Bacterial Contamination of Healthcare Students’ Mobile Phones: Impact of Specific Absorption Rate (SAR), Users’ Demographics and Device Characteristics on Bacterial Load
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Questionnaire Administration
2.3. Microbiological Analysis
2.4. Statistical Analysis
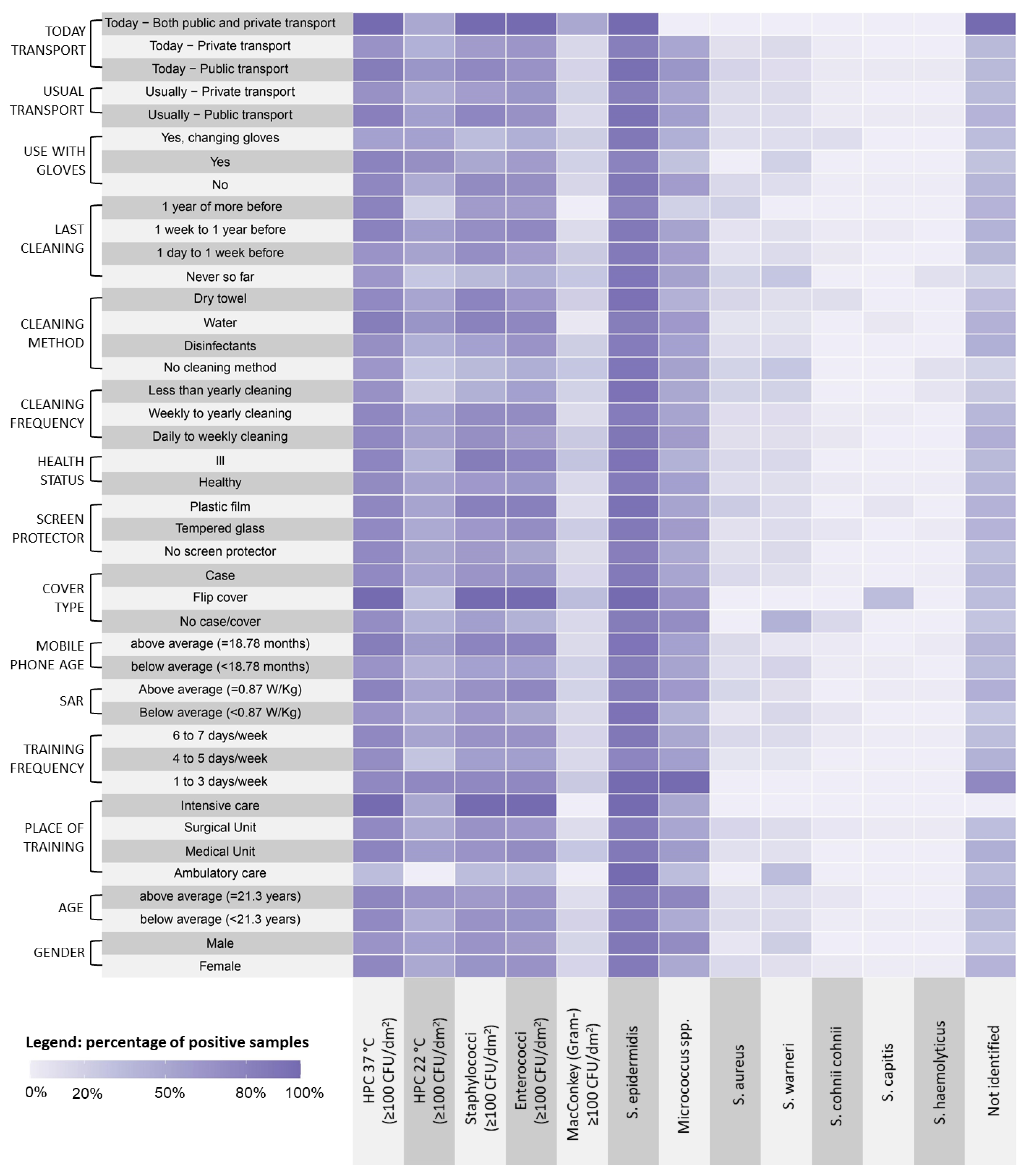
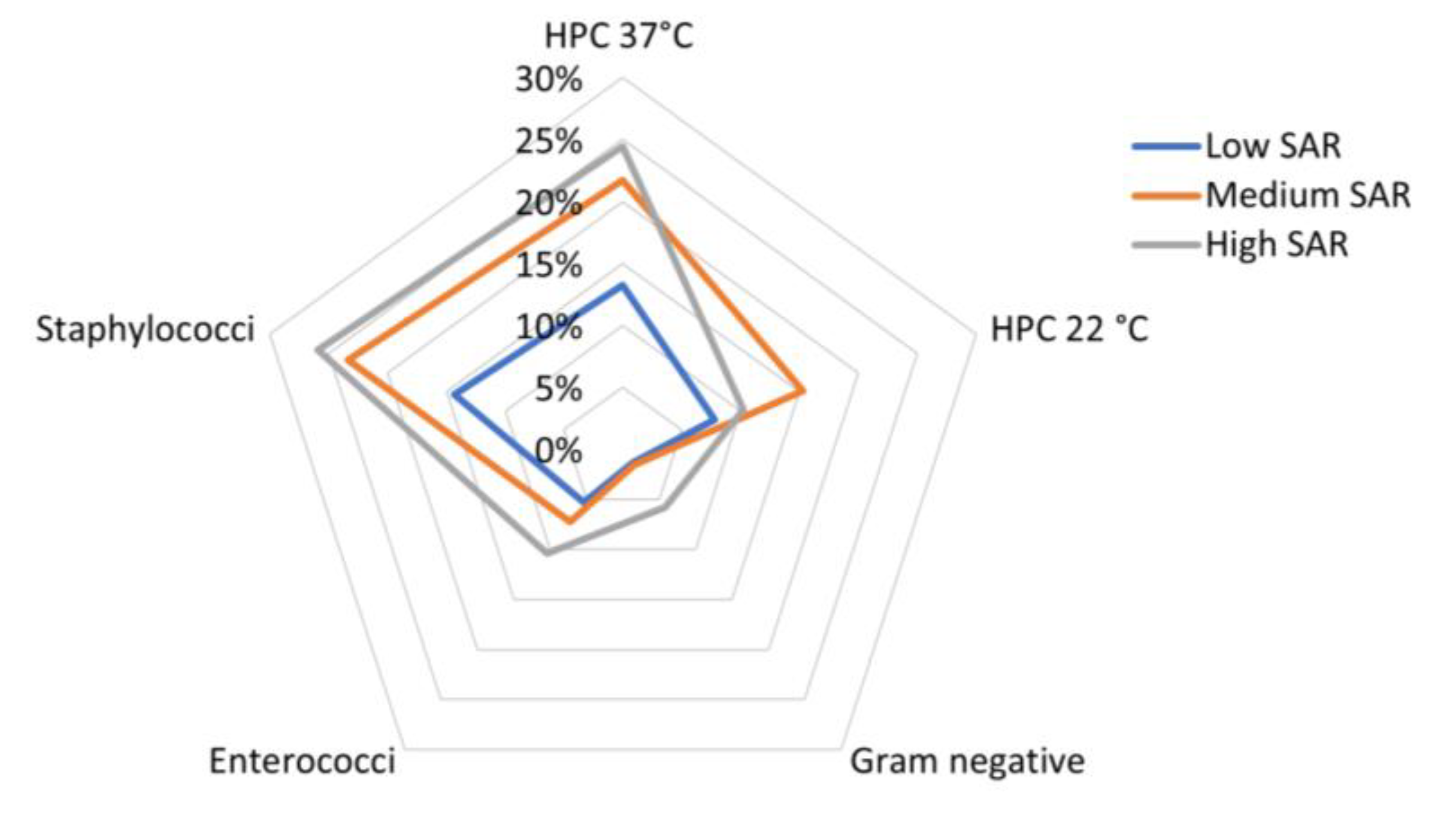
3. Results
3.1. Study Population
3.2. Microbiological Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dubljanin, E.; Crvenkov, T.; Vujčić, I.; Grujičić, S.S.; Dubljanin, J.; Džamić, A. Fungal contamination of medical students’ mobile phones from the University of Belgrade, Serbia: A cross-sectional study. Sci. Rep. 2022, 12, 16852. [Google Scholar] [CrossRef]
- Olsen, M.; Lohning, A.; Campos, M.; Jones, P.; McKirdy, S.; Alghafri, R.; Tajouri, L. Mobile phones of paediatric hospital staff are never cleaned and commonly used in toilets with implications for healthcare nosocomial diseases. Sci. Rep. 2021, 11, 12999. [Google Scholar] [CrossRef]
- Akinyemi, K.O.; Atapu, A.D.; Adetona, O.O.; Coker, A.O. The potential role of mobile phones in the spread of bacterial infections. J. Infect. Dev. Ctries 2009, 3, 628–632. [Google Scholar] [CrossRef]
- Kayed, K.; Khoder, G.; Farhat, J.; Ghemarawi, R. Mobile Phones: Reservoirs of Resistant Bacteria during the COVID-19 Pandemic in Abu Dhabi, United Arab Emirates. Microorganisms 2023, 11, 523. [Google Scholar] [CrossRef] [PubMed]
- Goldblatt, J.G.; Krief, I.; Klonsky, T.; Haller, D.; Milloul, V.; Sixsmith, D.M.; Srugo, I.; Potasman, I. Use of cellular telephones and transmission of pathogens by medical staff in New York and Israel. Infect. Control. Hosp. Epidemiol. 2007, 28, 500–503. [Google Scholar] [CrossRef] [PubMed]
- D’Alò, G.L.; Cicciarella Modica, D.; Maurici, M.; Mozzetti, C.; Messina, A.; Distefano, A.; De Filippis, P.; Pica, F. Microbial contamination of the surface of mobile phones and implications for the containment of the COVID-19 pandemic. Travel Med. Infect. Dis. 2020, 37, 101870. [Google Scholar] [CrossRef]
- Kuriyama, A.; Fujii, H.; Hotta, A.; Asanuma, R.; Irie, H. Prevalence of bacterial contamination of touchscreens and posterior surfaces of smartphones owned by healthcare workers: A cross-sectional study. BMC Infect. Dis. 2021, 21, 681. [Google Scholar] [CrossRef] [PubMed]
- Lubwama, M.; Kateete, D.P.; Ayazika, K.T.; Nalwanga, W.; Kagambo, D.B.; Nsubuga, M.D.; Arach, A.K.; Ssetaba, L.J.; Wamala, J.N.; Rwot, L.A.; et al. Microbiological Contamination of Mobile Phones and Mobile Phone Hygiene of Final-Year Medical Students in Uganda: A Need for Educational Intervention. Adv. Med. Educ. Pract. 2021, 12, 1247–1257. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.H.; Chen, S.Y.; Lu, J.J.; Chang, C.J.; Chang, Y.; Hsieh, P.H. Nasal colonization and bacterial contamination of mobile phones carried by medical staff in the operating room. PLoS ONE 2017, 12, 0175811. [Google Scholar] [CrossRef]
- Cantais, A.; Grattard, F.; Gagnaire, J.; Mory, O.; Plat, A.; Lleres-Vadeboin, M.; Berthelot, P.; Bourlet, T.; Botelho-Nevers, E.; Pozzetto, B.; et al. Longitudinal Study of Viral and Bacterial Contamination of Hospital Pediatricians’ Mobile Phones. Microorganisms 2020, 8, 2011. [Google Scholar] [CrossRef]
- Asfaw, T.; Genetu, D. High Rate of Bacterial Contamination on Healthcare Worker’s Mobile Phone and Potential Role in Dissemination of Healthcare-Associated Infection at Debre Berhan Referral Hospital, North Shoa Zone, Ethiopia. Risk Manag. Healthc. Policy. 2021, 14, 2601–2608. [Google Scholar] [CrossRef] [PubMed]
- Beckstrom, A.C.; Cleman, P.E.; Cassis-Ghavami, F.L.; Kamitsuka, M.D. Surveillance study of bacterial contamination of the parent’s cell phone in the NICU and the effectiveness of an anti-microbial gel in reducing transmission to the hands. J. Perinatal. 2013, 33, 960–963. [Google Scholar] [CrossRef] [PubMed]
- Yao, N.; Yang, X.F.; Zhu, B.; Liao, C.Y.; He, Y.M.; Du, J.; Liu, N.; Zhou, C.B. Bacterial Colonization on Healthcare Workers’ Mobile Phones and Hands in Municipal Hospitals of Chongqing, China: Cross-contamination and Associated Factors. J. Epidemiol. Glob. Health. 2022, 12, 390–399. [Google Scholar] [CrossRef] [PubMed]
- Ontario Agency for Health Protection and Promotion (Public Health Ontario); Provincial Infectious Diseases Advisory Committee. Best Practices for Environmental Cleaning for Prevention and Control of Infections in All Health Care Settings, 3rd ed.; Queen’s Printer for Ontario: Toronto, ON, Canada, 2018.
- Qadi, M.; Khayyat, R.; AlHajhamad, M.A.; Naji, Y.I.; Maraqa, B.; Abuzaitoun, K.; Mousa, A.; Daqqa, M. Microbes on the Mobile Phones of Healthcare Workers in Palestine: Identification, Characterization, and Comparison. Can. J. Infect. Dis. Med. Microbiol. 2021, 2021, 8845879. [Google Scholar] [CrossRef]
- Suleyman, G.; Alangaden, G.; Bardossy, A.C. The Role of Environmental Contamination in the Transmission of Nosocomial Pathogens and Healthcare-Associated Infections. Curr. Infect. Dis. Rep. 2018, 20, 12. [Google Scholar] [CrossRef]
- Hesseling, M.; Haag, R.; Sicks, B. Review of microbial touchscreen contamination for the determination of reasonable ultraviolet disinfection doses. GMS Hyg. Infect. Control 2021, 16, 8662742. [Google Scholar]
- De Groote, P.; Blot, K.; Conoscenti, E.; Labeau, S.; Blot, S. Mobile phones as a vector for Healthcare-Associated Infection: A systematic review. Intensive Crit. Care Nurs. 2022, 72, 103266. [Google Scholar] [CrossRef]
- Cicciarella Modica, D.; Maurici, M.; D’Alò, G.L.; Mozzetti, C.; Messina, A.; Distefano, A.; Pica, F.; De Filippis, P. Taking Screenshots of the Invisible: A Study on Bacterial Contamination of Mobile Phones from University Students of Healthcare Professions in Rome, Italy. Microorganisms 2020, 8, 1075. [Google Scholar] [CrossRef]
- Bhardwaj, N.; Khatri, M.; Bhardwaj, S.K.; Sonne, C.; Deep, A.; Kim, K.H. A review on mobile phones as bacterial reservoirs in healthcare environments and potential device decontamination approaches. Environ. Res. 2020, 186, 109569. [Google Scholar] [CrossRef] [PubMed]
- Maurici, M.; D’Alò, G.L.; Fontana, C.; Santoro, V.; Gaziano, R.; Ciotti, M.; Cicciarella Modica, D.; De Filippis, P.; Sarmati, L.; De Carolis, G.; et al. Microbiology and Clinical Outcome of Hospital-Acquired Respiratory Infections in an Italian Teaching Hospital: A Retrospective Study. Healthcare 2022, 10, 2271. [Google Scholar] [CrossRef]
- Toney-Butlet, T.J.; Gasner, A.; Carver, N. Hand Hygiene; StatPearls Publishing: Tampa, FL, USA, 2022. [Google Scholar]
- Koroglu, M.; Gunal, S.; Yildiz, F.; Savas, M.; Ozer, A.; Altindis, M. Comparison of keypads and touch-screen mobile phones/devices as potential risk for microbial contamination. J. Infect. Dev. Ctries 2015, 9, 1308–1314. [Google Scholar] [CrossRef] [PubMed]
- Bodena, D.; Teklemariam, Z.; Balakrishnan, S.; Tesfa, T. Bacterial contamination of mobile phones of health professionals in Eastern Ethiopia: Antimicrobial susceptibility and associated factors. Trop. Med. Health. 2019, 47, 15. [Google Scholar] [CrossRef]
- Ya’aba, Y.; Chuku, A.; Okposhi, U.S.; Hadi, N.S.; Ramalan, S.A. Bacterial Contamination Associated with Mobile Cell Phones among Undergraduate Students of Federal University of Lafia, Nasarawa State, Nigeria. Nig. J. Basic Appl. Sci. 2020, 28, 36–42. [Google Scholar] [CrossRef]
- Pal, S.; Juyal, D.; Adekhandi, S.; Sharma, M.; Prakash, R.; Sharma, N.; Rana, A.; Parihar, A. Mobile phones: Reservoirs for the transmission of nosocomial pathogens. Adv. Biomed. Res. 2015, 4, 144. [Google Scholar] [PubMed]
- Kang, K.; Ni, Y.; Li, J.; Imamovic, L.; Sarkar, C.; Kobler, M.D.; Heshiki, Y.; Zheng, T.; Kumari, S.; Wong, J.C.Y.; et al. The Environmental Exposures and Inner- and Intercity Traffic Flows of the Metro System May Contribute to the Skin Microbiome and Resistome. Cell. Rep. 2018, 24, 1190–1202. [Google Scholar] [CrossRef]
- Braddy, C.M.; Blair, J.E. Colonization of personal digital assistants used in a health care setting. Am. J. Infect. Control 2005, 33, 230–232. [Google Scholar] [CrossRef]
- Mushabati, N.A.; Samutela, M.T. Bacterial contamination of mobile phones of healthcare workers at the University Teaching Hospital, Lusaka, Zambia. Infect. Prev. Pract. 2021, 3, 100126. [Google Scholar] [CrossRef] [PubMed]
- Di Lodovico, S.; Del Vecchio, A.; Cataldi, V.; Di Campli, E.; Di Bartolomeo, S.; Cellini, L.; Di Giulio, M. Microbial Contamination of Smartphone Touchscreens of Italian University Students. Curr. Microbiol. 2018, 75, 336–342. [Google Scholar] [CrossRef]
- Carlberg, M.; Koppel, T.; Hedendahl, L.K.; Hardell, L. Is the Increasing Incidence of Thyroid Cancer in the Nordic Countries Caused by Use of Mobile Phones? Int. J. Environ. Res. Public Health 2020, 17, 9129. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, O.P.; Morgan, L.L.; de Salles, A.A.; Han, Y.-Y.; Herberman, R.B.; Davis, D.L. Exposure Limits: The underestimation of absorbed cell phone radiation, especially in children. Electromagn. Biol. Med. 2011, 31, 34–51. [Google Scholar] [CrossRef] [PubMed]
- Kshetrimayum, R.S. Mobile phones: Bad for your health? IEEE Potentials 2008, 27, 18–20. [Google Scholar] [CrossRef]
- Szeto, J.; Genetu, D. Increased organic contamination found on mobile phones after touching it while using the toilet. J. Environ. Public. Health 2015. [Google Scholar] [CrossRef]
- Beard, B.B.; Kainz, W.; Onishi, T.; Iyama, T.; Watanabe, S.; Fujiwara, O.; Wang, J.; Bit-Babik, G.; Faraone, A.; Wiart, J.; et al. Comparisons of Computed Mobile Phone Induced SAR in the SAM Phantom to That in Anatomically Correct Models of the Human Head. IEEE Trans. Electromagn. Compat. 2006, 48, 397–407. [Google Scholar] [CrossRef]
- Arya, R.; Antonisamy, B.; Kumar, S. Sample size estimation in prevalence studies. Indian J. Pedriatr. 2012, 79, 1482–1488. [Google Scholar] [CrossRef]
- Castiglia, P.; Liguori, G.; Montagna, M.T.; Napoli, C.; Pasquarella, C.; Bergomi, M.; Fabiani, L.; Monarca, S.; Petti, S.; Siti Working Group Hygiene in Dentistry. Italian multi-center study on infection hazards during dental practice: Control of environmental microbial contamination in public dental surgeries. BMC Public Health 2008, 8, 187. [Google Scholar] [CrossRef]
- Grice, E.A.; Segre, J.A. The skin microbiome. Nat. Rev. Microbiol. 2011, 9, 244–253. [Google Scholar] [CrossRef]
- Walvick, M.D.; Amato, M. Ophthalmic methicillin-resistant Staphylococcus aureus infections: Sensitivity and resistance profiles of 234 isolates. J. Community Health 2011, 36, 1024–1026. [Google Scholar] [CrossRef] [PubMed]
- Becker, K.; Heilmann, C.; Peters, G. Coagulase-negative staphylococci. Clin. Microbiol. Rev. 2014, 27, 870–926. [Google Scholar] [CrossRef]
- Gomes, F.; Teixeira, P.; Oliveira, R. Mini-review: Staphylococcus epidermidis as the most frequent cause of nosocomial infections: Old and new fighting strategies. Biofouling. 2014, 30, 131–141. [Google Scholar] [CrossRef]
- Egert, M.; Späth, K.; Weik, K.; Kunzelmann, H.; Horn, C.; Kohl, M.; Blessing, F. Bacteria on smartphone touchscreens in a German university setting and evaluation of two popular cleaning methods using commercially available cleaning products. Folia Microbiol. 2015, 60, 159–164. [Google Scholar] [CrossRef]
- Dancer, S.J. How do we assess hospital cleaning? A proposal for microbiological standards for surface hygiene in hospitals. J. Hosp. Infect. 2004, 56, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Hughes, K.A.; Cornwall, J.; Theis, J.C.; Brooks, H.J. Bacterial contamination of unused, disposable non-sterile gloves on a hospital orthopaedic ward. Australas Med. J. 2013, 6, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Suarez, C.; Peña, C.; Arch, O.; Dominguez, M.A.; Tubau, F.; Juan, C.; Gavaldá, L.; Sora, M.; Oliver, A.; Pujol, M.; et al. Large sustained endemic outbreak of multiresistant Pseudomonas aeruginosa: A new epidemiological scenario for nosocomial acquisition. BMC Infect. Dis. 2011, 11, 272. [Google Scholar] [CrossRef] [PubMed]
- Kramer, A.; Ebke, I.; Kampf, G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect. Dis. 2006, 6, 130. [Google Scholar] [CrossRef] [PubMed]
- Solano, C.; Echeverz, M.; Lasa, I. Biofilm dispersion and quorum sensing. Curr. Opin. Microbiol. 2014, 18, 96–104. [Google Scholar] [CrossRef]
- Tan, C.H.; Lee, K.W.; Burmølle, M.; Kjelleberg, S.; Rice, S.A. All together now: Experimental multispecies biofilm model systems. Environ. Microbiol. 2017, 19, 42–53. [Google Scholar] [CrossRef]
- Jiang, L.; Ng, I.H.L.; Hou, Y.; Li, D.; Tan, L.W.L.; Ho, H.J.A.; Chen, M.I.C. Infectious disease transmission: Survey of contacts between hospital-based healthcare workers and working adults from the general population. J. Hosp. Infect. 2018, 98, 404–411. [Google Scholar] [CrossRef]
| Variables | Values | n | % |
|---|---|---|---|
| Degree course | Nursing | 59 | 71.1 |
| Obstetrics | 13 | 15.7 | |
| Other | 11 | 13.2 | |
| Gender | Male | 18 | 21.7 |
| Female | 65 | 78.3 | |
| Mean students age (21.29 years) | Below average | 65 | 78.3 |
| Above average | 18 | 21.7 | |
| Type of internship ward * | Ambulatory care | 3 | 3.6 |
| Medical ward | 33 | 39.8 | |
| Surgical ward | 43 | 51.8 | |
| Intensive care | 2 | 2.4 | |
| Weekly internship attendance (in days) * | 1–3 | 4 | 4.8 |
| 4–5 | 14 | 16.9 | |
| 6–7 | 64 | 77.1 | |
| Use of MP during training * | No | 8 | 9.6 |
| Yes | 74 | 89.2 | |
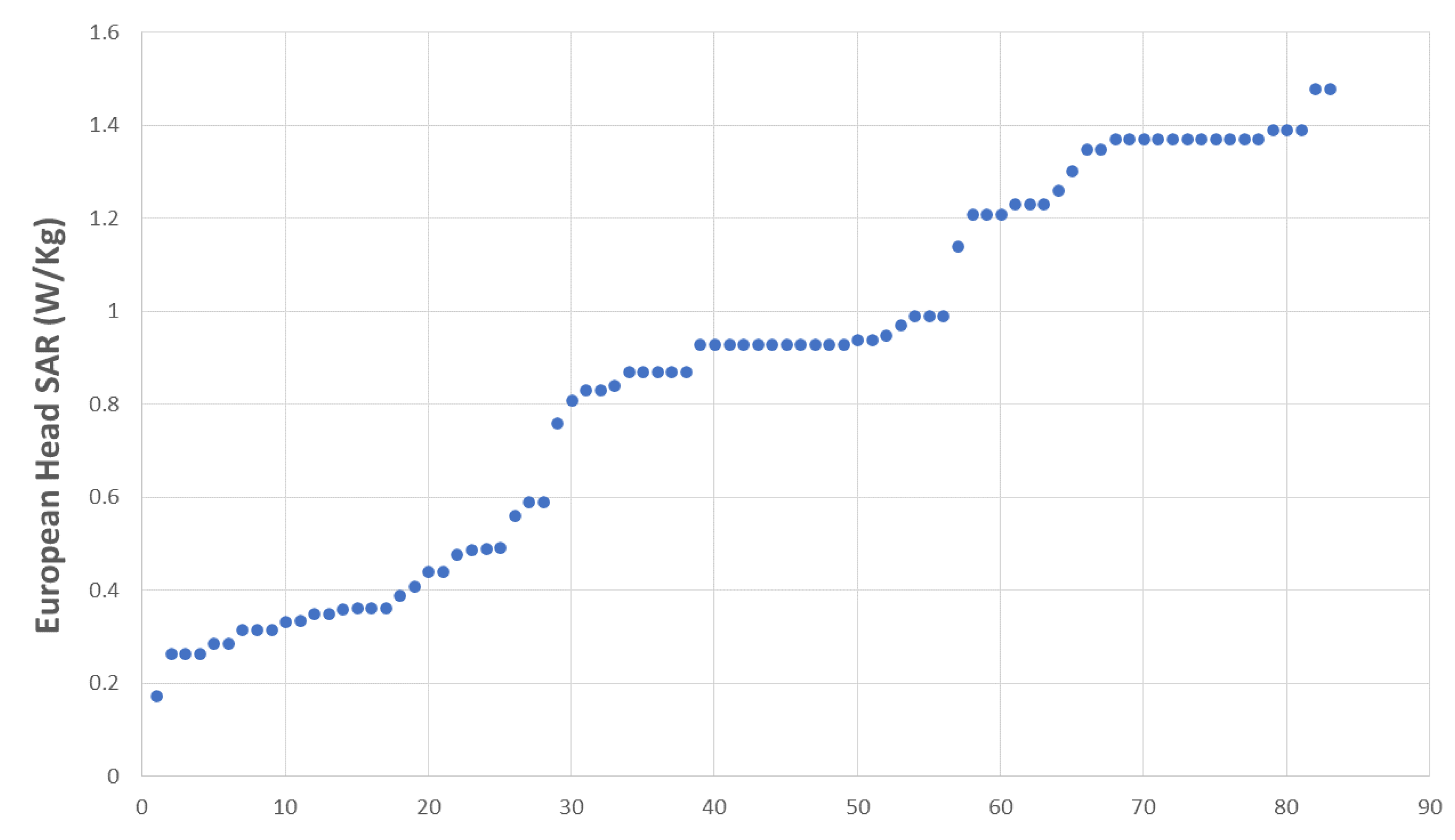
| Mean European head SAR (0.87 W/Kg) | Below average | 33 | 39.8 |
| Above average | 50 | 60.2 | |
| Mean MP age (18.78 months) | Below average | 45 | 54.2 |
| Above average | 38 | 45.8 | |
| Type of MP cover | None | 7 | 8.4 |
| Flip-cover | 3 | 3.6 | |
| Case | 73 | 88 | |
| Type of touchscreen protective film | None | 31 | 37.3 |
| Glass | 35 | 42.2 | |
| Plastic | 17 | 20.5 | |
| Acute illness ongoing * | No | 68 | 81.9 |
| Yes | 14 | 16.9 | |
| Frequency of MP cleaning | Up to 1/week | 20 | 24.1 |
| From 1/8 days to 1/11 months | 47 | 56.6 | |
| 1/year or never | 16 | 19.3 | |
| Method of MP cleaning | None | 11 | 13.3 |
| Disinfectants | 27 | 32.5 | |
| Water/detergents | 26 | 31.3 | |
| Dry towels | 19 | 22.9 | |
| Last cleaning performed * | Never | 11 | 13.3 |
| From 1 day to 7 days ago | 24 | 28.9 | |
| From 8 days to 11 months ago | 41 | 49.4 | |
| 1 year or more ago | 5 | 6 | |
| Use of MP with gloves | No | 64 | 77.1 |
| Yes | 10 | 12 | |
| Yes, but I change gloves soon after | 9 | 10.9 | |
| Usual means of transport | Public | 35 | 42.2 |
| Private | 48 | 57.8 | |
| Means of transport on the day of sampling | Public | 28 | 33.7 |
| Private | 53 | 63.9 | |
| Both | 2 | 2.4 |
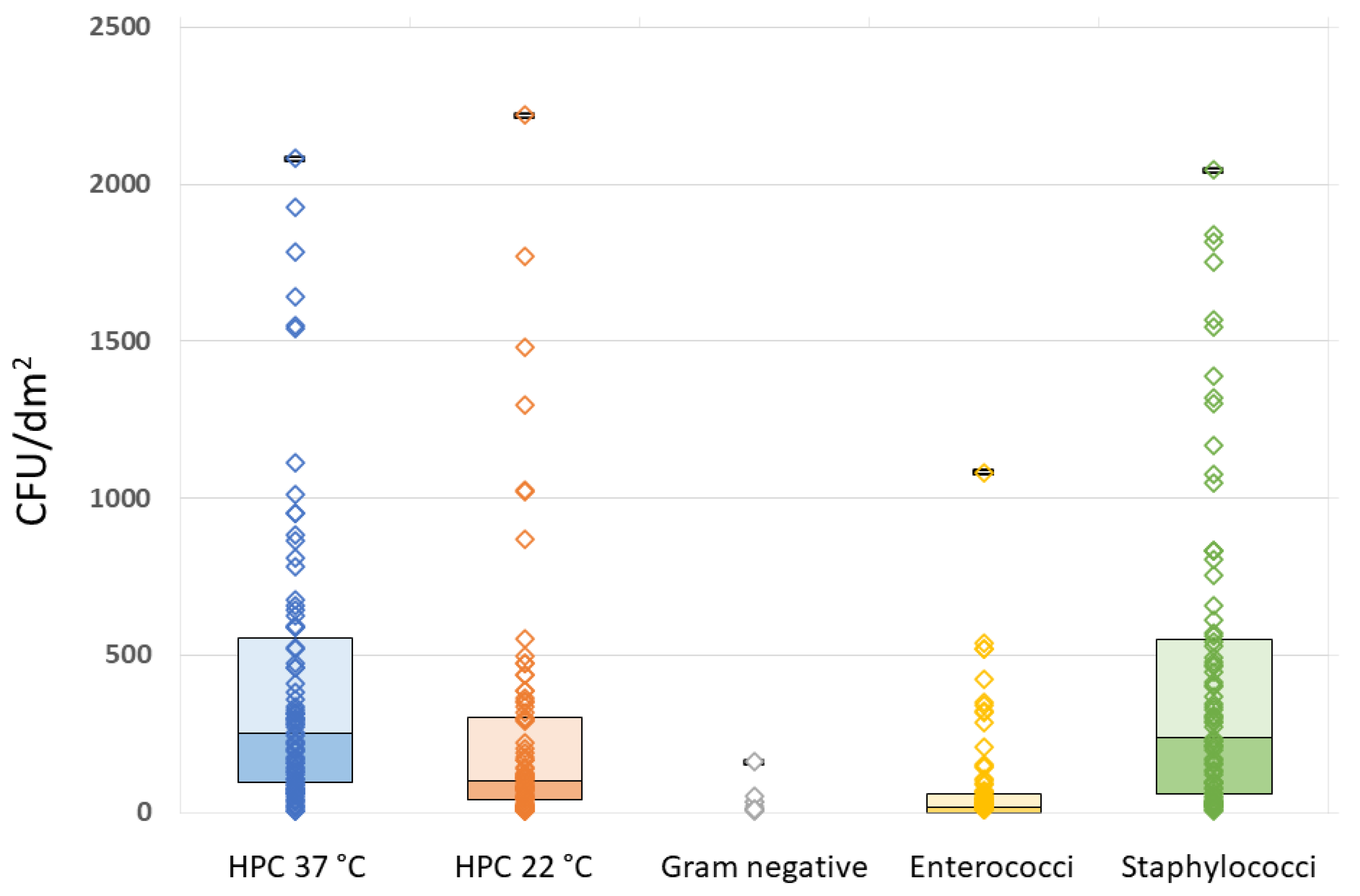
| HPC 37 °C (CFU/dm2) | HPC 22 °C (CFU/dm2) | Gram-neg. CFU/dm2 | Enterococci (CFU/dm2) | Staphylococci (CFU/dm2) | ||
|---|---|---|---|---|---|---|
| N | Detectable | 82 | 81 | 14 | 55 | 81 |
| Not detectable | 1 | 2 | 69 | 28 | 2 | |
| Mean | 416.16 | 253.24 | 27.79 | 124.46 | 442.49 | |
| Median | 263.59 | 105.30 | 10.41 | 43.04 | 272.03 | |
| Std. Deviation | 466.53 | 398.98 | 41.00 | 194.83 | 505.09 | |
| Range | 2076.77 | 2217.01 | 153.90 | 1072.66 | 2035.88 | |
| Minimum | 5.21 | 5.21 | 8.33 | 8.89 | 8.33 | |
| Maximum | 2081.98 | 2222.22 | 162.23 | 1081.55 | 2044.21 | |
| European Head SAR (W/Kg) | HPC 37 °C (CFU/dm2) | HPC 22 °C (CFU/dm2) | Gram-neg. (CFU/dm2) | Enterococci (CFU/dm2) | Staphylococci (CFU/dm2) | MP Age in Months | |
|---|---|---|---|---|---|---|---|
| HPC 37 °C (CFU/dm2) | 0.262 * | 0.840 ** | 0.658 * | 0.633 ** | 0.727 ** | −0.055 | |
| HPC 22 °C (CFU/dm2) | 0.099 | 0.840 ** | 0.733 ** | 0.684 ** | 0.716 ** | −0.065 | |
| Gram-neg. (CFU/dm2) | 0.260 | 0.658 * | 0.733 ** | 0.884 ** | 0.436 | −0.151 | |
| Enterococci (CFU/dm2) | 0.108 | 0.633 ** | 0.684 ** | 0.884 ** | 0.390 ** | −0.129 | |
| Staphylococci (CFU/dm2) | 0.262 * | 0.727 ** | 0.716 ** | 0.436 | 0.390 ** | 0.021 | |
| MP age in months | −0.110 | −0.055 | −0.065 | −0.151 | −0.129 | 0.021 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maurici, M.; Pica, F.; D’Alò, G.L.; Cicciarella Modica, D.; Distefano, A.; Gorjao, M.; Simonelli, M.S.; Serafinelli, L.; De Filippis, P. Bacterial Contamination of Healthcare Students’ Mobile Phones: Impact of Specific Absorption Rate (SAR), Users’ Demographics and Device Characteristics on Bacterial Load. Life 2023, 13, 1349. https://doi.org/10.3390/life13061349
Maurici M, Pica F, D’Alò GL, Cicciarella Modica D, Distefano A, Gorjao M, Simonelli MS, Serafinelli L, De Filippis P. Bacterial Contamination of Healthcare Students’ Mobile Phones: Impact of Specific Absorption Rate (SAR), Users’ Demographics and Device Characteristics on Bacterial Load. Life. 2023; 13(6):1349. https://doi.org/10.3390/life13061349
Chicago/Turabian StyleMaurici, Massimo, Francesca Pica, Gian Loreto D’Alò, Domenico Cicciarella Modica, Alessandra Distefano, Margarida Gorjao, Maria Sofia Simonelli, Livio Serafinelli, and Patrizia De Filippis. 2023. "Bacterial Contamination of Healthcare Students’ Mobile Phones: Impact of Specific Absorption Rate (SAR), Users’ Demographics and Device Characteristics on Bacterial Load" Life 13, no. 6: 1349. https://doi.org/10.3390/life13061349
APA StyleMaurici, M., Pica, F., D’Alò, G. L., Cicciarella Modica, D., Distefano, A., Gorjao, M., Simonelli, M. S., Serafinelli, L., & De Filippis, P. (2023). Bacterial Contamination of Healthcare Students’ Mobile Phones: Impact of Specific Absorption Rate (SAR), Users’ Demographics and Device Characteristics on Bacterial Load. Life, 13(6), 1349. https://doi.org/10.3390/life13061349






