Abstract
Background: Lipoprotein(a) [Lp(a)] is recognized as an independent risk factor for cardiovascular diseases; however, the impact of fat-based diets on its levels remains unclear. Objective: This study aims to assess and analyze current evidence on the impact of various types of fat-based diets on Lp(a) levels. Material and Methods: A comprehensive search of the PubMed database was conducted on 9 July 2024, focusing on clinical and randomized trials published since 2000. Out of 697 identified studies, 33 met the inclusion criteria and were selected for analysis. Results: The findings suggest that modifications in fat-based diets, particularly concerning the type and amount of consumed fats and fatty acids, can significantly influence plasma Lp(a) levels. Diets rich in unsaturated fats, including polyunsaturated and monounsaturated fatty acids, were associated with more favorable effects in lowering Lp(a) levels. In contrast, diets high in saturated fats were linked to elevated Lp(a) levels. However, these conclusions were not consistent across all studies considered. Conclusions: This work highlights the importance of a personalized dietary approach, considering both genetic predispositions and dietary habits. While diet alone may not drastically alter Lp(a) levels due to their strong genetic determination, a comprehensive strategy involving a healthy diet rich in unsaturated fats, regular physical activity, and effective weight management is recommended to reduce the risk of cardiovascular diseases. Further research is needed to clarify the mechanisms through which different fats affect Lp(a) and to develop targeted dietary recommendations.
1. Introduction
Lipoprotein(a) [Lp(a)] is a complex present in blood plasma, consisting of one LDL particle containing apoB-100 and a large, polymorphic glycoprotein apo(a). The LPA gene responsible for the production of Lp(a) is primarily transcribed in the liver [1]. Plasma Lp(a) concentrations exhibit significant individual variability and are inherited. Discovered by Kåre Berg in 1963, Lp(a) has attracted interest due to its association with atherosclerotic diseases, particularly coronary heart disease (CHD), despite its unclear physiological role [2].
One of the challenges in quantifying Lp(a) is the size polymorphism of apo(a). It is hypothesized that differences in apo(a) size may affect test results, depending on the assay used and its antibody specificity [3]. Despite diagnostic challenges, the fact remains that high Lp(a) levels impact cardiovascular risk (CVR). Epidemiological studies suggest that approximately 20% of the European population has high Lp(a) levels, which is also more common in individuals with familial hypercholesterolemia, further increasing CVR. Effective early treatment to reduce Lp(a) levels is crucial in lowering this risk [4].
Lp(a) also inhibits fibrinolysis, linking cholesterol transport with the coagulation system [5]. Studies also indicate the potential of Lp(a) as an acute-phase protein and its ability to carry oxidized phospholipids, which may contribute to atherosclerosis development [6,7]. This includes its mediation in monocyte adhesion and migration through interaction with β2-integrin Mac-1, which is key in the inflammatory process and plaque formation [8].
To date, several therapeutic options exist to lower Lp(a) levels in the blood [9]. Statins lower LDL cholesterol levels, but their effect on Lp(a) is variable. For example, ezetimibe reduces Lp(a) by about 7%, PCSK9 inhibitors by 23–25%, and mipomersen by 26.4% [10,11]. Other methods, such as microsomal triglyceride transfer protein inhibitors and cholesterol ester transfer protein inhibitors, niacin, and thyroid hormone mimetics, can reduce Lp(a) by 20–30% [12,13,14]. Aspirin may also lower Lp(a), particularly in individuals with high baseline levels [15]. Lipoprotein apheresis is the most effective, reducing Lp(a) by 60–90% [16]. However, therapy choice remains dependent on the individual characteristics of the patient [9].
For this reason, a detailed literature review was conducted to evaluate the impact of the least invasive method of changing plasma Lp(a) levels, namely dietary modification. This work compares how dietary changes may influence Lp(a) levels, which could be crucial in preventing cardiovascular events in individuals with high levels of this lipoprotein.
Dietary interventions can influence Lp(a) levels through several biological pathways. One key pathway is via alterations in hepatic lipid metabolism, as the liver is the primary site of Lp(a) production. Diets rich in unsaturated fats, particularly omega-3 fatty acids, may reduce Lp(a) synthesis by modulating transcription factors involved in lipid homeostasis, such as peroxisome proliferator-activated receptors (PPARs) and sterol regulatory element-binding proteins (SREBPs). Furthermore, diets high in fiber, especially soluble fiber, may improve bile acid excretion, leading to a compensatory increase in hepatic LDL receptor activity, which can lower circulating Lp(a) levels indirectly. Certain dietary patterns, like those rich in polyphenols, have been shown to reduce oxidative stress and inflammation, both of which are associated with increased Lp(a) levels. In contrast, diets high in saturated fats and trans fats can elevate Lp(a) by upregulating inflammatory pathways and LDL particle production, potentially increasing the hepatic secretion of Lp(a). Additionally, certain amino acids, like lysine, have been proposed to interfere with the binding of Lp(a) to fibrinogen, reducing its pro-atherogenic effects. Finally, alcohol consumption in moderate amounts has been shown to lower Lp(a) levels, possibly through enhanced clearance mechanisms, although the exact mechanisms remain under investigation.
2. Materials and Methods
Search Methods: The “PubMed” database was searched. As of 9 July 2024, entering the keywords “lipoprotein (a), diet” into the PubMed search engine yielded 697 results, of which 128 remained after narrowing down to research studies. Ultimately, 33 studies were included in the review. The time criteria included studies published from 2000 to the date of the search. There were no restrictions on the publication status regarding entries in the registry.
Objectives: The objective of this study was to analyze and evaluate current evidence on the effects of various fat-based diets on Lp(a) levels.
Selection Criteria: This review included clinical and randomized controlled trials involving humans. Only English-language studies were considered. Studies that ambiguously demonstrated the effect of diet on Lp(a), lacked lipid fractionation, including the separation of Lp(a), or involved changes in pharmacological treatment during the study period were excluded.
Main Results: The review included 33 records of varying quality and sample size. The selected studies are research papers that are statistically significant and directly related to the topic of the impact of diet on Lp(a) levels. An additional 7 studies were included to supplement the review with information provided in the introduction. The results are shown in the PRISMA diagram (Figure 1).
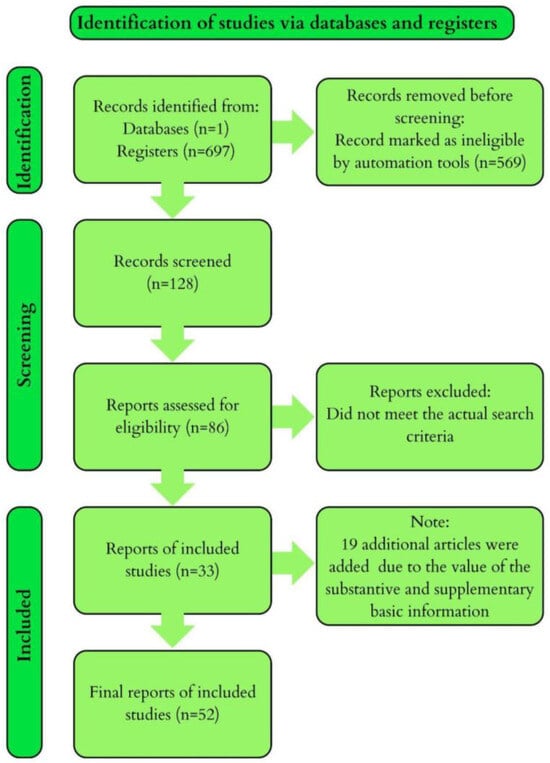
Figure 1.
The results of our research visualized in the PRISMA diagram.
3. Results
The results we collected are presented in the form of a table (Table 1) with detailed descriptions of all studies included in the review.

Table 1.
Publications Investigating the Impact of Diet on Lp(a) Levels.
4. Discussion
Research on the impact of different types of diets on Lp(a) levels has shown effects dependent on the type of fat. In the context of dietary interventions that may affect Lp(a) levels, it is crucial to consider both the amount and type of fats consumed. Literature examples indicate varying effects of different types of fats. For instance, H.G. Prawo et al., using a diet with reduced total fat and SFA for 12 weeks, observed an increase in Lp(a) levels while simultaneously reducing LDL-C. Similarly, in the study by M.P. St-Onge et al., involving 45 participants over three phases lasting 25 days each, a diet rich in PUFA led to an increase in Lp(a), while a low-fat diet decreased Lp(a) levels. On the other hand, U. Hoppu et al. observed a gradual increase in Lp(a) from the beginning of the study to the fourth year in 127 mothers and their children with reduced SFA intake and increased MUFA and PUFA intake. It is possible that the increase in Lp(a) in this research may be related to other long-term changes in the body that are not directly linked to diet [17,45,47].
Delgado-Alarcón et al. compared the impact of three different breakfasts on Lp(a) levels over a month, finding that meals rich in PUFA and MUFA led to significant reductions of Lp(a). In contrast, the 6-week study by A.M. Tindall et al., with similar diets, did not show changes in Lp(a) levels, although the sample size was about half as large (34 people). Similarly, W. Stonehouse et al. found no change in Lp(a) in a study with a similar number of participants and diets. Likewise, S. Gulati et al., in a 24-week period enriched with MUFA and PUFA, did not achieve statistically significant changes in Lp(a). The studies by R. Loganathan et al., S. Vega-Lopez et al., and A.H. Lichtenstein et al. also did not observe significant differences in Lp(a) between different diets enriched with unsaturated fatty acids [18,19,20,24,25,26,27].
The study by S. Vega-Lopez et al. with 30 participants tested a diet enriched with partially hydrogenated soybean oil, which led to a decrease in Lp(a). Soybean oil is primarily a source of PUFA but also contains MUFA and saturated fats [49]. In a larger group (124 people), C. Bamberger et al.’s 8-week study found no significant impact of walnut-enriched diets on Lp(a) levels. Walnuts are rich in various types of fats, including MUFA and PUFA and a small amount of saturated fats [50], making them a focus of interest as a dietary addition. Similarly, pecans, which have a higher MUFA content compared to PUFA, were included in the diet in the study by S. Jaranam et al. and led to a decrease in Lp(a). A decrease in Lp(a) was also observed in the study by D.J.A. Jenkins et al. with almond supplementation, which is mainly a source of monounsaturated fats, while the same dietary addition in J.F. Ruisinger et al.’s study did not result in significant differences in Lp(a) [21,31,32,33].
A small group of 20 participants in D. Iggman’s study examined the effect of canola oil, a source of unsaturated fatty acids, on lipid profiles compared to a dairy-based diet rich in saturated fatty acids. The canola oil diet increased Lp(a) levels. In a study with 162 participants, B. Vessby et al. found that consuming a diet rich in MUFA increased Lp(a) by 12%, although trans fats were at the same level across all tested diets. Conversely, D. Zambón et al. demonstrated a reduction of Lp(a) with a diet supplemented with monounsaturated fats over 6 weeks, with significant decreases observed only in men. Supplementation with flaxseed oil significantly reduced Lp(a) gene expression in peripheral blood mononuclear cells compared to the placebo group in the study by A.A. Hashemzadeh et al. Flaxseed oil is a rich source of fats, particularly PUFA [21,23,28,29].
J.M. Gaullier et al. studied the impact of linoleic acid, free fatty acids, and triglycerides at different concentrations in diets with 180 overweight adults, observing a significant increase in Lp(a). The following year, the same authors published a study where 134 participants from the first study received 3.4 g of linoleic acid daily for another year, which significantly increased Lp(a) after 24 months [34].
In the study by Gebauer S.K. et al. with 106 healthy adults over 24 days, diets with vascenic acid, industrially produced trans fatty acids, and conjugated linoleic acid cis-9, trans-11 (c9,t11-CLA) showed a change only with vascenic acid (increasing Lp(a)). In the study by S.H. Vermunt et al., neither a diet high in trans isomers of alpha-linolenic acid nor a low one showed changes in Lp(a). Similarly, in M. Pfeuffer et al.’s study, including safflower oil, showed no changes. The study by M. Ohman et al. on omega-3 fatty acid supplementation also showed no changes in Lp(a). Participants in P.T. Voon et al.’s study consumed three different diets over 5 weeks, where fats constituted two-thirds of 30% of calories from fat, and only the diet containing coconut oil reduced postprandial Lp(a). This is because long-chain SFA increases postprandial Lp(a), but coconut oil contains shorter-chain fatty acids that lower postprandial Lp(a) [41,42,43,46,48].
The study by T. Tholstrup et al. with 16 healthy men consuming meals with 1 g of fat (mainly saturated) per kg of body weight after a 12 h fast, including stearic and palmitic acids, led to elevated Lp(a) levels. In contrast, the study by C. Seidel et al. with 15 women and 16 men showed that a diet with reduced saturated fatty acids over 13 weeks resulted in the lowest Lp(a) levels compared to standard diets.
It is also worth noting the variability in the results obtained by researchers. When analyzing the available data, it should be emphasized that some studies were based on smaller sample sizes or were of variable quality, which could have affected the reliability and clarity of the results [35,36].
Some studies focused on phytosterols, natural compounds present in various plant parts. The average person consumes 100–400 mg of phytosterols daily, mainly from vegetable oils, bread, cereals, nuts, and vegetables. Due to their cholesterol-like structure, they compete with cholesterol in the intestine, reducing its absorption and lowering LDL-C levels in plasma [51,52]. However, studies by S.S. AbuMweis et al., Y.M. Chan et al., A. Garoufi et al., and M.B. Madsen did not show an impact on Lp(a) levels with phytosterol-enriched diets. In contrast, J.M.M. Fito et al. found a significant reduction of Lp(a) after 6 months of a plant-rich diet among 930 individuals with high CVD risk [37,38,39,44].
Research has demonstrated that the type of fat in the diet can influence Lp(a) levels. Diets high in SFA generally increase Lp(a) levels, whereas reducing SFA in the diet sometimes leads to an increase in Lp(a) levels but more commonly results in a reduction of LDL-C without affecting Lp(a). Diets rich in MUFA and PUFA can have varying effects. Increasing MUFA in the diet may either increase or decrease Lp(a) levels, depending on whether it is the sole dietary supplement and the percentage of fats in the diet as well as the duration of the intervention. Similarly, PUFA can affect Lp(a) in different ways. Some studies show an increase in Lp(a) with PUFA-rich diets, while others show a decrease. Reducing SFA intake and increasing MUFA and PUFA can have a beneficial impact on the overall lipid profile, though the effect on Lp(a) may vary. The diversity in the effects of SFA, MUFA, and PUFA on Lp(a) levels results from genetics, metabolism, diet composition, and the specific characteristics of each fat. Each of these variables can influence study outcomes and the body’s response. Lifestyle and physical activity can also significantly influence Lp(a) levels. Regular physical activity contributes to improving the lipid profile, which can lead to a reduction of Lp(a) levels by decreasing inflammation and enhancing lipid metabolism. Conversely, lifestyle factors such as smoking, excessive alcohol consumption, and obesity can raise Lp(a) levels and increase the risk of cardiovascular diseases. This phenomenon is associated with hormonal and metabolic changes, as well as the development of chronic inflammation, which can stimulate Lp(a) production and lead to disturbances in lipid metabolism. An important topic to address is the adaptation of the diet to demographic and genetic profiles. Dietary interventions must be tailored to genetic and demographic profiles, as responses to dietary changes vary between individuals. For example, people with familial hypercholesterolemia or certain ethnic groups may metabolize fats differently, requiring a more targeted approach. Personalized nutrition, which takes into account genotype and ethnic background, allows for better control of Lp(a) levels and other lipids, potentially reducing the risk of cardiovascular diseases more effectively.
Coconut oil: containing short-chain fatty acids, coconut oil may lower postprandial Lp(a). Nuts and seeds: dietary supplementation with nuts, such as almonds, pecans, or walnuts, may contribute to lowering Lp(a) levels. Flaxseed oil: flaxseed oil has been shown to reduce Lp(a) gene expression, which could be beneficial for individuals with high levels of this lipoprotein. Limiting trans fats: trans fats, such as vascenic acid, increase Lp(a) levels, so their elimination from the diet is beneficial. The impact of dietary fats on lipid levels is variable. Generally, increasing dietary cholesterol raises LDL-C levels, but individual responses can differ. Current dietary guidelines recommend consuming a high amount of vegetables, fruits, legumes, nuts, whole grains, and fish, replacing SFA with MUFA and PUFA, reducing cholesterol intake, avoiding processed meats, refined carbohydrates, and sugary drinks, and eliminating trans fats.
5. Summary
Elevated Lp(a) levels are a genetically regulated, independent CVD risk factor. However, variability in Lp(a) levels among individuals and population groups also suggests a role for non-genetic factors. Diets with lower saturated fat content have a moderate impact on Lp(a) levels, usually increasing them, in contrast to LDL cholesterol, which decreases. Diets rich in MUFA and PUFA can either decrease or increase Lp(a) depending on the diet duration, fat content percentage, and supplements used.
Research shows that the effect of diet on Lp(a) levels is variable; however, a common trend is the claim that adopting a diet rich in vegetables, fruits, legumes, nuts, whole grains, and fish, replacing SFA with MUFA and PUFA, reducing cholesterol intake, and avoiding trans fats may benefit the overall lipid profile and cardiovascular health. Nevertheless, this subject requires further study to draw firm conclusions and establish recommendations for controlling Lp(a) levels.
Author Contributions
Conceptualization, M.S. and A.S.; methodology, K.N.; software, R.K.; validation, M.S., A.S. and J.Z.-F.; formal analysis, J.Z.-F.; investigation, R.K.; resources, M.S.; data curation, M.S.; writing—original draft preparation, K.N.; writing—review and editing, R.K.; visualization, K.N.; supervision, J.Z.-F.; project administration, M.S.; funding acquisition, A.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Jawi, M.M.; Frohlich, J.; Chan, S.Y. Lipoprotein(a) the Insurgent: A New Insight into the Structure, Function, Metabolism, Pathogenicity, and Medications Affecting Lipoprotein(a) Molecule. J. Lipids 2020, 2020, e3491764. [Google Scholar] [CrossRef] [PubMed]
- Sandholzer, C.; Hallman, D.M.; Saha, N.; Sigurdsson, G.; Lackner, C.; Császár, A.; Boerwinkle, E.; Utermann, G. Effects of the apolipoprotein(a) size polymorphism on the lipoprotein(a) concentration in 7 ethnic groups. Hum. Genet. 1991, 86, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Vinci, P.; Di Girolamo, F.G.; Panizon, E.; Tosoni, L.M.; Cerrato, C.; Pellicori, F.; Altamura, N.; Pirulli, A.; Zaccari, M.; Biasinutto, C.; et al. Lipoprotein(a) as a Risk Factor for Cardiovascular Diseases: Pathophysiology and Treatment Perspectives. Int. J. Environ. Res. Public Health 2023, 20, 6721. [Google Scholar] [CrossRef] [PubMed]
- Kronenberg, F.; Mora, S.; Stroes, E.S.G. Consensus and guidelines on lipoprotein(a)—Seeing the forest through the trees. Curr. Opin. Infect. Dis. 2022, 33, 342–352. [Google Scholar] [CrossRef]
- Nordestgaard, B.G.; Chapman, M.J.; Ray, K.; Borén, J.; Andreotti, F.; Watts, G.F.; Ginsberg, H.; Amarenco, P.; Catapano, A.; Descamps, O.S.; et al. Lipoprotein(a) as a cardiovascular risk factor: Current status. Eur. Heart J. 2010, 31, 2844–2853. [Google Scholar] [CrossRef]
- Schmidt, K.; Noureen, A.; Kronenberg, F.; Utermann, G. Structure, function, and genetics of lipoprotein (a). J. Lipid Res. 2016, 57, 1339–1359. [Google Scholar] [CrossRef]
- McCormick, S.P.A. Lipoprotein(a): Biology and Clinical Importance. Clin. Biochem. Rev. 2004, 25, 69–80. [Google Scholar]
- Sotiriou, S.N.; Orlova, V.V.; Al-Fakhri, N.; Ihanus, E.; Economopoulou, M.; Isermann, B.; Bdeir, K.; Nawroth, P.P.; Preissner, K.T.; Gahmberg, C.G.; et al. Lipoprotein(a) in atherosclerotic plaques recruits inflammatory cells through interaction with Mac-1 integrin. FASEB J. 2006, 20, 559–561. [Google Scholar] [CrossRef]
- Paragh, G.; Zilahi, P.; Kolozsvári, L.R.; Lőrincz, H.; Fülöp, P.; Harangi, M. Novel Therapeutic Approaches for the Management of Elevated Lipoprotein(a): From Traditional Agents to Future Treatment Options. Life 2024, 14, 374. [Google Scholar] [CrossRef]
- Awad, K.; Mikhailidis, D.P.; Katsiki, N.; Muntner, P.; Banach, M. Effect of Ezetimibe Monotherapy on Plasma Lipoprotein(a) Concentrations in Patients with Primary Hypercholesterolemia: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Drugs 2018, 78, 453–462. [Google Scholar] [CrossRef]
- Santos, R.D.; Raal, F.J.; Catapano, A.L.; Witztum, J.L.; Steinhagen-Thiessen, E.; Tsimikas, S. Mipomersen, an Antisense Oligonucleotide to Apolipoprotein B-100, Reduces Lipoprotein(a) in Various Populations with Hypercholesterolemia. Arterioscler. Thromb. Vasc. Biol. 2015, 35, 689–699. [Google Scholar] [CrossRef] [PubMed]
- Sahebkar, A.; Reiner, Ž.; Simental-Mendía, L.E.; Ferretti, G.; Cicero, A.F.G. Effect of extended-release niacin on plasma lipoprotein(a) levels: A systematic review and meta-analysis of randomized placebo-controlled trials. Metabolism 2016, 65, 1664–1678. [Google Scholar] [CrossRef] [PubMed]
- Samaha, F.F.; McKenney, J.M.; Bloedon, L.T.; Sasiela, W.J.; Rader, D.J. Inhibition of microsomal triglyceride transfer protein alone or with ezetimibe in patients with moderate hypercholesterolemia. Nat. Clin. Pract. Cardiovasc. Med. 2008, 5, 497–505. [Google Scholar] [CrossRef] [PubMed]
- Grover, G.J.; Egan, D.M.; Sleph, P.G.; Beehler, B.C.; Chiellini, G.; Nguyen, N.-H.; Baxter, J.D.; Scanlan, T.S. Effects of the Thyroid Hormone Receptor Agonist GC-1 on Metabolic Rate and Cholesterol in Rats and Primates: Selective Actions Relative to 3,5,3′-Triiodo-l-Thyronine. Endocrinology 2004, 145, 1656–1661. [Google Scholar] [CrossRef] [PubMed]
- Akaike, M.; Azuma, H.; Kagawa, A.; Matsumoto, K.; Hayashi, I.; Tamura, K.; Nishiuchi, T.; Iuchi, T.; Takamori, N.; Aihara, K.-I.; et al. Effect of Aspirin Treatment on Serum Concentrations of Lipoprotein(a) in Patients with Atherosclerotic Diseases. Clin. Chem. 2002, 48, 1454–1459. [Google Scholar] [CrossRef]
- Korneva, V.A.; Kuznetsova, T.Y.; Julius, U. Modern Approaches to Lower Lipoprotein(a) Concentrations and Consequences for Cardiovascular Diseases. Biomedicines 2021, 9, 1271. [Google Scholar] [CrossRef]
- Law, H.G.; Khan, M.A.; Zhang, W.; Bang, H.; Rood, J.; Most, M.; Lefevre, M.; Berglund, L.; Enkhmaa, B. Reducing saturated fat intake lowers LDL-C but increases Lp(a) levels in African Americans: The GET-READI feeding trial. J. Lipid Res. 2023, 64, 100420. [Google Scholar] [CrossRef]
- Delgado-Alarcón, J.M.; Hernández Morante, J.J.; Aviles, F.V.; Albaladejo-Otón, M.D.; Morillas-Ruíz, J.M. Effect of the Fat Eaten at Breakfast on Lipid Metabolism: A Crossover Trial in Women with Cardiovascular Risk. Nutrients 2020, 12, 1695. [Google Scholar] [CrossRef]
- Tindall, A.M.; Kris-Etherton, P.M.; Petersen, K.S. Replacing Saturated Fats with Unsaturated Fats from Walnuts or Vegetable Oils Lowers Atherogenic Lipoprotein Classes Without Increasing Lipoprotein(a). J. Nutr. 2020, 150, 818–825. [Google Scholar] [CrossRef]
- Stonehouse, W.; Benassi-Evans, B.; James-Martin, G.; Abeywardena, M. Fatty acid regio-specificity of triacylglycerol molecules may affect plasma lipid responses to dietary fats—A randomised controlled cross-over trial. Eur. J. Clin. Nutr. 2019, 74, 268–277. [Google Scholar] [CrossRef]
- Hashemzadeh, A.A.; Nasoohi, N.; Raygan, F.; Aghadavod, E.; Akbari, E.; Taghizadeh, M.; Memarzadeh, M.R.; Asemi, Z. Flaxseed Oil Supplementation Improve Gene Expression Levels of PPAR-γ, LP(a), IL-1 and TNF-α in Type 2 Diabetic Patients with Coronary Heart Disease. Lipids 2017, 52, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Bamberger, C.; Rossmeier, A.; Lechner, K.; Wu, L.; Waldmann, E.; Stark, R.G.; Altenhofer, J.; Henze, K.; Parhofer, K.G. A Walnut-Enriched Diet Reduces Lipids in Healthy Caucasian Subjects, Independent of Recommended Macronutrient Replacement and Time Point of Consumption: A Prospective, Randomized, Controlled Trial. Nutrients 2017, 9, 1097. [Google Scholar] [CrossRef] [PubMed]
- Iggman, D.; Gustafsson, I.B.; Berglund, L.; Vessby, B.; Marckmann, P.; Risérus, U. Replacing dairy fat with rapeseed oil causes rapid improvement of hyperlipidaemia: A randomized controlled study. J. Intern. Med. 2011, 270, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Gulati, S.; Misra, A.; Pandey, R.M. Effect of Almond Supplementation on Glycemia and Cardiovascular Risk Factors in Asian Indians in North India with Type 2 Diabetes Mellitus: A 24-Week Study. Metab. Syndr. Relat. Disord. 2017, 15, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Loganathan, R.; Nagapan, G.; Teng, K.T.; Voon, P.T.; Yap, S.Y.; Ng, Y.T.; Ng, T.K.; Choo, Y.M.; Ong, A.S.; Ong, S.H.; et al. Diets enriched with palm olein, cocoa butter and extra virgin olive oil exhibited similar lipid response: A randomized controlled study in young healthy adults. Nutr. Res. 2022, 105, 113–125. [Google Scholar] [CrossRef]
- Vega-López, S.; Ausman, L.M.; Jalbert, S.M.; Erkkilä, A.T.; Lichtenstein, A.H. Palm and partially hydrogenated soybean oils adversely alter lipoprotein profiles compared with soybean and canola oils in moderately hyperlipidemic subjects. Am. J. Clin. Nutr. 2006, 84, 54–62. [Google Scholar] [CrossRef]
- Lichtenstein, A.H.; Matthan, N.R.; Jalbert, S.M.; Resteghini, N.A.; Schaefer, E.J.; Ausman, L.M. Novel soybean oils with different fatty acid profiles alter cardiovascular disease risk factors in moderately hyperlipidemic subjects. Am. J. Clin. Nutr. 2006, 84, 497–504. [Google Scholar] [CrossRef]
- Zambón, D.; Sabaté, J.; Munoz, S.; Campero, B.; Casals, E.; Merlos, M.; Laguna, J.C.; Ros, E. Substituting Walnuts for Monounsaturated Fat Improves the Serum Lipid Profile of Hypercholesterolemic Men and Women. Ann. Intern. Med. 2000, 132, 538. [Google Scholar] [CrossRef]
- Vessby, B.; Uusitupa, M.; Hermansen, K.; Riccardi, G.; Rivellese, A.A.; Tapsell, L.C.; Nälsén, C.; Berglund, L.; Louheranta, A.; Rasmussen, B.M.; et al. Substituting Dietary Saturated for Monounsaturated Fat Impairs Insulin Sensitivity in Healthy Men and Women: The KANWU Study. Diabetologia 2001, 44, 312–319. [Google Scholar] [CrossRef]
- Vega-López, S.; Matthan, N.R.; Ausman, L.M.; Ai, M.; Otokozawa, S.; Schaefer, E.J.; Lichtenstein, A.H. Substitution of vegetable oil for a partially-hydrogenated fat favorably alters cardiovascular disease risk factors in moderately hypercholesterolemic postmenopausal women. Atherosclerosis 2009, 207, 208–212. [Google Scholar] [CrossRef][Green Version]
- Rajaram, S.; Burke, K.; Connell, B.; Myint, T.; Sabaté, J. A Monounsaturated Fatty Acid–Rich Pecan-Enriched Diet Favorably Alters the Serum Lipid Profile of Healthy Men and Women. J. Nutr. 2001, 131, 2275–2279. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.J.; Kendall, C.W.; Marchie, A.; Parker, T.L.; Connelly, P.W.; Qian, W.; Haight, J.S.; Faulkner, D.; Vidgen, E.; Lapsley, K.G.; et al. Dose Response of Almonds on Coronary Heart Disease Risk Factors: Blood Lipids, Oxidized Low-Density Lipoproteins, Lipoprotein(a), Homocysteine, and Pulmonary Nitric Oxide. Circulation 2002, 106, 1327–1332. [Google Scholar] [CrossRef] [PubMed]
- Ruisinger, J.F.; Gibson, C.A.; Backes, J.M.; Smith, B.K.; Sullivan, D.K.; Moriarty, P.M.; Kris-Etherton, P. Statins and almonds to lower lipoproteins (the STALL Study). J. Clin. Lipidol. 2015, 9, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Gaullier, J.-M.; Halse, J.; Høye, K.; Kristiansen, K.; Fagertun, H.; Vik, H.; Gudmundsen, O. Conjugated linoleic acid supplementation for 1 y reduces body fat mass in healthy overweight humans. Am. J. Clin. Nutr. 2004, 79, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Tholstrup, T.; Samman, S. Postprandial Lipoprotein(a) Is Affected Differently by Specific Individual Dietary Fatty Acids in Healthy Young Men. J. Nutr. 2004, 134, 2550–2555. [Google Scholar] [CrossRef]
- Seidel, C.; Deufel, T.; Jahreis, G. Effects of Fat-Modified Dairy Products on Blood Lipids in Humans in Comparison with Other Fats. Ann. Nutr. Metab. 2005, 49, 42–48. [Google Scholar] [CrossRef]
- AbuMweis, S.S.; A Vanstone, C.; Ebine, N.; Kassis, A.; Ausman, L.M.; Jones, P.J.H.; Lichtenstein, A.H. Intake of a Single Morning Dose of Standard and Novel Plant Sterol Preparations for 4 Weeks Does Not Dramatically Affect Plasma Lipid Concentrations in Humans. J. Nutr. 2006, 136, 1012–1016. [Google Scholar] [CrossRef]
- Chan, Y.M.; Demonty, I.; Pelled, D.; Jones, P.J.H. Olive oil containing olive oil fatty acid esters of plant sterols and dietary diacylglycerol reduces low-density lipoprotein cholesterol and decreases the tendency for peroxidation in hypercholesterolaemic subjects. Br. J. Nutr. 2007, 98, 563–570. [Google Scholar] [CrossRef]
- Garoufi, A.; Vorre, S.; Soldatou, A.; Tsentidis, C.; Kossiva, L.; Drakatos, A.; Marmarinos, A.; Gourgiotis, D. Plant sterols–enriched diet decreases small, dense LDL-cholesterol levels in children with hypercholesterolemia: A prospective study. Ital. J. Pediatr. 2014, 40, 42. [Google Scholar] [CrossRef]
- Madsen, M.B.; Jensen, A.M.; Schmidt, E.B. The effect of a combination of plant sterol-enriched foods in mildly hypercholesterolemic subjects. Clin. Nutr. 2007, 26, 792–798. [Google Scholar] [CrossRef]
- Gebauer, S.K.; Destaillats, F.; Dionisi, F.; Krauss, R.M.; Baer, D.J. Vaccenic acid and trans fatty acid isomers from partially hydrogenated oil both adversely affect LDL cholesterol: A double-blind, randomized controlled trial. Am. J. Clin. Nutr. 2015, 102, 1339–1346. [Google Scholar] [CrossRef] [PubMed]
- Vermunt, S.H.F.; Beaufrère, B.; Riemersma, R.A.; Sébédio, J.L.; Chardigny, J.M.; Mensink, R.P. Dietarytransα-linolenic acid from deodorised rapeseed oil and plasma lipids and lipoproteins in healthy men: The TransLinE Study. Br. J. Nutr. 2001, 85, 387–392. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pfeuffer, M.; Fielitz, K.; Laue, C.; Winkler, P.; Rubin, D.; Helwig, U.; Giller, K.; Kammann, J.; Schwedhelm, E.; Böger, R.H.; et al. CLA does not impair endothelial function and decreases body weight as compared with safflower oil in overweight and obese male subjects. J. Am. Coll. Nutr. 2011, 30, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Fitó, M.; Estruch, R.; Salas-Salvadó, J.; Martínez-Gonzalez, M.A.; Arós, F.; Vila, J.; Corella, D.; Díaz, O.; Sáez, G.; de la Torre, R.; et al. Effect of the Mediterranean diet on heart failure biomarkers: A randomized sample from the PREDIMED trial. Eur. J. Heart Fail. 2014, 16, 543–550. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.P.; Zhang, S.; Darnell, B.; Allison, D.B. Baseline Serum C-Reactive Protein Is Associated with Lipid Responses to Low-Fat and High-Polyunsaturated Fat Diets. J. Nutr. 2009, 139, 680–683. [Google Scholar] [CrossRef]
- Öhman, M.; Åkerfeldt, T.; Nilsson, I.; Rosen, C.; Hansson, L.-O.; Carlsson, M.; Larsson, A. Biochemical effects of consumption of eggs containing omega-3 polyunsaturated fatty acids. Upsala J. Med. Sci. 2008, 113, 315–324. [Google Scholar] [CrossRef]
- Hoppu, U.; Isolauri, E.; Koskinen, P.; Laitinen, K. Diet and blood lipids in 1–4 year-old children. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 980–986. [Google Scholar] [CrossRef]
- Voon, P.T.; Ng, T.K.W.; Lee, V.K.M.; Nesaretnam, K. Diets high in palmitic acid (16:0), lauric and myristic acids (12:0 + 14:0), or oleic acid (18:1) do not alter postprandial or fasting plasma homocysteine and inflammatory markers in healthy Malaysian adults. Am. J. Clin. Nutr. 2011, 94, 1451–1457. [Google Scholar] [CrossRef]
- Yang, Z.-H.; Nill, K.; Takechi-Haraya, Y.; Playford, M.P.; Nguyen, D.; Yu, Z.-X.; Pryor, M.; Tang, J.; Rojulpote, K.V.; Mehta, N.N.; et al. Differential Effect of Dietary Supplementation with a Soybean Oil Enriched in Oleic Acid versus Linoleic Acid on Plasma Lipids and Atherosclerosis in LDLR-Deficient Mice. Int. J. Mol. Sci. 2022, 23, 8385. [Google Scholar] [CrossRef]
- Petrović-Oggiano, G.; Debeljak-Martačić, J.; Ranković, S.; Pokimica, B.; Mirić, A.; Glibetić, M.; Popović, T. The Effect of Walnut Consumption on n-3 Fatty Acid Profile of Healthy People Living in a Non-Mediterranean West Balkan Country, a Small Scale Randomized Study. Nutrients 2020, 12, 192. [Google Scholar] [CrossRef]
- Li, X.; Xin, Y.; Mo, Y.; Marozik, P.; He, T.; Guo, H. The Bioavailability and Biological Activities of Phytosterols as Modulators of Cholesterol Metabolism. Molecules 2022, 27, 523. [Google Scholar] [CrossRef] [PubMed]
- Tasdighi, E.; Adhikari, R.; Almaadawy, O.; Leucker, T.M.; Blaha, M.J. LP(a): Structure, Genetics, Associated Cardiovascular Risk, and Emerging Therapeutics. Annu. Rev. Pharmacol. Toxicol. 2023, 64, 135–157. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).