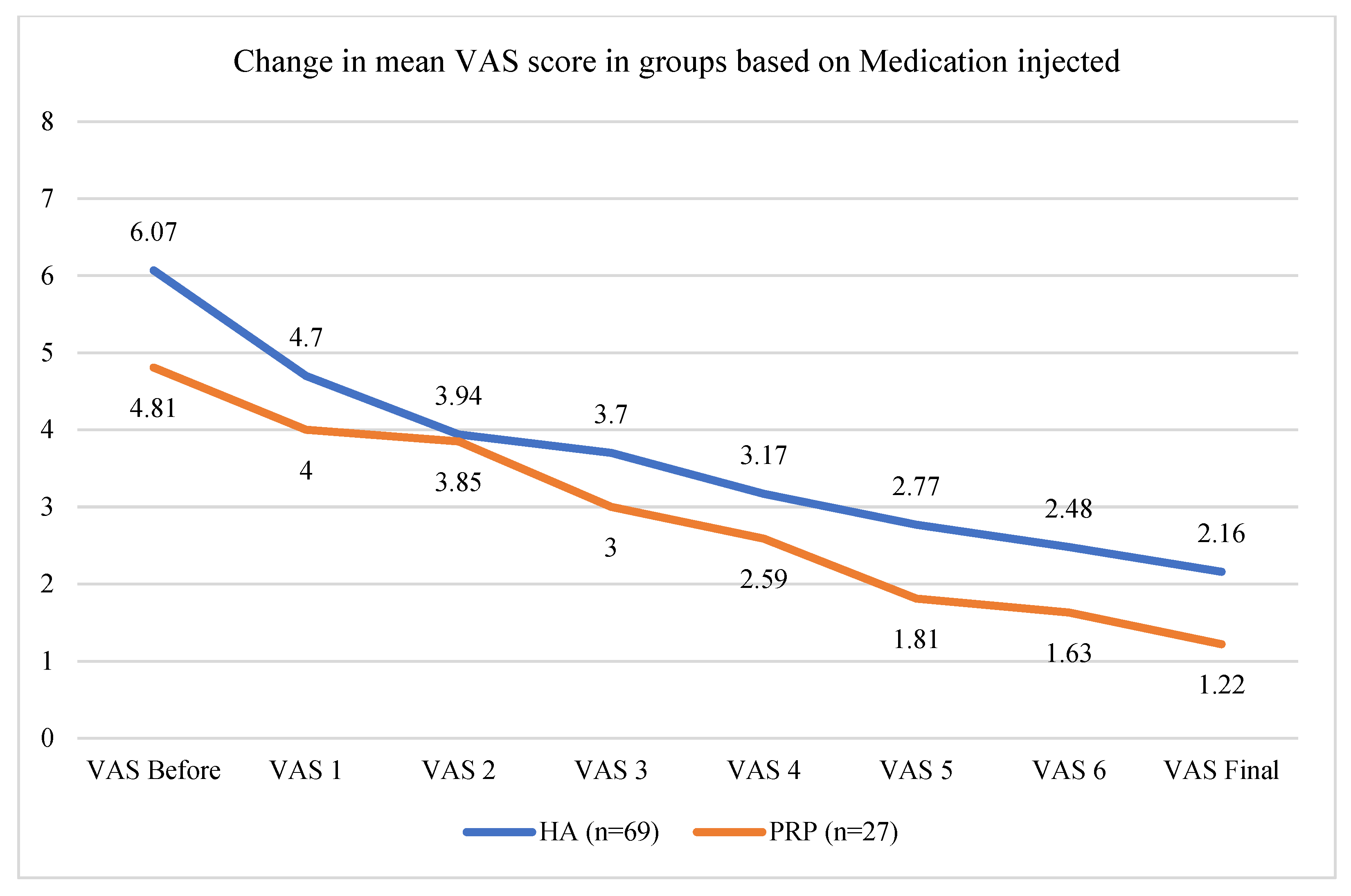
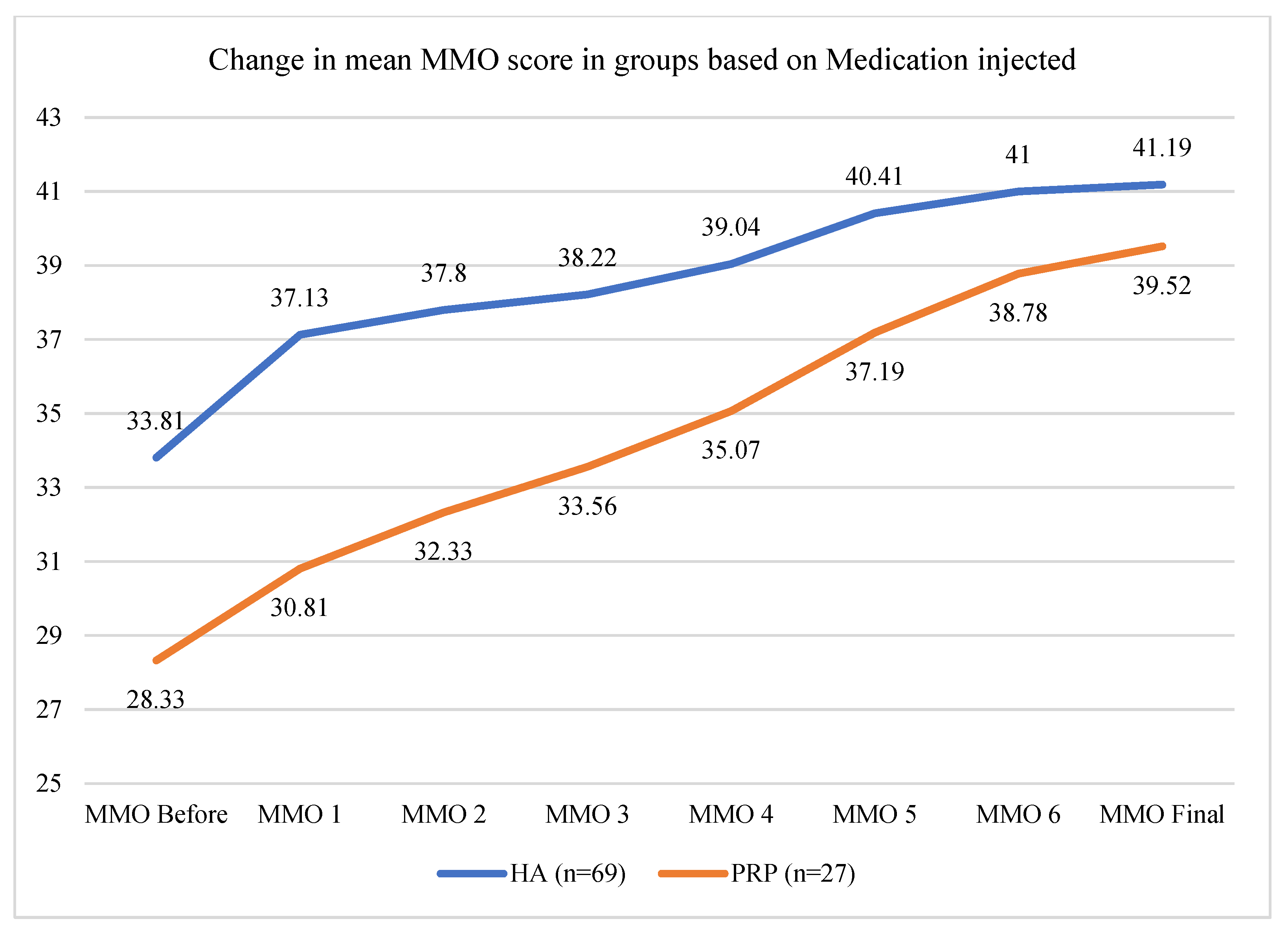
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Manfredini, D. Etiopathogenesis of disk displacement of the temporomandibular joint: A review of the mechanisms. Indian J. Dent. Res. 2009, 20, 212–221. [Google Scholar] [CrossRef]
- Poluha, R.L.; De La Torre Canales, G.; Costa, Y.M.; Grossmann, E.; Bonjardim, L.R.; Conti, P.C.R. Temporomandibular joint disc displacement with reduction: A review of mechanisms and clinical presentation. J. Appl. Oral Sci. 2019, 27, e20180433. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Ren, X.; Lin, P.; Jin, S.; Zhang, Z. Exploring the causal effects of sleep characteristics on TMD-related pain: A two-sample Mendelian randomization study. Clin. Oral Investig. 2024, 28, 384. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, A.A.; Saini, R.S.; Okshah, A.; Alhadidi, A.A.F.; Kanji, M.A.; Vyas, R.; Binduhayyim, R.I.H.; Ahmed, N.; Mosaddad, S.A.; Heboyan, A. The association between genetic factors and temporomandibular disorders: A systematic literature review. Arch. Oral Biol. 2024, 166, 106032. [Google Scholar] [CrossRef]
- Yap, A.U.; Lei, J.; Liu, C.; Fu, K.Y. Characteristics of painful temporomandibular disorders and their influence on jaw functional limitation and oral health-related quality of life. J. Oral Rehabil. 2024, 51, 1748–1758. [Google Scholar] [CrossRef] [PubMed]
- Que, H.; Zhang, Q.; Xu, S.; Chu, T.; Xu, L.; Wang, Y. Bi-directional two-sample Mendelian randomization identifies causal association of depression with temporomandibular disorders. J. Oral Rehabil. 2024, 51, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Warzocha, J.; Gadomska-Krasny, J.; Mrowiec, J. Etiologic Factors of Temporomandibular Disorders: A Systematic Review of Literature Containing Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) and Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) from 2018 to 2022. Healthcare 2024, 12, 575. [Google Scholar] [CrossRef]
- Asadauskas, A.; Luedi, M.M.; Urman, R.D.; Andereggen, L. Modern Approaches to the Treatment of Acute Facial Pain. Curr. Pain Headache Rep. 2024, 28, 793–801. [Google Scholar] [CrossRef]
- Nitzan, D.W.; Dolwick, M.F.; Martinez, G.A. Temporomandibular joint arthrocentesis: A simplified treatment for severe, limited mouth opening. J. Oral Maxillofac. Surg. 1991, 49, 1163–1167. [Google Scholar] [CrossRef]
- Singh, S.; Varghese, D. Single puncture arthrocentesis of temporomandibular joint; introducing a novel device: A pilot study. Natl. J. Maxillofac. Surg. 2013, 4, 193. [Google Scholar] [CrossRef]
- Murakami, K.I.; Matsuki, M.; Iizuka, T.; Ono, T. Recapturing the persistent anteriorly displaced disk by mandibular manipulation after pumping and hydraulic pressure to the upper joint cavity of the temporomandibular joint. Cranio 1987, 5, 17. [Google Scholar] [CrossRef] [PubMed]
- Alowaimer, H.A.; Al Shutwi, S.S.; Alsaegh, M.K.; Alruwaili, O.M.; Alrashed, A.R.; AlQahtani, S.H.; Batais, M.S. Comparative Efficacy of Non-Invasive Therapies in Temporomandibular Joint Dysfunction: A Systematic Review. Cureus 2024, 16, e56713. [Google Scholar] [CrossRef] [PubMed]
- Tran, C.; Ghahreman, K.; Huppa, C.; Gallagher, J.E. Management of temporomandibular disorders: A rapid review of systematic reviews and guidelines. Int. J. Oral Maxillofac. Surg. 2022, 51, 1211–1225. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.M.; Yun, J.; Zhou, T.Q.; Zhang, Y.; Gao, C. Arthrocentesis for temporomandibular joint disorders: A network meta-analysis of randomised controlled trials. BMC Oral Health 2024, 24, 1108. [Google Scholar] [CrossRef]
- Nitzan, D.W. Arthrocentesis--incentives for using this minimally invasive approach for temporomandibular disorders. Oral Maxillofac. Surg. Clin. N. Am. 2006, 18, 311–328. [Google Scholar] [CrossRef]
- McCain, J.P. Arthroscopy of the human temporomandibular joint. J. Oral Maxillofac. Surg. 1988, 46, 648–655. [Google Scholar] [CrossRef]
- Delgado, D.A.; Lambert, B.S.; Boutris, N.; McCulloch, P.C.; Robbins, A.B.; Moreno, M.R.; Harris, J.D. Validation of Digital Visual Analog Scale Pain Scoring With a Traditional Paper-based Visual Analog Scale in Adults. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2018, 2, e088. [Google Scholar] [CrossRef]
- Eriksson, L.; Westesson, P.L. Discectomy as an effective treatment for painful temporomandibular joint internal derangement: A 5-year clinical and radiographic follow-up. J. Oral Maxillofac. Surg. 2001, 59, 750–758. [Google Scholar] [CrossRef]
- Ângelo, D.F.; Lopes, C.S.; Sanz, D.; Faria-Teixeira, M.C.; Marques, R.; Maffia, F.; Cardoso, H.J. Temporomandibular Joint Minimally Invasive Procedures in the Pediatric Population: A Prospective Study. J. Clin. Med. 2024, 13, 672. [Google Scholar] [CrossRef]
- d’Apuzzo, F.; Rotolo, R.P.; Fordellone, M.; Cuomo, G.; Jamilian, A.; Nucci, L.; Grassia, V. Temporomandibular Disorders and Serological Tests in Patients with Rheumatoid Arthritis. Appl. Sci. 2023, 13, 11488. [Google Scholar] [CrossRef]
- Yan, Q.; Liao, L.; He, D. Risk factors associated with temporomandibular joint disorder: A mendelian randomization analysis. J. Oral Rehabil. 2024, 51, 2239–2247. [Google Scholar] [CrossRef] [PubMed]
- van der Meer, H.A.; van der Wal, A.C.; van Hinte, G.; Speksnijder, C.M. Counselling for patients with a temporomandibular disorder: A scoping review and concept analysis. J. Oral Rehabil. 2024, 51, 2484–2497. [Google Scholar] [CrossRef] [PubMed]
- Houck, J.; Patel, S.S.; Desai, B.K. Arthrocentesis. In Atlas of Emergency Medicine Procedures, 2nd ed.; Springer Nature: Cham, Switzerland, 2023; pp. 555–559. [Google Scholar] [CrossRef]
- Grossmann, E.; Guilherme Vargas Pasqual, P.; Poluha, R.L.; Iwaki, L.C.V.; Iwaki Filho, L.; Setogutti, Ê.T. Single-Needle Arthrocentesis with Upper Compartment Distension versus Conventional Two-Needle Arthrocentesis: Randomized Clinical Trial. Pain Res. Manag. 2017, 2017, 2435263. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.W.; Lee, S.J.; Kim, E.H.; Lee, D.K.; Kang, M.H.; Song, I.S.; Jun, S.H. Effect of arthrocentesis on the clinical outcome of various treatment methods for temporomandibular joint disorders. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 44. [Google Scholar] [CrossRef] [PubMed]
- Santagata, M.; De Luca, R.; Lo Giudice, G.; Troiano, A.; Lo Giudice, G.; Corvo, G.; Tartaro, G. Arthrocentesis and sodium hyaluronate infiltration in temporomandibular disorders treatment. Clinical and MRI evaluation. J. Funct. Morphol. Kinesiol. 2020, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Rossini, R.; Grossmann, E.; Poluha, R.L.; Setogutti, Ê.T.; Dos Santos, M.F. Double-Needle Arthrocentesis with Viscosupplementation in Patients with Temporomandibular Joint Disc Displacement without Reduction. Clinics 2021, 76, e2840. [Google Scholar] [CrossRef]
- Sequeira, J.; Rao, B.H.S.; Kedia, P.R. Efficacy of Sodium Hyaluronate for Temporomandibular Joint Disorder by Single-Puncture Arthrocentesis. J. Maxillofac. Oral Surg. 2019, 18, 88. [Google Scholar] [CrossRef]
- Monteiro, J.L.G.C.; Almeida de Arruda, J.A.; Dias de Oliveira e Silva, E.; Cavalcanti do Egito Vasconcelos, B. Is Single-Puncture TMJ Arthrocentesis Superior to the Double-Puncture Technique for the Improvement of Outcomes in Patients With TMDs? J. Oral Maxillofac. Surg. 2020, 78, 1319.e1–1319.e15. [Google Scholar] [CrossRef]
- Siewert-Gutowska, M.; Pokrowiecki, R.; Kamiński, A.; Zawadzki, P.; Stopa, Z. State of the Art in Temporomandibular Joint Arthrocentesis—A Systematic Review. J. Clin. Med. 2023, 12, 4439. [Google Scholar] [CrossRef]
- Guarda-Nardini, L.; De Almeida, A.; Manfredini, D. Arthrocentesis of the Temporomandibular Joint: Systematic Review and Clinical Implications of Research Findings. J. Oral Facial Pain Headache 2021, 35, 17–29. [Google Scholar] [CrossRef]
- Nagori, S.A.; Roy Chowdhury, S.K.; Thukral, H.; Jose, A.; Roychoudhury, A. Single puncture versus standard double needle arthrocentesis for the management of temporomandibular joint disorders: A systematic review. J. Oral Rehabil. 2018, 45, 810–818. [Google Scholar] [CrossRef] [PubMed]
- Navaneetham, R.; Navaneetham, A.; Nagaraj, V.; Gnapika, N.; Sankarnarayan, G. Single-Puncture Versus Double-Puncture Technique Arthrocentesis in the Treatment of Internal Derangement of TM Joint-A Comparative Clinical Study. J. Maxillofac. Oral Surg. 2023, 22, 1060–1065. [Google Scholar] [CrossRef] [PubMed]
- Nagori, S.A.; Jose, A.; Roychoudhury, A. Comparison of intraoperative outcomes with single and double puncture techniques of arthrocentesis of the temporomandibular joint. Br. J. Oral Maxillofac. Surg. 2020, 58, 928–932. [Google Scholar] [CrossRef] [PubMed]
- Grossmann, E.; Poluha, R.L. Double-Puncture Versus Single-Puncture Arthrocentesis: A Randomized Controlled Trial with 3 Years of Follow-Up. J. Oral Facial Pain Headache 2022, 36, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Lucchese, A.; Bondemark, L.; Marcolina, M.; Manuelli, M. Changes in oral microbiota due to orthodontic appliances: A systematic review. J. Oral Microbiol. 2018, 10, 1476645. [Google Scholar] [CrossRef]
- Cardoneanu, A.; Macovei, L.A.; Burlui, A.M.; Mihai, I.R.; Bratoiu, I.; Rezus, I.I.; Richter, P.; Tamba, B.-I.; Rezus, E. Temporomandibular Joint Osteoarthritis: Pathogenic Mechanisms Involving the Cartilage and Subchondral Bone, and Potential Therapeutic Strategies for Joint Regeneration. Int. J. Mol. Sci. 2023, 24, 171. [Google Scholar] [CrossRef]
- Cömert Kiliç, S.; Güngörmüş, M. Is arthrocentesis plus platelet-rich plasma superior to arthrocentesis plus hyaluronic acid for the treatment of temporomandibular joint osteoarthritis: A randomized clinical trial. Int. J. Oral Maxillofac. Surg. 2016, 45, 1538–1544. [Google Scholar] [CrossRef]

| Stage | Clinical Symptoms | Radiological Imaging | Group Assignment in the Study |
|---|---|---|---|
| 1. Early | Painless clicking; unrestricted function | Mild disc displacement; normal condyle | Disc displacement (DD) |
| 2. Early/Intermediate | Intermittent painful clicking and locking | Mild disc displacement and deformity; normal condyle | |
| 3. Intermediate | Frequent joint pain and locking; painful restricted function; chewing difficulties | Moderate disc displacement and deformity; normal condyle | |
| 4. Intermediate/Late | Chronic pain and restricted mandibular function | Severe disc displacement and deformity; abnormal condyle | Osteoarthritis (OA) |
| 5. Late | Severe joint dysfunction (crepitus) with variable pain | Severe disc displacement with perforation and deformity; degenerative condylar changes |
| VAS (on 0–10 Scale) | MMO | |
|---|---|---|
| Good | No pain or only mild pain: level ≤ 2 | ≥35 mm |
| Acceptable | No pain or only mild pain: level ≤ 2 | ≥30 mm and <35 mm |
| Insufficient | Constant or moderate pain: level > 2 | <30 mm |
| Frequency | % | ||
|---|---|---|---|
| TMJ disorder | OA | 48 | 50% |
| DD | 48 | 50% | |
| Medication injected | HA | 69 | 71.88% |
| PRP | 27 | 28.13% | |
| Treatment | 1-needle | 60 | 62.50% |
| 2-needle | 36 | 37.50% | |
| Intracapsular medication application | yes | 81 | 84.38% |
| no | 15 | 15.63% | |
| Further surgical treatment—arthroscopy | yes | 20 | 20.83% |
| no | 76 | 79.17% |
| Mean | Std. Deviation | Minimum | Maximum | Paired t-Test Results (Before and After the Treatment) | |
|---|---|---|---|---|---|
| Age | 43.58 | 16.45 | 18 | 87 | |
| Volume of fluid used (mL) | 37.6 | 11.9 | 25 | 60 | |
| VAS Before | 5.72 | 1.8 | 2 | 9 | t(96) = 15.286 p < 0.001 |
| VAS Final | 1.9 | 1.66 | 0 | 8 | |
| MMO Before | 32.27 | 8.11 | 18 | 46 | t(96) = −9.126 p < 0.001 |
| MMO Final | 40.72 | 4.07 | 26 | 48 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siewert, M.; Pokrowiecki, R.; Zawadzki, P.J.; Stopa, Z. Arthrocentesis of Temporomandibular Joints—A Clinical Comparative Study. Life 2024, 14, 1594. https://doi.org/10.3390/life14121594
Siewert M, Pokrowiecki R, Zawadzki PJ, Stopa Z. Arthrocentesis of Temporomandibular Joints—A Clinical Comparative Study. Life. 2024; 14(12):1594. https://doi.org/10.3390/life14121594
Chicago/Turabian StyleSiewert, Marta, Rafał Pokrowiecki, Paweł J. Zawadzki, and Zygmunt Stopa. 2024. "Arthrocentesis of Temporomandibular Joints—A Clinical Comparative Study" Life 14, no. 12: 1594. https://doi.org/10.3390/life14121594
APA StyleSiewert, M., Pokrowiecki, R., Zawadzki, P. J., & Stopa, Z. (2024). Arthrocentesis of Temporomandibular Joints—A Clinical Comparative Study. Life, 14(12), 1594. https://doi.org/10.3390/life14121594







