Hess Lancaster Screen Test with Eye Tracker: An Objective Method for the Measurement of Binocular Gaze Direction
Abstract
1. Introduction
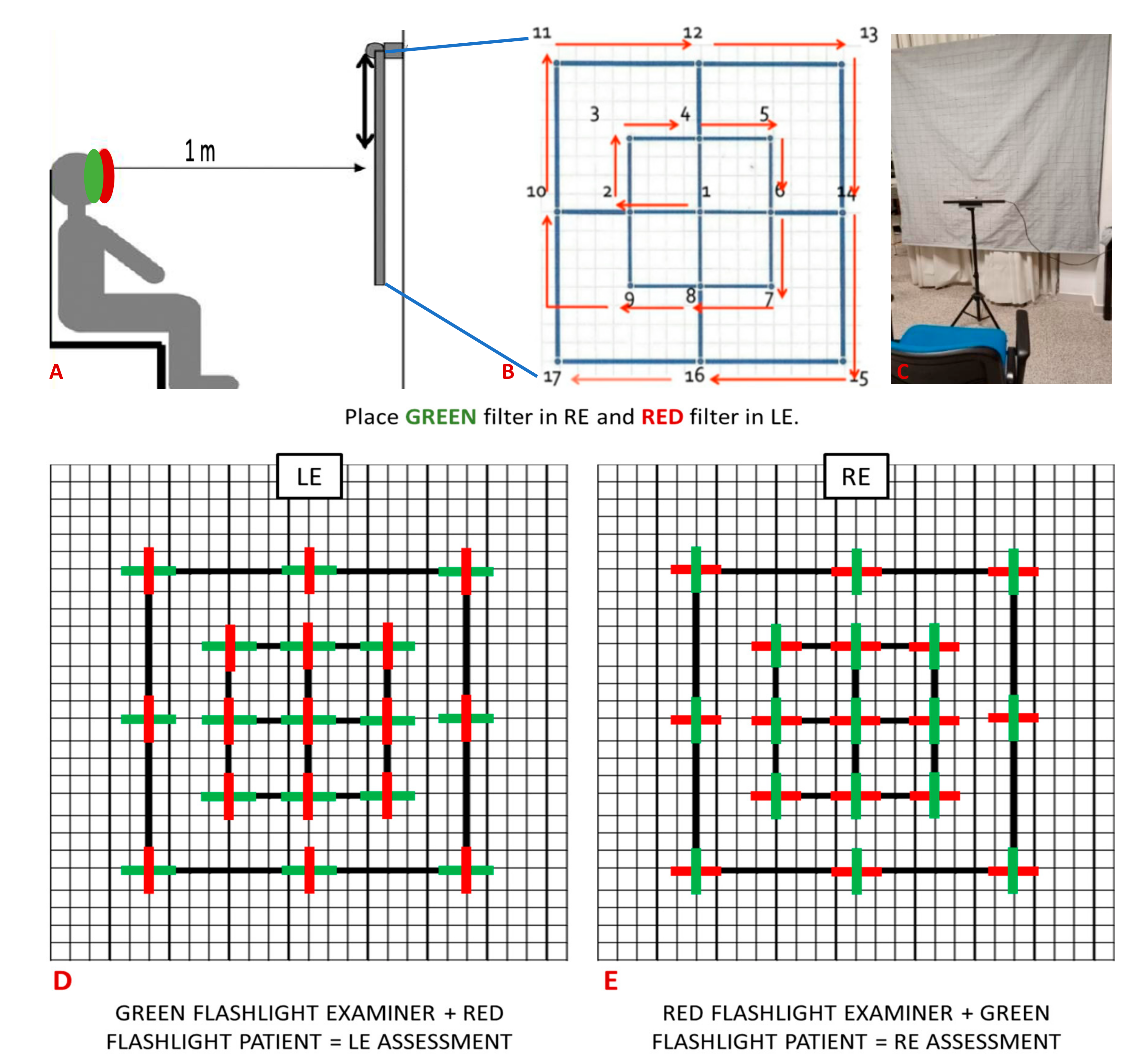
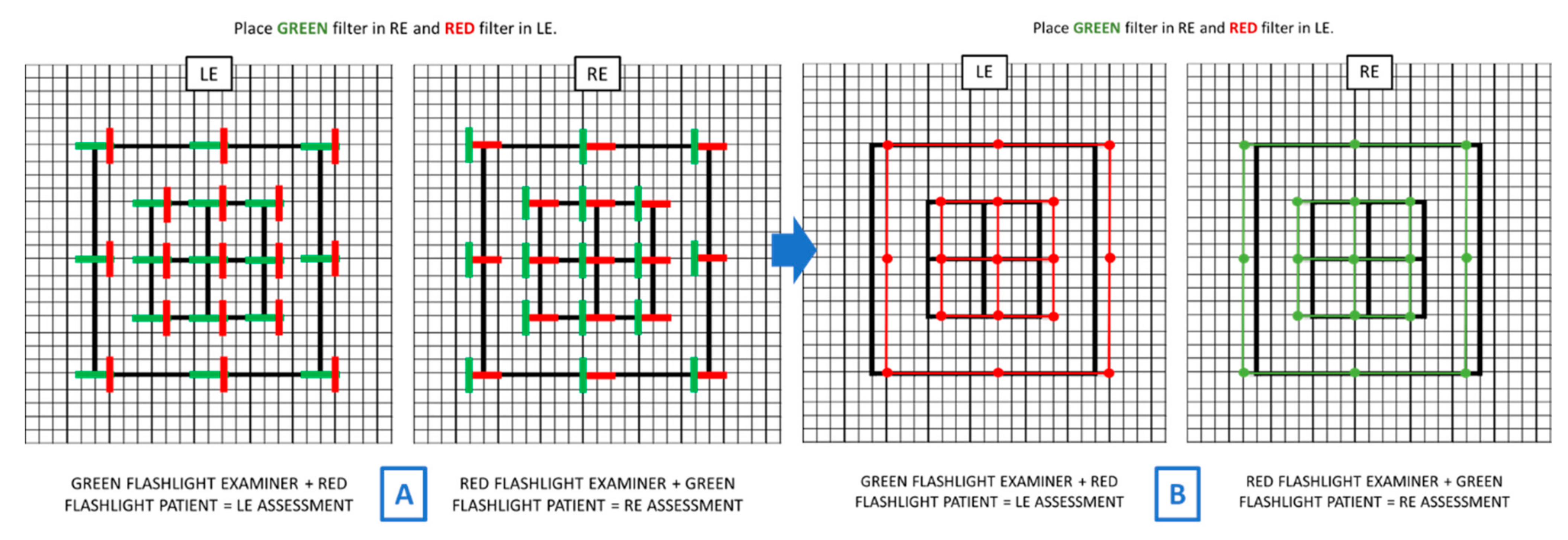
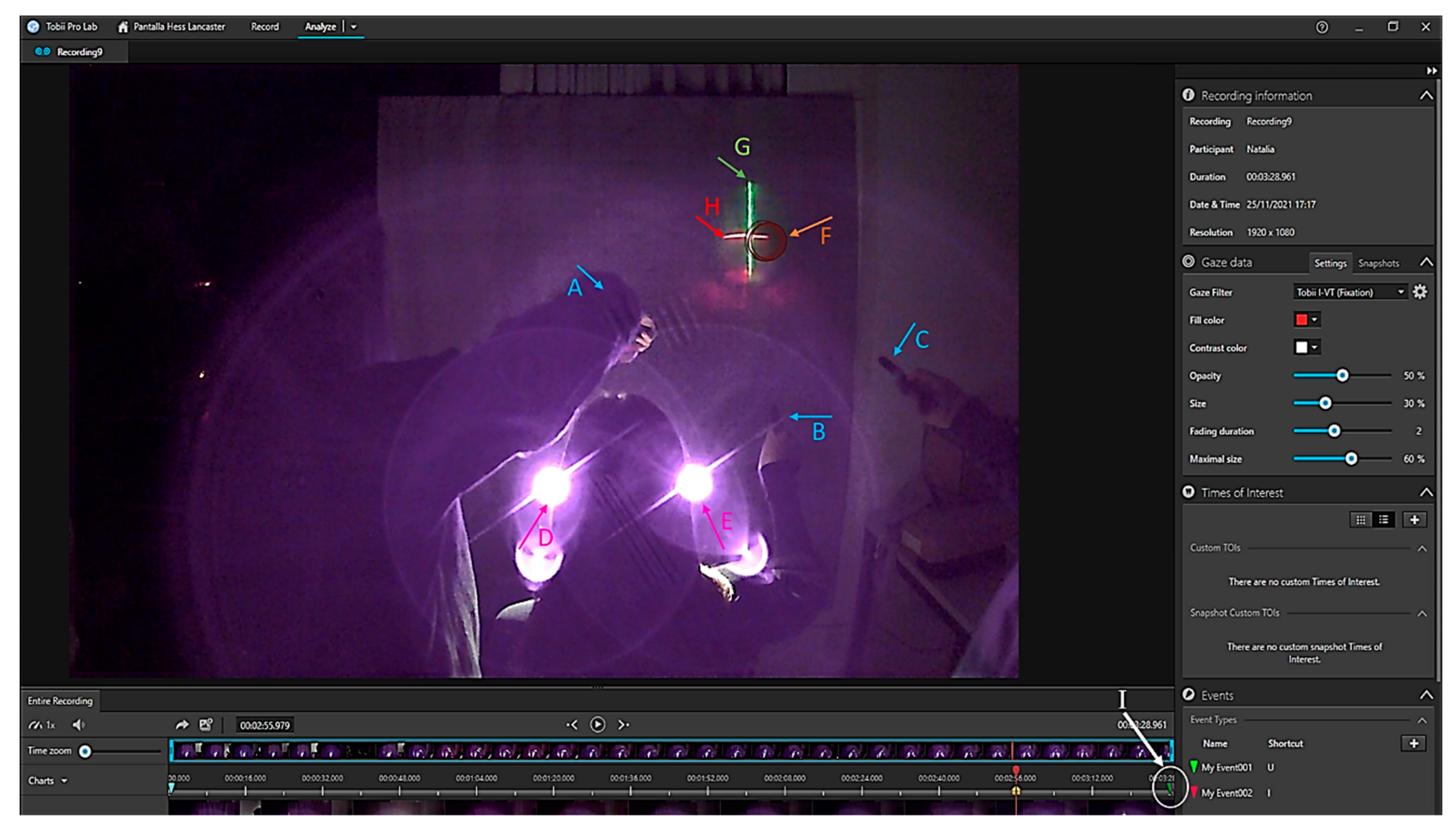
2. Materials and Methods
2.1. Sample Description
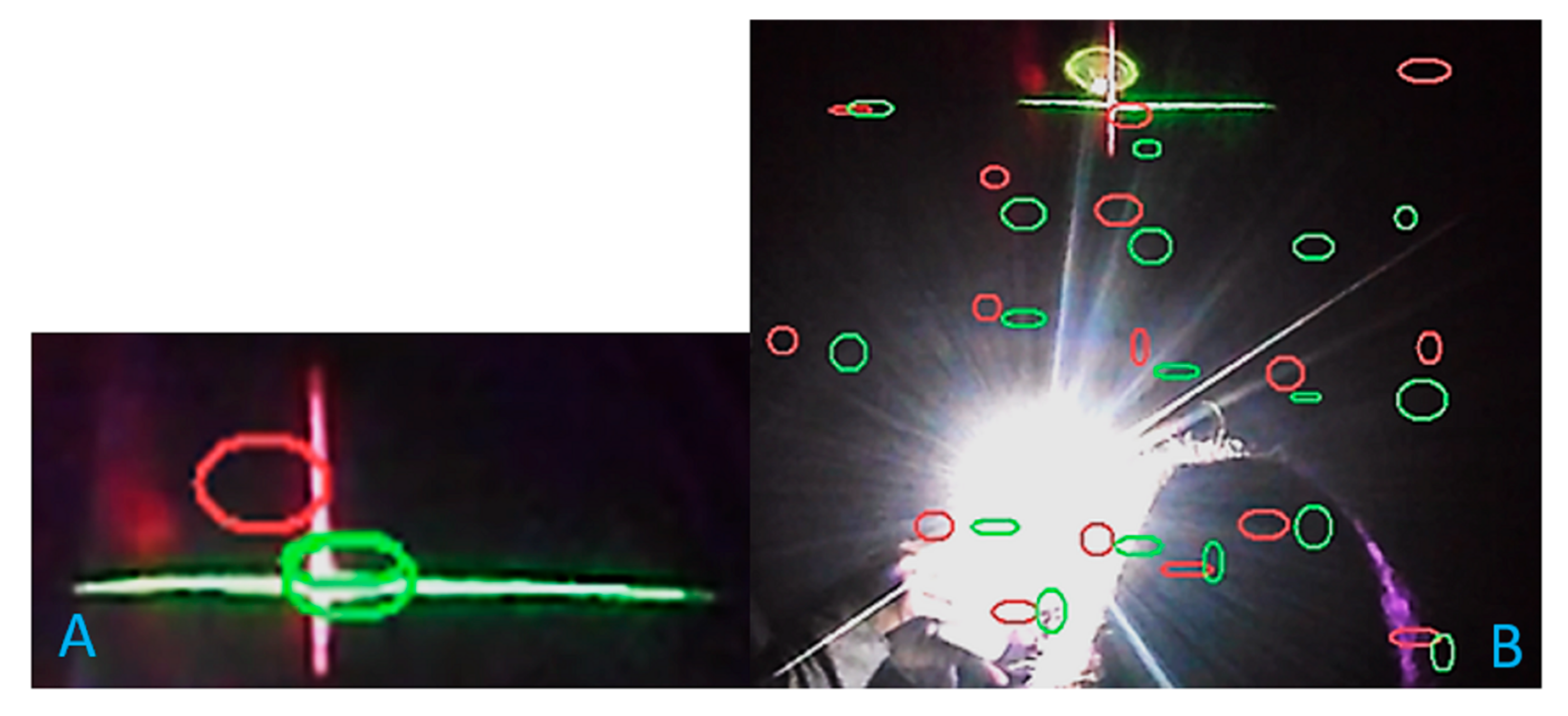
2.2. Experimental Protocol
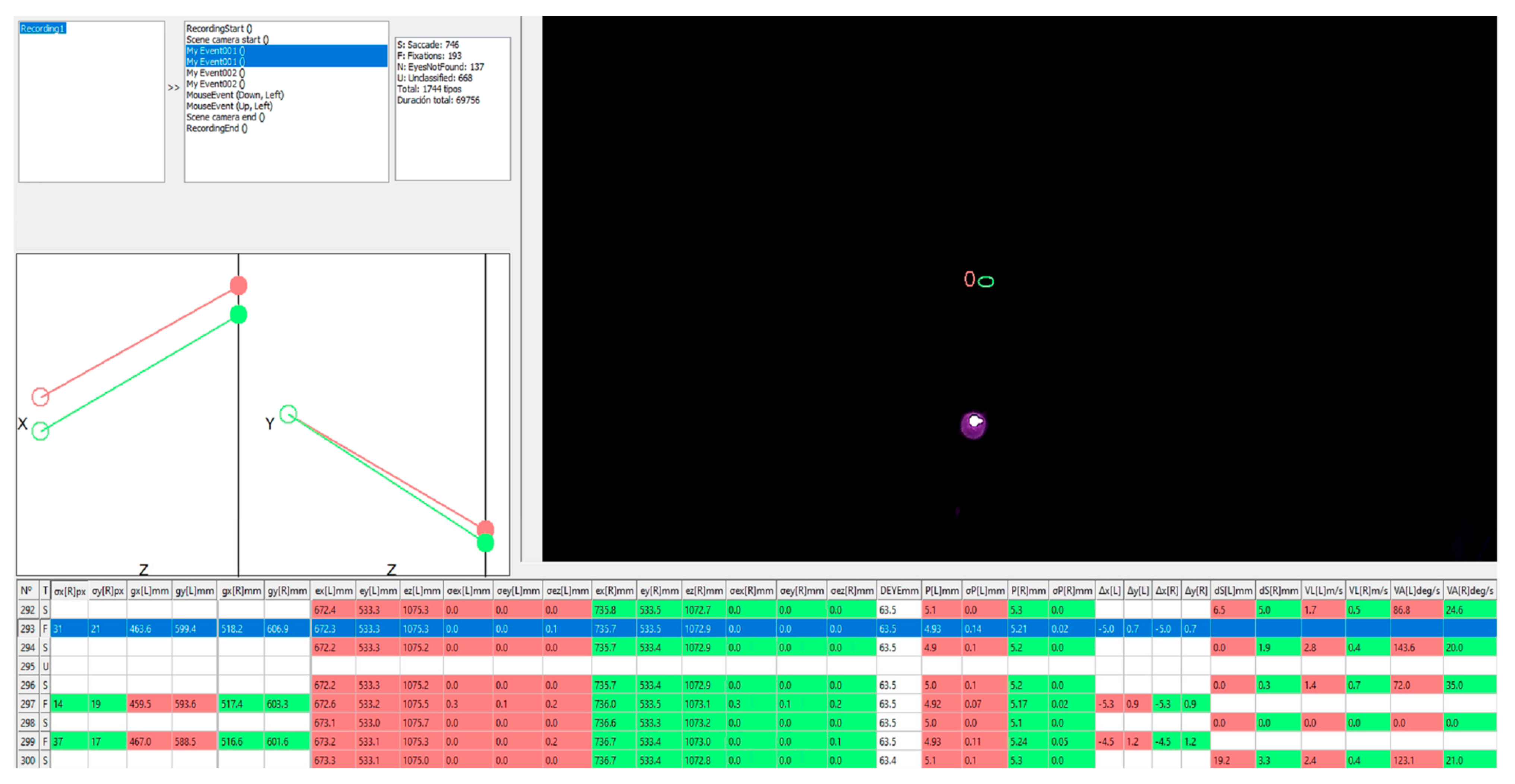
2.3. Data Collection
2.4. Statistical Analysis
3. Results
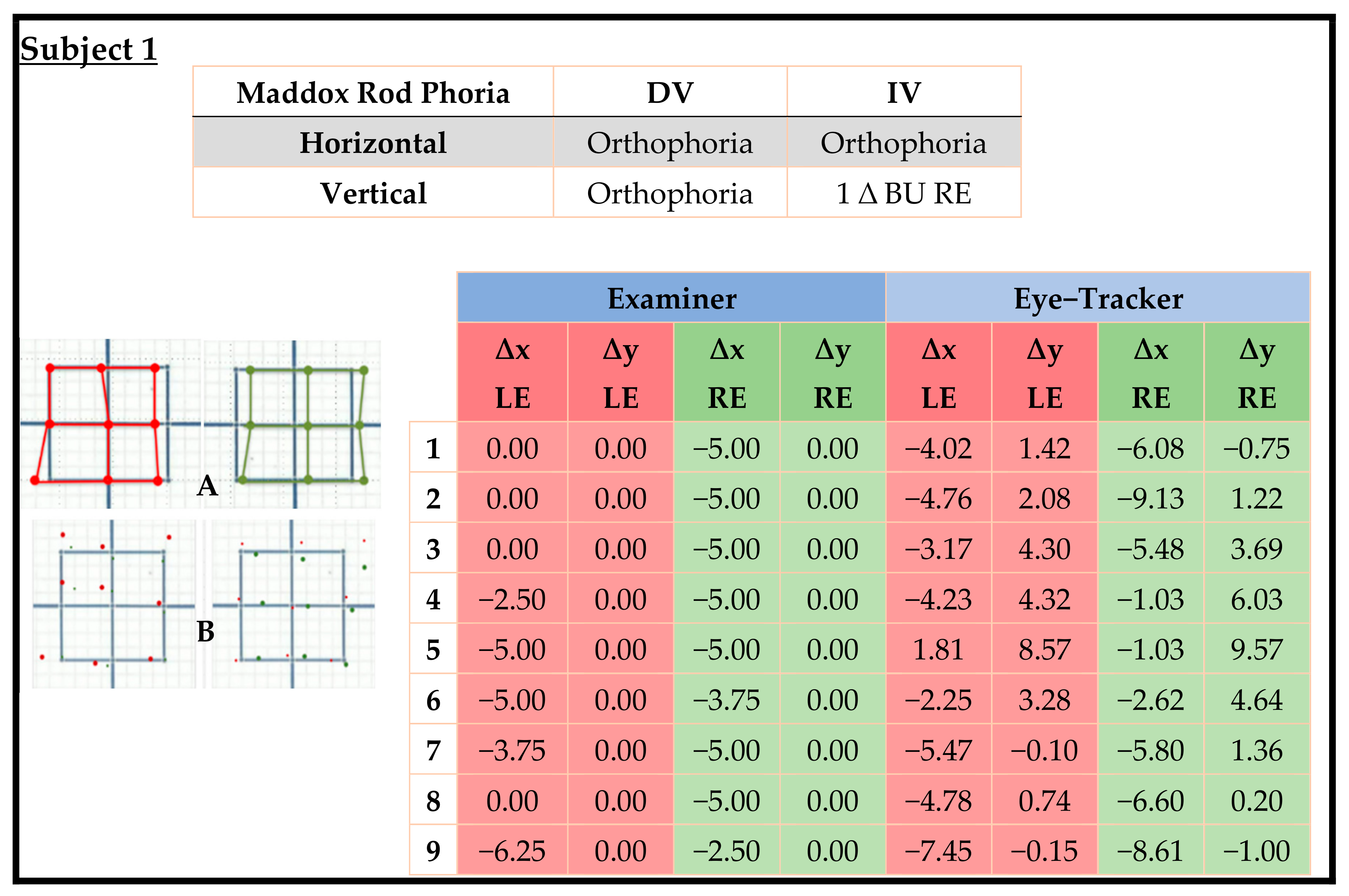
Subjective Method vs. Objective Method Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schreiber, K.; Crawford, J.D.; Fetter, M.; Tweed, D. The motor side of depth vision. Nature 2001, 410, 819–822. [Google Scholar] [CrossRef]
- Grosvenor, T.P. Primary Care Optometry; Elsevier Health Sciences: Amsterdam, The Netherlands, 2007; ISBN 0750675756. [Google Scholar]
- Etezad, R.M.; Sagheb, H.S.; Daneshyar, A. Normative Values for the Fusional Amplitudes and the Prevalence of Heterophoria in Adults; Khatam-Al-Anbia Eye Hospital-2009: Mashhad, Iran, 2010. [Google Scholar]
- Radaković, M.; Ivetić, V.; Naumović, N.; Čanadanović, V.; Stankov, B. Heterophoria and fusional convergence and divergence in preschool children. Med. Glas. 2012, 9, 293–298. [Google Scholar]
- Hashemi, H.; Pakzad, R.; Heydarian, S.; Yekta, A.; Aghamirsalim, M.; Shokrollahzadeh, F.; Khoshhal, F.; Pakbin, M.; Ramin, S.; Khabazkhoob, M. Global and regional prevalence of strabismus: A comprehensive systematic review and meta-analysis. Strabismus 2019, 27, 54–65. [Google Scholar] [CrossRef] [PubMed]
- Von Noorden, G.K. Binocular Vision and Ocular Motility. Theory and Management of Strabismus; Mosby, Inc. A Harcourt Health Sciences Company: St. Louis, MI, USA, 1990. [Google Scholar]
- Wright, K.W.; Spiegel, P.H.; Thompson, L.S. Handbook of Pediatric Strabismus and Amblyopia; Springer: Berlin/Heidelberg, Germany, 2006; ISBN 0387279245. [Google Scholar]
- Holmes, J.M.; Leske, D.A.; Hohberger, G.G. Defining Real Change in Prism-Cover Test Measurements. Am. J. Ophthalmol. 2008, 145, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Roodhooft, J.M. Screen tests used to map out ocular deviations. Bull. Soc. Belge Ophtalmol. 2007, 305, 57–67. [Google Scholar]
- Hess, W.R.I. Ein einfaches messendes Verfahren zur Motilitätsprüfung der Augen. Ophthalmologica 1916, 35, 201–219. [Google Scholar] [CrossRef]
- Roper-Hall, G. The hess screen test. Am. Orthopt. J. 2006, 56, 166–174. [Google Scholar] [CrossRef]
- Lancaster, W.B. Detecting, measuring, plotting and interpreting ocular deviations. Arch. Ophthalmol. 1939, 22, 867–880. [Google Scholar] [CrossRef]
- Christoff, A.; Guyton, D.L. The Lancaster red-green test. Am. Orthopt. J. 2006, 56, 157–165. [Google Scholar] [CrossRef]
- Harms, H. Über die Untersuchung von Augenmuskellähmungen. Albr. Graefes Arch. Ophthalmol. 1941, 144, 129–149. [Google Scholar] [CrossRef]
- Awadein, A. A computerized version of the Lancaster red-green test. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2013, 17, 197–202. [Google Scholar] [CrossRef]
- Watts, P.; Nayak, H.; Lim, M.K.; Ashcroft, A.; Al Madfai, H.; Palmer, H. Validity and ease of use of a computerized Hess chart. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2011, 15, 451–454. [Google Scholar] [CrossRef]
- Bergamin, O.; Zee, D.S.; Roberts, D.C.; Landau, K.; Lasker, A.G.; Straumann, D. Three-dimensional Hess screen test with binocular dual search coils in a three-field magnetic system. Investig. Ophthalmol. Vis. Sci. 2001, 42, 660–667. [Google Scholar]
- Weber, K.P.; Landau, K.; Palla, A.; Haslwanter, T.; Straumann, D. Ocular rotation axes during dynamic Bielschowsky head-tilt testing in unilateral trochlear nerve palsy. Investig. Ophthalmol. Vis. Sci. 2004, 45, 455–465. [Google Scholar] [CrossRef]
- Mehringer, W.; Wirth, M.; Risch, F.; Roth, D.; Michelson, G.; Eskofier, B. Hess Screen Revised: How Eye Tracking and Virtual Reality change Strabismus Assessment. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Mexico, 1–5 November 2021; pp. 2058–2062. [Google Scholar] [CrossRef]
- Weber, K.P.; Rappoport, D.; Dysli, M.; Schmückle Meier, T.; Marks, G.B.; Bockisch, C.J.; Landau, K.; MacDougall, H.G. Strabismus Measurements with Novel Video Goggles. Ophthalmology 2017, 124, 1849–1856. [Google Scholar] [CrossRef]
- Houben, M.M.J.; Goumans, J.; van der Steen, J. Recording three-dimensional eye movements: Scleral search coils versus video oculography. Investig. Ophthalmol. Vis. Sci. 2006, 47, 179–187. [Google Scholar] [CrossRef]
- Yang, H.K.; Seo, J.-M.; Hwang, J.-M.; Kim, K.G. Automated analysis of binocular alignment using an infrared camera and selective wavelength filter. Investig. Ophthalmol. Vis. Sci. 2013, 54, 2733–2737. [Google Scholar] [CrossRef]
- Miladinović, A.; Quaia, C.; Ajčević, M.; Diplotti, L.; Cumming, B.G.; Pensiero, S.; Accardo, A. Ocular-following responses in school-age children. PLoS ONE 2022, 17, e0277443. [Google Scholar] [CrossRef]
- Liu, F.; Zhao, J.; Han, T.; Shen, Y.; Li, M.; Liu, J.; Yang, D.; Fang, Y.; Yan, L.; Zhou, X. Screening for Stereopsis Using an Eye-Tracking Glasses-Free Display in Adults: A Pilot Study. Front. Med. 2022, 8, 814908. [Google Scholar] [CrossRef]
- Quaia, C.; Fitzgibbon, E.J.; Optican, L.M.; Cumming, B.G. Binocular summation for reflexive eye movements: A potential diagnostic tool for stereodeficiencies. Investig. Ophthalmol. Vis. Sci. 2018, 59, 5816–5822. [Google Scholar] [CrossRef]
- Klainguti, G.; Ancos, E.; Presset, C. Inclination of the Hess-Weiss coordimetric graph. An indirect sign of ocular torsion? Klin. Monbl. Augenheilkd. 1997, 210, 299–301. [Google Scholar] [CrossRef] [PubMed]
- Spielmann, A.; Spielmann, A.C. The tilt of the lancaster chart: An indirect qualitative and probably quantitative sign of cyclodeviation. Am. Orthopt. J. 1997, 47, 91–98. [Google Scholar] [CrossRef]
- Hugonnier, R. Linteret du test rouge-vert de lancaster dans letude des diplopies. In Proceedings of the Presse Medicale; masson editeur 120 blvd saint-germain, 75280 paris 06, france. Elsevier: Amsterdam, The Netherlands, 1952; Volume 60, p. 1560. [Google Scholar]
- Zee, D.S.; Chu, F.C.; Optican, L.M.; Carl, J.R.; Reingold, D. Graphic analysis of paralytic strabismus with the Lancaster red-green test. Am. J. Ophthalmol. 1984, 97, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, C.; Hatch, J.F.; Sanchez, R.M. A new computer-assisted Lancaster test (CALT). Ophthalmic Lit. 1995, 4, 310. [Google Scholar]
- Woo, S.J.; Hwang, J.-M. Efficacy of the Lancaster Red–Green Test for the Diagnosis of Superior Oblique Palsy. Optom. Vis. Sci. 2006, 83, 830–835. [Google Scholar] [CrossRef]
- Armesto, A.; Ugrin, M.C.; Travelletti, E.; Schlaen, A.; Piantanida, N. Hess Lancaster screen test with the head tilted: A useful test in the diagnosis of bilateral fourth nerve palsies. Eur. J. Ophthalmol. 2008, 18, 278–281. [Google Scholar] [CrossRef]
- Pfenninger, L.; Landau, K.; Bergamin, O. Comparison of Harms tangent screen and search coil recordings in patients with trochlear nerve palsy. Vision Res. 2006, 46, 1404–1410. [Google Scholar] [CrossRef]
- Thorisdottir, R.L.; Sundgren, J.; Sheikh, R.; Blohmé, J.; Hammar, B.; Kjellström, S.; Malmsjö, M. Comparison of a new digital KM screen test with conventional Hess and Lees screen tests in the mapping of ocular deviations. J. AAPOS 2018, 22, 277–280.e6. [Google Scholar] [CrossRef]
- Pratt-Johnson, J.A. Fusion and suppression: Development and loss. J. Pediatr. Ophthalmol. Strabismus 1992, 29, 4–9. [Google Scholar] [CrossRef]
- Roper-Hall, G. Overview and Comparison of Screen Test Methods Used in Quantifying Ocular Motility Disorders. Am. Orthopt. J. 2006, 56, 151–156. [Google Scholar] [CrossRef]
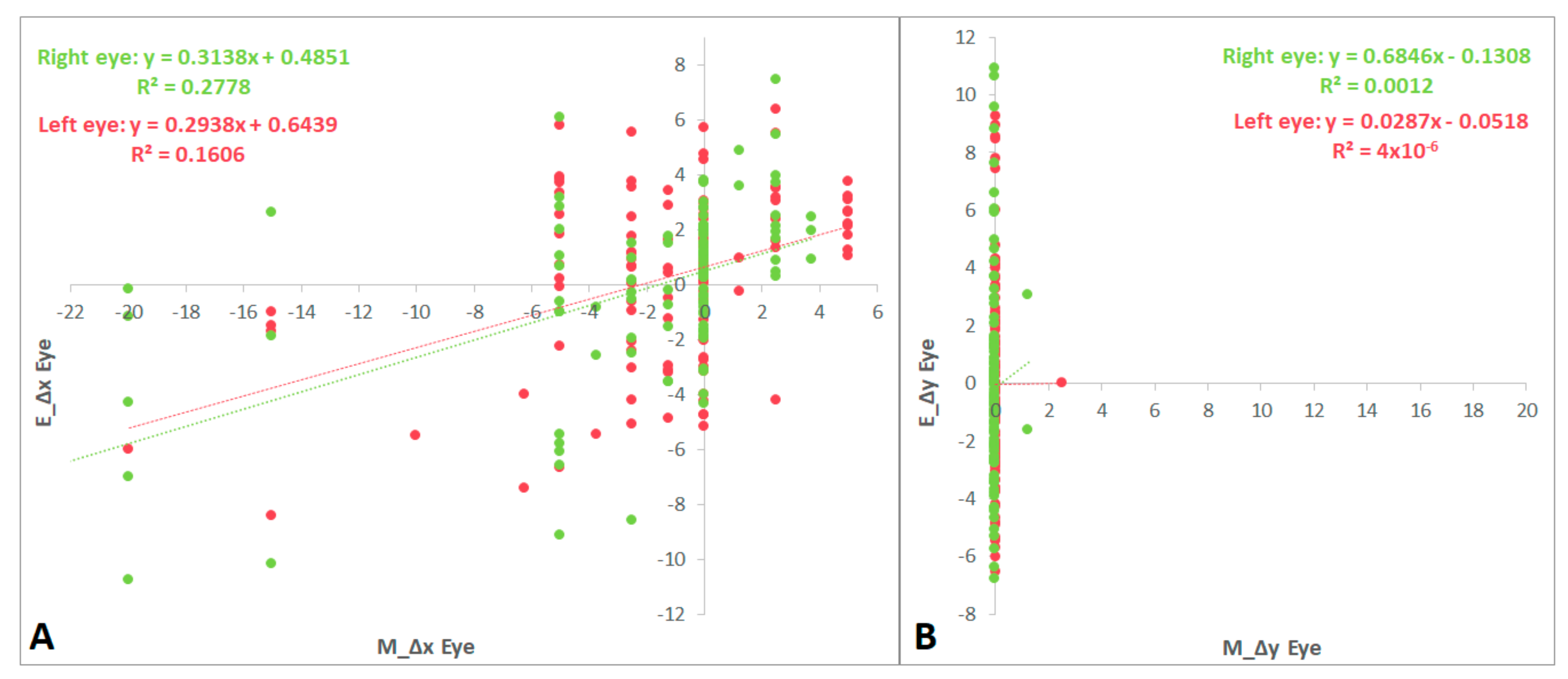
| Examiner vs. Eye-Tracker Values | Differences (p) | Correlation Coefficient (cc) (p) |
|---|---|---|
| ∆x LE | <0.001 | 0.401 (<0.001) |
| ∆y LE | 0.815 | 0.002 (0.983) |
| ∆x RE | <0.001 | 0.527 (<0.001) |
| ∆y RE | 0.650 | 0.034 (0.716) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orduna-Hospital, E.; Maurain-Orera, L.; Lopez-de-la-Fuente, C.; Sanchez-Cano, A. Hess Lancaster Screen Test with Eye Tracker: An Objective Method for the Measurement of Binocular Gaze Direction. Life 2023, 13, 668. https://doi.org/10.3390/life13030668
Orduna-Hospital E, Maurain-Orera L, Lopez-de-la-Fuente C, Sanchez-Cano A. Hess Lancaster Screen Test with Eye Tracker: An Objective Method for the Measurement of Binocular Gaze Direction. Life. 2023; 13(3):668. https://doi.org/10.3390/life13030668
Chicago/Turabian StyleOrduna-Hospital, Elvira, Luz Maurain-Orera, Carmen Lopez-de-la-Fuente, and Ana Sanchez-Cano. 2023. "Hess Lancaster Screen Test with Eye Tracker: An Objective Method for the Measurement of Binocular Gaze Direction" Life 13, no. 3: 668. https://doi.org/10.3390/life13030668
APA StyleOrduna-Hospital, E., Maurain-Orera, L., Lopez-de-la-Fuente, C., & Sanchez-Cano, A. (2023). Hess Lancaster Screen Test with Eye Tracker: An Objective Method for the Measurement of Binocular Gaze Direction. Life, 13(3), 668. https://doi.org/10.3390/life13030668






