Insights into the Risk Factors and Outcomes of Post-COVID-19 Syndrome—Results from a Retrospective, Cross-Sectional Study in Romania
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Sample Size
2.3. Questionnaire
2.4. Data Analysis
3. Results
3.1. Characteristics of the Enrolled Subjects
3.2. SARS-CoV-2 Vaccination Status
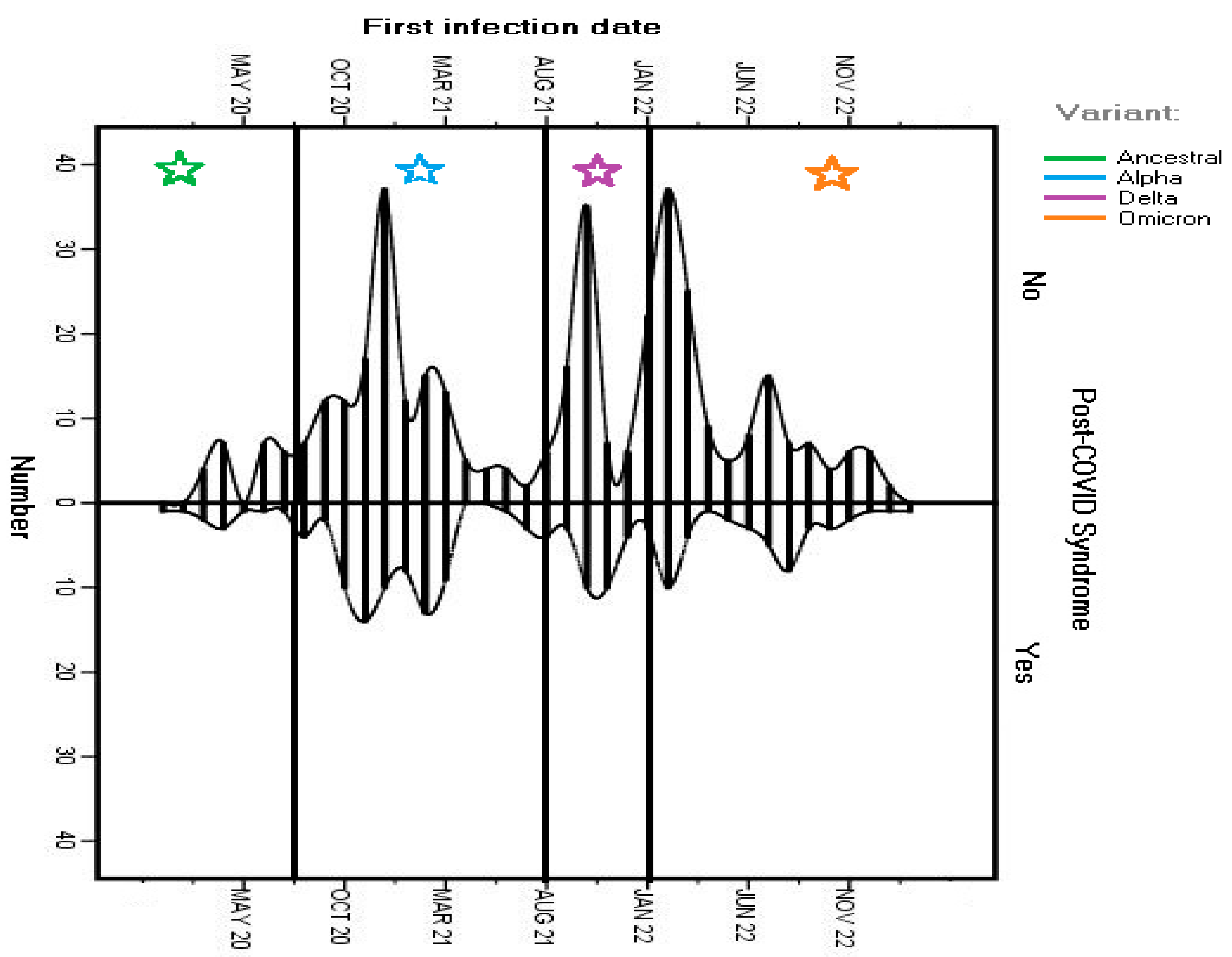
3.3. Diagnosis of SARS-CoV-2 Infection
3.4. Persistence of Symptoms After the Acute Infection
3.5. Perceived Aggravating Factors for Post-COVID-19 Syndrome
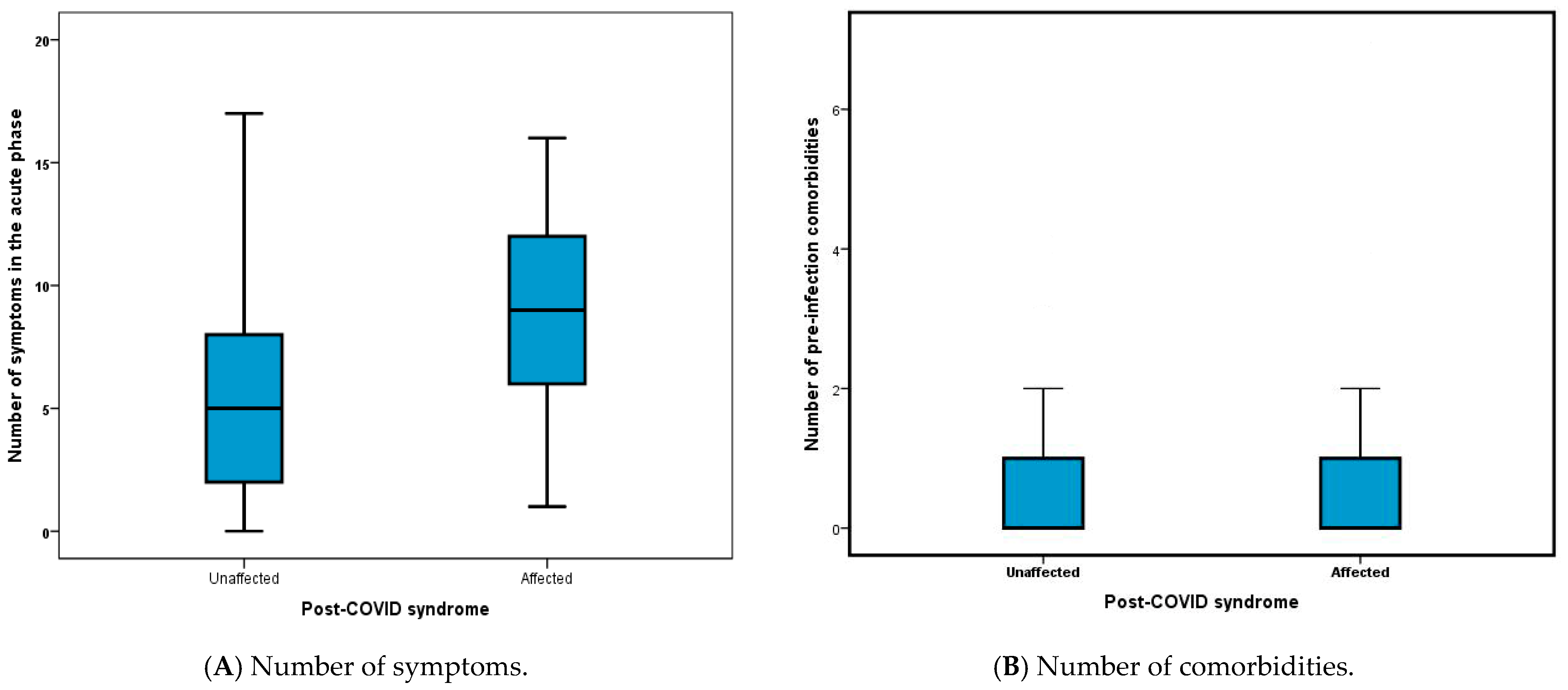
3.6. Risk Factors for Post-COVID-19 Symptomatology
3.7. Effect of SARS-CoV-2 Vaccination on the Development and Evolution of Post-COVID-19 Symptomatology
3.8. Multivariate Analysis
3.9. Health Status and Quality of Life in Subjects with Long COVID
3.10. Medical Resources Accessed for Post-COVID-19 Syndrome
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus, 6 October 2021. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 (accessed on 25 August 2024).
- Peluso, M.J.; Deeks, S.G. Mechanisms of long COVID and the path toward therapeutics. Cell 2024, 187, 5500–5529. [Google Scholar] [CrossRef]
- Fernandez-de-Las-Peñas, C.; Notarte, K.I.; Macasaet, R.; Velasco, J.V.; Catahay, J.A.; Ver, A.T.; Chung, W.; Valera-Calero, J.A.; Navarro-Santana, M. Persistence of post-COVID symptoms in the general population two years after SARS-CoV-2 infection: A systematic review and meta-analysis. J. Infect. 2024, 88, 77–88. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 21, 133–146, Erratum in: Nat. Rev. Microbiol. 2023, 21, 408. [Google Scholar] [CrossRef]
- Pollack, B.; von Saltza, E.; McCorkell, L.; Santos, L.; Hultman, A.; Cohen, A.K.; Soares, L. Female reproductive health impacts of Long COVID and associated illnesses including ME/CFS, POTS, and connective tissue disorders: A literature review. Front. Rehabil. Sci. 2023, 4, 1122673. [Google Scholar] [CrossRef]
- Ford, N.D.; Agedew, A.; Dalton, A.F.; Singleton, J.; Perrine, C.G.; Saydah, S. Notes from the Field: Long COVID Prevalence Among Adults—United States, 2022. Morb. Mortal. Wkly. Rep. 2024, 73, 135–136. [Google Scholar] [CrossRef]
- Yin, K.; Peluso, M.J.; Luo, X.; Thomas, R.; Shin, M.G.; Neidleman, J.; Andrew, A.; Young, K.C.; Ma, T.; Hoh, R.; et al. Long COVID manifests with T cell dysregulation, inflammation and an uncoordinated adaptive immune response to SARS-CoV-2. Nat. Immunol. 2024, 25, 218–225. [Google Scholar] [CrossRef]
- Cervia-Hasler, C.; Brüningk, S.C.; Hoch, T.; Fan, B.; Muzio, G.; Thompson, R.C.; Ceglarek, L.; Meledin, R.; Westermann, P.; Emmenegger, M.; et al. Persistent complement dysregulation with signs of thromboinflammation in active Long COVID. Science 2024, 383, eadg7942. [Google Scholar] [CrossRef]
- Enciu, B.G.; Pițigoi, D.; Zaharia, A.; Popescu, R.; Niculcea, A.; Crăciun, M.-D.; Pistol, A. COVID-19 Vaccination in Romania and the Benefits of the National Electronic Registry of Vaccinations. Vaccines 2023, 11, 370. [Google Scholar] [CrossRef]
- Cozma, A.; Sitar-Tăut, A.V.; Orășan, O.H.; Leucuța, D.C.; Pocol, T.C.; Sălăgean, O.; Crișan, C.; Sporiș, N.D.; Lazar, A.L.; Mălinescu, T.V.; et al. The Impact of Long COVID on the Quality of Life. Medicina 2024, 60, 1359. [Google Scholar] [CrossRef]
- Ursescu, C.; Teodoru, G.; Bucurica, S.; Nica, R.I.; Lazăr, Ș.D.; Popescu, M.N.; Ciobanu, I.; Berteanu, M. Using the ClinFIT COVID-19 Instrument to Assess the Functional Impairments Specific to Post-COVID-19 Patients in Romania. Diagnostics 2024, 14, 1540. [Google Scholar] [CrossRef]
- Cioboata, R.; Nicolosu, D.; Streba, C.T.; Vasile, C.M.; Olteanu, M.; Nemes, A.; Gheorghe, A.; Calarasu, C.; Turcu, A.A. Post-COVID-19 Syndrome Based on Disease Form and Associated Comorbidities. Diagnostics 2022, 12, 2502. [Google Scholar] [CrossRef] [PubMed]
- Sample Size Calculator. Available online: https://www.abs.gov.au/websitedbs/d3310114.nsf/home/sample+size+calculator (accessed on 25 May 2023).
- EuroQol Research Foundation. EQ-5D-3L User Guide, 2018. Available online: https://euroqol.org/publications/user-guides (accessed on 15 September 2024).
- Tsampasian, V.; Elghazaly, H.; Chattopadhyay, R.; Debski, M.; Naing, T.K.P.; Garg, P.; Clark, A.; Ntatsaki, E.; Vassiliou, V.S. Risk Factors Associated with Post-COVID-19 Condition: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2023, 183, 566–580. [Google Scholar] [CrossRef] [PubMed]
- Perumal, R.; Shunmugam, L.; Naidoo, K.; Abdool Karim, S.S.; Wilkins, D.; Garzino-Demo, A.; Brechot, C.; Parthasarathy, S.; Vahlne, A.; Nikolich, J.Ž. Long COVID: A review and proposed visualization of the complexity of long COVID. Front. Immunol. 2023, 14, 1117464. [Google Scholar] [CrossRef] [PubMed]
- Al-Husinat, L.; Nusir, M.; Al-Gharaibeh, H.; Alomari, A.A.; Smadi, M.M.; Battaglini, D.; Pelosi, P. Post-COVID-19 syndrome symptoms after mild and moderate SARS-CoV-2 infection. Front. Med. 2022, 9, 1017257. [Google Scholar] [CrossRef]
- Romanian National Center for Disease Control and Surveillance. Information on the SARS-CoV-2 VOC Cases in Romania. Available online: https://www.cnscbt.ro/index.php/analiza-cazuri-confirmate-covid19/3557-s-33-2023-informare-cazuri-cu-variante-de-ingrijorare-voc-si-variante-de-interes-voi/file (accessed on 15 September 2024). (In Romanian).
- Dascalu, S.; Geambasu, O.; Valentin Raiu, C.; Azoicai, D.; Damian Popovici, E.; Apetrei, C. COVID-19 in Romania: What Went Wrong? Front. Public Health 2021, 9, 813941. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chivu-Economescu, M.; Vremera, T.; Ruta, S.M.; Grancea, C.; Leustean, M.; Chiriac, D.; David, A.; Matei, L.; Diaconu, C.C.; Gatea, A.; et al. Assessment of the Humoral Immune Response Following COVID-19 Vaccination in Healthcare Workers: A One Year Longitudinal Study. Biomedicines 2022, 10, 1526. [Google Scholar] [CrossRef]
- Canas, L.S.; Molteni, E.; Deng, J.; Sudre, C.H.; Murray, B.; Kerfoot, E.; Antonelli, M.; Rjoob, K.; Capdevila Pujol, J.; Polidori, L.; et al. Profiling post-COVID-19 condition across different variants of SARS-CoV-2: A prospective longitudinal study in unvaccinated wild-type, unvaccinated alpha-variant, and vaccinated delta-variant populations. Lancet Digit. Health 2023, 5, e421–e434. [Google Scholar] [CrossRef]
- Hernández-Aceituno, A.; García-Hernández, A.; Larumbe-Zabala, E. COVID-19 long-term sequelae: Omicron versus Alpha and Delta variants. Infect. Dis. Now. 2023, 53, 104688. [Google Scholar] [CrossRef]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631, Erratum in: Nat. Med. 2021, 27, 1116. [Google Scholar] [CrossRef]
- Compeer, B.; Neijzen, T.R.; van Lelyveld, S.F.L.; Martina, B.E.E.; Russell, C.A.; Goeijenbier, M. Uncovering the Contrasts and Connections in PASC: Viral Load and Cytokine Signatures in Acute COVID-19 versus Post-Acute Sequelae of SARS-CoV-2 (PASC). Biomedicines 2024, 12, 1941. [Google Scholar] [CrossRef]
- Sylvester, S.V.; Rusu, R.; Chan, B.; Bellows, M.; O’Keefe, C.; Nicholson, S. Sex differences in sequelae from COVID-19 infection and in long COVID syndrome: A review. Curr. Med Res. Opin. 2022, 38, 1391–1399. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Yao, Q.; Gu, X.; Wang, Q.; Ren, L.; Wang, Y.; Hu, P.; Guo, L.; Liu, M.; Xu, J.; et al. 1-year outcomes in hospital survivors with COVID-19: A longitudinal cohort study. Lancet 2021, 398, 747–758, Erratum in: Lancet. 2022 399, 1778. [Google Scholar] [CrossRef] [PubMed]
- Zang, C.; Zhang, Y.; Xu, J.; Bian, J.; Morozyuk, D.; Schenck, E.J.; Khullar, D.; Nordvig, A.S.; Shenkman, E.A.; Rothman, R.L.; et al. Data-driven analysis to understand long COVID using electronic health records from the RECOVER initiative. Nat. Commun. 2023, 14, 1948. [Google Scholar] [CrossRef] [PubMed]
- Bazdar, S.; Bloemsma, L.D.; Baalbaki, N.; Blankestijn, J.M.; Cornelissen, M.E.B.; Beijers, R.J.H.C.G.; Sondermeijer, B.M.; van Wijck, Y.; Downward, G.S.; Maitland-van der Zee, A.H.; et al. Hemoglobin and Its Relationship with Fatigue in Long-COVID Patients Three to Six Months after SARS-CoV-2 Infection. Biomedicines 2024, 12, 1234. [Google Scholar] [CrossRef]
- Hanson, A.L.; Mulè, M.P.; Ruffieux, H.; Mescia, F.; Bergamaschi, L.; Pelly, V.S.; Turner, L.; Kotagiri, P.; Göttgens, B.; Hess, C.; et al. Iron dysregulation and inflammatory stress erythropoiesis associates with long-term outcome of COVID-19. Nat. Immunol. 2024, 25, 471–482. [Google Scholar] [CrossRef]
- Moustafa, I.M.; Ahbouch, A.; Kader, R.P.; Shousha, T.M.; Alrahoomi, A. A Comparison of Sensorimotor Integration and Motor Fitness Components between Collegiate Athletes with and without Long COVID: A Cross-Sectional Study with Pair-Matched Controls. J. Clin. Med. 2024, 13, 2469. [Google Scholar] [CrossRef]
- Jaywant, A.; Gunning, F.M.; Oberlin, L.E.; Santillana, M.; Ognyanova, K.; Druckman, J.N.; Baum, M.A.; Lazer, D.; Perlis, R.H. Cognitive Symptoms of Post-COVID-19 Condition and Daily Functioning. JAMA Netw. Open 2024, 7, e2356098. [Google Scholar] [CrossRef]
- Ziauddeen, N.; Pantelic, M.; O’Hara, M.E.; Hastie, C.; Alwan, N.A. Impact of long COVID-19 on work: A co-produced survey. Lancet 2023, 402 (Suppl. S1), S98. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Nijs, J.; Neblett, R.; Polli, A.; Moens, M.; Goudman, L.; Shekhar Patil, M.; Knaggs, R.D.; Pickering, G.; Arendt-Nielsen, L. Phenotyping Post-COVID Pain as a Nociceptive, Neuropathic, or Nociplastic Pain Condition. Biomedicines 2022, 10, 2562. [Google Scholar] [CrossRef]
- Bobowik, P.; Gajewski, J.; Wiszomirska, I.; Maciejewska-Skrendo, A.; Leźnicka, K.; Kaczmarczyk, K. The Impact of Resistance Training on Equilibrium Abilities and Quality of Life in Older Adults after SARS-CoV-2 Survival. J. Clin. Med. 2024, 13, 2747. [Google Scholar] [CrossRef]
- Svensson, A.; Svensson-Raskh, A.; Holmström, L.; Hallberg, C.; Bezuidenhout, L.; Moulaee Conradsson, D.; Ståhlberg, M.; Bruchfeld, J.; Fedorowski, A.; Nygren-Bonnier, M. Individually tailored exercise in patients with postural orthostatic tachycardia syndrome related to post-COVID-19 condition—A feasibility study. Sci. Rep. 2024, 14, 20017. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Xu, E.; Bowe, B.; Al-Aly, Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 2022, 28, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Loboda, D.; Sarecka-Hujar, B.; Nowacka-Chmielewska, M.; Szoltysek-Boldys, I.; Zielinska-Danch, W.; Gibinski, M.; Wilczek, J.; Gardas, R.; Grabowski, M.; Lejawa, M.; et al. Relationship of Non-Invasive Arterial Stiffness Parameters with 10-Year Atherosclerotic Cardiovascular Disease Risk Score in Post-COVID-19 Patients—The Results of a Cross-Sectional Study. Life 2024, 14, 1105. [Google Scholar] [CrossRef] [PubMed]
- Docherty, A.B.; Farrell, J.; Thorpe, M.; Egan, C.; Dunn, S.; Norman, L.; Shaw, C.A.; Law, A.; Leeming, G.; Norris, L.; et al. Patient emergency health-care use before hospital admission for COVID-19 and long-term outcomes in Scotland: A national cohort study. Lancet Digit Health 2023, 5, e446–e457, Erratum in: Lancet Digit Health 2023, 5, e550. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Venkatesh, A.K.; Yu, H.; Malicki, C.; Gottlieb, M.; Elmore, J.G.; Hill, M.J.; Idris, A.H.; Montoy, J.C.C.; O’Laughlin, K.N.; Rising, K.L.; et al. The association between prolonged SARS-CoV-2 symptoms and work outcomes. PLoS ONE 2024, 19, e0300947. [Google Scholar] [CrossRef]
- Brannock, M.D.; Chew, R.F.; Preiss, A.J.; Hadley, E.C.; Redfield, S.; McMurry, J.A.; Leese, P.J.; Girvin, A.T.; Crosskey, M.; Zhou, A.G.; et al. Long COVID risk and pre-COVID vaccination in an EHR-based cohort study from the RECOVER program. Nat. Commun. 2023, 14, 2914. [Google Scholar] [CrossRef]
- MacCallum-Bridges, C.; Hirschtick, J.L.; Patel, A.; Orellana, R.C.; Elliott, M.R.; Fleischer, N.L. The impact of COVID-19 vaccination prior to SARS-CoV-2 infection on prevalence of long COVID among a population-based probability sample of Michiganders, 2020–2022. Ann. Epidemiol. 2024, 92, 17–24. [Google Scholar] [CrossRef]
- Berteanu, M.; Cinteza, D.C.; Bighea, A. Recommenedations of the Medical Commission for Physical and Rehabilitation Medicine for Medical Rehabilitation of Post COVID-19 Patients. 2022. Available online: https://www.inrmfb.ro/wp-content/uploads/2021/04/Recomandari-MFR-post-covid.pdf (accessed on 25 August 2024). (In Romanian).


| Demographics | Subgroup | Number-N, (%) |
|---|---|---|
| Gender | Male | 134 (24.4%) |
| Female | 413 (75.2%) | |
| Prefer not to disclose | 2 (0.4%) | |
| Age group | 18–24 | 107 (19. 5%) |
| 25–34 | 116 (21.1%) | |
| 35–44 | 153 (27.9%) | |
| 45–54 | 124 (22.6%) | |
| 55–64 | 40 (7.3%) | |
| 65–74 | 8 (1.5%) | |
| 75+ | 1 (0.2%) | |
| Background | Urban | 499 (90.9%) |
| Rural | 50 (9.1%) | |
| Educational level | Bachelor’s degree or higher | 377 (68.7%) |
| Secondary form of education | 161 (29.3%) | |
| Primary education | 11 (2%) | |
| Healthcare worker | Yes | 239 (43.5%) |
| No | 307 (55.9%) | |
| Health status and habits | ||
| Smoking status | Never smoker | 270 (49.2%) |
| Current smoker | 115 (20.9%) | |
| Occasional smoker | 69 (12.6%) | |
| Former smoker (1 year+) | 92 (16.8%) | |
| BMI | <30 | 474 (86.3%) |
| >30 | 75 (13.7%) | |
| Pre-infection chronic condition | Hypertension | 42 (7.6%) |
| Other cardiovascular disease | 22 (4%) | |
| Autoimmune/endocrine | 31 (5.7%) | |
| Anxiety/depression | 27 (4.9%) | |
| Chronic pulmonary disease | 20 (3.6%) | |
| Anemia | 18 (3.3%) | |
| Diabetes mellitus | 13 (2.4%) | |
| Neurological condition | 5 (0.9%) | |
| Malignancy | 5 (0.9%) | |
| Chronic kidney disease | 4 (0.7%) | |
| Chronic hepatic disease | 3 (0.5%) | |
| Immune deficiency | 3 (0.5%) | |
| Others | 15 (2.7%) |
| Vaccinated with 1 Dose | Vaccinated with 2 Doses | Vaccinated with 3 Doses | Not Vaccinated | |
|---|---|---|---|---|
| Post-COVID syndrome | 13 | 61 | 51 | 37 |
| No post-COVID syndrome | 33 | 117 | 186 | 51 |
| SARS-CoV-2 Infection | Clinical Form | Number (%) |
|---|---|---|
| Severity of infection | Asymptomatic | 48 (8.7%) |
| Mild form, not hospitalized | 438 (79.8%) | |
| Hospitalized, with no supplemental oxygen | 48 (8.7%) | |
| Hospitalized with oxygen provided by a nasal cannula | 7 (1.3%) | |
| Hospitalized with high-flow oxygen | 7 (1.3%) | |
| Intubated | 1 (0.2%) | |
| Reinfection | 1 episode | 133 (24.2%) |
| More than 2 episodes | 47 (8.6%) | |
| Reinfection severity | Worse the first time | 85 (47.5%) |
| Always the same severity | 48 (26.8%) | |
| Worse the second time | 34 (18.9%) | |
| Worse the third/fourth time | 12 (6.7%) |
| Persistent Symptoms after the Acute Infection (n, %) | ||||
|---|---|---|---|---|
| Symptom | During the First 4 Weeks n = 549 | After 3 Months n = 162 | After 6 Months n = 129 | After 12 Months n = 101 |
| Persistent fever | 223 (40.6%) | 2 (0.4%) | 1 (0.2%) | 0 |
| Anosmia/ageusia/dysgeusia | 279 (50.8%) | 47 (8.6%) | 32 (5.8%) | 18 (3.3%) |
| Fatigue/asthenia | 440 (80.1%) | 93 (16.9%) | 71 (12.9%) | 48 (8.7%) |
| Persistent headache | 325 (59.2%) | 47 (8.6%) | 32 (5.8%) | 20 (3.6%) |
| Dysphagia/odynophagia | 240 (43.7%) | 13 (2.4%) | 10 (1.8%) | 7 (1.3%) |
| Dyspnea | 171 (31.1%) | 43 (7.8%) | 32 (5.8%) | 16 (2.9%) |
| Myalgia/arthralgia | 334 (60.8%) | 53 (9.7%) | 41 (7.5%) | 29 (5.3%) |
| Persistent cough | 266 (48.5%) | 28 (5.1%) | 17 (3.1%) | 7 (1.3%) |
| Rhinorrhea/persistent sneezing/sore eyes | 244 (44.4%) | 29 (5.3%) | 19 (3.5%) | 11 (2%) |
| Adenopathies | 81 (14.8%) | 14 (2.6%) | 12 (2.2%) | 7 (1.3%) |
| Anorexia | 147 (26.8%) | 13 (2.4%) | 9 (1.6%) | 7 (1.3%) |
| Nausea/vomiting/gastro-intestinal disturbance | 117 (21.3%) | 19 (3.5%) | 16 (2.9%) | 7 (1.3%) |
| Cognitive dysfunctions | 190 (34.6%) | 63 (11.5%) | 49 (8.9%) | 35 (6.4%) |
| Anxiety/depression | 144 (26.2%) | 49 (8.9%) | 35 (6.4%) | 24 (4.4%) |
| Palpitations | 171 (31.1%) | 65 (11.8%) | 50 (9.1%) | 33 (6%) |
| Sleep disturbances | 199 (36.2%) | 62 (11.3%) | 53 (9.7%) | 39 (7.1%) |
| Pearson/Fisher’s Test (p-Value) | OR | 95% CI Min–Max | ||
|---|---|---|---|---|
| Not being vaccinated | 0.0047 | 2.046 | 1.245 | 3.363 |
| Obesity | 0.761 | 1.085 | 0.641 | 1.836 |
| Presence of any comorbidity pre-infection | 0.008 | 1.657 | 1.138 | 2.413 |
| Reinfection | <0.001 | 2.405 | 1.642 | 3.523 |
| Number of symptoms in the first 4 weeks >5 | <0.001 | 4.243 | 2.809 | 6.411 |
| Tested Variable | ROC p-Value | Area Under the Curve | OR Logistic Regression (p-Value) | 95% CI | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Number of pre-infection comorbidities | 0.009 | 0.571 | 3.637 (p = 0.012) | 2.376 | 5.568 |
| Reinfection episodes | <0.001 | 0.600 | 1.673 (p = 0.004) | 1.118 | 2.502 |
| Number of acute symptoms | <0.001 | 0.716 | 1.968 (p < 0.001) | 1.149 | 3.371 |
| Status—not vaccinated | 0.087 | 0.546 | 1.824 (p = 0.014) | 1.212 | 2.744 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bejan, I.; Popescu, C.P.; Ruta, S.M. Insights into the Risk Factors and Outcomes of Post-COVID-19 Syndrome—Results from a Retrospective, Cross-Sectional Study in Romania. Life 2024, 14, 1519. https://doi.org/10.3390/life14111519
Bejan I, Popescu CP, Ruta SM. Insights into the Risk Factors and Outcomes of Post-COVID-19 Syndrome—Results from a Retrospective, Cross-Sectional Study in Romania. Life. 2024; 14(11):1519. https://doi.org/10.3390/life14111519
Chicago/Turabian StyleBejan, Ioana, Corneliu Petru Popescu, and Simona Maria Ruta. 2024. "Insights into the Risk Factors and Outcomes of Post-COVID-19 Syndrome—Results from a Retrospective, Cross-Sectional Study in Romania" Life 14, no. 11: 1519. https://doi.org/10.3390/life14111519
APA StyleBejan, I., Popescu, C. P., & Ruta, S. M. (2024). Insights into the Risk Factors and Outcomes of Post-COVID-19 Syndrome—Results from a Retrospective, Cross-Sectional Study in Romania. Life, 14(11), 1519. https://doi.org/10.3390/life14111519






