Risk Prediction Model of Early-Onset Preeclampsia Based on Risk Factors and Routine Laboratory Indicators
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clinical and Biochemical Data Collection
2.3. Instruments and Reagents
2.4. Statistical Analysis
2.4.1. Logistic Regression Model
2.4.2. Machine Learning
Decision Tree Model
Support Vector Machine (SVM)
3. Results
3.1. Participants’ Clinical Characteristics
3.2. Comparison of Risk Factors
3.3. Comparison of Routine Laboratory Indicators
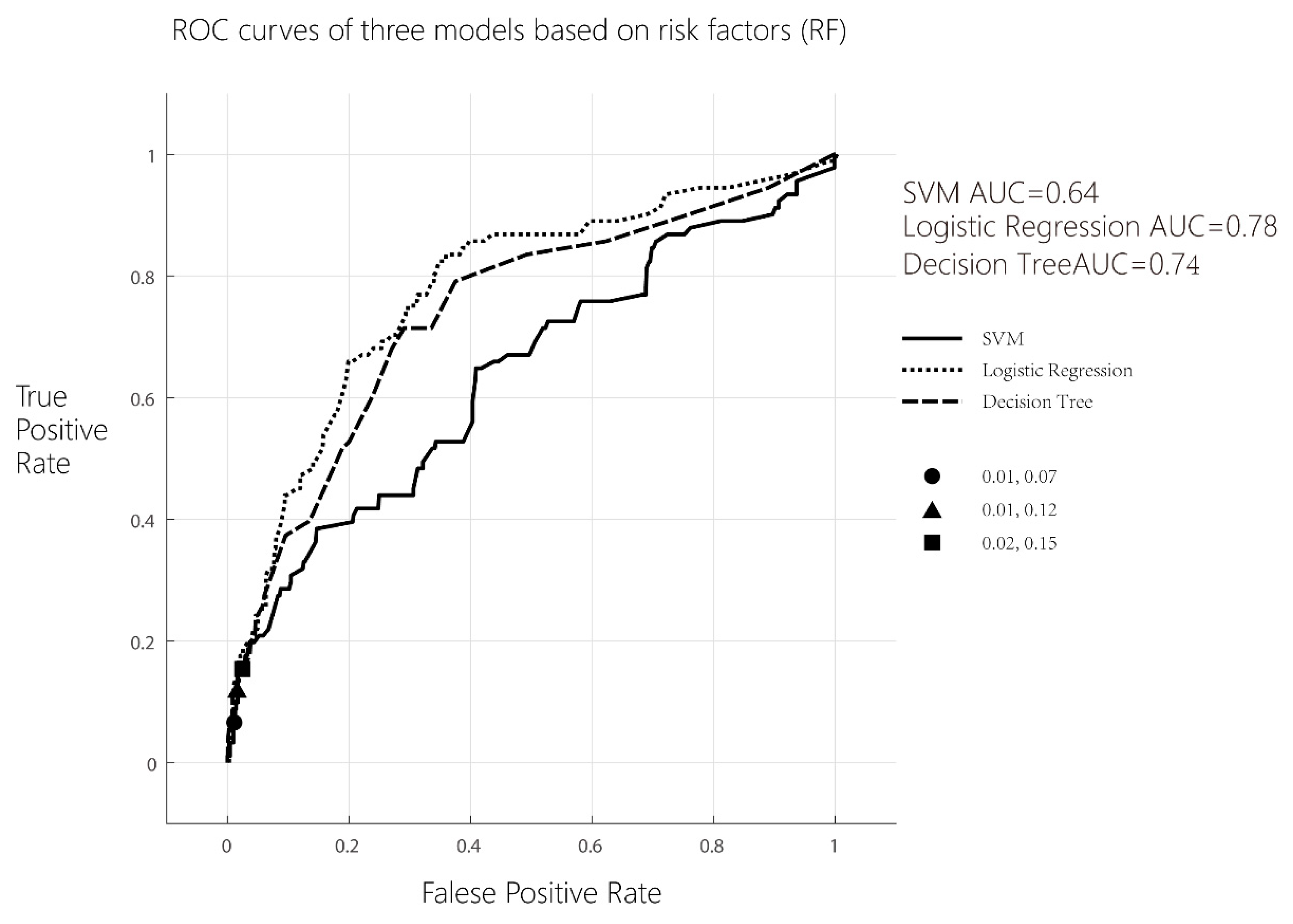
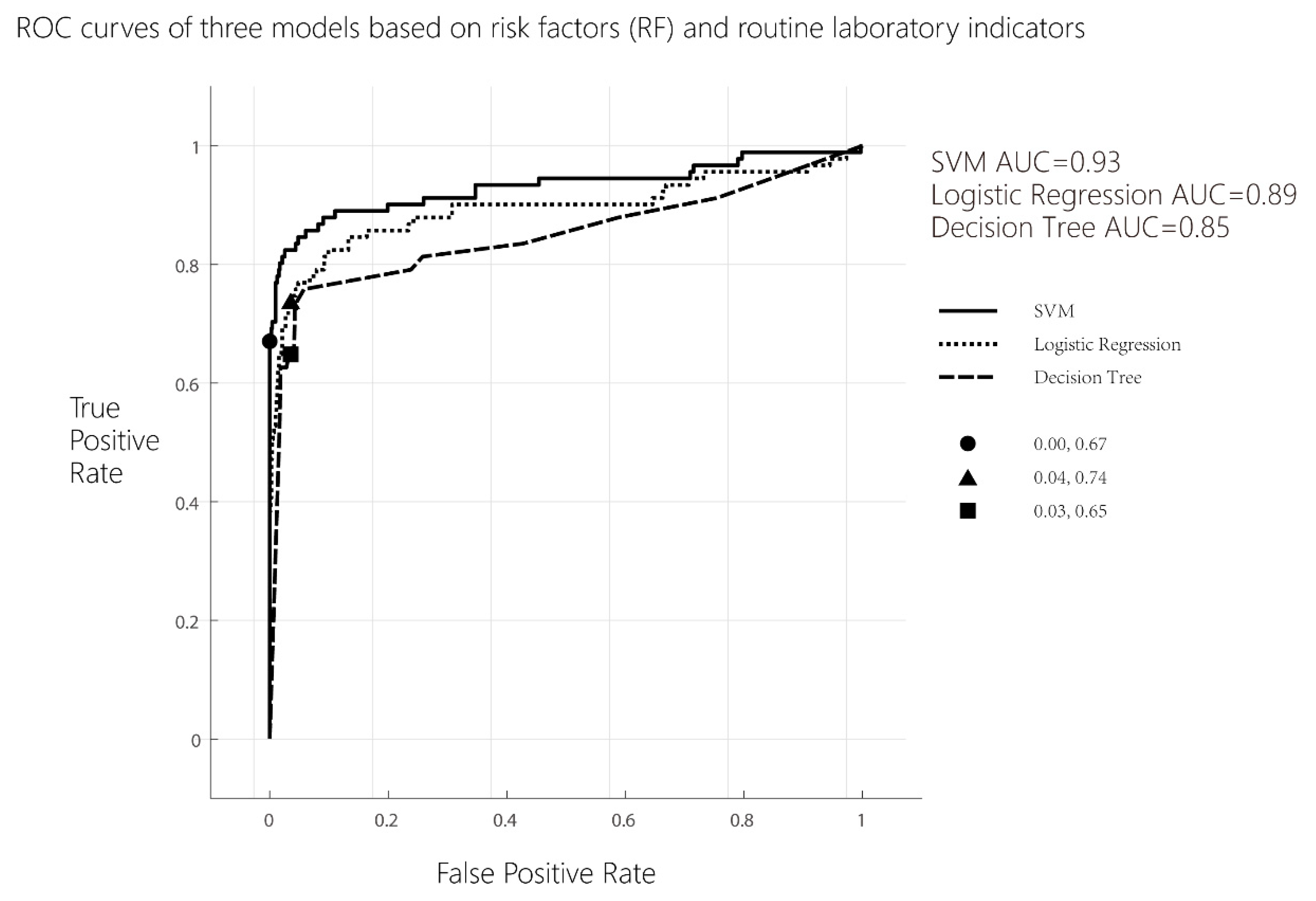
3.4. Results of Each Model and Receiver Operating Curve (ROC) Analysis
- Logistic regression analysis
- b.
- Decision tree model analysis
- c.
- Support vector machine (SVM) analysis
- d.
- Delong test of ROCs differ between models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Khan, K.S.; Wojdyla, D.; Say, L.; Gülmezoglu, A.M.; Van Look, P.F. WHO analysis of causes of maternal death: A systematic review. Lancet 2006, 367, 1066–1074. [Google Scholar] [CrossRef]
- Duley, L. The Global Impact of Pre-eclampsia and Eclampsia. Semin. Perinatol. 2009, 33, 130–137. [Google Scholar] [CrossRef]
- Habli, M.; Eftekhari, N.; Wiebracht, E.; Bombrys, A.; Khabbaz, M.; How, H.; Sibai, B. Long-term maternal and subsequent pregnancy outcomes 5 years after hemolysis, elevated liver enzymes, and low platelets (HELLP) syndrome. Am. J. Obs. Gynecol. 2009, 201, 381–385. [Google Scholar] [CrossRef]
- Nelson, D.B.; Ziadie, M.S.; McIntire, D.D.; Rogers, B.B.; Leveno, K.J. Placental pathology suggesting that preeclampsia is more than one disease. Am. J. Obs. Gynecol. 2014, 210, 61–66. [Google Scholar] [CrossRef]
- De Kat, A.C.; Hirst, J.; Woodward, M.; Kennedy, S.; Peters, S.A. Prediction models for preeclampsia: A systematic review. Pregnancy Hypertens. 2019, 16, 48–66. [Google Scholar] [CrossRef]
- Poon, L.C.; Shennan, A.; Hyett, J.A.; Kapur, A.; Hadar, E.; Divakar, H.; McAuliffe, F.; da Silva Costa, F.; von Dadelszen, P.; McIntyre, H.D.; et al. The International Federation of Gynecology and Obstetrics (FIGO) initiative on pre-eclampsia: A pragmatic guide for first-trimester screening and prevention. Int. J. Gynaecol. Obstet. 2019, 145 (Suppl. S1), 1–33. [Google Scholar] [CrossRef]
- Payne, B.A.; Hutcheon, J.A.; Ansermino, J.M.; Hall, D.R.; Bhutta, Z.A.; Bhutta, S.Z.; Biryabarema, C.; Grobman, W.A.; Groen, H.; Haniff, F.; et al. A risk prediction model for the assessment and triage of women with hypertensive disorders of pregnancy in low-resourced settings: The miniPIERS (Pre-eclampsia Integrated Estimate of RiSk) multi-country prospective cohort study. PLoS Med. 2014, 11, e1001589. [Google Scholar] [CrossRef]
- Thangaratinam, S.; Allotey, J.; Marlin, N.; Mol, B.W.; Von Dadelszen, P.; Ganzevoort, W.; Akkermans, J.; Ahmed, A.; Daniels, J.; Deeks, J.; et al. Development and validation of Prediction models for Risks of complications in Early-onset Pre-eclampsia (PREP): A prospective cohort study. Health Technol. Assess. 2017, 21, 1–100. [Google Scholar] [CrossRef]
- Chappell, L.C.; Duckworth, S.; Seed, P.T.; Griffin, M.; Myers, J.; Mackillop, L.; Simpson, N.; Waugh, J.; Anumba, D.; Kenny, L.C.; et al. Diagnostic accuracy of placental growth factor in women with suspected preeclampsia: A prospective multicenter study. Circulation 2013, 128, 2121–2131. [Google Scholar] [CrossRef]
- Zeisler, H.; Llurba, E.; Chantraine, F.; Vatish, M.; Staff, A.C.; Sennström, M.; Olovsson, M.; Brennecke, S.P.; Stepan, H.; Allegranza, D.; et al. Predictive Value of the sFlt-1:PlGF Ratio in Women with Suspected Preeclampsia. N. Engl. J. Med. 2016, 374, 13–22. [Google Scholar] [CrossRef]
- North, R.A.; McCowan, L.M.; Dekker, G.A.; Poston, L.; Chan, E.H.; Stewart, A.W.; Black, M.A.; Taylor, R.S.; Walker, J.J.; Baker, P.N.; et al. Clinical risk prediction for pre-eclampsia in nulliparous women: Development of model in international prospective cohort. BMJ 2011, 342, d1875. [Google Scholar] [CrossRef]
- Obermeyer, Z.; Emanuel, E.J. Predicting the Future—Big Data, Machine Learning, and Clinical Medicine. N. Engl. J. Med. 2016, 375, 1216–1219. [Google Scholar] [CrossRef]
- Darcy, A.M.; Louie, A.K.; Roberts, L.W. Machine Learning and the Profession of Medicine. JAMA 2016, 315, 551–552. [Google Scholar] [CrossRef]
- Frizzell, J.D.; Liang, L.; Schulte, P.J.; Yancy, C.W.; Heidenreich, P.A.; Hernandez, A.F.; Bhatt, D.L.; Fonarow, G.C.; Laskeyet, W.K. Prediction of 30-Day All-Cause Readmissions in Patients Hospitalized for Heart Failure: Comparison of Machine Learning and Other Statistical Approaches. JAMA Cardiol. 2017, 2, 204–209. [Google Scholar] [CrossRef]
- Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin Summary, Number 222. Obstet. Gynecol. 2020, 135, 1492–1495. [CrossRef]
- Ives, C.W.; Sinkey, R.; Rajapreyar, I.; Tita, A.T.N.; Oparil, S. Preeclampsia—Pathophysiology and Clinical Presentations: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 76, 1690–1702. [Google Scholar] [CrossRef]
- Phipps, E.A.; Thadhani, R.; Benzing, T.; Karumanchi, S.A. Pre-eclampsia: Pathogenesis, novel diagnostics and therapies. Nat. Rev. Nephrol. 2019, 15, 275–289. [Google Scholar] [CrossRef]
- Good clinical practice advice: First trimester screening and prevention of pre-eclampsia in singleton pregnancy. Int. J. Gynaecol. Obstet. 2019, 144, 325–329. [CrossRef]
- ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia. Obs. Gynecol. 2019, 133, 1.
- Hecht, J.L.; Ordi, J.; Carrilho, C.; Ismail, M.R.; Zsengeller, Z.K.; Karumanchi, S.A.; Rosen, S. The pathology of eclampsia: An autopsy series. Hypertens. Pregnancy 2017, 36, 259–268. [Google Scholar] [CrossRef]
- Gaber, L.W.; Spargo, B.H.; Lindheimer, M.D. Renal pathology in pre-eclampsia. Baillieres Clin. Obs. Gynaecol. 1994, 8, 443–468. [Google Scholar] [CrossRef] [PubMed]
- Garovic, V.D.; Wagner, S.J.; Turner, S.T.; Rosenthal, D.W.; Watson, W.J.; Brost, B.C.; Rose, C.H.; Gavrilova, L.; Craigo, P.; Bailey, K.R.; et al. Urinary podocyte excretion as a marker for preeclampsia. Am. J. Obs. Gynecol. 2007, 196, 320–321. [Google Scholar] [CrossRef] [PubMed]
- Dey, M.; Arora, D.; Narayan, N.; Kumar, R. Serum Cholesterol and Ceruloplasmin Levels in Second Trimester can Predict Development of Pre-eclampsia. N. Am. J. Med. Sci. 2013, 5, 41–46. [Google Scholar] [CrossRef] [PubMed]
- van Rijn, B.B.; Veerbeek, J.H.; Scholtens, L.C.; Post, U.E.; Koster, M.P.; Peeters, L.L.; Koenen, S.V.; Bruinse, H.W.; Franx, A. C-reactive protein and fibrinogen levels as determinants of recurrent preeclampsia: A prospective cohort study. J. Hypertens. 2014, 32, 408–414. [Google Scholar] [CrossRef]
- Alma, L.J.; Bokslag, A.; Maas, A.; Franx, A.; Paulus, W.J.; de Groot, C. Shared biomarkers between female diastolic heart failure and pre-eclampsia: A systematic review and meta-analysis. ESC Heart Fail. 2017, 4, 88–98. [Google Scholar] [CrossRef]
- Mary, S.; Kulkarni, M.J.; Malakar, D.; Joshi, S.R.; Mehendale, S.S.; Giri, A.P. Placental Proteomics Provides Insights into Pathophysiology of Pre-Eclampsia and Predicts Possible Markers in Plasma. J. Proteome Res. 2017, 16, 1050–1060. [Google Scholar] [CrossRef]
- Wang, Y.; Shi, D.; Chen, L. Lipid profile and cytokines in hypertension of pregnancy: A comparison of preeclampsia therapies. J. Clin. Hypertens. 2018, 20, 394–399. [Google Scholar] [CrossRef]
- Huang, S.; Cai, N.; Pacheco, P.P.; Narrandes, S.; Wang, Y.; Xu, W. Applications of Support Vector Machine (SVM) Learning in Cancer Genomics. Cancer Genom. Proteom. 2018, 15, 41–51. [Google Scholar]
- Serra, B.; Mendoza, M.; Scazzocchio, E.; Meler, E.; Nolla, M.; Sabrià, E.; Rodríguez, I.; Carreras, E. A new model for screening for early-onset preeclampsia. Am. J. Obs. Gynecol. 2020, 222, 601–608. [Google Scholar] [CrossRef]
- Akolekar, R.; Syngelaki, A.; Poon, L.; Wright, D.; Nicolaides, K.H. Competing Risks Model in Early Screening for Preeclampsia by Biophysical and Biochemical Markers. Fetal Diagn. Ther. 2013, 33, 8–15. [Google Scholar] [CrossRef]
- Jhee, J.H.; Lee, S.; Park, Y.; Lee, S.E.; Kim, Y.A.; Kang, S.-W.; Kwon, J.-Y.; Park, J.T. Prediction model development of late-onset preeclampsia using machine learning-based methods. PLoS ONE 2019, 14, e221202. [Google Scholar] [CrossRef] [PubMed]
| Variables | Control Group (n = 709) | PE Group (n = 91) | Statistical Magnitude | p Value |
|---|---|---|---|---|
| Age, year | 35 (32–38) a | 33 (31–35.5) a | 4.32 b | <0.001 * |
| Body mass index, BMI | 21.71 (19.93–23.81) a | 23.73 (23.12–24.43) a | −4.68 b | <0.001 * |
| Medical history, n (%) | ||||
| Diabetes | 155 (21.86) | 29 (31.87) | 4.56 c | 0.033 * |
| Thrombotic disease | 2 (0.28) | 0 (0.00) | <0.001 c | 0.998 |
| Systemic lupus erythematosus (SLE) | 5 (0.71) | 3 (3.30) | 3.17 c | 0.075 |
| Antiphospholipid syndrome (APS) | 20 (2.82) | 7 (7.69) | 7.31 c | 0.026 * |
| Kidney disease | 5 (0.71) | 6 (6.59) | 16.51 c | <0.001 * |
| Obstructive sleep apnea hypopnea syndrome (OSAHS) | 0 (0.00) | 2 (2.20) | 8.05 c | 0.005 * |
| History of eclampsia or preeclampsia | 4 (0.56) | 6 (6.59) | 19.12 c | <0.001 * |
| History of gestation, n (%) | 591 (83.36) | 51 (56.04) | 46.69 c | <0.001 * |
| Primipara, n (%) | 238 (33.57) | 72 (79.12) | 74.97 c | <0.001 * |
| Fertilization way, n (%) | ||||
| Assisted reproductive technology (ART) | 119 (16.78) | 32 (35.16) | 16.61 c | <0.001 * |
| Natural conception | 590 (83.22) | 59 (64.84) |
| Variable | Control Group (n = 709) | PE Group (n = 91) | Statistical Magnitude | p Value |
|---|---|---|---|---|
| Blood cell count | ||||
| PLT, ×109/L | 244 (211–283) a | 256.5 (226.25–300.5) a | −2.58 b | <0.001 * |
| LYM, ×109/L | 1.79 (1.48–2.1) a | 1.98 (1.74–2.40) a | −3.56 b | <0.001 * |
| NEU, ×109/L | 5.24 (4.28–6.55) a | 6.25 (5.24–8.35) a | −4.63 b | <0.001 * |
| PLT/LYM | 135.19 (114.35–163.73) a | 125.46 (106.26–158.16) a | 1.51 b | 0.13 |
| NEU/LYM | 2.95 (2.29–3.73) a | 2.97 (2.42–4.14) a | −0.97 b | 0.33 |
| Index of coagulation function | ||||
| PT, s | 11.3 (11–11.7) a | 10.9 (10.5–11.3) a | 5.53 b | <0.001 * |
| PTA, % | 91 (88–96) a | 97 (92–102) a | −5.15 b | <0.001 * |
| APTT, s | 31.2 (29.3–33.1) a | 29.6 (27.7–31.3) a | 4.30 b | <0.001 * |
| TT, s | 13.5 (12.9–14) a | 13.4 (12.7–14) a | 1.06 b | 0.29 |
| FIB, g/L | 3.27 (2.92–3.66) a | 3.51 (3.1–3.98) a | −3.38 b | <0.001 * |
| D-Dimer, mg/L | 0.15 (0.15–0.18) a | 0.15 (0.15–0.17) a | 1.13 b | 0.26 |
| FDP, μg/mL | 2.5 (2.5–2.5) a | 2.5 (2.5–2.5) a | −0.79 b | 0.43 |
| Liver function index | ||||
| ALT, U/L | 13 (10–18) a | 18 (13–27.5) a | −4.67 b | <0.001 * |
| AST, U/L | 16 (14–19) a | 19 (15–25) a | −4.70 b | <0.001 * |
| T-Bil, umol/L | 12 (10–14.8) a | 10 (8.9–12.6) a | 4.71 b | <0.001 * |
| D-Bil, umol/L | 1.3 (1–1.8) a | 1.1 (0.6–1.8) a | 2.27 b | 0.02 * |
| TBA, umol/L | 1.6 (1–2.3) a | 1.4 (1–2.35) a | 0.54 b | 0.59 |
| ALP, U/L | 49 (43–58) a | 53 (44–64) a | −1.92 b | 0.05 |
| TP, g/L | 72.4 (70.1–74.7) a | 72 (70.9–74.9) a | −0.24 b | 0.81 |
| ALB, g/L | 43.01 ± 2.42 c | 43.04 ± 3.00 c | −0.08 d | 0.94 |
| GGT, U/L | 14 (11–18) c | 17 (14–28) c | −4.86 b | <0.001 * |
| GLB, g/L | 29 (27–31) c | 30 (28–32) c | −1.12 b | 0.26 |
| Renal function index | ||||
| UREA, mmol/L | 3.1 (2.7–3.7) a | 3.2 (2.8–3.7) a | −1.09 b | 0.28 |
| Cr, umol/L | 59 (54–63) a | 60 (54–65) a | −0.87 b | 0.39 |
| Ca, mmol/L | 2.3 (2.24–2.35) a | 2.33 (2.27–2.4) a | −3.40 b | <0.001 * |
| P, mmol/L | 1.232 ± 0.136 c | 1.228 ± 0.138 c | 0.21 d | 0.83 |
| UA, umol/L | 210 (184–239) a | 238 (214–279.75) a | −5.57 b | <0.001 * |
| Cystatin C, mg/L | 0.62 (0.57–0.68) a | 0.59 (0.54–0.66) a | 1.18 b | 0.24 |
| Blood lipid indicators | ||||
| TCHO, mmol/L | 4.01 (3.56–4.48) a | 4.27 (3.87–4.79) a | −3.09 b | <0.001 * |
| TG, mmol/L | 1.06 (0.8–1.43) a | 1.39 (1.15–1.83) a | −5.00 b | <0.001 * |
| HDL-C, mmol/L | 1.43 (1.24–1.63) a | 1.33 (1.14–1.58) a | 1.40 b | 0.16 |
| LDL-C, mmol/L | 2.16 (1.79–2.53) a | 2.38 (2.11–2.93) a | −3.84 b | <0.001 * |
| ApoA1, g/L | 1578 (1355–1893) a | 1508 (1293–2057) a | 0.10 b | 0.92 |
| ApoB, g/L | 621 (519–738) a | 702 (520–828) a | −2.35 b | 0.02 * |
| Lp(a), mg/L | 87 (44–188) a | 87 (42–188.5) a | 0.29 b | 0.77 |
| sdLDL-C, mmol/L | 0.7 (0.56–0.87) a | 0.93 (0.77–1.00) a | −3.33 b | <0.001 * |
| Complement/inflammatory markers | ||||
| CRP, mg/dL | 1.04 (0.5–2.6) a | 1.71 (0.895–3.68) a | −2.68 b | 0.007 * |
| C1q, mg/L | 184 (166–211) a | 194 (171.75–224.75) a | −2.11 b | 0.03 * |
| SVM~Decision Tree | |
| Difference between areas | 0.08 |
| Standard Error a | 0.044 |
| 95% Confidence Interval | 0.047 to 0.220 |
| z statistic | 3.02 |
| Significance level | p = 0.0025 |
| Logistic Regression~Decision Tree | |
| Difference between areas | 0.04 |
| Standard Error a | 0.025 |
| 95% Confidence Interval | −0.009 to 0.088 |
| z statistic | 1.57 |
| Significance level | p = 0.1162 |
| Logistic Regression~SVM | |
| Difference between areas | 0.12 |
| Standard Error a | 0.034 |
| 95% Confidence Interval | 0.106 to 0.238 |
| z statistic | 5.08 |
| Significance level | p < 0.0001 |
| SVM~Decision Tree | |
| Difference between areas | 0.07 |
| Standard Error a | 0.027 |
| 95% Confidence Interval | 0.026 to 0.132 |
| z statistic | 2.92 |
| Significance level | p = 0.0035 |
| Logistic Regression~Decision Tree | |
| Difference between areas | 0.09 |
| Standard Error a | 0.033 |
| 95% Confidence Interval | −0.050 to 0.077 |
| z statistic | 0.41 |
| Significance level | p = 0.6837 |
| Logistic Regression~SVM | |
| Difference between areas | 0.07 |
| Standard Error a | 0.023 |
| 95% Confidence Interval | 0.020 to 0.112 |
| z statistic | 2.82 |
| Significance level | p = 0.0049 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xue, Y.; Yang, N.; Gu, X.; Wang, Y.; Zhang, H.; Jia, K. Risk Prediction Model of Early-Onset Preeclampsia Based on Risk Factors and Routine Laboratory Indicators. Life 2023, 13, 1648. https://doi.org/10.3390/life13081648
Xue Y, Yang N, Gu X, Wang Y, Zhang H, Jia K. Risk Prediction Model of Early-Onset Preeclampsia Based on Risk Factors and Routine Laboratory Indicators. Life. 2023; 13(8):1648. https://doi.org/10.3390/life13081648
Chicago/Turabian StyleXue, Yuting, Nan Yang, Xunke Gu, Yongqing Wang, Hua Zhang, and Keke Jia. 2023. "Risk Prediction Model of Early-Onset Preeclampsia Based on Risk Factors and Routine Laboratory Indicators" Life 13, no. 8: 1648. https://doi.org/10.3390/life13081648
APA StyleXue, Y., Yang, N., Gu, X., Wang, Y., Zhang, H., & Jia, K. (2023). Risk Prediction Model of Early-Onset Preeclampsia Based on Risk Factors and Routine Laboratory Indicators. Life, 13(8), 1648. https://doi.org/10.3390/life13081648







