Anti-Diabetic and Anti-Adipogenic Effect of Harmine in High-Fat-Diet-Induced Diabetes in Mice
Abstract
1. Introduction
2. Materials and Methods
2.1. Experiments Preparations
2.1.1. Preparation of Harmine
2.1.2. Induction of T2DM by HFD
2.2. Experimental Animals
2.3. Experimental Design
2.4. Measured Parameters
2.4.1. Intraperitoneal Glucose Tolerance Test (ipGTT)
2.4.2. Blood Glucose Levels
2.4.3. Body Weights
2.4.4. Relative Organ Body Weight
2.4.5. Body Mass Index (BMI)
2.5. Biochemical of Blood
2.5.1. Blood Sampling
2.5.2. Blood Glucose Levels
2.5.3. Determination of Insulin Levels
2.5.4. Determination of HbA1c
2.5.5. Determination of Serum Alanine Aminotransferase Activity (ALT)
2.5.6. Determination of Serum Uric Acid and Creatinine Concentrations
2.5.7. Determination of Lipid Profile
2.5.8. Determination of Malondialdehyde (MDA) and Total Antioxidant Capacity Content in Serum
2.6. Histological Examination
2.7. Morphometric Study
2.8. Electron Microscopy Analysis
2.9. Statistical Analysis
3. Results
3.1. Characterization of Diabetic Animal Mode
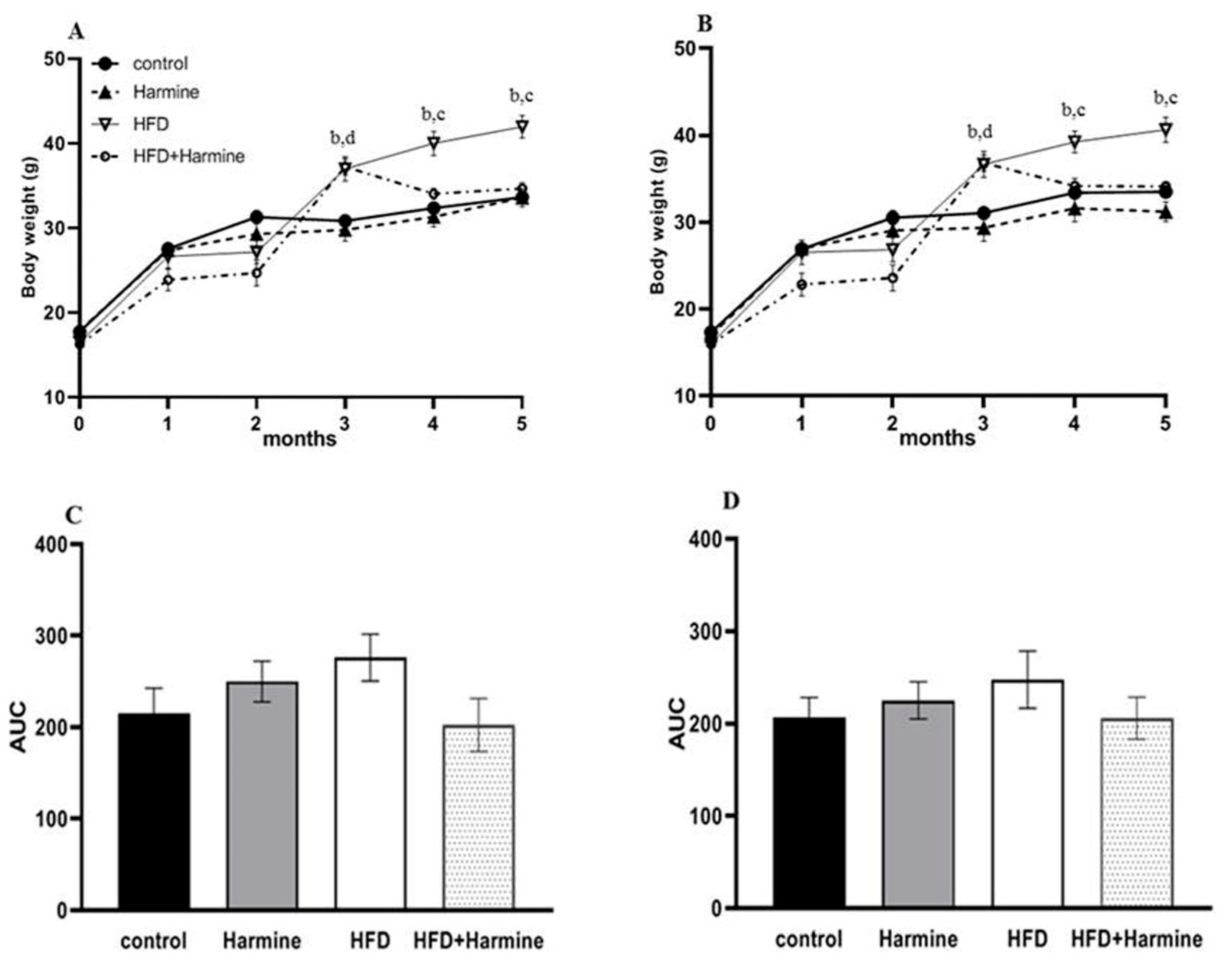
3.1.1. Body Weight
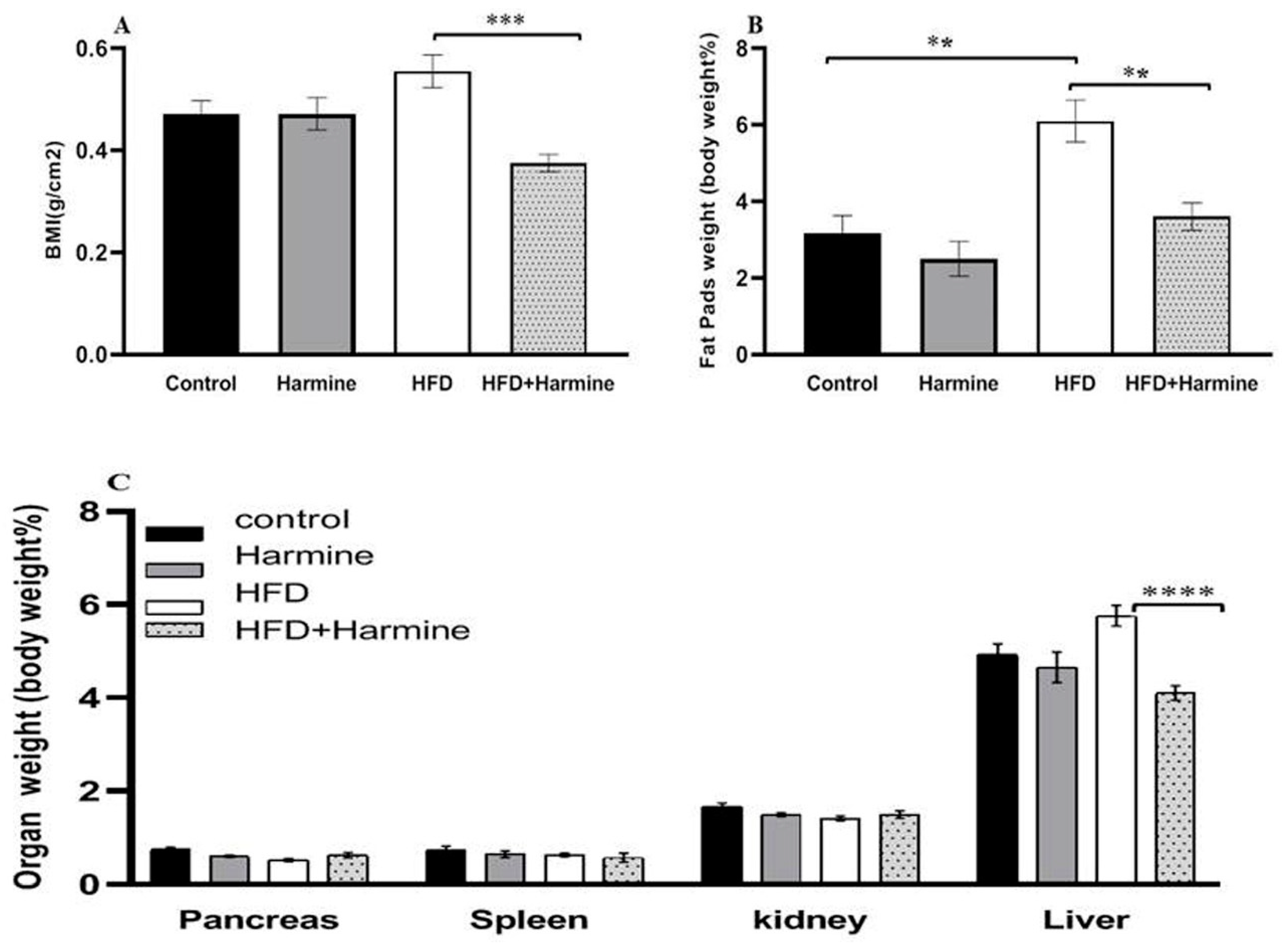
3.1.2. Body Mass Index and Relative Organ Weight
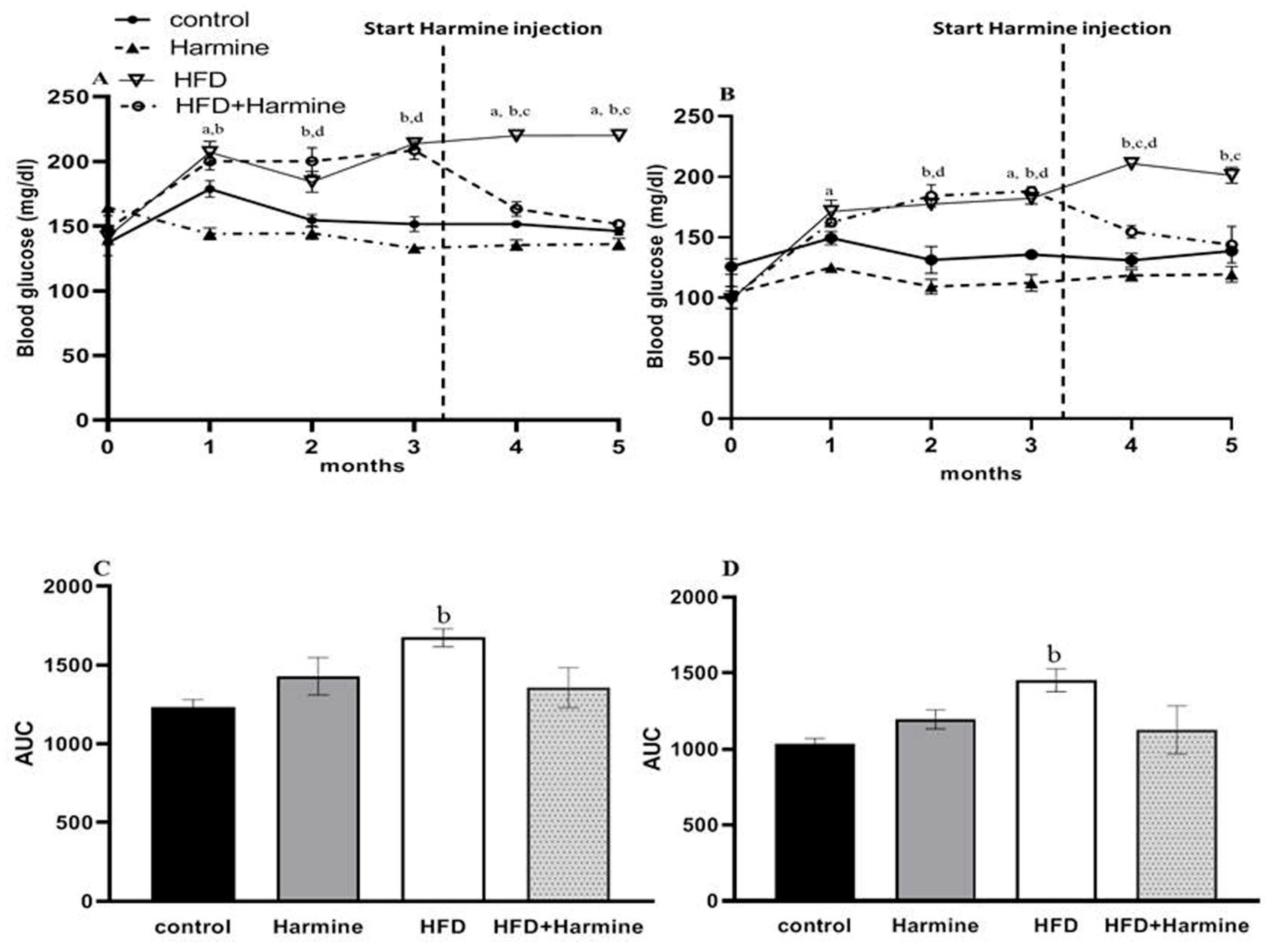
3.1.3. Blood Glucose Levels
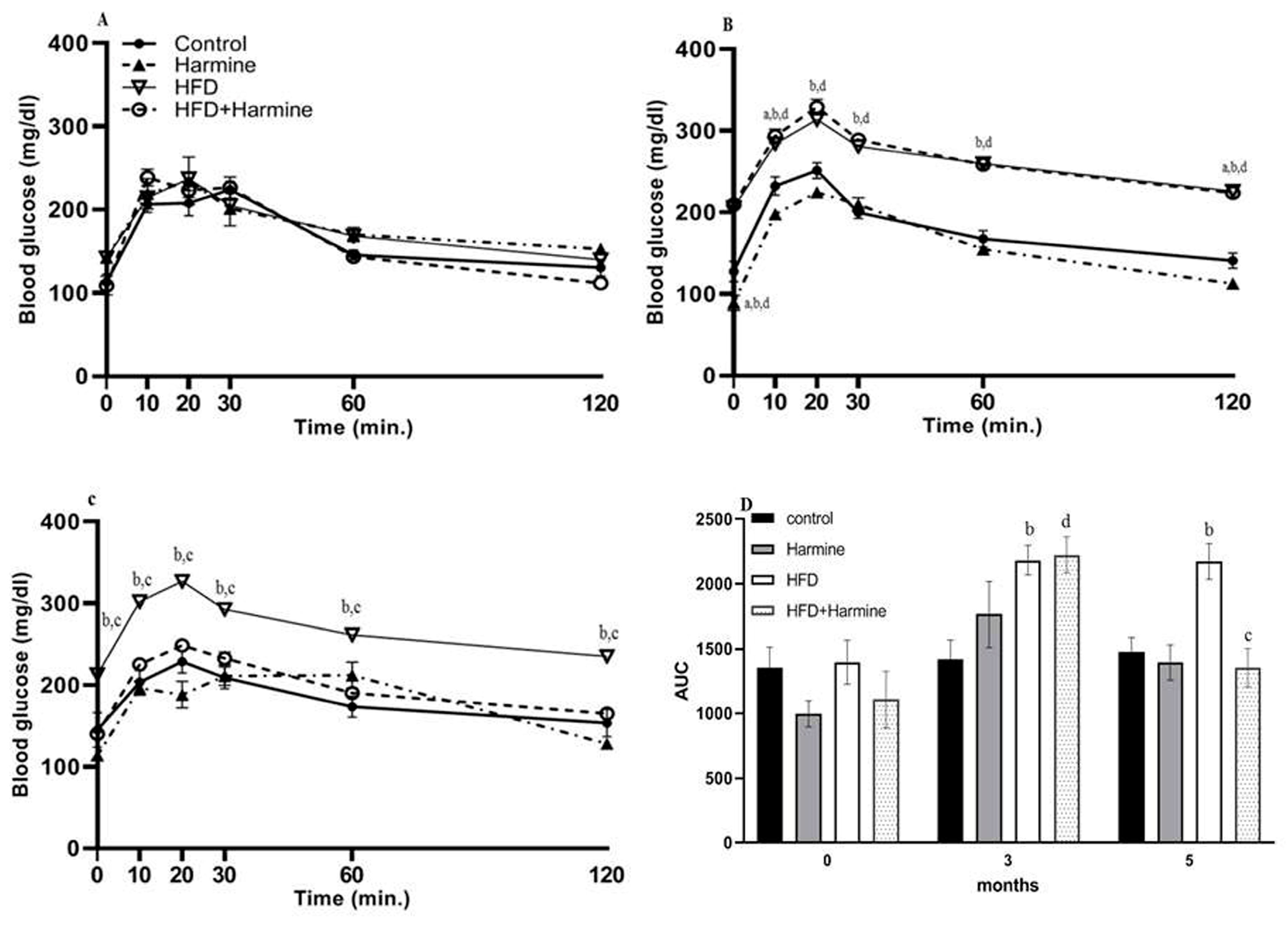
3.1.4. Intraperitoneal Glucose Tolerance Test (ipGTT)
3.2. Biochemical Parameters
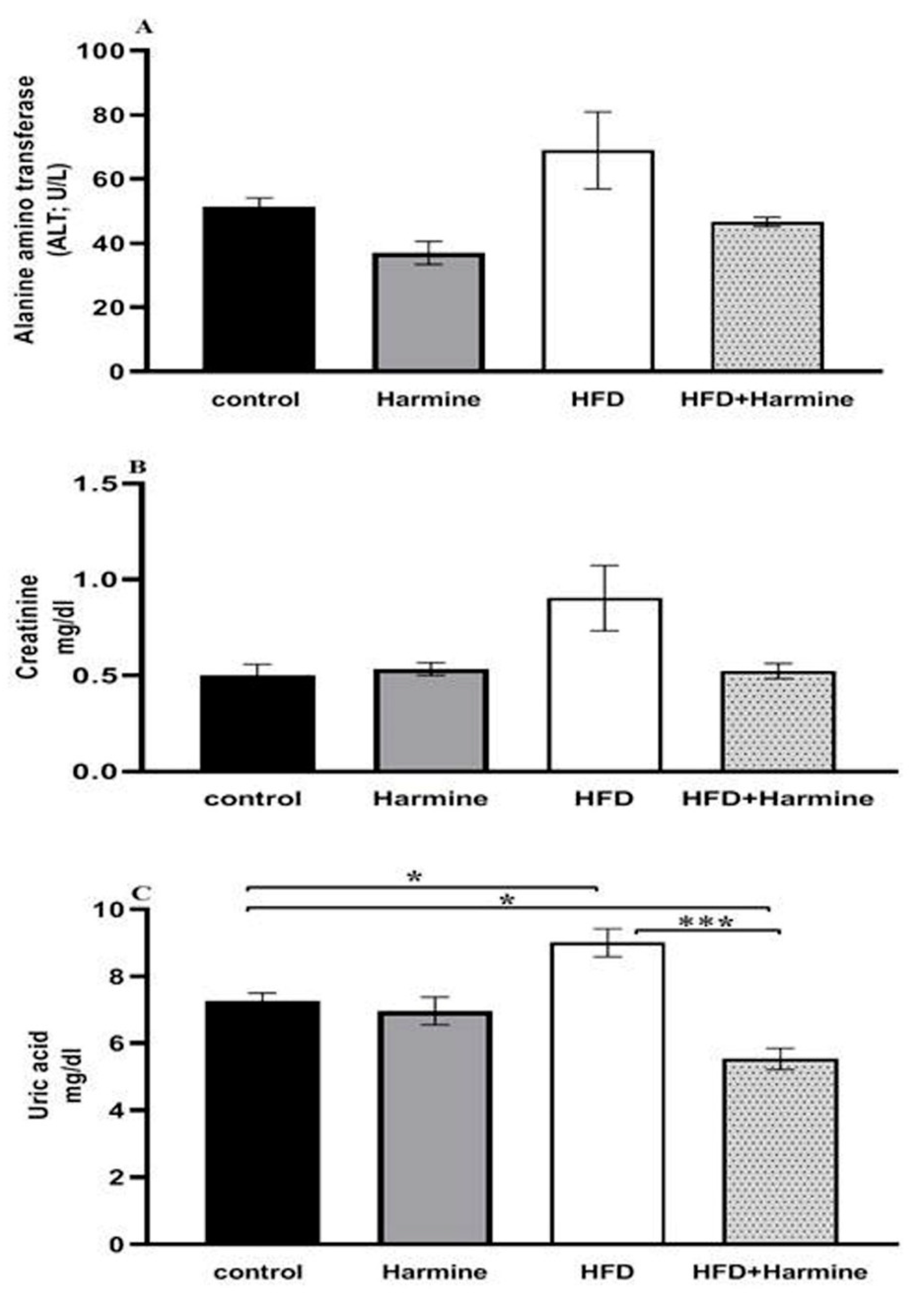
3.2.1. ALT Activity, Creatinine, and Uric Acid Concentrations
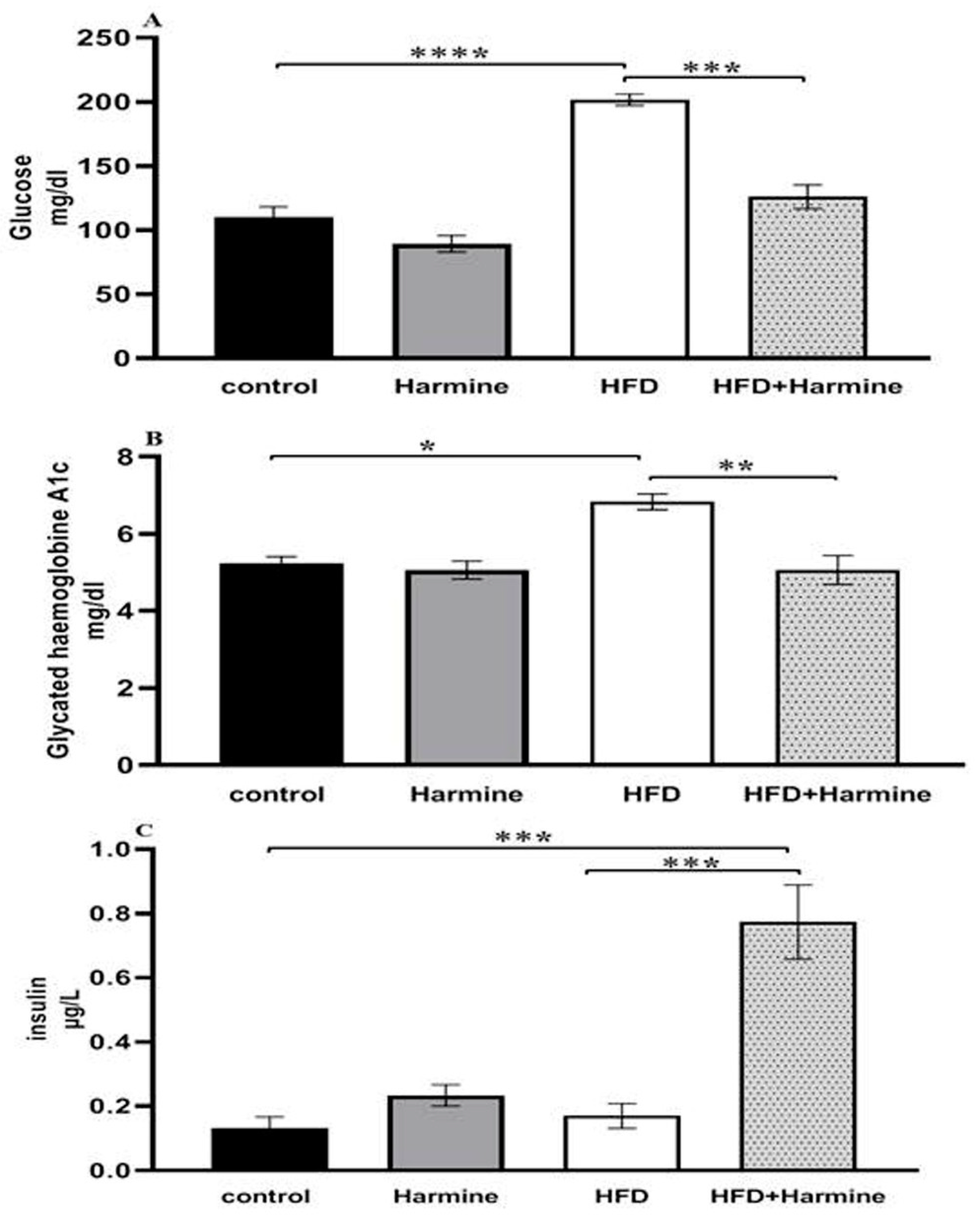
3.2.2. Blood Glucose Levels, Glycated Hemoglobin A1C, and Insulin
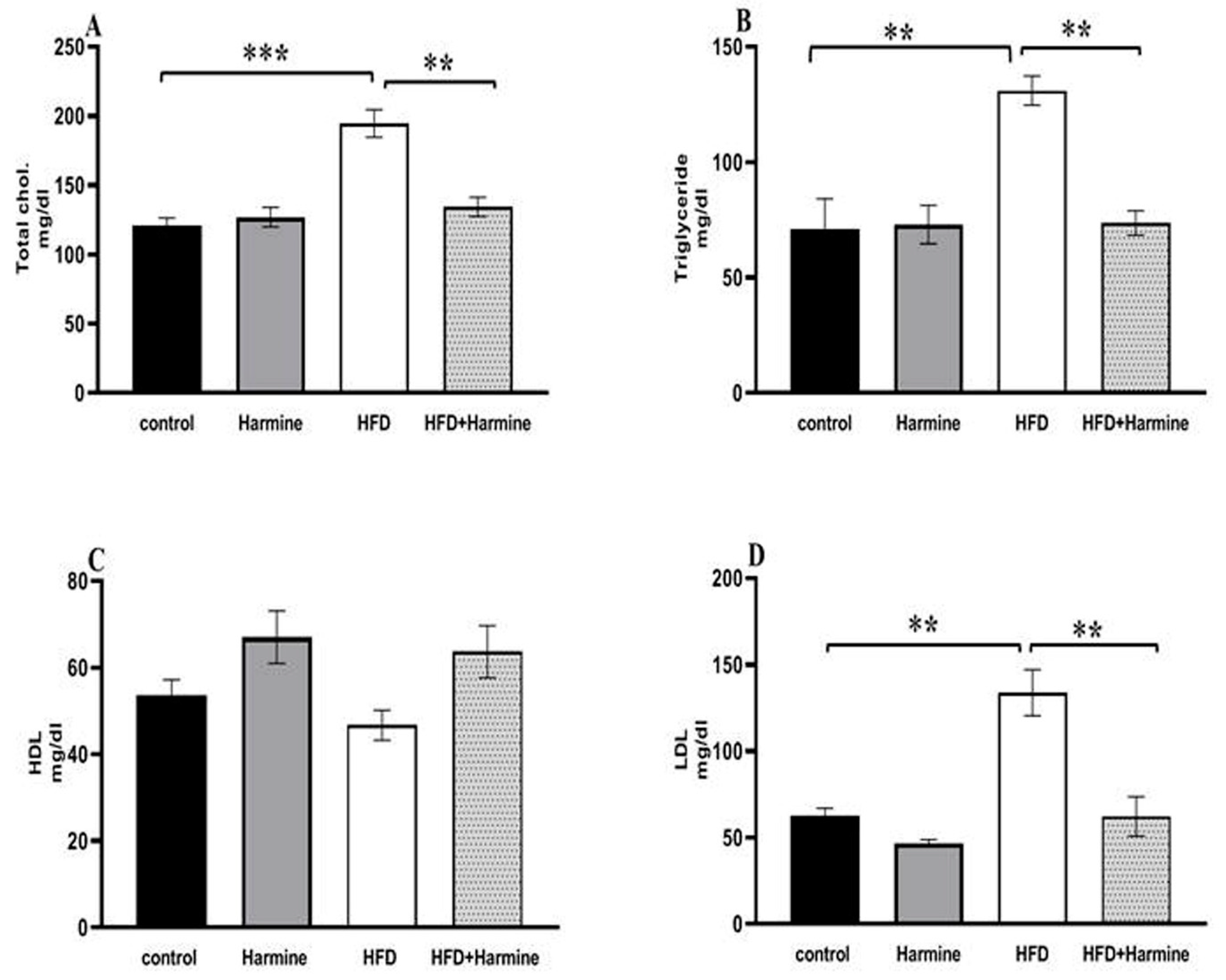
3.2.3. Lipid Profile
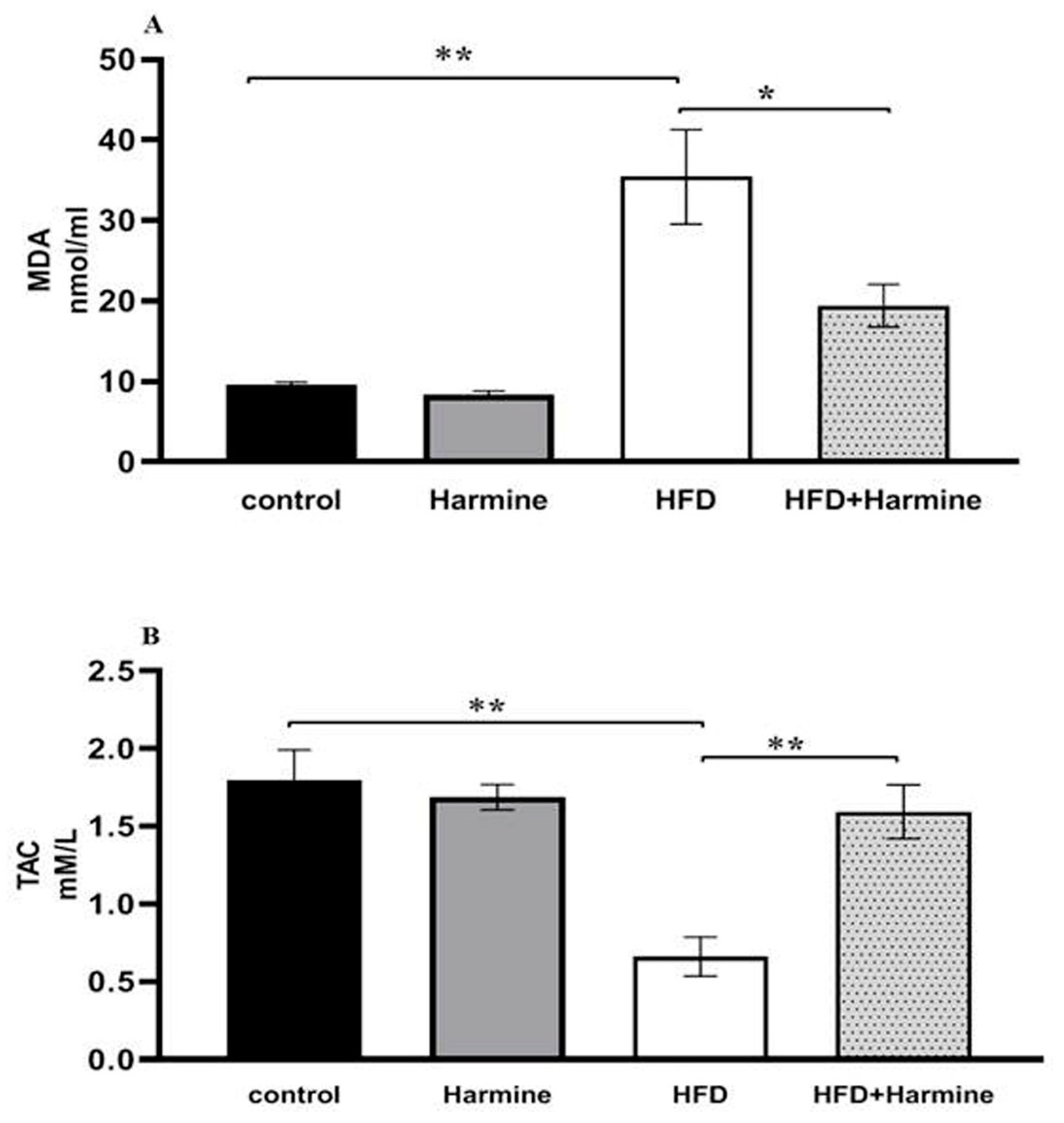
3.2.4. Malondialdehyde and Total Antioxidant Capacity
3.3. Histological Studies
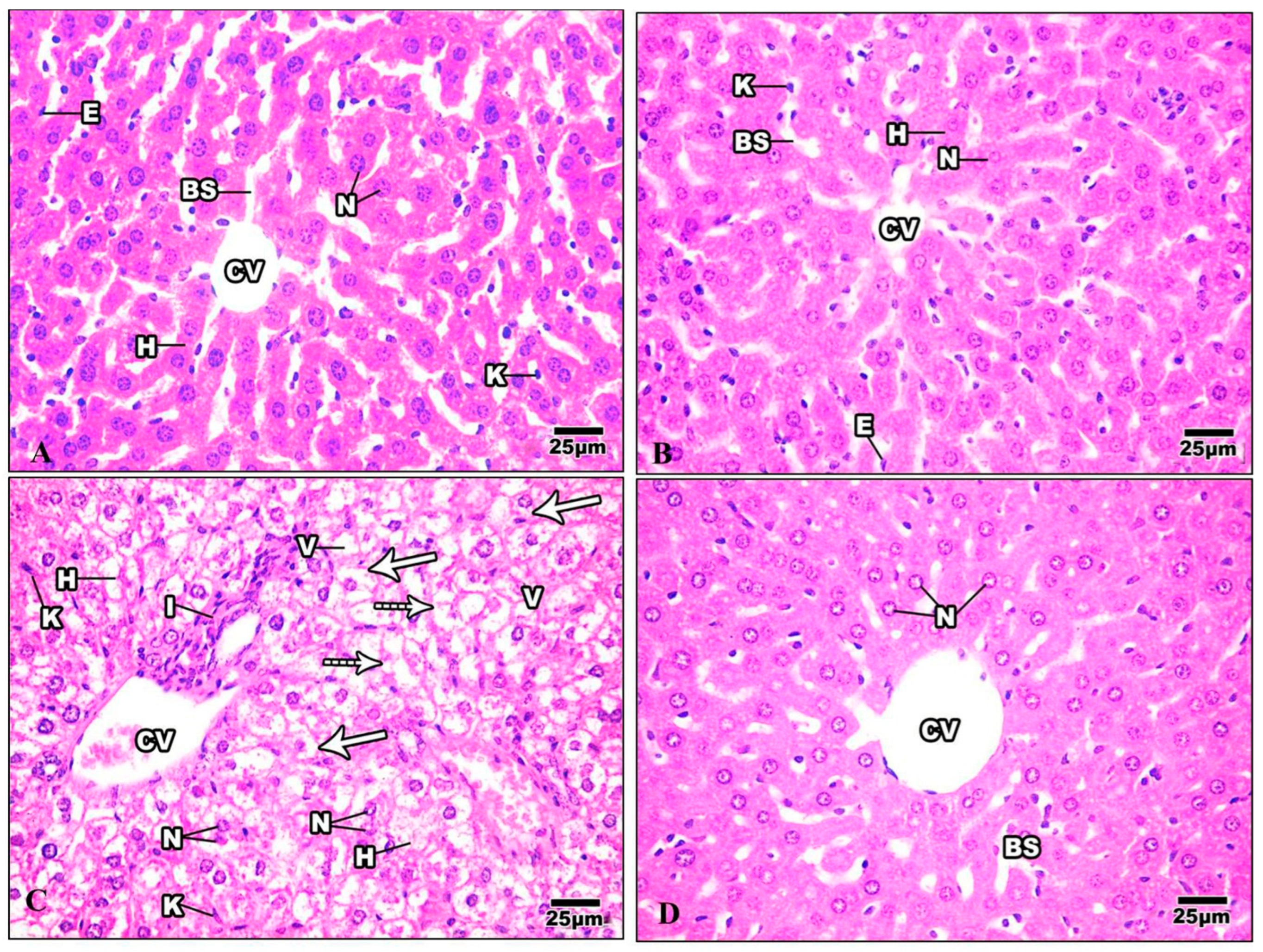
3.3.1. Liver
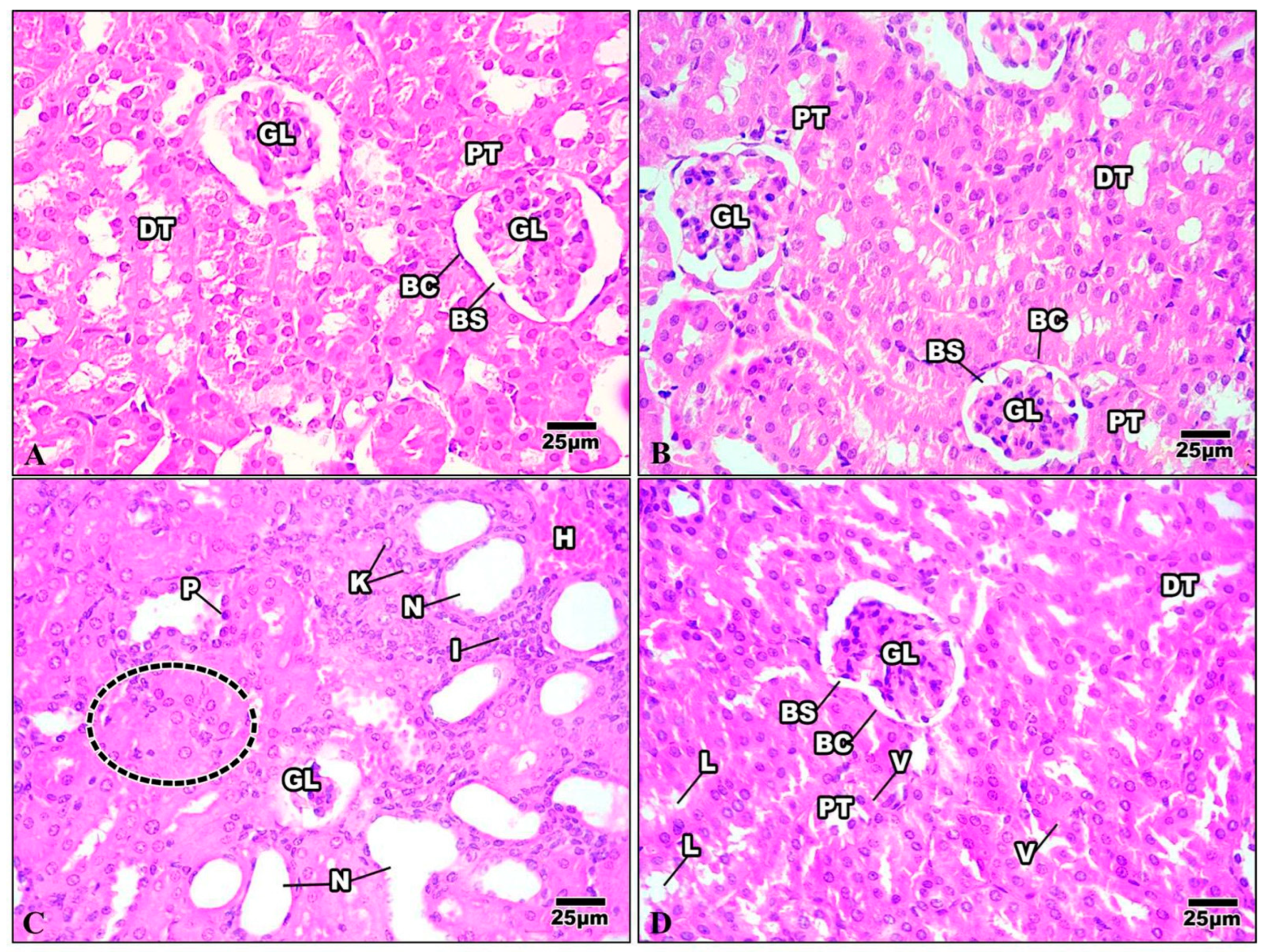
3.3.2. Kidney
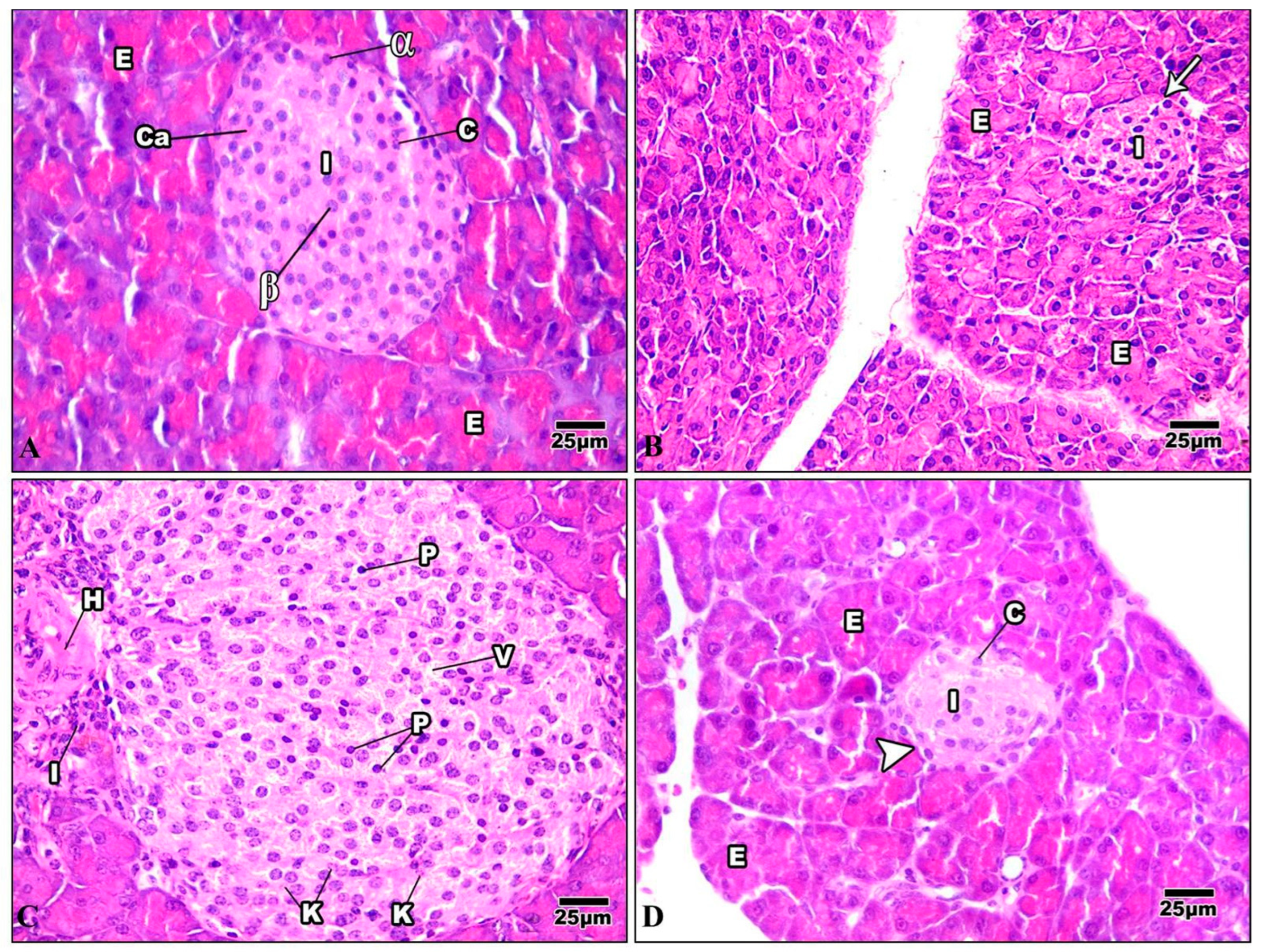
3.3.3. Pancreas
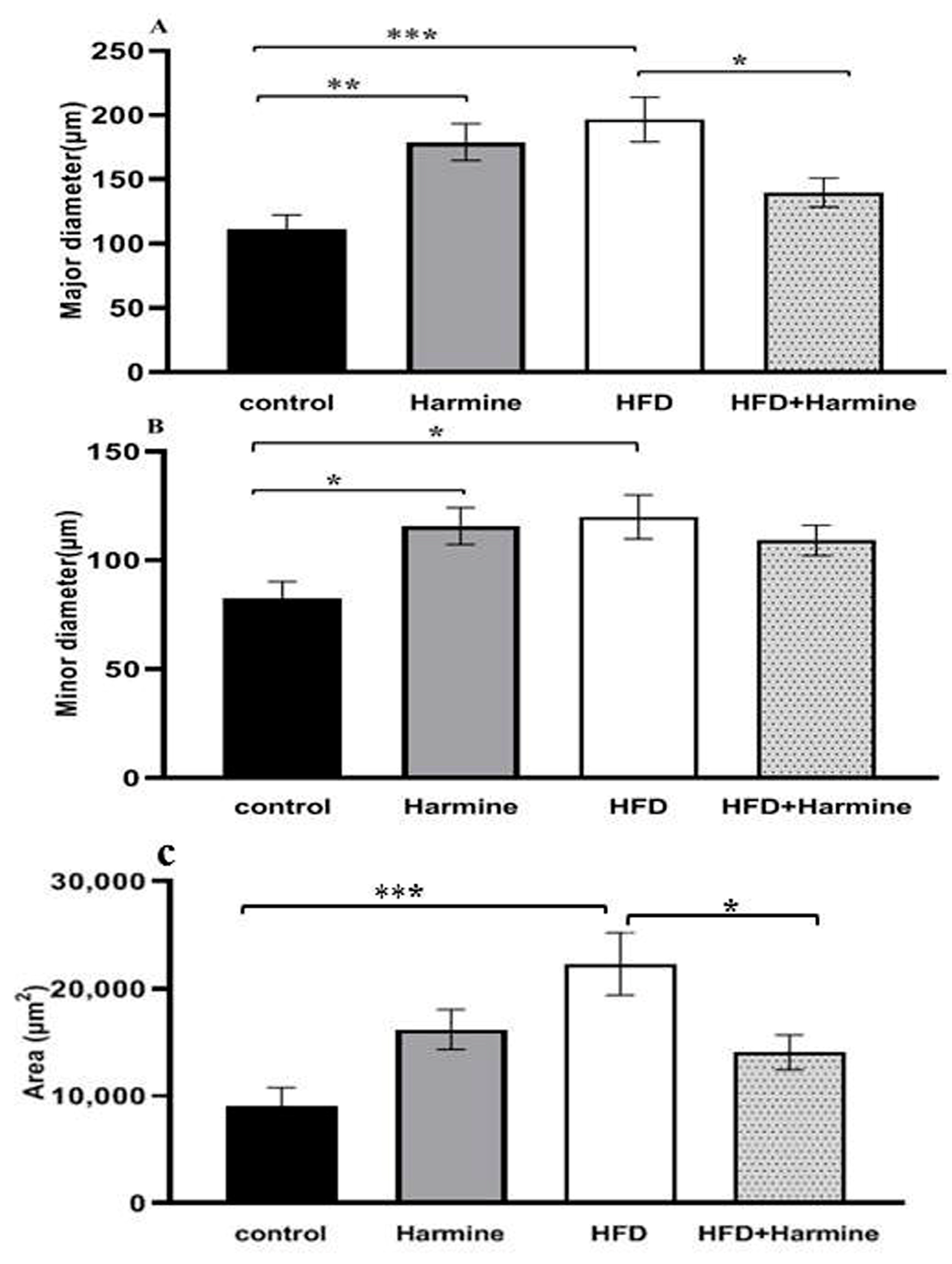
3.4. Morphometric Observations of Pancreatic Islets
3.5. Ultrastructural Studies
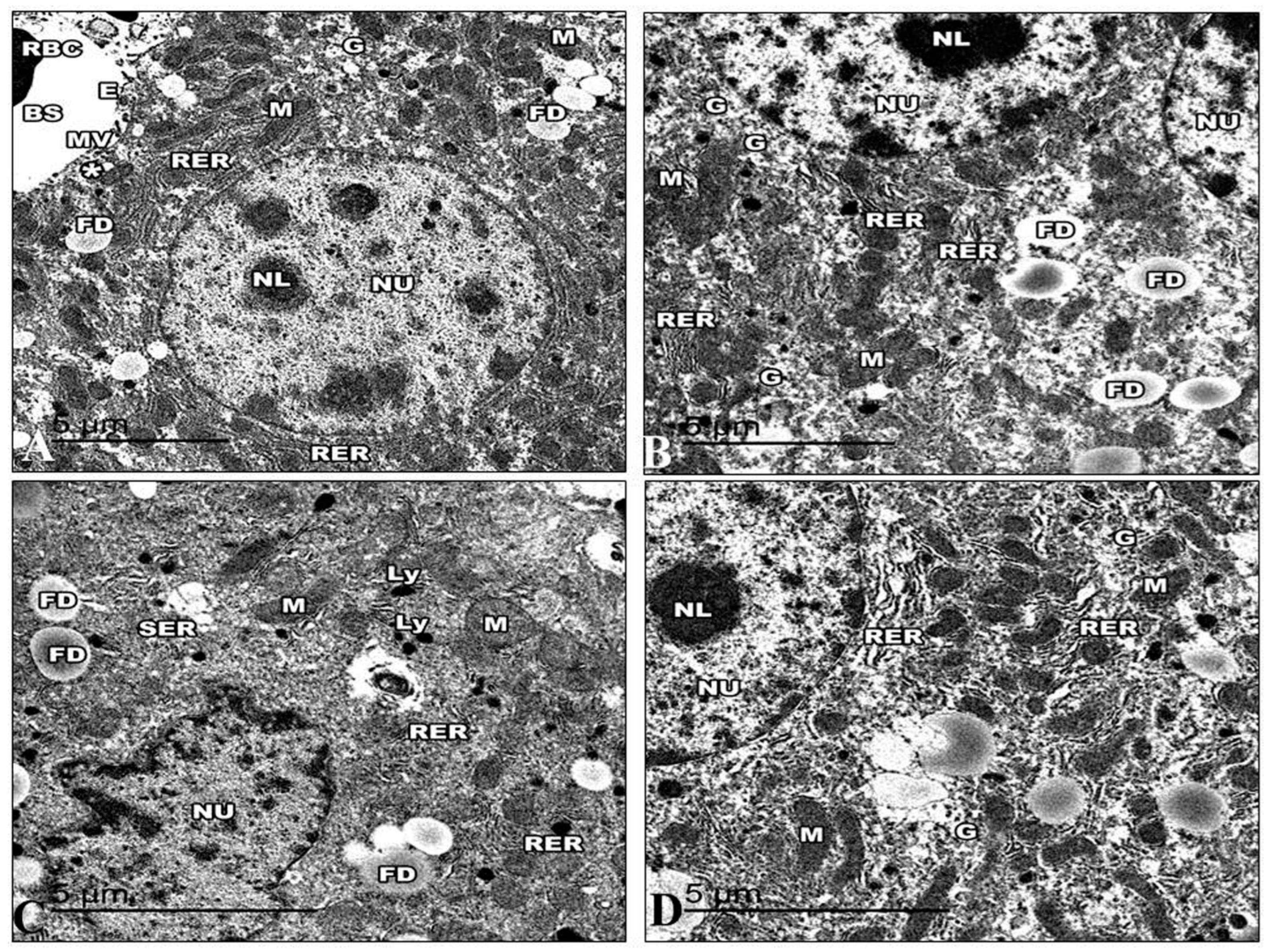
3.5.1. Liver
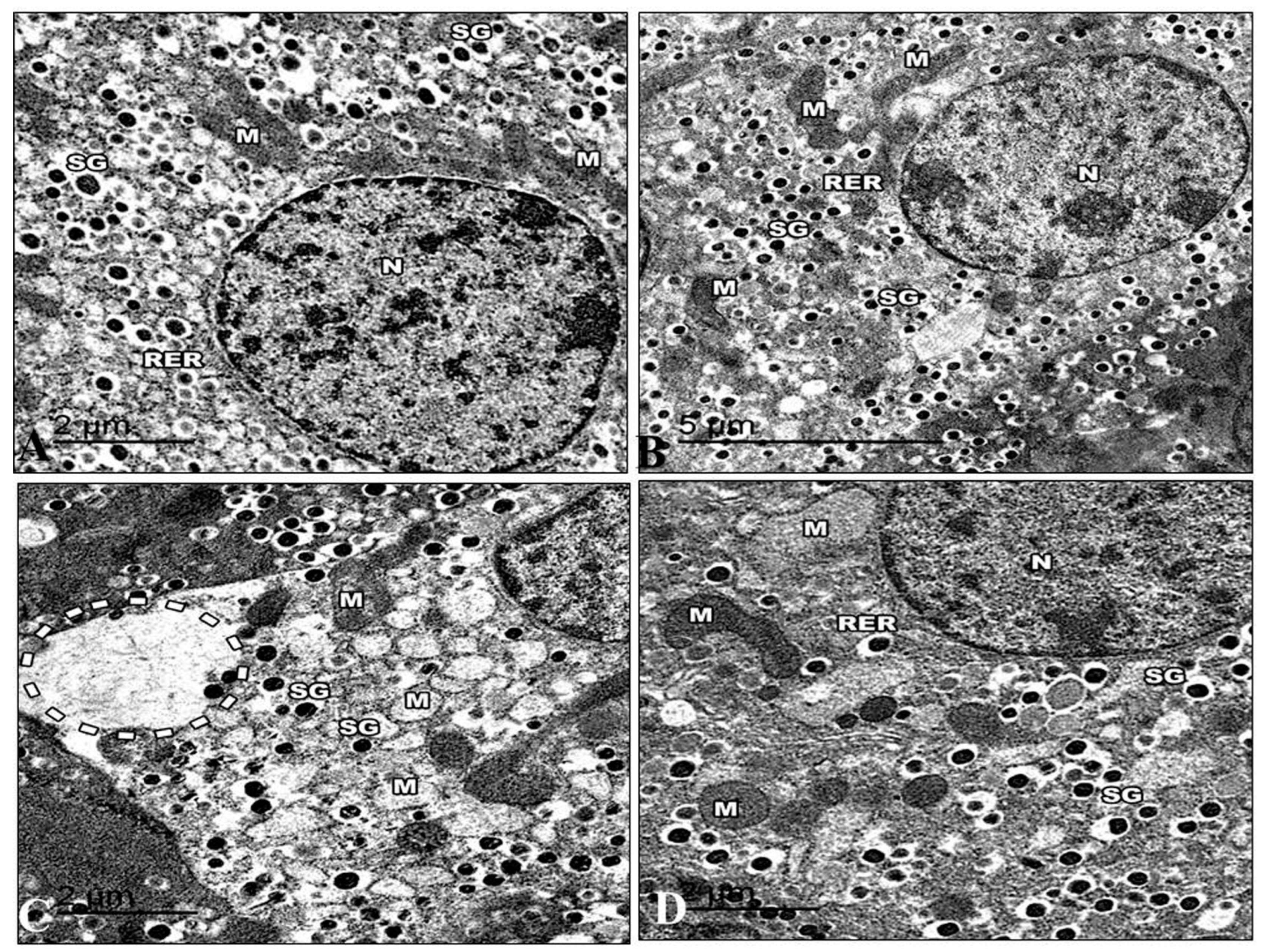
3.5.2. Pancreas
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Seong, J.; Kang, J.Y.; Sun, J.S.; Kim, K.W. Hypothalamic inflammation and obesity: A mechanistic review. Arch. Pharm. Res. 2019, 42, 383–392. [Google Scholar] [CrossRef]
- Brown, J.C.; Harhay, M.O.; Harhay, M.N. The Value of Anthropometric Measures in Nutrition and Metabolism: Comment on Anthropometrically Predicted Visceral Adipose Tissue and Blood-Based Biomarkers: A Cross-Sectional Analysis. Nutr. Metab. Insights 2019, 12, 1178638819831712. [Google Scholar] [CrossRef] [PubMed]
- Deacon, C.F. Physiology and Pharmacology of DPP-4 in Glucose Homeostasis and the Treatment of Type 2 Diabetes. Front. Endocrinol. 2019, 10, 80. [Google Scholar] [CrossRef] [PubMed]
- Freeman, A.M.; Pennings, N. Insulin Resistance. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Rachdaoui, N. Insulin: The Friend and the Foe in the Development of Type 2 Diabetes Mellitus. Int. J. Mol. Sci. 2020, 21, 1770. [Google Scholar] [CrossRef] [PubMed]
- Kharroubi, A.T.; Darwish, H.M. Diabetes mellitus: The epidemic of the century. World J. Diabetes 2015, 6, 850–867. [Google Scholar] [CrossRef]
- Ganz, M.L.; Wintfeld, N.; Li, Q.; Alas, V.; Langer, J.; Hammer, M. The association of body mass index with the risk of type 2 diabetes: A case-control study nested in an electronic health records system in the United States. Diabetol. Metab. Syndr. 2014, 6, 50. [Google Scholar] [CrossRef]
- Wang, C.Y.; Liao, J.K. A Mouse Model of Diet-Induced Obesity and Insulin Resistance. In Mtor: Methods and Protocols; Weichhart, T., Ed.; Methods in Molecular Biology; Humana Press: Totowa, NJ, USA, 2012; Volume 821, pp. 421–433. [Google Scholar]
- Bano, G. Glucose homeostasis, obesity and diabetes. Best Pract. Res. Clin. Obstet. Gynaecol. 2013, 27, 715–726. [Google Scholar] [CrossRef]
- Alnohair, S. Obesity in Gulf Countries. Int. J. Health Sci. -Ijhs 2014, 8, 79–83. [Google Scholar] [CrossRef]
- Kutbi, M.S.; Alhrgan, S.T.; Almehmadi, M.M.; Abdullah, A.A.A.; Alkhudhari, A.A.I.; Soqati, A.A.; Alhammad, A.A.; Felimban, N.S.; Darweesh, B.A.; Altowairqi, M.H.R.; et al. Prevalence and management of obesity. Indo Am. J. Pharm. Sci. 2018, 5, 11904–11909. [Google Scholar] [CrossRef]
- Papandreou, C.; Abu Mourad, T.; Jildeh, C.; Abdeen, Z.; Philalithis, A.; Tzanakis, N. Obesity in Mediterranean region (1997–2007): A systematic review. Obes. Rev. 2008, 9, 389–399. [Google Scholar] [CrossRef]
- Afshari, M.; Teymourlouy, A.A.; Asadi-Lari, M.; Maleki, M. Global Health diplomacy for noncommunicable diseases prevention and control: A systematic review. Glob. Health 2020, 16, 41. [Google Scholar] [CrossRef]
- Aboulghate, M.; Elaghoury, A.; Elebrashy, I.; Elkafrawy, N.; Elshishiney, G.; Abul-Magd, E.; Bassiouny, E.; Toaima, D.; Elezbawy, B.; Fasseeh, A.; et al. The Burden of Obesity in Egypt. Front. Public. Health 2021, 9, 718978. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.M.M.; Lima, D.R.A. Coffee consumption, obesity and type 2 diabetes: A mini-review. Eur. J. Nutr. 2016, 55, 1345–1358. [Google Scholar] [CrossRef]
- Lumeng, C.N.; Saltiel, A.R. Inflammatory links between obesity and metabolic disease. J. Clin. Investig. 2011, 121, 2111–2117. [Google Scholar] [CrossRef]
- Gregor, M.F.; Hotamisligil, G.S. Inflammatory Mechanisms in Obesity. Annu. Rev. Immunol. 2011, 29, 415–445. [Google Scholar] [CrossRef]
- Samuel, V.T.; Shulman, G.I. Mechanisms for Insulin Resistance: Common Threads and Missing Links. Cell 2012, 148, 852–871. [Google Scholar] [CrossRef]
- Harith, H.H.; Morris, M.J.; Kavurma, M.M. On the TRAIL of obesity and diabetes. Trends Endocrinol. Metab. 2013, 24, 578–587. [Google Scholar] [CrossRef]
- Jacob, B.; Narendhirakannan, R.T. Role of medicinal plants in the management of diabetes mellitus: A review. 3 Biotech 2019, 9, 4. [Google Scholar] [CrossRef]
- Kooti, W.; Farokhipour, M.; Asadzadeh, Z.; Ashtary-Larky, D.; Asadi-Samani, M. The role of medicinal plants in the treatment of diabetes: A systematic review. Electron. Physician 2016, 8, 1832–1842. [Google Scholar] [CrossRef]
- Zhang, L.; Li, D.C.; Yu, S.L. Pharmacological effects of harmine and its derivatives: A review. Arch. Pharmacal. Res. 2020, 43, 1259–1275. [Google Scholar] [CrossRef] [PubMed]
- Sethi, J.K.; Vidal-Puig, A.J. Targeting fat to prevent diabetes. Cell Metab. 2007, 5, 323–325. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, P.; Alvarez-Perez, J.C.; Felsenfeld, D.P.; Liu, H.T.; Sivendran, S.; Bender, A.; Kumar, A.; Sanchez, R.; Scott, D.K.; Garcia-Ocana, A.; et al. A high-throughput chemical screen reveals that harmine-mediated inhibition of DYRK1A increases human pancreatic beta cell replication. Nat. Med. 2015, 21, 383. [Google Scholar] [CrossRef]
- Kumar, K.; Wang, P.; Sanchez, R.; Swartz, E.A.; Stewart, A.F.; Devita, R.J. Development of Kinase-Selective, Harmine-Based DYRK1A Inhibitors that Induce Pancreatic Human beta-Cell Proliferation. J. Med. Chem. 2018, 61, 7687–7699. [Google Scholar] [CrossRef]
- Liu, X.; Li, M.; Tan, S.; Wang, C.; Fan, S.; Huang, C. Harmine is an inflammatory inhibitor through the suppression of NF-κB signaling. Biochem. Biophys. Res. Commun. 2017, 489, 332–338. [Google Scholar] [CrossRef]
- Waki, H.; Park, K.W.; Mitro, N.; Pei, L.M.; Damoiseaux, R.; Wilpitz, D.C.; Reue, K.; Saez, E.; Tontonoz, P. The small molecule harmine is an antidiabetic cell-type-specific regulator of PPAR gamma expression. Cell Metab. 2007, 5, 357–370. [Google Scholar] [CrossRef] [PubMed]
- Axen, K.V.; Axen, K. Very low-carbohydrate versus isocaloric high-carbohydrate diet in dietary obese rats. Obesity 2006, 14, 1344–1352. [Google Scholar] [CrossRef]
- Rodrigues Silva, V.R.; Katashima, C.; Lenhare, L.; Silva, C.; Morari, J.; Camargo, R.; Velloso, L.; Saad, M.; Silva, A.; Pauli, J.; et al. Chronic exercise reduces hypothalamic transforming growth factor-β1 in middle-aged obese mice. Aging 2017, 9, 1926–1940. [Google Scholar] [CrossRef]
- Mori, N.; Kurata, M.; Yamazaki, H.; Hosokawa, H.; Nadamoto, T.; Inoue, K.; Fushiki, T. Intragastric Administration of Allyl Isothiocyanate Reduces Hyperglycemia in Intraperitoneal Glucose Tolerance Test (IPGTT) by Enhancing Blood Glucose Consumption in Mice. J. Nutr. Sci. Vitaminol. 2013, 59, 56–63. [Google Scholar] [CrossRef]
- Abdelrazek, H.M.A.; Kilany, O.E.; Muhammad, M.A.A.; Tag, H.M.; Abdelazim, A.M. Black Seed Thymoquinone Improved Insulin Secretion, Hepatic Glycogen Storage, and Oxidative Stress in Streptozotocin-Induced Diabetic Male Wistar Rats. Oxid. Med. Cell Longev. 2018, 2018, 8104165. [Google Scholar] [CrossRef]
- Kilany, O.E.; Abdelrazek, H.M.A.; Aldayel, T.S.; Abdo, S.; Mahmoud, M.M.A. Anti-obesity potential of Moringa olifera seed extract and lycopene on high fat diet induced obesity in male Sprauge Dawely rats. Saudi J. Biol. Sci. 2020, 27, 2733–2746. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, T.; Matsui, S. Effect of Acetic Acid Concentration on the Color Reaction in the o-Toluidine-Boric Acid Method for Blood Glucose Estimation. Jpn. J. Clin. Chem. 1972, 1, 346–353. [Google Scholar] [CrossRef]
- Misciagna, G.; Logroscino, G.; De Michele, G.; Cisternino, A.M.; Guerra, V.; Freudenheim, J.L. Fructosamine, glycated hemoglobin, and dietary carbohydrates. Clin. Chim. Acta 2004, 340, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Hood, S.; Wang, Y.; Bezverkov, R.; Dou, C.; Datta, A.; Yuan, C. Direct enzymatic assay for %HbA1c in human whole blood samples. Clin. Biochem. 2008, 41, 576–583. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.K.; Jeong, J.; Kang, E.Y.; Go, G.W. Red Pepper (Capsicum annuum L.) Seed Extract Improves Glycemic Control by Inhibiting Hepatic Gluconeogenesis via Phosphorylation of FOXO1 and AMPK in Obese Diabeticdb/dbMice. Nutrients 2020, 12, 2546. [Google Scholar] [CrossRef]
- Jacobs, R.M.; Lumsden, J.H.; Taylor, J.A.; Grift, E. Effects of interferents on the kinetic Jaffé reaction and an enzymatic colorimetric test for serum creatinine concentration determination in cats, cows, dogs and horses. Can. J. Vet. Res. 1991, 55, 150–154. [Google Scholar]
- Fairney, A. Clinical guide to laboratory tests—Tietz, NW. Lancet 1984, 1, 487–488. [Google Scholar]
- Sardesai, V.M.; Manning, J.A. The Determination of Triglycerides in Plasma and Tissues. Clin. Chem. 1968, 14, 156–161. [Google Scholar] [CrossRef]
- van Duijnhoven, F.J.; Bueno-De-Mesquita, H.B.; Calligaro, M.; Jenab, M.; Pischon, T.; Jansen, E.H.; Frohlich, J.; Ayyobi, A.; Overvad, K.; Toft-Petersen, A.P.; et al. Blood lipid and lipoprotein concentrations and colorectal cancer risk in the European Prospective Investigation into Cancer and Nutrition. Gut 2011, 60, 1094–1102. [Google Scholar] [CrossRef] [PubMed]
- Suryawanshi, N.P.; Bhutey, A.K.; Nagdeote, A.N.; Jadhav, A.A.; Manoorkar, G.S. Study of lipid peroxide and lipid profile in diabetes mellitus. Indian. J. Clin. Biochem. 2006, 21, 126–130. [Google Scholar] [CrossRef]
- Koracevic, D.; Koracevic, G.; Djordjevic, V.; Andrejevic, S.; Cosic, V. Method for the measurement of antioxidant activity in human fluids. J. Clin. Pathol. 2001, 54, 356–361. [Google Scholar] [CrossRef]
- Fischer, A.H.; Jacobson, K.A.; Rose, J.; Zeller, R. Hematoxylin and eosin staining of tissue and cell sections. CSH Protoc. 2008, 2008, pdb.prot4986. [Google Scholar] [CrossRef]
- da Silva, T.A.; Lemes, R.M.; Oliveira, C.J.F.; Almeida, A.D.; Chica, J.E.L. Data on morphometric analysis of the pancreatic islets from C57BL/6 and BALB/c mice. Data Brief 2016, 8, 1094–1098. [Google Scholar] [CrossRef] [PubMed]
- Lynn, J.A. Rapid Toluidine Blue Staining of Epon-Embedded and Mounted “Adjacent” Sections. Am. J. Clin. Pathol. 1965, 44, 57–58. [Google Scholar] [CrossRef] [PubMed]
- Hopwood, D. Theoretical and practical aspects of glutaraldehyde fixation. In Fixation in Histochemistry; Stoward, P.J., Ed.; Springer: Boston, MA, USA, 1973; pp. 47–83. [Google Scholar]
- Spurr, A.R. A low-viscosity epoxy resin embedding medium for electron microscopy. J. Ultrastruct. Res. 1969, 26, 31. [Google Scholar] [CrossRef]
- Son, D.J.; Hwang, S.Y.; Kim, M.H.; Park, U.K.; Kim, B.S. Anti-Diabetic and Hepato-Renal Protective Effects of Ziyuglycoside II Methyl Ester in Type 2 Diabetic Mice. Nutrients 2015, 7, 5469–5483. [Google Scholar] [CrossRef]
- Beiroa, D.; Imbernon, M.; Gallego, R.; Senra, A.; Herranz, D.; Villarroya, F.; Serrano, M.; Ferno, J.; Salvador, J.; Escalada, J.; et al. GLP-1 Agonism Stimulates Brown Adipose Tissue Thermogenesis and Browning Through Hypothalamic AMPK. Diabetes 2014, 63, 3346–3358. [Google Scholar] [CrossRef]
- Bi, P.P.; Shan, T.Z.; Liu, W.Y.; Yue, F.; Yang, X.; Liang, X.R.; Wang, J.H.; Li, J.; Carlesso, N.; Liu, X.Q.; et al. Inhibition of Notch signaling promotes browning of white adipose tissue and ameliorates obesity. Nat. Med. 2014, 20, 911–918. [Google Scholar] [CrossRef]
- Roberts, L.D.; Boström, P.; O’Sullivan, J.F.; Schinzel, R.T.; Lewis, G.D.; Dejam, A.; Lee, Y.-K.; Palma, M.J.; Calhoun, S.; Georgiadi, A.; et al. β-Aminoisobutyric acid induces browning of white fat and hepatic β-oxidation and is inversely correlated with cardiometabolic risk factors. Cell Metab. 2014, 19, 96–108. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, R.; Meng, Y.; Li, S.W.; Donelan, W.; Zhao, Y.; Qi, L.; Zhang, M.X.; Wang, X.L.; Cui, T.X.; et al. Irisin Stimulates Browning of White Adipocytes Through Mitogen-Activated Protein Kinase p38 MAP Kinase and ERK MAP Kinase Signaling. Diabetes 2014, 63, 514–525. [Google Scholar] [CrossRef]
- Nie, T.; Hui, X.Y.; Mao, L.F.; Nie, B.M.; Li, K.; Sun, W.; Gao, X.F.; Tang, X.F.; Xu, Y.; Jiang, B.S.; et al. Harmine Induces Adipocyte Thermogenesis through RAC1-MEK-ERK-CHD4 Axis. Sci. Rep. 2016, 6, 36382. [Google Scholar] [CrossRef]
- Tsuru, H.; Osaka, M.; Hiraoka, Y.; Yoshida, M. HFD-induced hepatic lipid accumulation and inflammation are decreased in Factor D deficient mouse. Sci. Rep. 2020, 10, 17593. [Google Scholar] [CrossRef]
- Boni-Schnetzler, M.; Boller, S.; Debray, S.; Bouzakri, K.; Meier, D.T.; Prazak, R.; Kerr-Conte, J.; Pattou, F.; Ehses, J.A.; Schuit, F.C.; et al. Free Fatty Acids Induce a Proinflammatory Response in Islets via the Abundantly Expressed Interleukin-1 Receptor I. Endocrinology 2009, 150, 5218–5229. [Google Scholar] [CrossRef]
- Yu, Y.; Mo, H.; Zhuo, H.; Yu, C.; Liu, Y. High Fat Diet Induces Kidney Injury via Stimulating Wnt/β-Catenin Signaling. Front. Med. 2022, 9, 851618. [Google Scholar] [CrossRef]
- Zhang, X.L.; Cui, Y.Q.; Fang, L.; Li, F. Chronic High-Fat Diets Induce Oxide Injuries and Fibrogenesis of Pancreatic Cells in Rats. Pancreas 2008, 37, E31–E38. [Google Scholar] [CrossRef]
- Fraulob, J.C.; Ogg-Diamantino, R.; Fernandes-Santos, C.; Aguila, M.B.; Mandarim-de-Lacerda, C.A. A Mouse Model of Metabolic Syndrome: Insulin Resistance, Fatty Liver and Non-Alcoholic Fatty Pancreas Disease (NAFPD) in C57BL/6 Mice Fed a High Fat Diet. J. Clin. Biochem. Nutr. 2010, 46, 212–223. [Google Scholar] [CrossRef] [PubMed]
- Path, G.; Mehana, A.E.; Pilz, I.H.; Alt, M.; Baumann, J.; Sommerer, I.; Hoffmeister, A.; Seufert, J. NUPR1 preserves insulin secretion of pancreatic beta-cells during inflammatory stress by multiple low-dose streptozotocin and high-fat diet. Am. J. Physiol. Endocrinol. Metab. 2020, 319, E338–E344. [Google Scholar] [CrossRef] [PubMed]
- Hull, R.L.; Kodama, K.; Utzschneider, K.M.; Carr, D.B.; Prigeon, R.L.; Kahn, S.E. Dietary-fat-induced obesity in mice results in beta cell hyperplasia but not increased insulin release: Evidence for specificity of impaired beta cell adaptation. Diabetologia 2005, 48, 1350–1358. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N.; Gill, J.M.R. Type 2 diabetes as a disease of ectopic fat? BMC Med. 2014, 12, 123. [Google Scholar] [CrossRef]
- Finegood, D.T.; McArthur, M.D.; Kojwang, D.; Thomas, M.J.; Topp, B.G.; Leonard, T.; Buckingham, R.E. beta-cell mass dynamics in Zucker diabetic fatty rats—Rosiglitazone prevents the rise in net cell death. Diabetes 2001, 50, 1021–1029. [Google Scholar] [CrossRef]
- Butler, A.E.; Janson, J.; Soeller, W.C.; Butler, P.C. Increased β-Cell Apoptosis Prevents Adaptive Increase in β-Cell Mass in Mouse Model of Type 2 Diabetes: Evidence for Role of Islet Amyloid Formation Rather Than Direct Action of Amyloid. Diabetes 2003, 52, 2304–2314. [Google Scholar] [CrossRef]
- Montanya, E.; Nacher, V.; Biarnes, M.; Soler, J. Linear correlation between beta-cell mass and body weight throughout the lifespan in Lewis rats—Role of beta-cell hyperplasia and hypertrophy. Diabetes 2000, 49, 1341–1346. [Google Scholar] [CrossRef] [PubMed]
- Gulen, M.I.; Bagla, A.G.; Yavuz, O.; Hismiogullari, A.A. Histopathological changes in rat pancreas and skeletal muscle associated with high fat diet induced insulin resistance. Biotech. Histochem. 2015, 90, 495–505. [Google Scholar] [CrossRef] [PubMed]
- Luria, A.; Bettaieb, A.; Xi, Y.; Shieh, G.J.; Liu, H.C.; Inoue, H.; Tsai, H.J.; Imig, J.D.; Haj, F.G.; Hammock, B.D. Soluble epoxide hydrolase deficiency alters pancreatic islet size and improves glucose homeostasis in a model of insulin resistance. Proc. Natl. Acad. Sci. USA 2011, 108, 9038–9043. [Google Scholar] [CrossRef] [PubMed]
- Camastra, S.; Manco, M.; Mari, A.; Baldi, S.; Gastaldelli, A.; Greco, A.V.; Mingrone, G.; Ferrannini, E. beta-cell function in morbidly obese subjects during free living—Long-term effects of weight loss. Diabetes 2005, 54, 2382–2389. [Google Scholar] [CrossRef] [PubMed]
- Slavin, B.G.; Zarow, C.; Warden, C.H.; Fisler, J.S. Histological, Immunocytochemical, and Morphometrical Analyses of Pancreatic Islets in the BSB Mouse Model of Obesity. Anat. Rec. -Adv. Integr. Anat. Evol. Biol. 2010, 293, 108–116. [Google Scholar] [CrossRef]
- Kiki, I.; Altunkaynak, B.Z.; Altunkaynak, M.E.; Vuraler, O.; Unal, D.; Kaplan, S. Effect of high fat diet on the volume of liver and quantitative feature of Kupffer cells in the female rat: A stereological and ultrastructural study. Obes. Surg. 2007, 17, 1381–1388. [Google Scholar] [CrossRef]
- McCuskey, R.S.; Ito, Y.; Robertson, G.R.; McCuskey, M.K.; Perry, M.; Farrell, G.C. Hepatic microvascular dysfunction during evolution of dietary steatohepatitis in mice. Hepatology 2004, 40, 386–393. [Google Scholar] [CrossRef]
- Yin, W.; Yuan, Z.; Wang, Z.; Yang, B.; Yang, Y. A diet high in saturated fat and sucrose alters glucoregulation and induces aortic fatty streaks in New Zealand White rabbits. Int. J. Exp. Diabetes Res. 2002, 3, 179–184. [Google Scholar] [CrossRef]
- Friedman, T.; Sinha-Hikim, I.; Parveen, M.; Najjar, S.; Liu, Y.; Mangubat, M.; Shin, C.-S.; Lyzlov, A.; Ivey, R.; Shaheen, M.; et al. Additive Effects of Nicotine and High-Fat Diet on Hepatic Steatosis in Male Mice. Endocrinology 2012, 153, 5809–5820. [Google Scholar] [CrossRef]
- Sha, J.B.; Sui, B.; Su, X.Q.; Meng, Q.F.; Zhang, C.G. Alteration of oxidative stress and inflammatory cytokines induces apoptosis in diabetic nephropathy. Mol. Med. Rep. 2017, 16, 7715–7723. [Google Scholar] [CrossRef]
- Masini, M.; Marselli, L.; Bugliani, M.; De Martino, L.; Masiello, P.; Marchetti, P.; Tata, V. Ultrastructural morphometric analysis of insulin secretory granules in human type 2 diabetes. Acta Diabetol. 2012, 49, 247–252. [Google Scholar] [CrossRef]
- Masini, M.; Marselli, L.; Himpe, E.; De Martino, L.; Bugliani, M.; Suleiman, M.; Boggi, U.; Filipponi, F.; Occhipinti, M.; Bouwens, L.; et al. Co-localization of acinar markers and insulin in pancreatic cells of subjects with type 2 diabetes. PLoS ONE 2017, 12, e0179398. [Google Scholar] [CrossRef] [PubMed]
- Dirice, E.; Walpita, D.; Vetere, A.; Meier, B.C.; Kahraman, S.; Hu, J.; Dančík, V.; Burns, S.M.; Gilbert, T.J.; Olson, D.E.; et al. Inhibition of DYRK1A Stimulates Human β-Cell Proliferation. Diabetes 2016, 65, 1660–1671. [Google Scholar] [CrossRef] [PubMed]
- Youdim, M.B.H.; Edmondson, D.; Tipton, K.F. The therapeutic potential of monoamine oxidase inhibitors. Nat. Rev. Neurosci. 2006, 7, 295–309. [Google Scholar] [CrossRef] [PubMed]
- Diwan, S.Y. Effect of Peganum harmala methanol extract on liver and kidney of mice administered MTX drug. Al-Nahrain J. Sci. 2013, 16, 161–166. [Google Scholar] [CrossRef]
- Lu, J.; Bankovic-Calic, N.; Ogborn, M.; Saboorian, M.H.; Aukema, H.M. Detrimental Effects of a High Fat Diet in Early Renal Injury Are Ameliorated by Fish Oil in Han:SPRD-cy Rats. J. Nutr. 2003, 133, 180–186. [Google Scholar] [CrossRef]
- Bhole, V.; Choi, J.W.; Kim, S.W.; de Vera, M.; Choi, H. Serum uric acid levels and the risk of type 2 diabetes: A prospective study. Am. J. Med. 2010, 123, 957–961. [Google Scholar] [CrossRef]
- Park, S.Y.; Cho, Y.R.; Kim, H.J.; Higashimori, T.; Danton, C.; Lee, M.K.; Dey, A.; Rothermel, B.; Kim, Y.B.; Kalinowski, A.; et al. Unraveling the temporal pattern of diet-induced insulin resistance in individual organs and cardiac dysfunction in C57BL/6 mice. Diabetes 2005, 54, 3530–3540. [Google Scholar] [CrossRef]
- Salvi, R.; Abderrahmani, A. Decompensation of β-Cells in Diabetes: When Pancreatic β-Cells Are on ICE(R). J. Diabetes Res. 2014, 2014, 768024. [Google Scholar] [CrossRef]
- Churuangsuk, C.; Lean, M.E.J.; Combet, E. Lower carbohydrate and higher fat intakes are associated with higher hemoglobin A1c: Findings from the UK National Diet and Nutrition Survey 2008–2016. Eur. J. Nutr. 2020, 59, 2771–2782. [Google Scholar] [CrossRef]
- Vergès, B. Lipid disorders in type 1 diabetes. Diabetes Metab. 2009, 35, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Eisinger, K.; Liebisch, G.; Schmitz, G.; Aslanidis, C.; Krautbauer, S.; Buechler, C. Lipidomic analysis of serum from high fat diet induced obese mice. Int. J. Mol. Sci. 2014, 15, 2991–3002. [Google Scholar] [CrossRef]
- Kolbus, D.; Ramos, O.; Berg, K.; Persson, J.; Wigren, M.; Björkbacka, H.; Fredrikson, G.; Nilsson, J. CD8+ T cell activation predominate early immune responses to hypercholesterolemia in Apoe-/- mice. BMC Immunol. 2010, 11, 58. [Google Scholar] [CrossRef]
- Arisue, K.; Uchida, K.; Takeuchi, N. Changes in serum lipid and lipoproteins in alloxan-diabetic rats--studies for one year. Jikken Dobutsu. Exp. Anim. 1994, 43, 217–226. [Google Scholar] [CrossRef][Green Version]
- Mollashahi, E.; Kazerani, H.R. Metabolic effects of methanol extract of harmal (peganum harmal) in rats fed with normal diet. J. Int. Med. Today 2020, 26, 414–431. [Google Scholar] [CrossRef]
- Roskams, T.; Yang, S.Q.; Koteish, A.; Durnez, A.; DeVos, R.; Huang, X.W.; Achten, R.; Verslype, C.; Diehl, A.M. Oxidative stress and oval cell accumulation in mice and humans with alcoholic and nonalcoholic fatty liver disease. Am. J. Pathol. 2003, 163, 1301–1311. [Google Scholar] [CrossRef]
- Kaneto, H.; Nakatani, Y.; Kawamori, D.; Miyatsuka, T.; Matsuoka, T.-a.; Matsuhisa, M.; Yamasaki, Y. Role of oxidative stress, endoplasmic reticulum stress, and c-Jun N-terminal kinase in pancreatic β-cell dysfunction and insulin resistance. Int. J. Biochem. Cell Biol. 2005, 37, 1595–1608. [Google Scholar] [CrossRef]
- Khan, Z.A.; Farhangkhoee, H.; Chakrabarti, S. Towards newer molecular targets for chronic diabetic complications. Curr. Vasc. Pharmacol. 2006, 4, 45–57. [Google Scholar] [CrossRef]
- Jin, L.; Xue, H.Y.; Jin, L.J.; Li, S.Y.; Xu, Y.P. Antioxidant and pancreas-protective effect of aucubin on rats with streptozotocin-induced diabetes. Eur. J. Pharmacol. 2008, 582, 162–167. [Google Scholar] [CrossRef]
- Picton, S.F.; Flatt, P.R.; McClenaghan, N.H. Differential acute and long term actions of succinic acid monomethyl ester exposure on insulin-secreting BRIN-BD11 cells. Int. J. Exp. Diabetes Res. 2001, 2, 19–27. [Google Scholar] [CrossRef]
- Evans, J.L.; Goldfine, I.D.; Maddux, B.A.; Grodsky, G.M. Are oxidative stress-activated signaling pathways mediators of insulin resistance and beta-cell dysfunction? Diabetes 2003, 52, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Komeili, G.; Hashemi, M.; Bameri-niafar, M. Evaluation of Antidiabetic and Antihyperlipidemic Effects of Peganum harmala Seeds in Diabetic Rats. Cholesterol 2016, 2016, 7389864. [Google Scholar] [CrossRef] [PubMed]
- Tarpley, M.; Oladapo, H.O.; Strepay, D.; Caligan, T.B.; Chdid, L.; Shehata, H.; Roques, J.R.; Thomas, R.; Laudeman, C.P.; Onyenwoke, R.U.; et al. Identification of harmine and beta-carboline analogs from a high-throughput screen of an approved drug collection; profiling as differential inhibitors of DYRK1A and monoamine oxidase A and for in vitro and in vivo anti-cancer studies. Eur. J. Pharm. Sci. 2021, 162, 105821. [Google Scholar] [CrossRef] [PubMed]
- Moloudizargari, M.; Mikaili, P.; Aghajanshakeri, S.; Asghari, M.H.; Shayegh, J. Pharmacological and therapeutic effects of Peganum harmala and its main alkaloids. Pharmacogn. Rev. 2013, 7, 199–212. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morsy, M.H.E.; Nabil, Z.I.; Darwish, S.T.; Al-Eisa, R.A.; Mehana, A.E. Anti-Diabetic and Anti-Adipogenic Effect of Harmine in High-Fat-Diet-Induced Diabetes in Mice. Life 2023, 13, 1693. https://doi.org/10.3390/life13081693
Morsy MHE, Nabil ZI, Darwish ST, Al-Eisa RA, Mehana AE. Anti-Diabetic and Anti-Adipogenic Effect of Harmine in High-Fat-Diet-Induced Diabetes in Mice. Life. 2023; 13(8):1693. https://doi.org/10.3390/life13081693
Chicago/Turabian StyleMorsy, Menna H. E., Zohour I. Nabil, Samah T. Darwish, Rasha A. Al-Eisa, and Amir E. Mehana. 2023. "Anti-Diabetic and Anti-Adipogenic Effect of Harmine in High-Fat-Diet-Induced Diabetes in Mice" Life 13, no. 8: 1693. https://doi.org/10.3390/life13081693
APA StyleMorsy, M. H. E., Nabil, Z. I., Darwish, S. T., Al-Eisa, R. A., & Mehana, A. E. (2023). Anti-Diabetic and Anti-Adipogenic Effect of Harmine in High-Fat-Diet-Induced Diabetes in Mice. Life, 13(8), 1693. https://doi.org/10.3390/life13081693





