The Role of Dietary Fats in the Development and Treatment of Endometriosis
Abstract
1. Introduction
2. Literature Search
3. Total Fats (TF)
4. Saturated Fatty Acids (SFAs)
5. Monounsaturated Fatty Acids (MUFAs)
6. Polyunsaturated Fatty Acids (PUFAs)
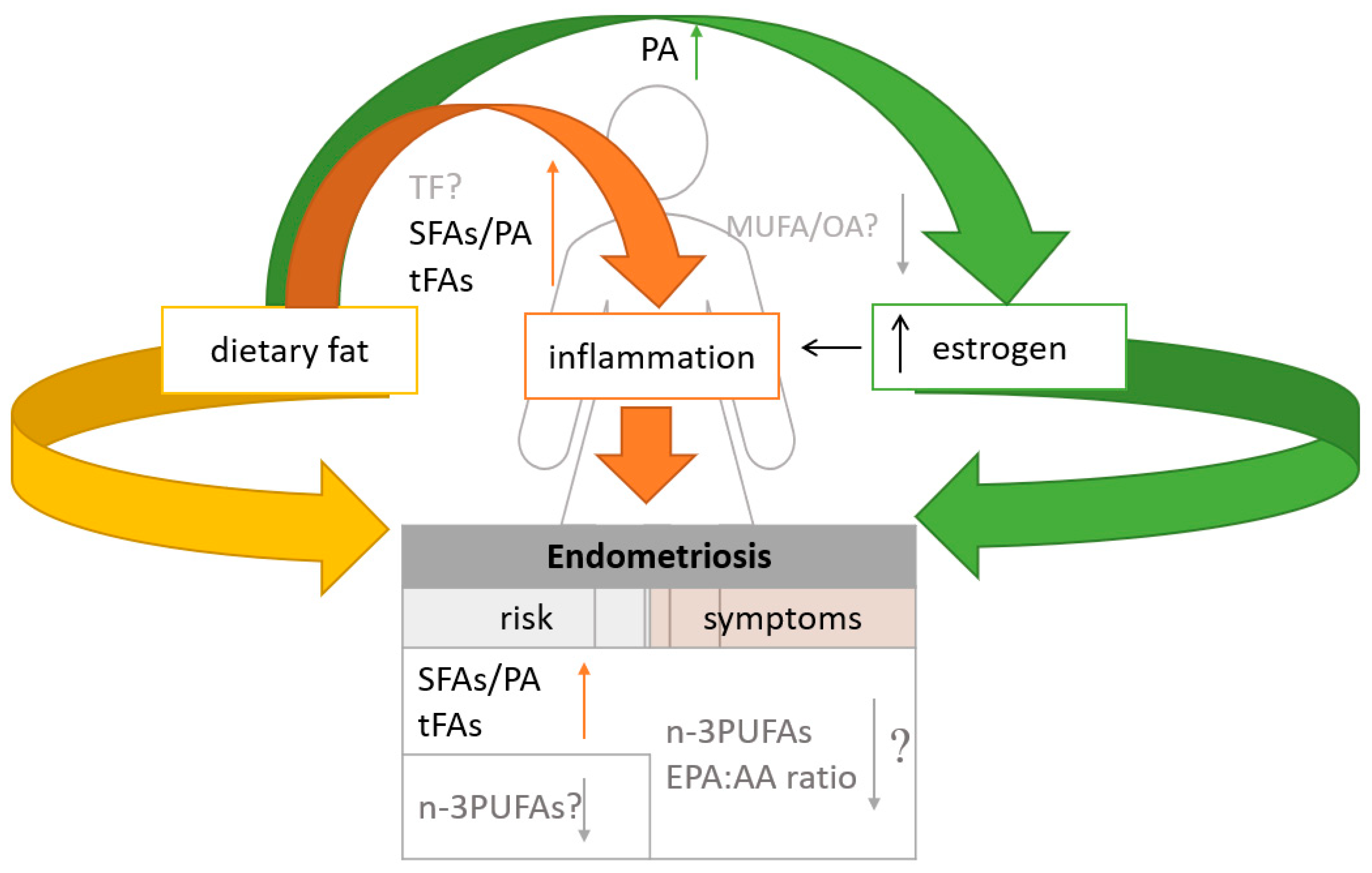
7. Trans Fatty Acids (tFAs)
8. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bulun, S.E.; Yilmaz, B.D.; Sison, C.; Miyazaki, K.; Bernardi, L.; Liu, S.; Kohlmeier, A.; Yin, P.; Milad, M.; Wei, J. Endometriosis. Endocr. Rev. 2019, 40, 1048–1079. [Google Scholar] [CrossRef] [PubMed]
- Macer, M.L.; Taylor, H.S. Endometriosis and Infertility. Obstet. Gynecol. Clin. N. Am. 2012, 39, 535–549. [Google Scholar] [CrossRef]
- Terzic, M.; Aimagambetova, G.; Garzon, S.; Bapayeva, G.; Ukybassova, T.; Terzic, S.; Norton, M.; Laganà, A.S. Ovulation Induction in Infertile Women with Endometriotic Ovarian Cysts: Current Evidence and Potential Pitfalls. Minerva Med. 2020, 111, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Missmer, S.A.; Cramer, D.W. The Epidemiology of Endometriosis. Obstet. Gynecol. Clin. N. Am. 2003, 30, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Tanbo, T.; Fedorcsak, P. Endometriosis-Associated Infertility: Aspects of Pathophysiological Mechanisms and Treatment Options. Acta Obstet. Gynecol. Scand. 2017, 96, 659–667. [Google Scholar] [CrossRef]
- Vinatier, D.; Orazi, G.; Cosson, M.; Dufour, P. Theories of Endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2001, 96, 21–34. [Google Scholar] [CrossRef]
- Basta, A.; Brucka, A.; Górski, J.; Kotarski, J.; Kulig, B.; Oszukowski, P.; Poreba, R.; Radowicki, S.; Radwan, J.; Sikora, J.; et al. The statement of Polish Society’s Experts Group concerning diagnostics and methods of endometriosis treatment. Ginekol. Pol. 2012, 83, 871–876. [Google Scholar]
- Litson, J.; Agnes, R.; Ravikumar, G. Histotyping and Grading of Endometriosis and Its Association with Clinico-Pathological Parameters. J. Obstet. Gynaecol. 2022, 43, 1–9. [Google Scholar] [CrossRef]
- Becker, C.M.; Bokor, A.; Heikinheimo, O.; Horne, A.; Jansen, F.; Kiesel, L.; King, K.; Kvaskoff, M.; Nap, A.; Petersen, K.; et al. ESHRE Guideline: Endometriosis. Hum. Reprod. Open 2022, 2022, hoac009. [Google Scholar] [CrossRef]
- Jurkiewicz-Przondziono, J.; Lemm, M.; Kwiatkowska-Pamuła, A.; Ziółko, E.; Wójtowicz, M.K. Influence of Diet on the Risk of Developing Endometriosis. Ginekol. Pol. 2017, 88, 96–102. [Google Scholar] [CrossRef]
- Czyzyk, A.; Podfigurna, A.; Szeliga, A.; Meczekalski, B. Update on Endometriosis Pathogenesis. Minerva Obstet. Gynecol. 2017, 69, 447–461. [Google Scholar] [CrossRef]
- Krakhotkin, D.V.; Silkina, M.N.; Chernylovskyi, V.A.; Gayvoronskaya, S.A. The Dienogest-Related Cystitis in Women with Endometriosis: A Prospective, Controlled, Comparative Study. J. Obstet. Gynaecol. 2022, 42, 2492–2497. [Google Scholar] [CrossRef]
- Chopyak, V.V.; Koval, H.D.; Havrylyuk, A.M.; Lishchuk-Yakymovych, K.A.; Potomkina, H.A.; Kurpisz, M.K. Immunopathogenesis of Endometriosis—A Novel Look at an Old Problem. Cent.-Eur. J. Immunol. 2022, 47, 109–116. [Google Scholar] [CrossRef]
- Garitazelaia, A.; Rueda-Martínez, A.; Arauzo, R.; de Miguel, J.; Cilleros-Portet, A.; Marí, S.; Bilbao, J.R.; Fernandez-Jimenez, N.; García-Santisteban, I. A Systematic Two-Sample Mendelian Randomization Analysis Identifies Shared Genetic Origin of Endometriosis and Associated Phenotypes. Life 2021, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Bartiromo, L.; Schimberni, M.; Villanacci, R.; Ottolina, J.; Dolci, C.; Salmeri, N.; Viganò, P.; Candiani, M. Endometriosis and Phytoestrogens: Friends or Foes? A Systematic Review. Nutrients 2021, 13, 2532. [Google Scholar] [CrossRef] [PubMed]
- Cai, X.; Liu, M.; Zhang, B.; Zhao, S.-J.; Jiang, S.-W. Phytoestrogens for the Management of Endometriosis: Findings and Issues. Pharmaceuticals 2021, 14, 569. [Google Scholar] [CrossRef] [PubMed]
- Attar, E.; Bulun, S.E. Aromatase and Other Steroidogenic Genes in Endometriosis: Translational Aspects. Hum. Reprod. Update 2006, 12, 49–56. [Google Scholar] [CrossRef]
- Tsubura, A.; Uehara, N.; Kiyozuka, Y.; Shikata, N. Dietary Factors Modifying Breast Cancer Risk and Relation to Time of Intake. J. Mammary Gland Biol. Neoplasia 2005, 10, 87–100. [Google Scholar] [CrossRef]
- Missmer, S.A.; Chavarro, J.E.; Malspeis, S.; Bertone-Johnson, E.R.; Hornstein, M.D.; Spiegelman, D.; Barbieri, R.L.; Willett, W.C.; Hankinson, S.E. A Prospective Study of Dietary Fat Consumption and Endometriosis Risk. Hum. Reprod. 2010, 25, 1528–1535. [Google Scholar] [CrossRef]
- Huang, M.; Liu, J.; Lin, X.; Goto, A.; Song, Y.; Tinker, L.F.; Chan, K.K.; Liu, S. Relationship between Dietary Carbohydrates Intake and Circulating Sex Hormone-Binding Globulin Levels in Postmenopausal Women. J. Diabetes 2018, 10, 467–477. [Google Scholar] [CrossRef]
- Minihane, A.M.; Vinoy, S.; Russell, W.R.; Baka, A.; Roche, H.M.; Tuohy, K.M.; Teeling, J.L.; Blaak, E.E.; Fenech, M.; Vauzour, D.; et al. Low-Grade Inflammation, Diet Composition and Health: Current Research Evidence and Its Translation. Br. J. Nutr. 2015, 114, 999–1012. [Google Scholar] [CrossRef]
- Liu, Z. Inflammation and Endometriosis. Front. Biosci. 2016, 21, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Christodoulakos, G.; Augoulea, A.; Lambrinoudaki, I.; Sioulas, V.; Creatsas, G. Pathogenesis of Endometriosis: The Role of Defective ‘Immunosurveillance’. Eur. J. Contracept. Reprod. Health Care 2007, 12, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Mantyh, P.W. Neurobiology of Substance P and the NK1 Receptor. J. Clin. Psychiatry 2002, 63 (Suppl. S11), 6–10. [Google Scholar]
- Richardson, J.D.; Vasko, M.R. Cellular Mechanisms of Neurogenic Inflammation. J. Pharmacol. Exp. Ther. 2002, 302, 839–845. [Google Scholar] [CrossRef]
- Pongratz, G.; Straub, R.H. The Sympathetic Nervous Response in Inflammation. Arthritis Res. Ther. 2014, 16, 504. [Google Scholar] [CrossRef] [PubMed]
- Asante, A.; Taylor, R.N. Endometriosis: The Role of Neuroangiogenesis. Annu. Rev. Physiol. 2011, 73, 163–182. [Google Scholar] [CrossRef]
- Scholl, B.; Bersinger, N.A.; Kuhn, A.; Mueller, M.D. Correlation between Symptoms of Pain and Peritoneal Fluid Inflammatory Cytokine Concentrations in Endometriosis. Gynecol. Endocrinol. 2009, 25, 701–706. [Google Scholar] [CrossRef]
- Kuteken, F.S.; Lancellotti, C.L.P.; Ribeiro, H.S.A.A.; Aldrighi, J.M.; Ribeiro, P.A.A.G. Expressão de Mediadores Neurotróficos e Pró-Inflamatórios Na Endometriose de Reto e Sigmoide. Rev. Bras. Ginecol. E Obs. 2012, 34, 568–574. [Google Scholar] [CrossRef]
- Koga, K.; Osuga, Y.; Yoshino, O.; Hirota, Y.; Yano, T.; Tsutsumi, O.; Taketani, Y. Elevated Interleukin-16 Levels in the Peritoneal Fluid of Women with Endometriosis May Be a Mechanism for Inflammatory Reactions Associated with Endometriosis. Fertil. Steril. 2005, 83, 878–882. [Google Scholar] [CrossRef]
- Leiva, M.C.; Hasty, L.A.; Lyttle, C.R. Inflammatory Changes of the Endometrium in Patients with Minimal-to-Moderate Endometriosis. Fertil. Steril. 1994, 62, 967–972. [Google Scholar] [CrossRef] [PubMed]
- Lousse, J.-C.; Van Langendonckt, A.; González-Ramos, R.; Defrère, S.; Renkin, E.; Donnez, J. Increased Activation of Nuclear Factor-Kappa B (NF-ΚB) in Isolated Peritoneal Macrophages of Patients with Endometriosis. Fertil. Steril. 2008, 90, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Capellino, S. Role of Estrogens in Inflammatory Response: Expression of Estrogen Receptors in Peritoneal Fluid Macrophages from Endometriosis. Ann. N. Y. Acad. Sci. USA 2006, 1069, 263–267. [Google Scholar] [CrossRef]
- Fritsche, K.L. The Science of Fatty Acids and Inflammation. Adv. Nutr. 2015, 6, 293S–301S. [Google Scholar] [CrossRef] [PubMed]
- Acosta-Montaño, P.; García-González, V. Effects of Dietary Fatty Acids in Pancreatic Beta Cell Metabolism, Implications in Homeostasis. Nutrients 2018, 10, 393. [Google Scholar] [CrossRef]
- Gazvani, M.R.; Smith, L.; Haggarty, P.; Fowler, P.A.; Templeton, A. High ω-3:ω-6 Fatty Acid Ratios in Culture Medium Reduce Endometrial-Cell Survival in Combined Endometrial Gland and Stromal Cell Cultures from Women with and without Endometriosis. Fertil. Steril. 2001, 76, 717–722. [Google Scholar] [CrossRef]
- Baer, D.J.; Judd, J.T.; Clevidence, B.A.; Tracy, R.P. Dietary Fatty Acids Affect Plasma Markers of Inflammation in Healthy Men Fed Controlled Diets: A Randomized Crossover Study. Am. J. Clin. Nutr. 2004, 79, 969–973. [Google Scholar] [CrossRef]
- Bedaiwy, M.A. Prediction of Endometriosis with Serum and Peritoneal Fluid Markers: A Prospective Controlled Trial. Hum. Reprod. 2002, 17, 426–431. [Google Scholar] [CrossRef]
- Mier-Cabrera, J.; Aburto-Soto, T.; Burrola-Méndez, S.; Jiménez-Zamudio, L.; Tolentino, M.C.; Casanueva, E.; Hernández-Guerrero, C. Women with Endometriosis Improved Their Peripheral Antioxidant Markers after the Application of a High Antioxidant Diet. Reprod. Biol. Endocrinol. 2009, 7, 54. [Google Scholar] [CrossRef]
- James, M.J.; Gibson, R.A.; Cleland, L.G. Dietary Polyunsaturated Fatty Acids and Inflammatory Mediator Production. Am. J. Clin. Nutr. 2000, 71, 343s–348s. [Google Scholar] [CrossRef] [PubMed]
- Netsu, S.; Konno, R.; Odagiri, K.; Soma, M.; Fujiwara, H.; Suzuki, M. Oral Eicosapentaenoic Acid Supplementation as Possible Therapy for Endometriosis. Fertil. Steril. 2008, 90, 1496–1502. [Google Scholar] [CrossRef]
- World Health Organization. WHO Fact Sheet, No 394 Healthy Diet. 2018. Available online: https://cdn.who.int/media/docs/default-source/healthy-diet/healthy-diet-fact-sheet-394.pdf (accessed on 24 February 2023).
- EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA). Scientific Opinion on Dietary Reference Values for Fats, Including Saturated Fatty Acids, Polyunsaturated Fatty Acids, Monounsaturated Fatty Acids, Trans Fatty Acids, and Cholesterol. EFSA J. 2010, 8, 1461. [Google Scholar] [CrossRef]
- Jarosz, M. Normy Żywienia dla Populacji Polskiej Nowelizacja; Instytut Żywności i Żywienia: Warszawa, Poland, 2012. [Google Scholar]
- Arab, A.; Karimi, E.; Vingrys, K.; Kelishadi, M.R.; Mehrabani, S.; Askari, G. Food Groups and Nutrients Consumption and Risk of Endometriosis: A Systematic Review and Meta-Analysis of Observational Studies. Nutr. J. 2022, 21, 58. [Google Scholar] [CrossRef] [PubMed]
- Trabert, B.; Peters, U.; De Roos, A.J.; Scholes, D.; Holt, V.L. Diet and Risk of Endometriosis in a Population-Based Case–Control Study. Br. J. Nutr. 2011, 105, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Samaneh, Y.; ShahidehJahanian, S.; Azadeh, M.; Anoshirvan, K. The Association of Food Consumption and Nutrient Intake with Endometriosis Risk in Iranian Women: A Case-Control Study. Int. J. Reprod. Biomed. 2019, 17, 661–670. [Google Scholar] [CrossRef]
- Britton, J.A.; Westhoff, C.; Howe, G.; Gammon, M.D. Diet and Benign Ovarian Tumors. Cancer Causes Control 2000, 11, 389–401. [Google Scholar] [CrossRef]
- Cani, P.D.; Bibiloni, R.; Knauf, C.; Waget, A.; Neyrinck, A.M.; Delzenne, N.M.; Burcelin, R. Changes in Gut Microbiota Control Metabolic Endotoxemia-Induced Inflammation in High-Fat Diet–Induced Obesity and Diabetes in Mice. Diabetes 2008, 57, 1470–1481. [Google Scholar] [CrossRef]
- Heard, M.E.; Melnyk, S.B.; Simmen, F.A.; Yang, Y.; Pabona, J.M.P.; Simmen, R.C.M. High-Fat Diet Promotion of Endometriosis in an Immunocompetent Mouse Model Is Associated with Altered Peripheral and Ectopic Lesion Redox and Inflammatory Status. Endocrinology 2016, 157, 2870–2882. [Google Scholar] [CrossRef]
- Savaris, A.L.; do Amaral, V.F. Nutrient Intake, Anthropometric Data and Correlations with the Systemic Antioxidant Capacity of Women with Pelvic Endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 158, 314–318. [Google Scholar] [CrossRef]
- Eshak, E.S.; Yamagishi, K.; Iso, H. Dietary Fat and Risk of Cardiovascular Disease. In Encyclopedia of Cardiovascular Research and Medicine; Elsevier: Amsterdam, The Netherlands, 2018; pp. 60–89. [Google Scholar] [CrossRef]
- Carta, G.; Murru, E.; Banni, S.; Manca, C. Palmitic Acid: Physiological Role, Metabolism and Nutritional Implications. Front. Physiol. 2017, 8, 902. [Google Scholar] [CrossRef]
- Carta, G.; Murru, E.; Lisai, S.; Sirigu, A.; Piras, A.; Collu, M.; Batetta, B.; Gambelli, L.; Banni, S. Dietary Triacylglycerols with Palmitic Acid in the Sn-2 Position Modulate Levels of N-Acylethanolamides in Rat Tissues. PLoS ONE 2015, 10, e0120424. [Google Scholar] [CrossRef] [PubMed]
- Rietschel, E.T.; Kirikae, T.; Schade, F.U.; Mamat, U.; Schmidt, G.; Loppnow, H.; Ulmer, A.J.; Zähringer, U.; Seydel, U.; Di Padova, F.; et al. Bacterial Endotoxin: Molecular Relationships of Structure to Activity and Function. FASEB J. 1994, 8, 217–225. [Google Scholar] [CrossRef]
- Hoshino, K.; Takeuchi, O.; Kawai, T.; Sanjo, H.; Ogawa, T.; Takeda, Y.; Takeda, K.; Akira, S. Cutting Edge: Toll-like Receptor 4 (TLR4)-Deficient Mice Are Hyporesponsive to Lipopolysaccharide: Evidence for TLR4 as the Lps Gene Product. J. Immunol. 1999, 162, 3749–3752. [Google Scholar] [CrossRef]
- Takeda, K.; Kaisho, T.; Akira, S. Toll-Like Receptors. Annu. Rev. Immunol. 2003, 21, 335–376. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Sohn, K.H.; Rhee, S.H.; Hwang, D. Saturated Fatty Acids, but Not Unsaturated Fatty Acids, Induce the Expression of Cyclooxygenase-2 Mediated through Toll-like Receptor 4. J. Biol. Chem. 2001, 276, 16683–16689. [Google Scholar] [CrossRef] [PubMed]
- Vergnaud, A.-C.; Norat, T.; Mouw, T.; Romaguera, D.; May, A.M.; Bueno-de-Mesquita, H.B.; van der A., D.; Agudo, A.; Wareham, N.; Khaw, K.-T.; et al. Macronutrient Composition of the Diet and Prospective Weight Change in Participants of the EPIC-PANACEA Study. PLoS ONE 2013, 8, e57300. [Google Scholar] [CrossRef]
- Seli, E.; Berkkanoglu, M.; Arici, A. Pathogenesis of Endometriosis. Obstet. Gynecol. Clin. N. Am. 2003, 30, 41–61. [Google Scholar] [CrossRef]
- Kris-Etherton, P.M. Monounsaturated Fatty Acids and Risk of Cardiovascular Disease. Circulation 1999, 100, 1253–1258. [Google Scholar] [CrossRef] [PubMed]
- Perdomo, L.; Beneit, N.; Otero, Y.F.; Escribano, Ó.; Díaz-Castroverde, S.; Gómez-Hernández, A.; Benito, M. Protective Role of Oleic Acid against Cardiovascular Insulin Resistance and in the Early and Late Cellular Atherosclerotic Process. Cardiovasc. Diabetol. 2015, 14, 75. [Google Scholar] [CrossRef]
- Medeiros-de-Moraes, I.M.; Gonçalves-de-Albuquerque, C.F.; Kurz, A.R.M.; de Jesus Oliveira, F.M.; de Abreu, V.H.P.; Torres, R.C.; Carvalho, V.F.; Estato, V.; Sperandio, M.; de Castro-Faria-Neto, H.C.; et al. Omega-9 Oleic Acid, the Main Compound of Olive Oil, Mitigates Inflammation during Experimental Sepsis. Oxid. Med. Cell. Longev. 2018, 2018, 1–13. [Google Scholar] [CrossRef]
- de Souza, C.O.; Valenzuela, C.A.; Baker, E.J.; Miles, E.A.; Rosa Neto, J.C.; Calder, P.C. Palmitoleic Acid Has Stronger Anti-Inflammatory Potential in Human Endothelial Cells Compared to Oleic and Palmitic Acids. Mol. Nutr. Food Res. 2018, 62, 1800322. [Google Scholar] [CrossRef] [PubMed]
- Demézio da Silva, C.V.; Felipe, V.L.; Shivappa, N.; Hebert, J.R.; Perini, J.A.; de Brito, P.D.; Cardoso, J.V.; Ferrari, R.; de Almeida Filho, G.L. Dietary Inflammatory Index Score and Risk of Developing Endometriosis: A Case–Control Study. J. Endometr. Pelvic Pain Disord. 2021, 13, 32–39. [Google Scholar] [CrossRef]
- Hopeman, M.M.; Riley, J.K.; Frolova, A.I.; Jiang, H.; Jungheim, E.S. Serum Polyunsaturated Fatty Acids and Endometriosis. Reprod. Sci. 2015, 22, 1083–1087. [Google Scholar] [CrossRef]
- Anderson, B.M.; Ma, D.W. Are All N-3 Polyunsaturated Fatty Acids Created Equal? Lipids Health Dis. 2009, 8, 33. [Google Scholar] [CrossRef]
- Lee, J.Y.; Zhao, L.; Hwang, D.H. Modulation of Pattern Recognition Receptor-Mediated Inflammation and Risk of Chronic Diseases by Dietary Fatty Acids. Nutr. Rev. 2010, 68, 38–61. [Google Scholar] [CrossRef] [PubMed]
- Pischon, T.; Hankinson, S.E.; Hotamisligil, G.S.; Rifai, N.; Willett, W.C.; Rimm, E.B. Habitual Dietary Intake of N-3 and n-6 Fatty Acids in Relation to Inflammatory Markers Among US Men and Women. Circulation 2003, 108, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Weiss, G.; Goldsmith, L.T.; Taylor, R.N.; Bellet, D.; Taylor, H.S. Inflammation in Reproductive Disorders. Reprod. Sci. 2009, 16, 216–229. [Google Scholar] [CrossRef] [PubMed]
- Scaioli, E.; Liverani, E.; Belluzzi, A. The Imbalance between N-6/n-3 Polyunsaturated Fatty Acids and Inflammatory Bowel Disease: A Comprehensive Review and Future Therapeutic Perspectives. Int. J. Mol. Sci. 2017, 18, 2619. [Google Scholar] [CrossRef]
- Gutiérrez, S.; Svahn, S.L.; Johansson, M.E. Effects of Omega-3 Fatty Acids on Immune Cells. Int. J. Mol. Sci. 2019, 20, 5028. [Google Scholar] [CrossRef]
- Camuesco, D.; Gálvez, J.; Nieto, A.; Comalada, M.; Rodríguez-Cabezas, M.E.; Concha, A.; Xaus, J.; Zarzuelo, A. Dietary Olive Oil Supplemented with Fish Oil, Rich in EPA and DHA (n-3) Polyunsaturated Fatty Acids, Attenuates Colonic Inflammation in Rats with DSS-Induced Colitis. J. Nutr. 2005, 135, 687–694. [Google Scholar] [CrossRef]
- Tomio, K.; Kawana, K.; Taguchi, A.; Isobe, Y.; Iwamoto, R.; Yamashita, A.; Kojima, S.; Mori, M.; Nagamatsu, T.; Arimoto, T.; et al. Omega-3 Polyunsaturated Fatty Acids Suppress the Cystic Lesion Formation of Peritoneal Endometriosis in Transgenic Mouse Models. PLoS ONE 2013, 8, e73085. [Google Scholar] [CrossRef] [PubMed]
- Canny, G.O.; Lessey, B.A. The Role of Lipoxin A4 in Endometrial Biology and Endometriosis. Mucosal Immunol. 2013, 6, 439–450. [Google Scholar] [CrossRef] [PubMed]
- Fjerbæk, A.; Knudsen, U.B. Endometriosis, Dysmenorrhea and Diet—What Is the Evidence? Eur. J. Obstet. Gynecol. Reprod. Biol. 2007, 132, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Hansen, S.O.; Knudsen, U.B. Endometriosis, Dysmenorrhoea and Diet. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 169, 162–171. [Google Scholar] [CrossRef]
- Nodler, J.L.; DiVasta, A.D.; Vitonis, A.F.; Karevicius, S.; Malsch, M.; Sarda, V.; Fadayomi, A.; Harris, H.R.; Missmer, S.A. Supplementation with Vitamin D or ω-3 Fatty Acids in Adolescent Girls and Young Women with Endometriosis (SAGE): A Double-Blind, Randomized, Placebo-Controlled Trial. Am. J. Clin. Nutr. 2020, 112, 229–236. [Google Scholar] [CrossRef]
- Signorile, P.G.; Viceconte, R.; Baldi, A. Novel Dietary Supplement Association Reduces Symptoms in Endometriosis Patients. J. Cell. Physiol. 2018, 233, 5920–5925. [Google Scholar] [CrossRef]
- Deutch, B. Menstrual Pain in Danish Women Correlated with Low N-3 Polyunsaturated Fatty Acid Intake. Eur. J. Clin. Nutr. 1995, 49, 508–516. [Google Scholar]
- Khanaki, K.; Nouri, M.; Ardekani, A.M.; Ghassemzadeh, A.; Shahnazi, V.; Sadeghi, M.R.; Darabi, M.; Mehdizadeh, A.; Dolatkhah, H.; Saremi, A.; et al. Evaluation of the Relationship between Endometriosis and Omega-3 and Omega-6 Polyunsaturated Fatty Acids. Iran. Biomed. J. 2012, 16, 38–43. [Google Scholar] [CrossRef]
- Covens, A.L.; Christopher, P.; Casper, R.F. The Effect of Dietary Supplementation with Fish Oil Fatty Acids on Surgically Induced Endometriosis in the Rabbit. Fertil. Steril. 1988, 49, 698–703. [Google Scholar] [CrossRef]
- Akyol, A.; Şimşek, M.; İlhan, R.; Can, B.; Baspinar, M.; Akyol, H.; Gül, H.F.; Gürsu, F.; Kavak, B.; Akın, M. Efficacies of Vitamin D and Omega-3 Polyunsaturated Fatty Acids on Experimental Endometriosis. Taiwan J. Obstet. Gynecol. 2016, 55, 835–839. [Google Scholar] [CrossRef]
- Herington, J.L.; Glore, D.R.; Lucas, J.A.; Osteen, K.G.; Bruner-Tran, K.L. Dietary Fish Oil Supplementation Inhibits Formation of Endometriosis-Associated Adhesions in a Chimeric Mouse Model. Fertil. Steril. 2013, 99, 543–550.e1. [Google Scholar] [CrossRef]
- Attaman, J.A.; Stanic, A.K.; Kim, M.; Lynch, M.P.; Rueda, B.R.; Styer, A.K. The Anti-Inflammatory Impact of Omega-3 Polyunsaturated Fatty Acids During the Establishment of Endometriosis-Like Lesions. Am. J. Reprod. Immunol. 2014, 72, 392–402. [Google Scholar] [CrossRef]
- Pereira, F.E.X.G.; das Chagas Medeiros, F.; Rocha, H.A.L.; da Silva; K.S. Effects of Omega-6/3 and Omega-9/6 Nutraceuticals on Pain and Fertility in Peritoneal Endometriosis in Rats. Acta Cir. Bras. 2019, 34, e201900405. [Google Scholar] [CrossRef] [PubMed]
- Oteng, A.-B.; Kersten, S. Mechanisms of Action of Trans Fatty Acids. Adv. Nutr. 2020, 11, 697–708. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, A.H. Dietary Trans Fatty Acids and Cardiovascular Disease Risk: Past and Present. Curr. Atheroscler. Rep. 2014, 16, 433. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations. Fats and Fatty Acids in Human Nutrition. Report of an Expert Consultation; FAO Food and Nutrition Paper; Food and Agriculture Organization of the United Nations: Rome, Italy, 2010; Volume 91, pp. 1–166. [Google Scholar]
- Parazzini, F.; Viganò, P.; Candiani, M.; Fedele, L. Diet and Endometriosis Risk: A Literature Review. Reprod. Biomed. Online 2013, 26, 323–336. [Google Scholar] [CrossRef] [PubMed]
- Capobianco, A.; Monno, A.; Cottone, L.; Venneri, M.A.; Biziato, D.; Di Puppo, F.; Ferrari, S.; De Palma, M.; Manfredi, A.A.; Rovere-Querini, P. Proangiogenic Tie2+ Macrophages Infiltrate Human and Murine Endometriotic Lesions and Dictate Their Growth in a Mouse Model of the Disease. Am. J. Pathol. 2011, 179, 2651–2659. [Google Scholar] [CrossRef]
- Saravanan, N.; Haseeb, A.; Ehtesham, N.Z.; Ghafoorunissa. Differential Effects of Dietary Saturated and Trans-Fatty Acids on Expression of Genes Associated with Insulin Sensitivity in Rat Adipose Tissue. Eur. J. Endocrinol. 2005, 153, 159–165. [Google Scholar] [CrossRef]
- Iwaki, M.; Matsuda, M.; Maeda, N.; Funahashi, T.; Matsuzawa, Y.; Makishima, M.; Shimomura, I. Induction of Adiponectin, a Fat-Derived Antidiabetic and Antiatherogenic Factor, by Nuclear Receptors. Diabetes 2003, 52, 1655–1663. [Google Scholar] [CrossRef]
- Lebovic, D.I.; Kir, M.; Casey, C.L. Peroxisome Proliferator–Activated Receptor-Gamma Induces Regression of Endometrial Explants in a Rat Model of Endometriosis. Fertil. Steril. 2004, 82, 1008–1013. [Google Scholar] [CrossRef]
- Lebovic, D.I.; Mwenda, J.M.; Chai, D.C.; Mueller, M.D.; Santi, A.; Fisseha, S.; D’Hooghe, T. PPAR-Gamma Receptor Ligand Induces Regression of Endometrial Explants in Baboons: A Prospective, Randomized, Placebo- and Drug-Controlled Study. Fertil. Steril. 2007, 88 (Suppl. S4), 1108–1119. [Google Scholar] [CrossRef] [PubMed]
- Mu, F.; Rich-Edwards, J.; Rimm, E.B.; Spiegelman, D.; Forman, J.P.; Missmer, S.A. Association Between Endometriosis and Hypercholesterolemia or Hypertension. Hypertension 2017, 70, 59–65. [Google Scholar] [CrossRef] [PubMed]
| Study Design | Subject | Results | |||||
|---|---|---|---|---|---|---|---|
| TF | SFAs | MUFAs | PUFAs n-3 | PUFAs n-6 | tFAs | ||
| Meta-analysis [45] | The association between i.a. fats and the risk of endometriosis among adult women; 8 publications, including 5 cohorts and 3 case-control. | No effect | ↑ | No effect | No effect | No effect | ↑ |
| Prospective study [19] | The relation between dietary fat intake and the risk of endometriosis; the experimental group n = 1199 women aged 25–42 years with endometriosis; median intake of total fat 24.2–38; SFAs 8.1–13.9; MUFAs 8.9–14.8; PUFAs 4.1–7.0; n-3, 0.4–0.8; n-6, 3.5–6.4; tFAs 0.9–2.3 % of energy. | No effect | No effect SFA; ↑ PA | No effect | ↓ | No effect | ↑ |
| Case-control [46] | Dietary risk factors, i.e., fats for endometriosis; the experimental group n = 284 women aged 20–65 years with endometriosis; median intake of total fat 54.8 g, SFAs 19.2 g, MUFAs 20.3 g, tFAs 3.2 g. | ↓ | ↓ | ↓ | - | - | ↓ |
| Case-control [47] | The relationship between food consumption and nutrient i.a. fat intake with risk of endometriosis; n = 156: n = 78 women with endometriosis and control group n = 78; the regression analyses (odds ratio). | No effect | - | ↓ ↓ OA | ↓ | - | - |
| Case-control [48] | The relation between i.a fats and benign ovarian tumors (BOTs) and nutrients, primarily dietary fat; the experimental group n = 393 women with BOTs, n = 280 women with endometrial tumors; median intake of total fat 48.9 g, SFAs 18.9 g, MUFAs 19.9 g, PUFAs 10.3 g. | ↑ | ↑ | ↑ | ↑ | ↑ | - |
| Case-control [51] | The relation between dietary fat intake and the risk of endometriosis; the experimental group n = 25 women with stage I–IV endometriosis; median intake of SFAs 18.56 g, n-3 PUFAs 0.66 g; n-6 PUFAs 9.61 g. | - | No effect | - | ↓ | ↓ | - |
| In vitro study [36] | The effects of composition of n-3 and n-6 PUFAs on in vitro proliferation of endometrial cells and their production of the cytokine interleukin-8 (IL-8); endometrial cells from women with and without endometriosis. | - | - | - | ↓ | - | - |
| Subject | Results | |
|---|---|---|
| n-3 PUFAs | n-6 PUFAs | |
| Dietary supplementation with fish oil containing EPA/DHA (experimental group) or olive oil (control group)—effect on surgically induced endometriosis in rabbit n = 38 [82]. | ↓ | - |
| The effect of n-3 PUFAs in a mouse endometriosis model by making full use of two types of genetically modified mice: fat-1 and 12/15-LOX KO [74]. | ↓ | - |
| Dietary fish oil supplementation and formation of endometriosis-associated adhesions in a chimeric mouse model; standard or menhaden fish oil (~40% omega-3 fatty acids)—supplemented diets for ≥2 weeks before initiation of experimental endometriosis [84]. | ↓ | - |
| The anti-inflammatory effect of EPA (n-3) compared with LA (n-6) in an endometriosis rat model [41]. | ↓ | - |
| PUFA n-3 and the establishment of endometriosis-like lesions; Wild Type (WT) and transgenic Fat-1 mice (high levels of endogenous n-3) endometriosis model; systemic host n-3 levels impact anti-inflammatory during early establishment of endometriosis [85]. | ↓ | - |
| The nutraceuticals n-6/3 and n-9/6 effect on endometriosis-associated infertility and pain; rats; fertility groups: control with endometriosis omega-6/3 (1.2 g/kg/day); omega-9/6 (1.2 g/kg/day); “pain groups”: control with endometriosis omega-6/3 (1.2 g/kg/day); omega-9/6 (1.2 g/kg/day) [86]. | ↓ | ↓ |
| Study Design | Subject | Results | |
|---|---|---|---|
| PUFAs n-3 | PUFAs n-6 | ||
| Comprehensive review [77] | Diet and dysmenorrhea among women with endometriosis; 11 trials with different designs, including a total of 1433 women. | ↓ | - |
| Double-blind, randomized, placebo-controlled trial [78] | Supplementation with i.a. PUFA n-3 (1000 mg fish oil), and pain related symptoms in women with endometriosis; n = 20, aged 12–25 years, 6 month. | ↓ | - |
| Cohort-study [79] | Dietary supplementation: 30 compositions containing i.a. linoleic acid (n-6), α-linolenic acid (n-3) n = 90 women with endometriosis; 3 months. | ↓ | ↓ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcinkowska, A.; Górnicka, M. The Role of Dietary Fats in the Development and Treatment of Endometriosis. Life 2023, 13, 654. https://doi.org/10.3390/life13030654
Marcinkowska A, Górnicka M. The Role of Dietary Fats in the Development and Treatment of Endometriosis. Life. 2023; 13(3):654. https://doi.org/10.3390/life13030654
Chicago/Turabian StyleMarcinkowska, Angelika, and Magdalena Górnicka. 2023. "The Role of Dietary Fats in the Development and Treatment of Endometriosis" Life 13, no. 3: 654. https://doi.org/10.3390/life13030654
APA StyleMarcinkowska, A., & Górnicka, M. (2023). The Role of Dietary Fats in the Development and Treatment of Endometriosis. Life, 13(3), 654. https://doi.org/10.3390/life13030654







