Transapical Approach to Septal Myectomy for Hypertrophic Cardiomyopathy
Abstract
1. Introduction
2. Materials and Methods
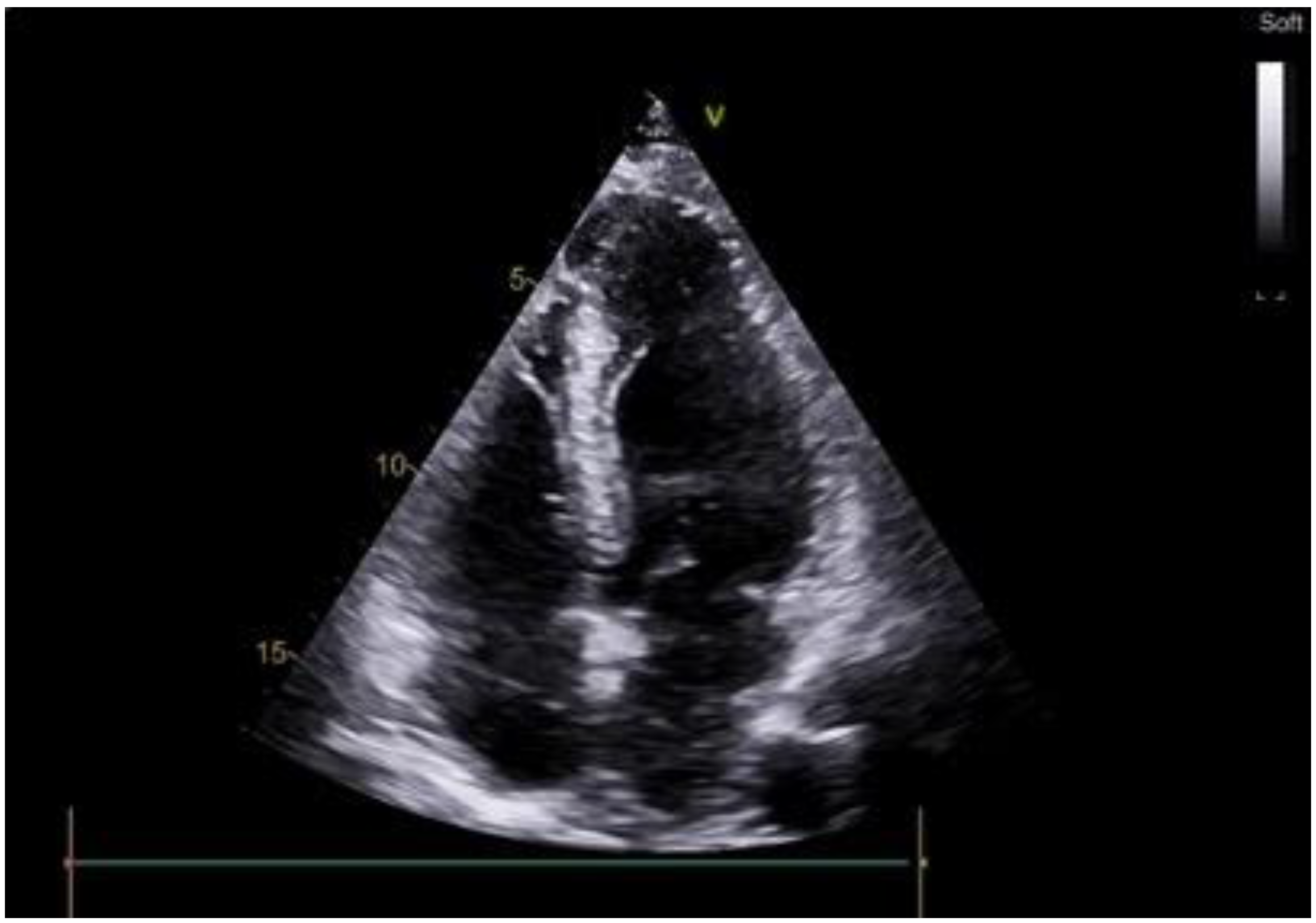
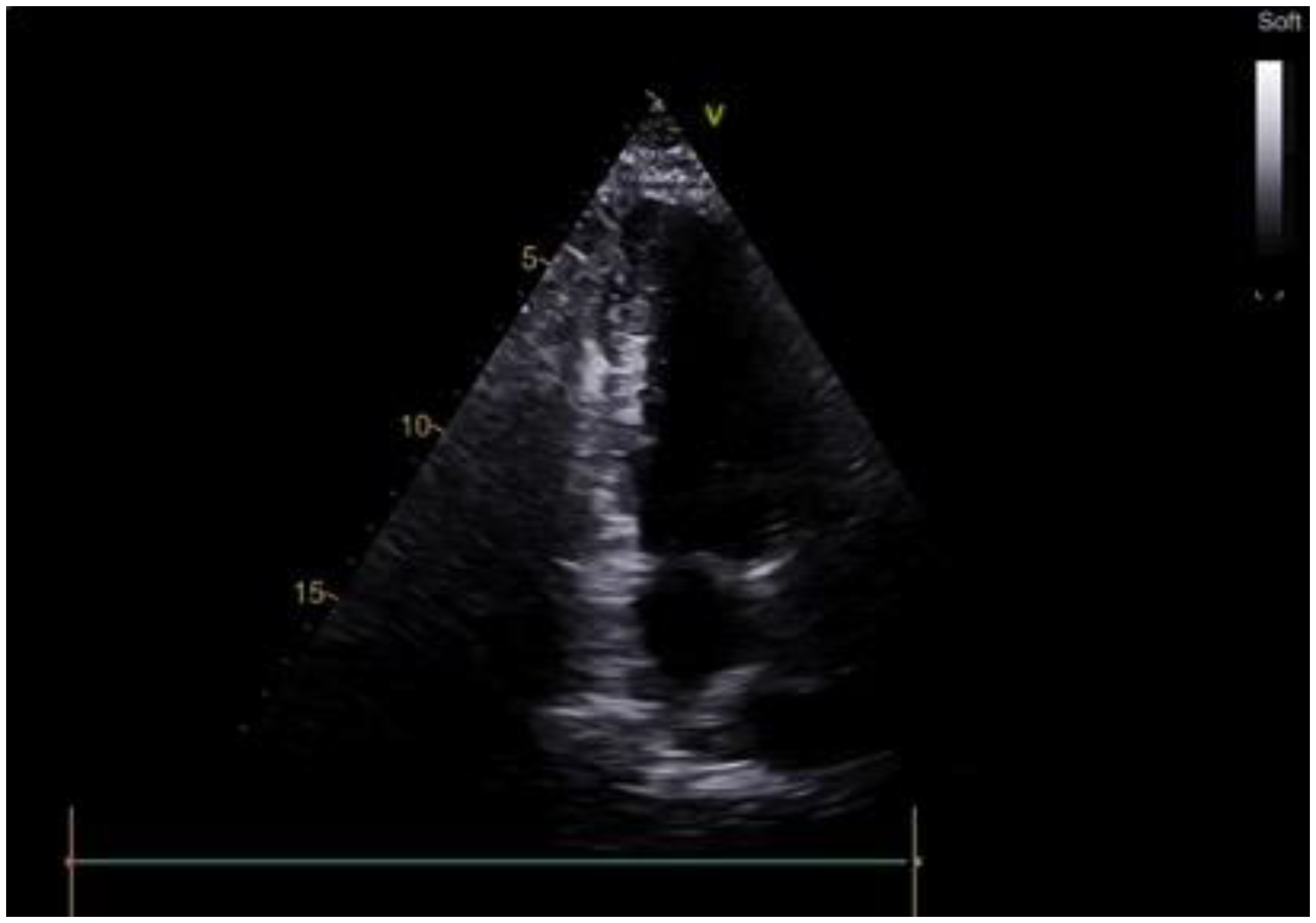
2.1. Case Scenario
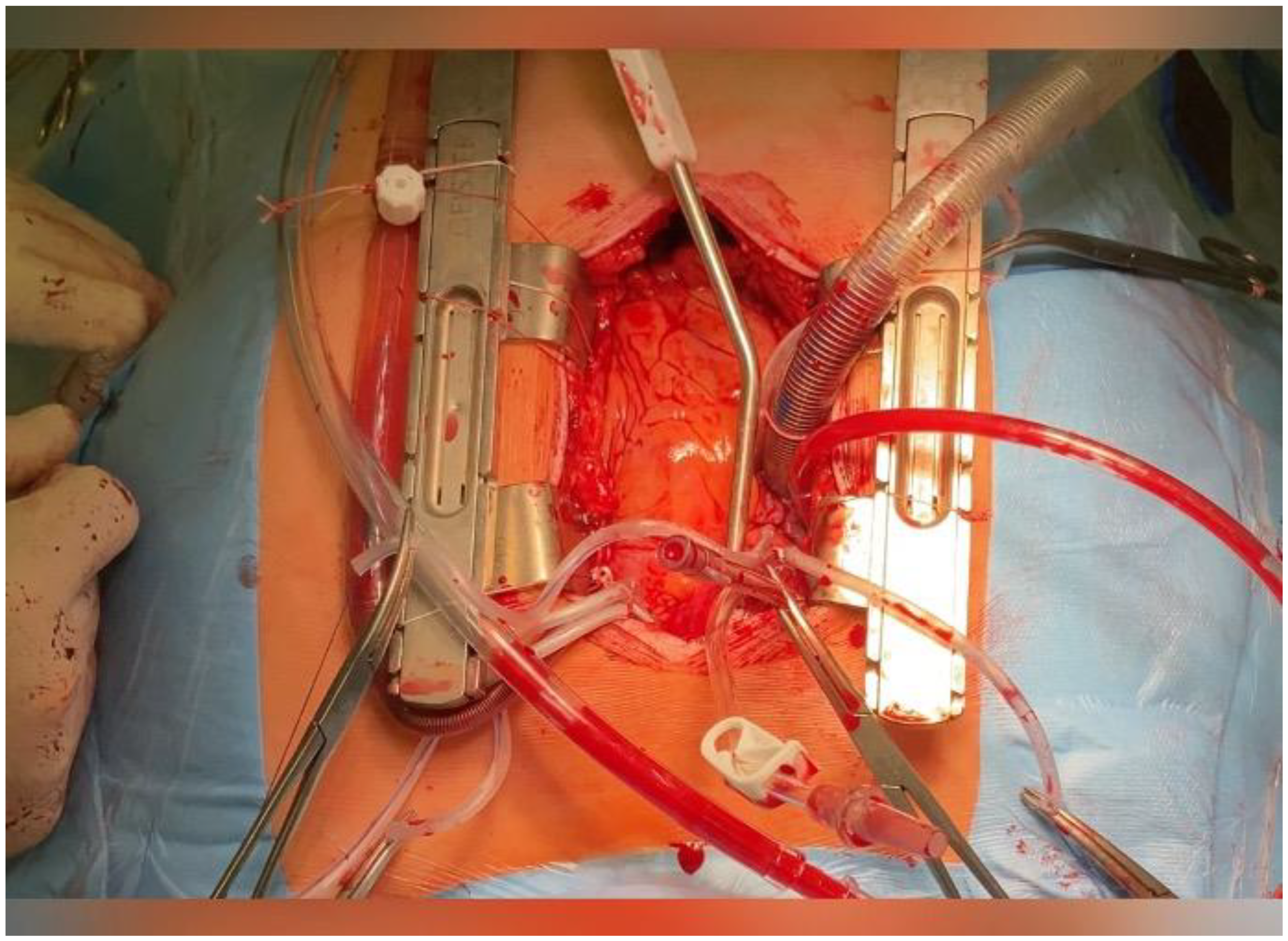
2.2. Surgical Procedure
3. Results
4. Discussion
4.1. Surgery
4.2. Clinical Bottom Line
5. Study Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Elliott, P.M.; Anastasakis, A.; Borger, M.A.; Borggrefe, M.; Cecchi, F.; Charron, P.; Hagege, A.A.; Lafont, A.; Limongelli, G.; Mahrholdt, H.; et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 2014, 35, 2733–2779. [Google Scholar] [CrossRef] [PubMed]
- Gersh, B.J.; Maron, B.J.; Bonow, R.O.; Dearani, J.A.; Fifer, M.A.; Link, M.S.; Naidu, S.S.; Nishimura, R.A.; Ommen, S.R.; Rakowski, H.; et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: Executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011, 124, 2761–2796. [Google Scholar] [CrossRef] [PubMed]
- Ommen, S.R.; Mital, S.; Burke, M.A.; Day, S.M.; Deswal, A.; Elliott, P.; Evanovich, L.L.; Hung, J.; Joglar, J.A.; Kantor, P.; et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: A report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation 2020, 142, e558–e631, Erratum in Circulation 2020, 142, e633. [Google Scholar] [CrossRef] [PubMed]
- Webb, J.G.; Sasson, Z.; Rakowski, H.; Liu, P.; Wigle, E.D. Apical hypertrophic cardiomyopathy: Clinical follow-up and diagnostic correlates. J. Am. Coll. Cardiol. 1990, 15, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, M.J.; Sonnenberg, B.; Woo, A.; Rakowski, P.; Parker, T.G.; Wigle, E.D.; Rakowski, H. Long-termoutcome in patients with apical hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2002, 39, 638–645. [Google Scholar] [CrossRef]
- Klarich, K.W.; Attenhofer Jost, C.H.; Binder, J.; Connolly, H.M.; Scott, C.G.; Freeman, W.K.; Ackerman, M.J.; Nishimura, R.A.; Tajik, A.J.; Ommen, S.R. Risk of death in long-term follow-up of patients with apical hypertrophic cardiomyopathy. Am. J. Cardiol. 2013, 111, 1784–1791, Erratum in Am. J. Cardiol. 2013, 112, 1271. [Google Scholar] [CrossRef]
- Moon, J.; Shim, C.Y.; Ha, J.W.; Cho, I.J.; Kang, M.K.; Yang, W.I.; Jang, Y.; Chung, N.; Cho, S.Y. Clinical and echocardiographic predictors of outcomes in patients with apical hypertrophic cardiomyopathy. Am. J. Cardiol. 2011, 108, 1614–1619. [Google Scholar] [CrossRef] [PubMed]
- Kubo, T.; Kitaoka, H.; Okawa, M.; Hirota, T.; Hoshikawa, E.; Hayato, K.; Yamasaki, N.; Matsumura, Y.; Yabe, T.; Nishinaga, M.; et al. Clinical profiles of hypertrophic cardiomyopathy with apical phenotype–comparison of pure-apical form and distal-dominant form. Circ. J. 2009, 73, 2330–2336. [Google Scholar] [CrossRef]
- Kotkar, K.D.; Said, S.M.; Schaff, H.V. Transapical approach for myectomy in hypertrophic cardiomyopathy. Ann. Cardiothorac. Surg. 2017, 6, 419–422. [Google Scholar] [CrossRef]
- Shimizu, A.; Takanashi, S.; Takamisawa, I.; Shimokawa, T.; Takayama, M.; Isobe, M. Transapical septal myectomy for hypertrophic cardiomyopathy, an experience from Japan. Asian Cardiovasc. Thorac. Ann. 2022, 30, 108–114. [Google Scholar] [CrossRef]
- Nguyen, A.; Schaff, H.V.; Nishimura, R.A.; Geske, J.B.; Dearani, J.A.; King, K.S.; Ommen, S.R. Apical myectomy for patients with hypertrophic cardiomyopathy and advanced heart failure. J. Thorac. Cardiovasc. Surg. 2020, 159, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Forteza, A.; de Villareal, J.E.; Martín, C.E.; Mingo, S.; García-Suárez, J.; García-Pavía, P. Apical myectomy in patients with apical hypertrophic cardiomyopathy and advanced heart failure. Rev. Esp. Cardiol. (Engl. Ed.) 2021, 74, 554–555. [Google Scholar] [CrossRef] [PubMed]
- Schaff, H.V.; Brown, M.L.; Dearani, J.A.; Abel, M.D.; Ommen, S.R.; Sorajja, P.; Tajik, A.J.; Nishimura, R.A. Apical myectomy: A new surgical technique for management of severely symptomatic patients with apical hypertrophic cardiomyopathy. J. Thorac. Cardiovasc. Surg. 2010, 139, 634–640. [Google Scholar] [CrossRef] [PubMed]
- Towe, E.C.; Bos, J.M.; Ommen, S.R.; Gersh, B.J.; Ackerman, M.J. Genotype-Phenotype Correlations in Apical Variant Hypertrophic Cardiomyopathy. Congenit. Heart Dis. 2015, 10, E139–E145. [Google Scholar] [CrossRef] [PubMed]
- Afanasyev, A.V.; Bogachev-Prokophiev, A.V.; Zheleznev, S.I.; Zalesov, A.S.; Budagaev, S.A.; Shajahmetova, S.V.; Nazarov, V.M.; Demin, I.I.; Sharifulin, R.M.; Pivkin, A.N.; et al. Early post-septal myectomy outcomes for hypertrophic obstructive cardiomyopathy. Asian Cardiovasc. Thorac. Ann. 2022, 30, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Bogachev-Prokophiev, A.; Afanasyev, A.V.; Zheleznev, S.; Pivkin, A.; Sharifulin, R.; Kozmin, D.; Karaskov, A. Septal Myectomy With Vs Without Subvalvular Apparatus Intervention in Patients With Hypertrophic Obstructive Cardiomyopathy: A Prospective Randomized Study. Semin. Thorac. Cardiovasc. Surg. 2019, 31, 424–431. [Google Scholar] [CrossRef] [PubMed]


| Author, Date, Journal, Country, and Study Type (Level of Evidence) | Patient Group | Outcomes | Key Results | Comments |
|---|---|---|---|---|
| Kotkar et al. [9], Ann Cardiothorac Surg Retrospective study (Level 2b) | 55 patients with an obstructive midventricular level and 60 patients with midventricular and apical variants of HCM. There were no patients with ventricular aneurysm and ventricular tachycardia. | Clinical outcomes | All patients had gradient relief. None of the patients developed an apical aneurysm or ventricular septal defect. | Retrospective nature of the study |
| Shimizu et al. [10], Asian Cardiovasc Thorac Ann. Cohort study (Level 2b) | 59 patients Age: 40 (39.3–60.7) NYHA class: 16 (27.4%) III/IV Apical Aneurysm n (%): 13 (22.0) | 30-day mortality; 5-year survival | Two perioperative deaths, one late death caused by acute myocardial infarction. 95% The intraventricular gradient had significantly decreased at discharge, and no reoperation for recurrent obstruction was conducted. | Single-center case series |
| Nguyen et al. [11], J Thorac Cardiovasc Surg Retrospective study (Level 2b) | 113 symptomatic patients: Male: 49 (43%) Age: 50.8 (39.3–60.7) NYHA class: 108 (96%) III/IV Ventricular tachycardia n (%): 20 (18) Apical Aneurysm n (%): 25 (22) | 30-day mortality 1-year survival 5-year survival 10-year survival Clinical symptoms | 4 (4%) deaths 96% 87% 74% 76% of patients reported improvement in symptoms, and 3 patients (3%) subsequently underwent cardiac transplantation for recurrent heart failure. Survival appeared superior in patients with hypertrophic cardiomyopathy listed for heart transplant. | Retrospective study at a single institution |
| Forteza et al. [12], Rev Esp Cardiol Cohort study (Level 2b) | 6 patients Male: 1 (16.7%) Age: 61 [40–68] years NYHA III/IV class: 6 (100%) Two patients were being evaluated for a heart transplant. There were no patients with ventricular aneurysm and ventricular tachycardia. LVEDd, mm 60.5 [44.8–70.7] LVESV, mm 21.1 [15.4–24.9] LVEF: 68 [61–78] Maximum midventricular thickness 26 [22.5–28.2] | Median follow-up: 18 months [IQR, 6–24 months] 60.5 [44.8–70.7] 98.5 [76.1–141.0] Clinical symptoms | NYHA III/IV class: 1 (16.7) The echocardiographic study, performed after 6 months in 5 patients and after 1 month in 1 patient, showed a significant increase in ventricular volume in all patients. LVED, mm 98.5 [76.1–141.0] LVESV, mm 42.2 [28.0–66.7] LVEF, % 55 [44–66] Maximum midventricular thickness 16.5 [13.7–19.2] | Apical myectomy is a safe and effective technique for treatment and may offer an alternative to heart transplants in patients with advanced heart failure. |
| Schaff et al. [13], J Thorac Cardiovasc Surg Cohort study (Level 2b) | 44 patients Male: 29 (66%) Age: 50 ± 17 NYHA III/IV class: 40 (91%) LVEF: 72% ± 8% LVEDV: 55 ± 17% mean indexed SV: 39 ± 17 mL/m2 Ventricular tachycardia n (%): 5 (11) | Operative mortality, Follow-up 1-year survival 5-year survival 10-year survival | 2 (4.5%) 2.6 ± 3.1 years (median, 1.3 years) NYHA I/II class: 33 (85%) Functional status was available in 33 (85%) of 39 alive patients 95% 81% 81% LVEF: 61 ± 12% LVEDV: 68 ± 18% mean indexed SV: 46 ± 13 mL/m2 | Transapical ventricular myectomy to increase LVEDV improves diastolic function and SV. |
| Author, Date, Journal, Country, and Study Type (Level of Evidence) | Patient Group | Outcomes | Key Results | Comments |
|---|---|---|---|---|
| Eriksson et al. [5], J Am Coll Cardiol Retrospective study (Level 2b) | 105 patients Age: 41.4 ± 14.5 NYHA I/II/III and IV class: 64/41/0 Exercise-induced ventricular fibrillation n (%): 1 (0.9) | Mean follow-up of | 13.6 ± 8.3 | Apical HCM in North American patients is not associated with SCD and has a benign prognosis in terms of cardiovascular mortality. One-third of these patients experienced serious cardiovascular complications, such as myocardial infarction and arrhythmias. |
| Cardiovascular mortality | 1.9% (2/105) | |||
| Annual cardiovascular mortality | 0.1% | |||
| Atrial fibrillation | 12% | |||
| Myocardial infarction | 10% | |||
| Probability of survival without morbid events at 15 years | 74% | |||
| Webb et al. [4], J Am Coll Cardiol Retrospective study (Level 2b) | 26 patients Age: mean 45 (range 15 to 72) Male: 20 (76.9%) Asymptomatic patients (n): 10 Atypical chest pain (n): 10 Angina (n): 6 Palpitations (n): 8 Exertional dyspnea (n): 5 Presyncope (n): 4 Fatigue (n): 4 Ventricular tachycardia n (%): 2 (7.7) | Mean follow-up 7.3 ± 6.2 years | The prognosis appeared relatively favorable in most but not all patients with apical HCM: no deaths occurred in a cohort of 26 patients over the mean follow-up period. | |
| Stable condition (n) | 21 | |||
| Myocardial infarction (n) | 1 | |||
| Angina (n) | 2 | |||
| Atrial fibrillation (n) | 2 | |||
| Towe et al. [14], Congenit Heart Dis. Cohort study (Level 2b) | 71 patients Male: 45 (63%) Age: 44.4 ± 19 years) Left ventricular wall thickness: 19.8 ± 6 mm Apical Aneurysm n (%): 4 (6) | Mean follow-up was 5.5 years (range 0.1–18.2 years) | 3 patients were lost to follow-up | |
| NYHA class I/II (n) | 52 | |||
| NYHA class III/IV (n) | 16 | |||
| Death (n) | 14 | |||
| Cardiac death (n) | 2 | |||
| SCD (n) | 1 | |||
| Arrhythmia (n) | 27 | |||
| LV aneurysm (n) | 2 | |||
| Stroke (n) | 1 | |||
| Apical myectomy (n) | 16 | |||
| Pacemaker (n) | 8 | |||
| ICD (n) | 21 | |||
| ICD shock | 2 | |||
| Klarich et al. [6], Am J Cardiol Retrospective study (Level 2b) | 193 patients Male: 120 (62%) Age: 58 ± 17 years CAD (n): 22 (11%) Apical aneurysm (n): 6 Apical dilatation with hypokinesis (n): 23 Ventricular tachycardia n (%): 21 (11) Apical Aneurysm n (%): 6 (3) | Mean follow-up period was 78 months (range, 1–350) Death from all causes (n) Heart failure Atrial fibrillation Died | 187 patients [97%] 55 patients (29%; 33 women) During follow-up, more females had heart failure (p = 0.001), atrial fibrillation (p = 0.009), or died (p < 0.001) than males. | Survival was worse than expected (p = 0.001); the observed versus expected 20-year survival was 47% versus 60%. SCD, resuscitated cardiac arrest, and/or defibrillator discharge were observed in 11 patients (6%) during follow-up. Apical HCM in this population was associated with increased mortality. |
| Moon et al. [7], Am J Cardiol Retrospective study (Level 2b) | 454 patients Male: 316 (69%) Age: 61 ± 11 years Ventricular tachycardia n (%): There were no data Apical Aneurysm n (%): There were no data | Follow-up period (43 ± 20 months) | Patients with apical HCM with poor clinical outcomes had more advanced diastolic dysfunction, reduced myocardial contraction/relaxation properties, and increased LV filling pressure at presentation. | |
| All-cause mortality (n) | 39 (9%) | |||
| MACE (n) | 110 (25%) | |||
| Hospitalization due to heart failure (n) | 88 (19%) | |||
| Stroke (n) | 26 (6%) | |||
| Atrial fibrillation (n) | 72 (16%) | |||
| Syncope or presyncope (n) | 5 (1%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Afanasyev, A.; Bogachev-Prokophiev, A.; Zheleznev, S.; Ovcharov, M.; Zalesov, A.; Sharifulin, R.; Demin, I.; Tsaroev, B.; Nazarov, V.; Chernyavskiy, A. Transapical Approach to Septal Myectomy for Hypertrophic Cardiomyopathy. Life 2024, 14, 125. https://doi.org/10.3390/life14010125
Afanasyev A, Bogachev-Prokophiev A, Zheleznev S, Ovcharov M, Zalesov A, Sharifulin R, Demin I, Tsaroev B, Nazarov V, Chernyavskiy A. Transapical Approach to Septal Myectomy for Hypertrophic Cardiomyopathy. Life. 2024; 14(1):125. https://doi.org/10.3390/life14010125
Chicago/Turabian StyleAfanasyev, Alexander, Alexander Bogachev-Prokophiev, Sergei Zheleznev, Mikhail Ovcharov, Anton Zalesov, Ravil Sharifulin, Igor’ Demin, Bashir Tsaroev, Vladimir Nazarov, and Alexander Chernyavskiy. 2024. "Transapical Approach to Septal Myectomy for Hypertrophic Cardiomyopathy" Life 14, no. 1: 125. https://doi.org/10.3390/life14010125
APA StyleAfanasyev, A., Bogachev-Prokophiev, A., Zheleznev, S., Ovcharov, M., Zalesov, A., Sharifulin, R., Demin, I., Tsaroev, B., Nazarov, V., & Chernyavskiy, A. (2024). Transapical Approach to Septal Myectomy for Hypertrophic Cardiomyopathy. Life, 14(1), 125. https://doi.org/10.3390/life14010125








