Inverted ILM Flap for a Needle Injury to the Macula after Peribulbar Anaesthesia: A Case Report and Literature Review
Abstract
1. Introduction
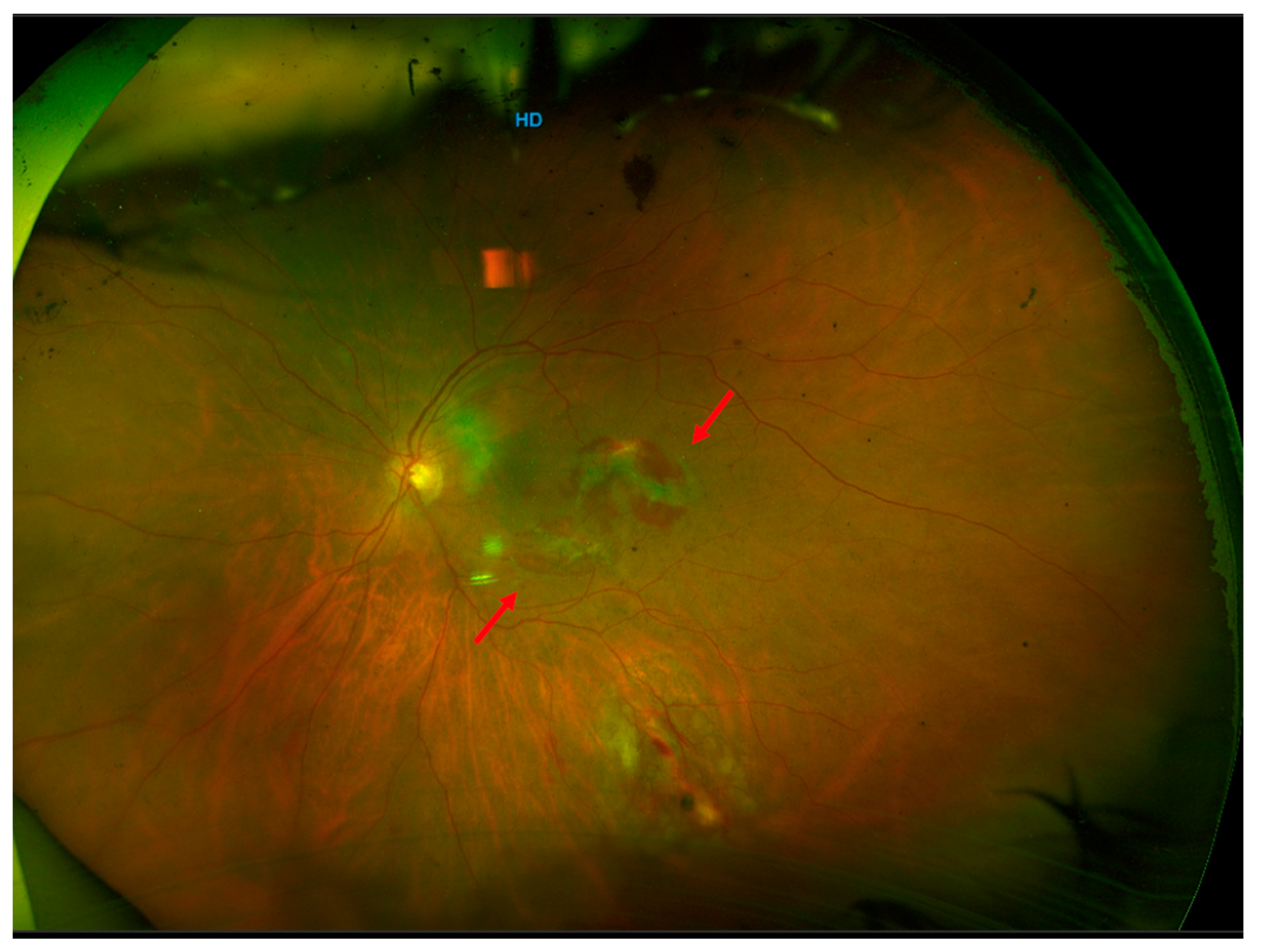
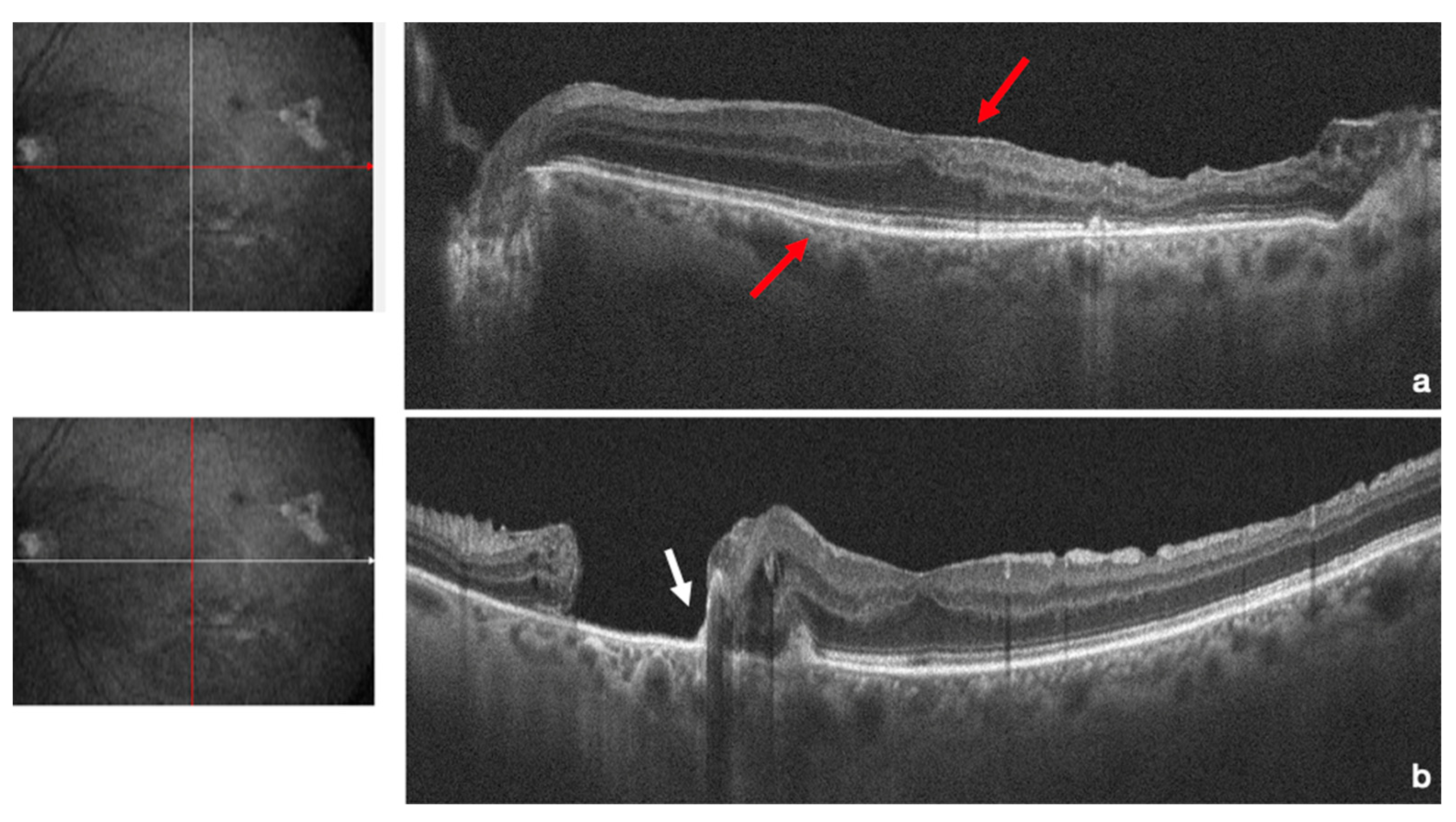
2. Case Report
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Davis, D.B., 2nd; Mandel, M.R. Posterior peribulbar anesthesia: An alternative to retrobulbar anesthesia. J. Cataract. Refract. Surg. 1986, 12, 182–184. [Google Scholar] [CrossRef]
- Lim, J.L.S.; Tsai, A.S.H. A review of retinal complications after globe penetration from peribulbar anesthesia. J. Clin. Ophthalmol. 2021, 5, 414–416. [Google Scholar]
- Schepens, C.L. A comparison of peribulbar and retrobulbar anesthesia for vitreoretinal surgical procedures. Arch. Ophthalmol. 1996, 114, 502. [Google Scholar] [CrossRef] [PubMed]
- Edge, R.; Navon, S. Scleral perforation during retrobulbar and peribulbar anesthesia: Risk factors and outcome in 50,000 consecutive injections. J. Cataract. Refract. Surg. 1999, 25, 1237–1244. [Google Scholar] [CrossRef] [PubMed]
- Duker, J.S.; Belmont, J.B.; Benson, W.E.; Brooks, H.L., Jr.; Brown, G.C.; Federman, J.L.; Fischer, D.H.; Tasman, W.S. Inadvertent globe perforation during retrobulbar and peribulbar anesthesia. Patient characteristics, surgical management, and visual outcome. Ophthalmology 1991, 98, 519–526. [Google Scholar] [CrossRef]
- Grizzard, W.S.; Kirk, N.M.; Pavan, P.R.; Antworth, M.V.; Hammer, M.E.; Roseman, R.L. Perforating ocular injuries caused by anesthesia personnel. Ophthalmology 1991, 98, 1011–1016. [Google Scholar] [CrossRef] [PubMed]
- Mimouni, M.; Abualhasan, H.; Mtanes, K.; Mazzawi, F.; Barak, Y. Patients’ Experience of Anxiety and Pain during Retrobulbar Injections prior to Vitrectomy. J. Ophthalmol. 2019, 2019, 8098765. [Google Scholar] [CrossRef] [PubMed]
- Babu, N.; Kumar, J.; Kohli, P.; Ahuja, A.; Shah, P.; Ramasamy, K. Clinical Presentation and Management of Eyes with Globe Perforation during Peribulbar and Retrobulbar Anesthesia: A Retrospective Case Series. Korean J. Ophthalmol. 2022, 36, 16–25. [Google Scholar] [CrossRef]
- Gomez-Benlloch, A.; Olivera, M.; Nadal, J.; Julio, G.; Elizalde, J. Globe penetration during loco-regional anesthesia: Prevalence and review of cases. Int. J. Ophthalmol. 2022, 15, 1683–1690. [Google Scholar] [CrossRef]
- Ripart, J.; Lefrant, J.Y.; de La Coussaye, J.E.; Prat-Pradal, D.; Vivien, B.; Eledjam, J.J. Peribulbar versus retrobulbar anesthesia for ophthalmic surgery: An anatomical comparison of extraconal and intraconal injections. Anesthesiology 2001, 94, 56–62. [Google Scholar] [CrossRef]
- Schrader, W.F.; Schargus, M.; Schneider, E.; Josifova, T. Risks and sequelae of scleral perforation during peribulbar or retrobulbar anesthesia. J. Cataract. Refract. Surg. 2010, 36, 885–889. [Google Scholar] [CrossRef]
- Foad, A.Z.; Mansour, M.A.; Ahmed, M.B.; Elgamal, H.R.; Ibrahim, H.E.E.; Elawamy, A. Real-time ultrasound-guided retrobulbar block vs blind technique for cataract surgery (pilot study). Local Reg. Anesth. 2018, 11, 123–128. [Google Scholar] [CrossRef]
- Hay, A.; Flynn, H.W., Jr.; Hoffman, J.I.; Rivera, A.H. Needle penetration of the globe during retrobulbar and peribulbar injections. Ophthalmology 1991, 98, 1017–1024. [Google Scholar] [CrossRef]
- Kumar, C.M. Needle-based blocks for the 21st century ophthalmology. Acta Ophthalmol. 2011, 89, 5–9. [Google Scholar] [CrossRef]
- Riad, W.; Ahmed, N. Single injection peribulbar anesthesia with a short needle combined with digital compression. Anesth. Analg. 2008, 107, 1751–1753. [Google Scholar] [CrossRef]
- Clarke, J.; Seah, H.M.; Foo, A.; Agzarian, M.; Lake, S. Computed tomography scan measurements of the globe and orbit to assess the risks of traumatic complications from medial peribulbar anaesthesia. BMC Anesthesiol. 2022, 22, 133. [Google Scholar] [CrossRef]
- Ball, J.L.; Woon, W.H.; Smith, S. Globe perforation by the second peribulbar injection. Eye 2002, 16, 663–665. [Google Scholar] [CrossRef] [PubMed]
- Liang, C.; Peyman, G.A.; Sun, G. Toxicity of intraocular lidocaine and bupivacaine. Am. J. Ophthalmol. 1998, 125, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Nishide, T.; Kadonosono, K.; Itoh, N.; Yazama, F.; Endoh, Y.; Sawada, H.; Ohno, S. The effect of intraocular lidocaine in white rabbit eyes. Nippon. Ganka Gakkai Zasshi 2000, 104, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Olmez, G.; Soker Cakmak, S.; Ipek Soker, S.; Nergiz, Y.; Yildiz, F. Effects of intravitreal ropivacaine on retinal thickness and integrity in the guinea pig. Curr. Ther. Res. Clin. Exp. 2005, 66, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Leme, F.C.O.; Moro, E.T.; Ferraz, A.A.F. Amaurosis and contralateral cranial nerve pairs III and VI paralysis after peribulbar block—Case report. Braz. J. Anesthesiol. 2018, 68, 299–302. [Google Scholar] [CrossRef]
- Alrajhi, R.K.; Almalki, A.M.; Alqahtani, A.S. Optic Nerve Injury, Vitreous Hemorrhage, and Rhegmatogenous Retinal Detachment Following Long Needle Peribulbar Anesthesia: A Case Report and Review of the Literature. Cureus 2022, 14, e31329. [Google Scholar] [CrossRef] [PubMed]
- Gopal, L.; Badrinath, S.S.; Parikh, S.; Chawla, G. Retinal detachment secondary to ocular perforation during retrobulbar anaesthesia. Indian J. Ophthalmol. 1995, 43, 13–15. [Google Scholar] [PubMed]
- Hochman, M.A.; Seery, C.M.; Zarbin, M.A. Pathophysiology and management of subretinal hemorrhage. Surv. Ophthalmol. 1997, 42, 195–213. [Google Scholar] [CrossRef] [PubMed]
- Wearne, M.J.; Flaxel, C.J.; Gray, P.; Sullivan, P.M.; Cooling, R.J. Vitreoretinal surgery after inadvertent globe penetration during local ocular anesthesia. Ophthalmology 1998, 105, 371–376. [Google Scholar] [CrossRef]
- Dubey, D.; Shanmugam, M.; Ramanjulu, R.; Mishra, K.C.D.; Doshi, B. Swept source optical coherence tomography in globe perforation. Indian J. Ophthalmol. 2019, 67, 1697–1698. [Google Scholar] [CrossRef]
- Dikci, S.; Yilmaz, T.; Gok, Z.E.; Demirel, S.; Genc, O. Choroidal neovascularization secondary to ocular penetration during retrobulbar anesthesia and its treatment. Oman J. Ophthalmol. 2017, 10, 44–46. [Google Scholar] [CrossRef]
- Al-Shehri, A.; Al-Ghamdi, A.; Al-Shehri, A.; Alakeely, A. Management of iatrogenic globe perforation during peribulbar anesthesia with submacular hemorrhage. Oman J. Ophthalmol. 2020, 13, 95–97. [Google Scholar] [CrossRef]
- Bloch, E.; Malik, M.; Bhardwaj, G.; Scott, A. Scleral perforation involving the papillomacular bundle secondary to peribulbar anaesthetic injection. Am. J. Ophthalmol. Case Rep. 2020, 18, 100657. [Google Scholar] [CrossRef]
- Shukla, D. Management of macular epiretinal membrane secondary to accidental globe perforation during retrobulbar anesthesia. Indian. J. Ophthalmol. 2013, 61, 234–235. [Google Scholar] [CrossRef]
- Naik, A.A.; Agrawal, S.A.; Navadiya, I.D.; Ramchandani, S.J. Management of macular epiretinal membrane secondary to accidental globe perforation during retrobulbar anesthesia. Indian. J. Ophthalmol. 2014, 62, 94–95. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scampoli, A.; Governatori, L.; Bernardinelli, P.; Picardi, S.M.; Culiersi, C.; Caporossi, T. Inverted ILM Flap for a Needle Injury to the Macula after Peribulbar Anaesthesia: A Case Report and Literature Review. Life 2023, 13, 1390. https://doi.org/10.3390/life13061390
Scampoli A, Governatori L, Bernardinelli P, Picardi SM, Culiersi C, Caporossi T. Inverted ILM Flap for a Needle Injury to the Macula after Peribulbar Anaesthesia: A Case Report and Literature Review. Life. 2023; 13(6):1390. https://doi.org/10.3390/life13061390
Chicago/Turabian StyleScampoli, Alessandra, Lorenzo Governatori, Patrizio Bernardinelli, Stefano Maria Picardi, Carola Culiersi, and Tomaso Caporossi. 2023. "Inverted ILM Flap for a Needle Injury to the Macula after Peribulbar Anaesthesia: A Case Report and Literature Review" Life 13, no. 6: 1390. https://doi.org/10.3390/life13061390
APA StyleScampoli, A., Governatori, L., Bernardinelli, P., Picardi, S. M., Culiersi, C., & Caporossi, T. (2023). Inverted ILM Flap for a Needle Injury to the Macula after Peribulbar Anaesthesia: A Case Report and Literature Review. Life, 13(6), 1390. https://doi.org/10.3390/life13061390





