Effectiveness of Manual Trigger Point Therapy in Patients with Myofascial Trigger Points in the Orofacial Region—A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Data Screening
2.3. Data Extraction
2.4. Risk of Bias (Quality Assessment)
2.5. Data Synthesis
3. Results
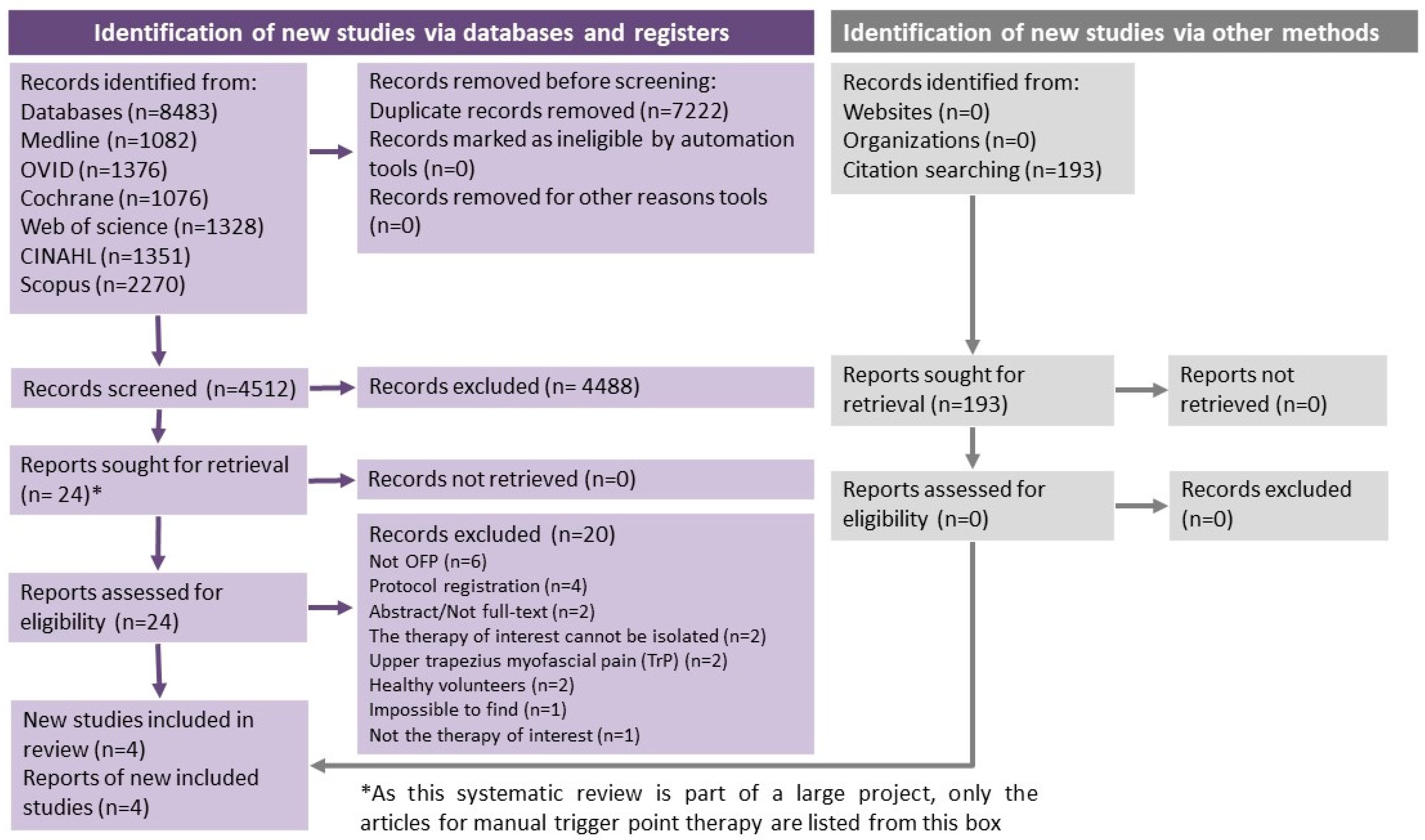
3.1. Study Selection
3.2. Study Characteristics—Synthesis of Results
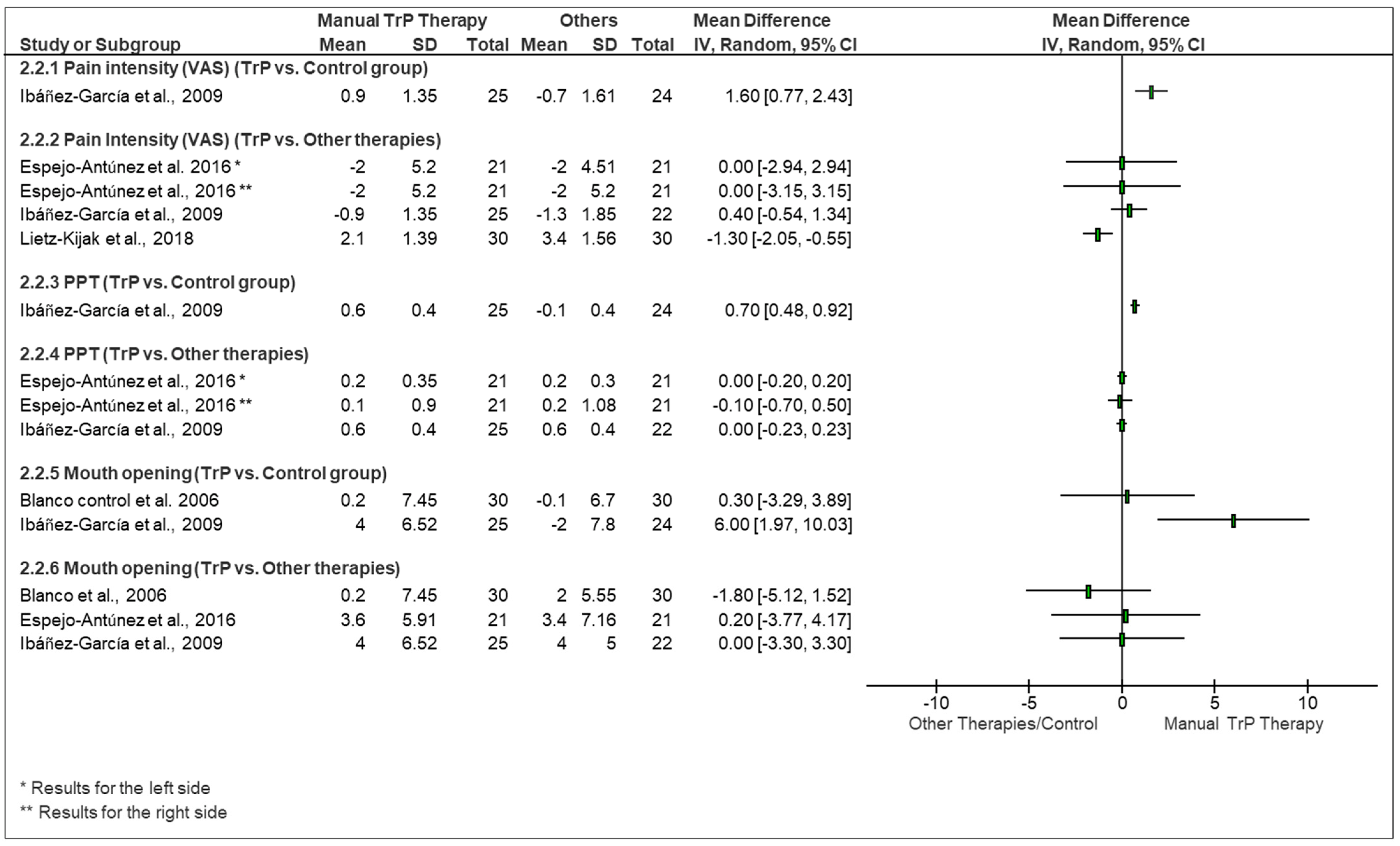
3.3. Pain Intensity
3.4. Pressure Pain Threshold
3.5. Maximum or Vertical Mouth Opening
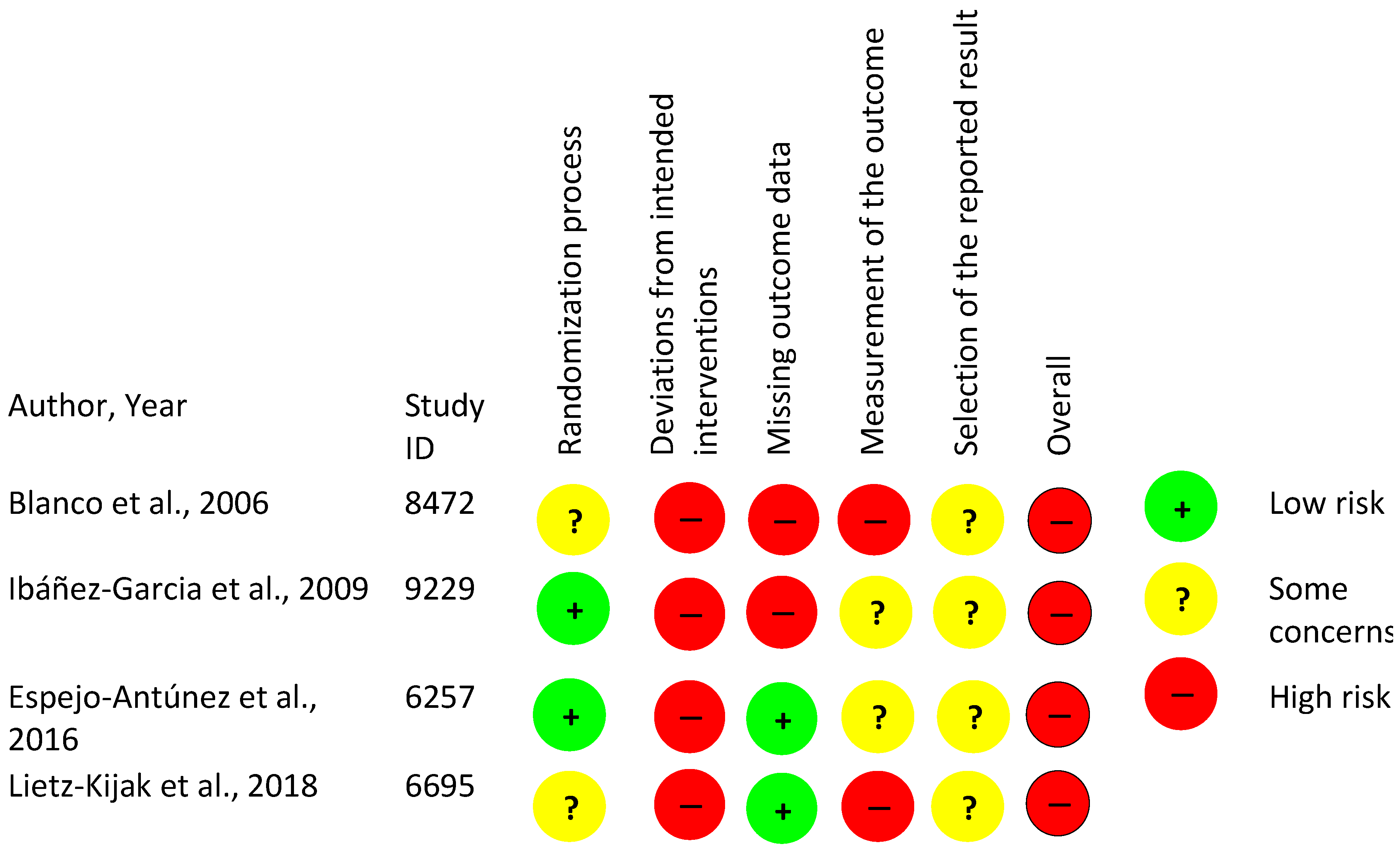
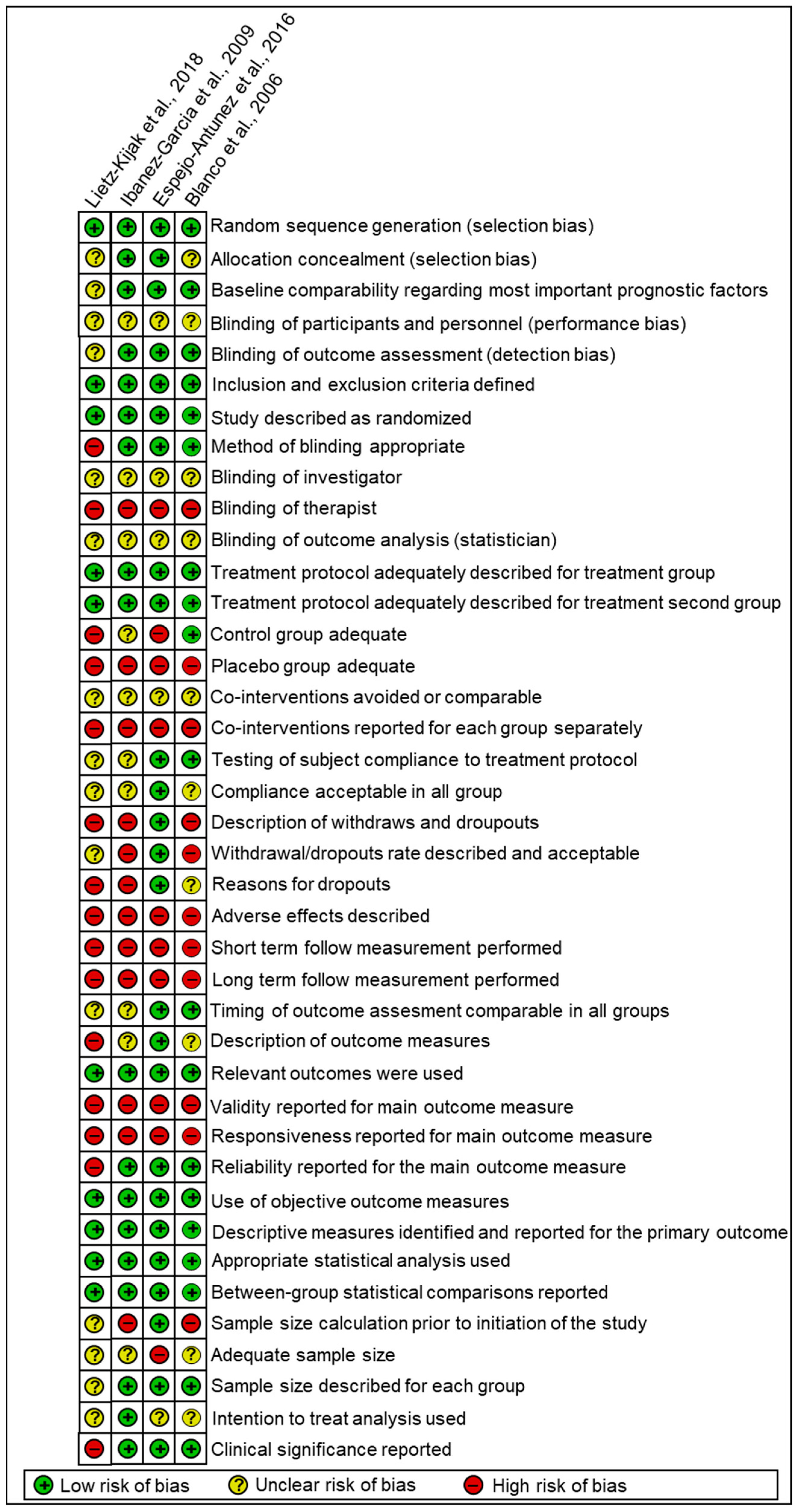
3.6. Risk of Bias of Analyzed Studies
3.7. Quality of Evidence
4. Discussion
4.1. Effectiveness of Manual Trigger Point Therapy in Comparison with Other Reviews
4.2. Methodological Biases and Evidence Quality
4.3. Future Directions
4.4. Clinical and Research Implications
4.5. Strengths and Limitations of This Review
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Search Strategies
Appendix A.1. Ovid MEDLINE(R) ALL 1946 to 20 April 2021
Appendix A.2. Embase 1974 to April 2021 (OVID Interface)
Appendix A.3. Wiley Cochrane Library Trials Database
Appendix A.4. Web of Science (Indexes=SCI-EXPANDED, SSCI, A&HCI, ESCI)
Appendix A.5. CINAHL Plus with Full Text
Appendix A.6. SCOPUS
Appendix B. Description of the Orofacial Pain Diagnosis
- 1.
- Orofacial pain associated with regional muscles: painful and nonpainful disorders affecting masticatory muscles, temporomandibular joint, and contiguous structures. These are specified according to the items below:
- (a)
- Primary myofascial pain: Pain in jaw, temple, ear or in front of ear, modified with jaw movement, function, or parafunction. It should present a familiar pain in the temporal or masseter muscles and the pain can also be referred.
- (b)
- Secondary myofascial pain: Persistent inflammation, structural changes, injury, or diseases of the nervous system. This pain can be developed, become worse or improve, according to the presumed causative disorder.
- 2.
- Orofacial pain associated with disorders of the temporomandibular joint (TMJ): condition attributed to arthralgia in the temporomandibular joint; classified as:
- (a)
- Primary TMJ arthralgia: Familiar pain in front of the ear, or in the ear confirmed by the palpation of the lateral pole or around the lateral pole, which modified with jaw movement, function, or parafunction.
- (b)
- Secondary TMJ arthralgia: TMJ pain related to inflammation, sensitization of the tissues, injury diseases of the nervous system, or structural changes.
- 3.
- Orofacial pain resembling presentations of primary headaches: pain exclusively in the facial area resembling primary headaches but without head pain; classified as:
- (a)
- Orofacial migraine: Unilateral pulsating pain with moderate or severe intensity. It can be aggravated by routine physical activity and present association with nausea and/or photophobia and phonophobia.
- (b)
- Tension-type orofacial pain: Facial muscle tension that occurs during rest and improves with voluntary muscle activity (e.g., mastication).
- 4.
- Idiopathic orofacial pain: pain without a clear causative disorder. Specified as:
- (a)
- Burning mouth syndrome: Intraoral sensation of burning and felt superficially in the oral mucosa, but the oral mucosa has a normal appearance.
- (b)
- Persistent idiopathic facial pain: Facial pain dull, aching or nagging, poorly located and without following the peripheral nerve distribution.
Appendix C. Trigger Point Therapy—Description of Techniques
Appendix D. Detailed Study Characteristics
| Study Details | Population Details | Treatment Details | Statistical Analysis Description | Limitation, Comments and Recommendations |
|---|---|---|---|---|
| First author: Cleofás Rodríguez Blanco,2006 [51] Country: Spain Language: English Trial registered: Unclear Study Design: RCT Study setting: Unclear RCT Type: Parallel Objective: To emphasize the immediate effect on MMO in performing a single treatment of latent mTrPs in the masseter muscle using a post-isometric relaxation, and the strain/counterstrain technique. Ethical approval: Yes | Population age: 25 ± 4.3 years Population sex: Mixed Population diagnosis: Latent mTrPs in the masseter muscle, either left or right sides Diagnosis tool used: Clinical Diagnoses; Simons diagnostic criteria Sampling method used: Convenience Sample size calculation: NR Total sample size: 90; 42 male, 48 female Recruitment period (start-end): NR No. of randomized groups: 3 | T1: Post-isometric relaxation technique T1 combined: Alone Duration of T1 (weeks): 0 weeks Duration of session/exposure (min): 0.55 min No. of sessions: 1 (3x exposure) Percentage of compliance: NR Compliance with treatment: Yes Application area (T1): Masseter muscles; Mouth T2: Strain/counterstrain technique T2 combined: Alone Duration T2 (weeks): unclear Duration of session/exposure (min): ~ 1.5 min, but more time was used to apply pressure on mTrP No. of sessions: 1 Application area (T2): Masseter muscles, Cervical region Manual TrP therapy concept (T2): Strain/counterstrain technique T3: Control T3 combined: Alone Duration of T3 (weeks): 0 weeks Duration of session/exposure (min): 5 min | Data Analysis description:
| Limitations/Comments:
Recommendations:
|
| First author: Jordi Ibáñez-García,2009 [52] Country: Spain Language: English Trial registered: Unclear Study Design: RCT Study setting: Unclear RCT Type: Parallel Objective: To compare the immediate effects on MMO and pressure pain sensitivity as a result of the treatment of latent mTrPs in the masseter muscle by treating with neuromuscular or strain/counterstrain technique. Ethical approval: Yes | Population age: 36 ± 14.7 years Population sex: Mixed Population diagnosis: Latent mTrPs in the masseter muscle, either left or right sides. Diagnosis tool used: Clinical Diagnoses; Simons diagnostic criteria Sampling method used: Convenience Sample size calculation: NR Total sample size: 71; 34 male, 37 female Recruitment period (start-end): NR No. of randomized groups: 3 | T1: Strain/counterstrain technique T1 combined: Alone Duration of T1 (weeks): 3 weeks Duration of session/exposure (min): 1.5 min No. of sessions: 3 Percentage of compliance: NR Compliance with treatment: NR Application area (T1): Masseter muscles, Cervical region Manual TrP therapy concept (T1): Strain/counterstrain technique T2: Neuromuscular technique T2 combined: Alone Duration of T2 (weeks): 3 weeks Duration of session/exposure (min): max. 0.666 min No. of sessions: 3 Application area (T2): Masseter muscles Manual TrP therapy concept (T2): Neuromuscular technique T3: Control T3 combined: Alone Duration of T3 (weeks): Unclear Duration of session/exposure (min): 5 min No. of sessions: 3 | Data Analysis description:
| Limitations/Comments:
Recommendations:
|
| First author: Luis Espejo-Antúnez,2016 [61] Country: Spain Language: English Trial registered: No Study Design: RCT Study setting: Unclear RCT Type: Parallel Objective: This study aimed to assess the immediate effects on MMO, pain and hamstrings extensibility by treating athletes diagnosed with TMD and hamstring shortening with either hamstring stretching alone or combined with ischemic compression of the masseter muscle. Ethical approval: Yes | Population age: 21.2 ± 1.6 years Population sex: Mixed Population diagnosis: Myogenic TMD and trigger points Diagnosis tool used: RDC/TMD, Clinical Diagnoses Duration of diagnosis: 6 months chronicity of pain Population other conditions: Hamstring shortening Population other characteristics: Participants with regular sports practice (≥5 h per week), without previous hamstrings injury Sampling method used: Convenience Sample size calculation: Yes Total sample size: 42; 14 male, 28 female Total sample size start-finish: NR Recruitment period (start-end): NR No. of randomized groups: 2 | T1: Proprioceptive neuromuscular facilitation technique T1 combined: Alone Duration of T1 (weeks): 0 weeks Duration of session/exposure (min): 1.6 min No. of sessions: 1 Percentage of compliance: 100% Compliance with treatment: Yes Application area (T1): Hamstrings T2: Hamstring stretching + ischemic compression technique T2 combined: Combined T2 how many therapies combined: 2 T2 which therapies are combined: Ischemic compression and proprioceptive neuromuscular facilitation technique Duration of T2 (weeks): 0 weeks Duration of session/exposure (min): 3.1 min No. of sessions: 1 Percentage of compliance: 100% Compliance with treatment: Yes Application area (T2): Masseter muscles and hamstrings Manual TrP therapy concept (T2): Ischemic compression | Data Analysis description:
| Limitations/Comments:
Recommendations:
|
| First author: Danuta Lietz-Kijak, 2018 [17] Country: Poland Language: English Trial registered: No Study Design: RCT Study setting: NR RCT Type: Parallel Objective: This study aimed at the evaluation of the effect on pain in patients diagnosed with TMD by treatment with kinesiotaping and trigger points inactivation. Ethical approval: Yes Trial registered: No | Population age: 25.87 ± 4.86 years Population sex: Mixed Population diagnosis: Latent trigger points and myogenic TMD Diagnosis tool used: RDC/TMD Population other characteristics: Diagnosed with an excessive strain of masseter muscles and muscular pain, without limitations in the movements of the mandible and disc derangement and joint pain Sampling method used: Convenience Sample size calculation: No Total sample size: 60; 29 male, 31 female Recruitment period (start-end): 2015–2016 No. of randomized groups: 2 | T1: Kinesiotaping T1 combined: Alone Duration of T1 (weeks): 0.71 weeks Duration of session/exposure (min): 7.200 min No. of sessions: 1 Percentage of compliance: NR Compliance with treatment: NR Application area (T1): Masseter muscles T2: Ischemic compression T2 combined: Alone Duration of T2 (weeks): 0.71 weeks No. of sessions: 3 (on the first, third and fifth day of treatment) Application area (T2): Masseter muscles Manual TrP therapy concept (T2): Ischemic compression | Data Analysis Description:
| Limitations/Comments:
Recommendations:
|
Appendix E. Risk of Bias—Compiled Set of Items Table
| Items | Blanco et al., 2006 [51] | Ibáñez García et al., 2009 [52] | Espejo Antúnez et al., 2016 [53] | Lietz et al., 2018 [17] | Total | |
|---|---|---|---|---|---|---|
| Consensus | Consensus | Consensus | Consensus | |||
| Inclusion and exclusion criteria clearly defined consensus | Yes | Yes | Yes | Yes | 4 | 100% |
| Study described as randomized consensus | Yes | Yes | Yes | Yes | 4 | 100% |
| Method of randomization described and appropriate consensus | Yes | Yes | Yes | Unclear | 3 | 75% |
| Method of randomization concealed Consensus | Unclear | Yes | Yes | Unclear | 2 | 50% |
| Baseline comparability regarding the most important prognostic indicators consensus | Yes | Yes | Yes | Unclear | 3 | 75% |
| Study described as double-blind consensus | No | No | No | Unclear | 0 | 0% |
| Method of blinding appropriate consensus | Yes | Yes | Yes | No | 3 | 75% |
| Blinding investigator consensus | Unclear | Unclear | Unclear | Unclear | 0 | 0% |
| Blinding of assessors’ consensus | Yes | Yes | Yes | Unclear | 3 | 75% |
| Blinding of participants consensus | Unclear | Unclear | Unclear | Unclear | 0 | 0% |
| Blinding of therapist consensus | No | No | No | No | 0 | 0% |
| Blinding of outcomes analysis (statistician) consensus | Unclear | Unclear | Unclear | Unclear | 0 | 0% |
| Treatment protocol adequately described for treatment group consensus | Yes | Yes | Yes | Yes | 4 | 100% |
| Treatment protocol adequately described for treatment second group consensus | Yes | Yes | Yes | Yes | 4 | 100% |
| Control group adequate consensus | Yes | Unclear | No | No | 1 | 25% |
| Placebo group adequate consensus | No | No | No | No | 0 | 0% |
| Co-interventions avoided or comparable consensus | Unclear | Unclear | Unclear | Unclear | 0 | 0% |
| Co-interventions reported for each group separately consensus | No | No | No | No | 0 | 0% |
| Testing of subject compliance to treatment protocol consensus | Yes | Unclear | Yes | Unclear | 2 | 50% |
| Compliance acceptable in all group consensus | Unclear | Unclear | Yes | Unclear | 1 | 25% |
| Description of withdraws and dropout’s consensus | No | No | Yes | No | 1 | 25% |
| Withdrawal/dropouts rate described and acceptable consensus | No | No | Yes | Unclear | 1 | 25% |
| Reasons for dropouts consensus | Unclear | No | Yes | No | 1 | 25% |
| Adverse effects described consensus | No | No | No | No | 0 | 0% |
| Short term follow measurement performed consensus | No | No | No | No | 0 | 0% |
| Long term follow measurement performed consensus | No | No | No | No | 0 | 0% |
| The timing of the outcome assessment was comparable in all group’s consensus | Yes | Unclear | Yes | Unclear | 2 | 50% |
| Description of outcome measures consensus | Unclear | Unclear | Yes | No | 1 | 25% |
| Relevant outcomes were used consensus | Yes | Yes | Yes | Yes | 4 | 100% |
| Validity reported for the main outcome measure consensus | No | No | No | No | 0 | 0% |
| Responsiveness reported for the main outcome measure consensus | No | No | No | No | 0 | 0% |
| Reliability reported for the main outcome measure consensus | Yes | Yes | Yes | No | 3 | 75% |
| Use of objective outcome measures consensus | Yes | Yes | Yes | Yes | 4 | 100% |
| Descriptive measures identified and reported for the primary outcome consensus | Yes | Yes | Yes | Yes | 4 | 100% |
| Appropriate statistical analysis used consensus | Yes | Yes | Yes | Yes | 4 | 100% |
| Between-group statistical comparisons reported Consensus | Yes | Yes | Yes | Yes | 4 | 100% |
| Sample size calculation prior to initiation of the study consensus | No | No | Yes | Unclear | 1 | 25% |
| Adequate sample size consensus | Unclear | Unclear | No | Unclear | 0 | 0% |
| Sample size described for each group consensus | Yes | Yes | Yes | Unclear | 3 | 75% |
| Intention to treat analysis used consensus | Unclear | Yes | Unclear | Unclear | 1 | 25% |
| Clinical significance reported consensus | Yes | Yes | Yes | No | 3 | 75% |
| Number of items accomplished/total of applicable items | 18/40 | 17/40 | 24/40 | 8/40 | ||
| Number of items applicable | 40 | 40 | 40 | 40 | ||
| % of items accomplished | 45% | 42.50% | 60% | 20% | ||
| Risk of Bias Tool Assessment | High | High | High | High |
References
- Li, L.; Stoop, R.; Clijsen, R.; Hohenauer, E.; Fernández-de-Las-Peñas, C.; Huang, Q.; Barbero, M. Criteria Used for the Diagnosis of Myofascial Trigger Points in Clinical Trials on Physical Therapy: Updated Systematic Review. Clin. J. Pain 2020, 36, 955–967. [Google Scholar] [CrossRef]
- Travell, J.G.; Simons, D.G.; Simons, L.S. Myofascial Pain and Dysfunction: The Trigger Point Manual: Vol. 1: Upper Half of Body; Williams & Wilkins: Baltimore, MD, USA, 1999. [Google Scholar]
- International Classification of Orofacial Pain, 1st edition (ICOP). Cephalalgia 2020, 40, 129–221. [CrossRef] [PubMed]
- Romero-Reyes, M.; Uyanik, J. Orofacial pain management: Current perspectives. J. Pain Res. 2014, 7, 99. [Google Scholar] [CrossRef] [PubMed]
- Jin, L.J.; Lamster, I.; Greenspan, J.; Pitts, N.; Scully, C.; Warnakulasuriya, S. Global burden of oral diseases: Emerging concepts, management and interplay with systemic health. Oral Dis. 2016, 22, 609–619. [Google Scholar] [CrossRef]
- LeResche, L. Epidemiology of temporomandibular disorders: Implications for the investigation of etiologic factors. Crit. Rev. Oral Biol. Med. 1997, 8, 291–305. [Google Scholar] [CrossRef] [PubMed]
- Kohlmann, T. Epidemiologie orofazialer Schmerzen. Der Schmerz 2002, 16, 339–345. [Google Scholar] [CrossRef]
- Manfredini, D.; Guarda-Nardini, L.; Winocur, E.; Piccotti, F.; Ahlberg, J.; Lobbezoo, F. Research diagnostic criteria for temporomandibular disorders: A systematic review of axis I epidemiologic findings. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2011, 112, 453–462. [Google Scholar] [CrossRef]
- Vier, C.; de Almeida, M.B.; Neves, M.L.; Dos Santos AR, S.; Bracht, M.A. The effectiveness of dry needling for patients with orofacial pain associated with temporomandibular dysfunction: A systematic review and meta-analysis. Braz. J. Phys. Ther. 2019, 23, 3–11. [Google Scholar] [CrossRef]
- Leeuw, R.D.; Klasser, G.D.; American Academy of Orofacial, P. Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management; Quintessence Publishing: Batavia, IL, USA, 2018. [Google Scholar]
- Ferrillo, M.; Ammendolia, A.; Paduano, S.; Calafiore, D.; Marotta, N.; Migliario, M.; Fortunato, L.; Giudice, A.; Michelotti, A.; de Sire, A. Efficacy of rehabilitation on reducing pain in muscle-related temporomandibular disorders: A systematic review and meta-analysis of randomized controlled trials. J. Back Musculoskelet. Rehabil. 2022, 35, 921–936. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Magee, D.; Gross, D. Effects of exercise therapy on endogenous pain-relieving peptides in musculoskeletal pain: A systematic review. Clin. J. Pain 2011, 27, 365–374. [Google Scholar]
- Armijo-Olivo, S.; Pitance, L.; Singh, V.; Neto, F.; Thie, N.; Michelotti, A. Effectiveness of manual therapy and therapeutic exercise for temporomandibular disorders: Systematic review and meta-analysis. Phys. Ther. 2016, 96, 9–25. [Google Scholar] [CrossRef] [PubMed]
- Calixtre, L.; Moreira, R.F.C.; Franchini, G.H.; Alburquerque-Sendín, F.; Oliveira, A.B. Manual therapy for the management of pain and limited range of motion in subjects with signs and symptoms of temporomandibular disorder: A systematic review of randomised controlled trials. J. Oral Rehabil. 2015, 42, 847–861. [Google Scholar] [CrossRef] [PubMed]
- Brantingham, J.W.; Cassa, T.K.; Bonnefin, D.; Pribicevic, M.; Robb, A.; Pollard, H.; Tong, V.; Korporaal, C. Manipulative and multimodal therapy for upper extremity and temporomandibular disorders: A systematic review. J. Manip. Physiol. 2013, 36, 143–201. [Google Scholar] [CrossRef]
- Paço, M.; Peleteiro, B.; Duarte, J.; Pinho, T. The Effectiveness of Physiotherapy in the Management of Temporomandibular Disorders: A Systematic Review and Meta-analysis. J. Oral Facial Pain Headache 2016, 30, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Lietz-Kijak, D.; Kopacz, Ł.; Ardan, R.; Grzegocka, M.; Kijak, E. Assessment of the short-term effectiveness of kinesiotaping and trigger points release used in functional disorders of the masticatory muscles. Pain Res. Manag. 2018, 2018, 5464985. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.C.; Duarte Moura, D.M.; Da Silva, L.G.D.; De Almeida, E.O.; Barbosa, G.A.S. Acupuncture in Temporomandibular Disorder Myofascial Pain Treatment: A Systematic Review. J. Oral Facial Pain Headache 2017, 31, 225–232. [Google Scholar] [CrossRef]
- Díaz-Sáez, M.; Sáenz-Jiménez, C.; Villafañe, J.H.; Paris-Alemany, A.; La Touche, R. Hypoalgesic and Motor Effects of Neural Mobilisation versus Soft-Tissue Interventions in Experimental Craniofacial Hyperalgesia: A Single-Blinded Randomised Controlled Trial. J. Clin. Med. 2021, 10, 4434. [Google Scholar] [CrossRef]
- Sajedi, S.M.; Abbasi, F.; Asnaashari, M.; Jafarian, A.A. Comparative Efficacy of Low-Level Laser Acupuncture and Cupping for Treatment of Patients with Myofascial Pain Dysfunction Syndrome: A Double-blinded, Randomized Clinical Trial: Comparison of the Effects of LLL Acupuncture and Cupping. Galen Med. J. 2022, 11, 1–13. [Google Scholar] [CrossRef]
- Gautschi, R.; Böhni, U. Das myofasziale Schmerzsyndrom. Man. Med. 2014, 52, 203–213. [Google Scholar] [CrossRef]
- Martins, W.R.; Blasczyk, J.C.; de Oliveira, M.A.F.; Gonçalves, K.F.L.; Bonini-Rocha, A.C.; Dugailly, P.-M.; de Oliveira, R.J. Efficacy of musculoskeletal manual approach in the treatment of temporomandibular joint disorder: A systematic review with meta-analysis. Man. Ther. 2016, 21, 10–17. [Google Scholar] [CrossRef]
- Denneny, D.; Frawley, H.C.; Petersen, K.; McLoughlin, R.; Brook, S.; Hassan, S.; Williams, A.C. Trigger point manual therapy for the treatment of chronic noncancer pain in adults: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2019, 100, 562–577. [Google Scholar] [CrossRef]
- de las Peñas, C.F.; Campo, M.S.; Fernandez-Carnero, J.; Palge, J.C.M. Manual therapies in myofascial trigger point treatment: A systematic review. J. Bodyw. Mov. Ther. 2005, 9, 27–34. [Google Scholar] [CrossRef]
- Falsiroli Maistrello, L.; Geri, T.; Gianola, S.; Zaninetti, M.; Testa, M. Effectiveness of trigger point manual treatment on the frequency, intensity and duration of attacks in primary headaches: A systematic review and meta-analysis of randomized controlled trials. Front. Neurol. 2018, 9, 254. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Glanville, J.M.; Lefebvre, C.; Miles, J.N.V.; Camosso-Stefinovic, J. How to identify randomized controlled trials in MEDLINE: Ten years on. J. Med. Libr. Assoc. 2006, 94, 130. [Google Scholar]
- McNeely, M.L.; Olivo, S.A.; Magee, D. A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys. Ther. 2006, 86, 710–725. [Google Scholar] [CrossRef]
- Travell, J.G.; Simons, D.G. Myofascial Pain and Dysfunction. The Trigger Point Manual; Williams & Wilkins: Baltimore, MD, USA, 1983; Volume 1. [Google Scholar]
- Simons, D.G. Understanding effective treatments of myofascial trigger points. J. Bodyw. Mov. Ther. 2002, 6, 81–88. [Google Scholar] [CrossRef]
- Ajimsha, M.; Al-Mudahka, N.; Al-Madzhar, J. Effectiveness of myofascial release: Systematic review of randomized controlled trials. J. Bodyw. Mov. Ther. 2015, 19, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Gautschi, R. Manuelle Triggerpunkt-Therapie: Myofasziale Schmerzen und Funktionsstörungen Erkennen, Verstehen und Behandeln; Thalia: Berlin, Germany, 2016. [Google Scholar]
- Page, P. Current concepts in muscle stretching for exercise and rehabilitation. Int. J. Sport. Phys. Ther. 2012, 7, 109. [Google Scholar]
- Mandroukas, A.; Vamvakoudis, E.; Metaxas, T.; Papadopoulos, P.; Kotoglou, K.; Stefanidis, P.; Christoulas, K.; Kyparos, A.; Mandroukas, K. Acute partial passive stretching increases range of motion and muscle strength. J. Sport. Med. Phys. Fit. 2014, 54, 289–297. [Google Scholar]
- Bordoni, B.; Marelli, F. The fascial system and exercise intolerance in patients with chronic heart failure: Hypothesis of osteopathic treatment. J. Multidiscip. Healthc. 2015, 8, 489. [Google Scholar] [CrossRef]
- Dardzinski, J.; Ostrov, B.; Hamann, L. Successful Use of a Strain and Counterstrain Technique with Physical Therapy: Myofascial Pain Unresponsive to Standard Treatment. JCR J. Clin. Rheumatol. 2000, 6, 169–174. [Google Scholar] [CrossRef]
- Jones, L.N. Strain and Counterstrain; American Academy of Osteopathy: Newark, OH, USA, 1981. [Google Scholar]
- Maquet, D.; Croisier, J.-L.; Demoulin, C.; Crielaard, J.-M. Pressure pain thresholds of tender point sites in patients with fibromyalgia and in healthy controls. Eur. J. Pain 2004, 8, 111–117. [Google Scholar] [CrossRef]
- Hong, C.-Z. Algometry in evaluation of trigger points and referred pain. J. Musculoskelet. Pain 1998, 6, 47–59. [Google Scholar] [CrossRef]
- Svechtarov, V.; Croisier, J.-L.; Demoulin, C.; Crielaard, J.-M. Mandibular range of motion and its relation to temporomandibular disorders. Scr. Sci. Med. Dent. 2015, 1, 21–26. [Google Scholar] [CrossRef]
- Higgins, J.P.; Sterne, J.A.; Savovic, J.; Page, M.J.; Hróbjartsson, A.; Boutron, I.; Reeves, B.; Eldridge, S. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst. Rev. 2016, 10, 29–31. [Google Scholar]
- Sterne, J.A.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Armijo-Olivo, S.; Ospina, M.; da Costa, B.R.; Egger, M.; Saltaji, H.; Fuentes, J.; Ha, C.; Cummings, G.G. Poor reliability between Cochrane reviewers and blinded external reviewers when applying the Cochrane risk of bias tool in physical therapy trials. PloS ONE 2014, 9, e96920. [Google Scholar] [CrossRef]
- Olivo, S.A.; Macedo, L.; Gadotti, I.C.; Fuentes, J.; Stanton, T.; Magee, D.J. Scales to assess the quality of randomized controlled trials: A systematic review. Phys. Ther. 2008, 88, 156–175. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, J.P.; Olivo, S.A.; Magee, D.J.; Gross, D.P. Effectiveness of interferential current therapy in the management of musculoskeletal pain: A systematic review and meta-analysis. Phys. Ther. 2010, 90, 1219–1238. [Google Scholar] [CrossRef]
- Calixtre, L.B.; Olivetira, A.B.; Alburquerque-Sendín, F.; Armijo-Olivo, S. What is the minimal important difference of pain intensity, mandibular function, and headache impact in patients with temporomandibular disorders? Clinical significance analysis of a randomized controlled trial. Musculoskelet. Sci. Pract. 2020, 46, 102108. [Google Scholar] [CrossRef] [PubMed]
- Kropmans, T.J.; Dijkstra, P.U.; Stegenga, B.; Stewart, R.; De Bont LG, M. Smallest detectable difference in outcome variables related to painful restriction of the temporomandibular joint. J. Dent. Res. 1999, 78, 784–789. [Google Scholar] [CrossRef]
- Fuentes, C.J.; Armijo-Olivo, S.; Magee, D.J.; Gross, D.P. A preliminary investigation into the effects of active interferential current therapy and placebo on pressure pain sensitivity: A random crossover placebo controlled study. Physiotherapy 2011, 97, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Blanco, C.R.; Peñas, C.F.D.L.; Xumet, J.E.H.; Algaba, C.P.; Rabadán, M.F.; de la Quintana, M.C.L. Changes in active mouth opening following a single treatment of latent myofascial trigger points in the masseter muscle involving post-isometric relaxation or strain/counterstrain. J. Bodyw. Mov. Ther. 2006, 10, 197–205. [Google Scholar] [CrossRef]
- Ibáñez-García, J.; Alburquerque-Sendín, F.; Rodríguez-Blanco, C.; Girao, D.; Atienza-Meseguer, A.; Planella-Abella, S.; Fernández-de-Las Peñas, C. Changes in masseter muscle trigger points following strain-counterstrain or neuro-muscular technique. J. Bodyw. Mov. Ther. 2009, 13, 2–10. [Google Scholar] [CrossRef]
- Espejo-Antúnez, L.; Castro-Valenzuela, E.; Ribeiro, F.; Albornoz-Cabello, M.; Silva, A.; Rodríguez-Mansilla, J. Immediate effects of hamstring stretching alone or combined with ischemic compression of the masseter muscle on hamstrings extensibility, active mouth opening and pain in athletes with temporomandibular dysfunction. J. Bodyw. Mov. Ther. 2016, 20, 579–587. [Google Scholar] [CrossRef]
- Dworkin, S.F. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and classification, critique. J. Orofac. Pain 1992, 6, 302–355. [Google Scholar]
- D’Ambrogio, K.J.; Roth, G.B. Positional Release Therapy: Assessment & Treatment of Musculoskeletal Dysfunction; Mosby Incorporated: Maryland Heights, MI, USA, 1997. [Google Scholar]
- Vernon, H.; Schneider, M. Chiropractic management of myofascial trigger points and myofascial pain syndrome: A systematic review of the literature. J. Manip. Physiol. Ther. 2009, 32, 14–24. [Google Scholar] [CrossRef]
- Hanten, W.P.; Olson, S.L.; Butts, N.L.; Nowicki, A.L. Effectiveness of a home program of ischemic pressure followed by sustained stretch for treatment of myofascial trigger points. Phys. Ther. 2000, 80, 997–1003. [Google Scholar] [CrossRef]
- Hou, C.-R.; Tsai, L.-C.; Cheng, K.-F.; Chung, K.-C.; Hong, C.-Z. Immediate effects of various physical therapeutic modalities on cervical myofascial pain and trigger-point sensitivity. Arch. Phys. Med. Rehabil. 2002, 83, 1406–1414. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Alonso-Blanco, C.; Fernández-Carnero, J.; Miangolarra-Page, J.C. The immediate effect of ischemic compression technique and transverse friction massage on tenderness of active and latent myofascial trigger points: A pilot study. J. Bodyw. Mov. Ther. 2006, 10, 3–9. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Mohamad, N.; de Oliveira-Souza AI, S.; de Castro-Carletti, E.M.; Ballenberger, N.; Fuentes, J. Performance, Detection, Contamination, Compliance, and Cointervention Biases in Rehabilitation Research: What Are They and How Can They Affect the Results of Randomized Controlled Trials? Basic Information for Junior Researchers and Clinicians. Am. J. Phys. Med. Rehabil. 2022, 101, 864–878. [Google Scholar] [CrossRef] [PubMed]
- Espejo-Antúnez, L.; Tejeda, J.F.-H.; Albornoz-Cabello, M.; Rodríguez-Mansilla, J.; De-La-Cruz-Torres, B.; Ribeiro, F.; Silva, A.G. Dry needling in the management of myofascial trigger points: A systematic review of randomized controlled trials. Complement. Ther. Med. 2017, 33, 46–57. [Google Scholar] [CrossRef]
| Study (Year) | Intervention vs. Comparison Group(s) | Outcome Measure—Measure Tool | Results between Groups MD [95% CI] | Results between Groups p Value and Clinical Significance Assessment | Conclusion |
|---|---|---|---|---|---|
| Blanco et al. (2006) [51] | SC (masseter) vs.PIR (masseter) vs. Control: no therapy | MMO (mm)—NR | MMO: SC vs. PIR −1.80 mm [−5.12, 1.52] SC vs. CO 0.30 mm [−3.29, 3.89] | MMO: SC vs. PIR (p = 0.4090; no significant difference between groups; NCS) SC vs. CO (p = 0.84, no significant difference between groups; NCS) | For participants with latent mTrPs in the masseter muscle, the post-isometric relaxation technique showed a greater effect on active mouth opening than the strain/counterstrain technique. |
| Ibáñez-García et al. (2009) [52] | SC (masseter) vs. NT (masseter) vs. Control: no therapy | Pain intensity (0–10 cm)—VAS PPT (kg/cm2)—mechanical pressure algometer MMO (mm)—NR | Pain intensity: SC vs. NT 0.40 cm [−0.54, 1.34] SC vs. CO 1.60 cm [0.77, 2.43] PPT: SC vs. NT 0.0 kg/cm2 [−0.23, 0.23] SC vs. CO 0.70 kg/cm2 [0.48, 0.92] MMO: SC vs. NT 0.00 mm [−3.30, 3.30] SC vs. CO 6.00 mm [1.97, 10.03] | Pain intensity: SC vs. NT (p = 0.9, no significant difference between groups; NCS) SC vs. CO (p <0.001, significant difference favoring SC; PCSR) PPT: SC vs. NT (p = 0.9, no significant difference between groups; NCS) SC vs. CO (p < 0.001, significant difference favoring SC; NCS) MMO: SC vs. NT (p = 0.9, no significant difference between groups; NCS) SC vs. CO (p < 0.001, significant difference favoring SC; CSR) | The neuromuscular or strain/ counterstrain technique showed in the results’ increased PPTs, increased active mouth opening, and decreased local pain by pressure over latent myofascial TrPs in the masseter muscle. For both intervention groups, the large effect sizes suggest a strong clinical effect, while the effect size of the control was small. |
| Espejo-Antúnez et al. (2016) [53] | IC (masseter) + HS (hamstrings) vs. HS (hamstrings) | Pain intensity (0–10 cm) – VAS PPT (kg/cm2) – mechanical pressure algometer MMO/VMO (mm) – calibrated caliper ROM (degree °) – computer analysis of photographs | Pain intensity: HS vs. HS+IC_R 0.00 cm [−3.15, 3.15] HS vs. HS+IC_L 0.00 cm [−2.94, 2.94] PPT: HS vs. HS+IC_R −0.10 kg/cm2 [−0.70, 0.50] HS vs. HS+IC_L 0.00 kg/cm2 [−0.20, 0.20] MMO/VMO: HS vs. HS+IC 0.20 mm [−3.77, 4.17] | Pain intensity: HS vs. HS+IC_R (p = 1.0; no significant difference between groups; NCS) HS vs. HS+IC_L (p = 1.0; no significant difference between groups; NCS) PPT: HS vs. HS+IC_R (p = 0.7616; no significant difference between groups; NCS) HS vs. HS+IC_L (p = 1.0; no significant difference between groups; NCS) MMO/VMO: HS vs. HS+IC (p = 0.4708; no significant difference between groups; NCS) | Both groups showed an increased hamstrings extensibility, active mouth opening, and pressure pain threshold, as well as decreased pain intensity. Adding ischemic compression did not result in further improvements in hamstrings extensibility or clinical features of TMD. |
| Lietz-Kijak et al. (2018) [17] | IC (masseter) vs. KT (masseter) | Pain intensity (0–10 cm) – VAS | Pain intensity: KT vs. IC −1.30 cm [−2.05, −0.55] | Pain intensity: KT vs. IC (p < 0.001; significant difference favoring KT; PCSR) | Significant analgesic effects were achieved by kinesiotaping (KT) and TrP inactivation for the treatment of painful forms of functional disorders of the masticatory muscles; however, more beneficial results were observed in the KT group. |
| Quality Assessment | Summary of Findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of Patients | Effect | |||||||||
| Comparisons | No. of Studies (Design; Time of measurement) | Risk of Bias | Inconsis-tency | Indirectness | Imprecision | Publication Bias | Patients in Tx group | Patients in Comparison/ Control Group | Estimate (MD) [95% CI] | Quality |
| Pain Intensity (assessed with VAS: scale from 0 – 10 cm)—Manual TrP therapy vs. Control | ||||||||||
| Strain/Counterstrain technique vs. Control (no treatment) | 1 RCT [52]; right after treatment | Very Serious (a) | NA | Serious (d) | Serious (e) | Undetected (f) | 25 | 24 | MD = 1.60 cm [0.77, 2.43] | Low |
| Pain Intensity (assessed with VAS: scale from 0 – 10 cm)—Manual TrP therapy vs. Other therapies | ||||||||||
| Hamstring stretching + Ischemic compression vs. Hamstring stretching (left) | 1 RCT [53]; right after treatment | Very Serious (a) | NA | No serious (c) | Serious (e) | Undetected (f) | 21 | 21 | MD = 0.00 cm [−2.94, 2.94] | Low |
| Hamstring stretching + Ischemic compression vs. Hamstring stretching (right) | 1 RCT [53]; right after treatment | Very Serious (a) | NA | No serious (c) | Serious (e) | Undetected (f) | 21 | 21 | MD = 0.00 cm [−3.15, 3.15] | Low |
| Strain/Counterstrain technique vs. Neuromuscular technique | 1 RCT [52]; right after treatment | Very Serious (a) | NA | Serious (d) | Serious (e) | Undetected (f) | 22 | 22 | MD = 0.40 cm [−0.54, 1.34] | Low |
| Ischemic compression vs. Kinesio taping | 1 RCT [17]; right after treatment | Very Serious (a) | NA | No serious (c) | Serious (e) | Undetected (f) | 30 | 30 | MD = −1.30 cm [−2.05, −0.55] | Low |
| Pressure Pain Threshold (assessed with pressure algometer: kg/cm2)—Manual TrP therapy vs. Control | ||||||||||
| Strain/Counterstrain technique vs. Control (no treatment) | 1 RCT [52]; right after treatment | Very Serious (a) | NA | Serious (d) | Serious (e) | Undetected (f) | 25 | 24 | MD = 0.70 kg/cm2 [0.48, 0.92] | Low |
| Pressure Pain Threshold (assessed with pressure algometer: kg/cm2)—Manual TrP therapy vs. Other therapies | ||||||||||
| Hamstring stretching + Ischemic compression vs. Hamstring stretching (left) | 1 RCT [53]; right after treatment | Very Serious (a) | NA | No Serious (c) | Serious (e) | Undetected (f) | 21 | 21 | MD = 0.00 kg/cm2 [−0.20, 0.20] | Low |
| Hamstring stretching + Ischemic compression vs. Hamstring stretching (right) | 1 RCT [53]; right after treatment | Very Serious (a) | NA | No Serious (c) | Serious (e) | Undetected (f) | 21 | 21 | MD = −0.10 kg/cm2 [−0.70, 0.50] | Low |
| Strain/Counterstrain technique vs. Neuromuscular technique | 1 RCT [52]; right after treatment | Very Serious (a) | NA | Serious (d) | Serious (e) | Undetected (f) | 25 | 22 | MD = 0.00 kg/cm2 [−0.23, 0.23] | Low |
| Mouth Opening (assessed with calibrated caliper (Blanco et al.): scale in mm; in Ibáñez-García: NR: scale in mm) – Manual TrP therapy vs. Control | ||||||||||
| Strain/Counterstrain technique vs. Control (no treatment) | 1 RCT [51]; right after treatment | Very Serious (a) | Very serious (b) | Serious (d) | Serious (e) | Undetected (f) | 30 | 30 | Total MD = 0.30 mm [−3.29, 3.89] | Very Low |
| Strain/Counterstrain technique vs. Control (no treatment) | 1 RCT [52]; right after treatment | Very Serious (a) | Very serious (b) | Serious (d) | Serious (e) | Undetected (f) | 30 | 30 | Total MD = 6.00 mm [1.97, 10.03] | Very Low |
| Mouth Opening (assessed with calibrated caliper (Espejo-Antúnez et al.): scale in mm; in Ibáñez-García: NR: scale in mm)—Manual TrP therapy vs. Other therapies | ||||||||||
| Strain/Counterstrain technique vs. post-isometric relax. | 1 RCT [51]; right after treatment | Very Serious (a) | NA | Serious (d) | Serious (e) | Undetected (f) | 30 | 30 | MD = −1.80 mm [−5.12, 1.52] | Very Low |
| Hamstring stretching + Ischemic comp. vs. Hamstring stretching | 1 RCT [53]; right after treatment | Very Serious (a) | NA | No serious (c) | Serious (e) | Undetected (f) | 21 | 21 | MD = 0.20 mm [−3.77, 4.17] | Low |
| Strain/Counterstrain technique vs. Neuromuscular technique | 1 RCT [52]; right after treatment | Very Serious (a) | NA | Serious (d) | Serious (e) | Undetected (f) | 25 | 22 | MD = 0.00 mm [−3.30, 3.30] | Very Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Müggenborg, F.; de Castro Carletti, E.M.; Dennett, L.; de Oliveira-Souza, A.I.S.; Mohamad, N.; Licht, G.; von Piekartz, H.; Armijo-Olivo, S. Effectiveness of Manual Trigger Point Therapy in Patients with Myofascial Trigger Points in the Orofacial Region—A Systematic Review. Life 2023, 13, 336. https://doi.org/10.3390/life13020336
Müggenborg F, de Castro Carletti EM, Dennett L, de Oliveira-Souza AIS, Mohamad N, Licht G, von Piekartz H, Armijo-Olivo S. Effectiveness of Manual Trigger Point Therapy in Patients with Myofascial Trigger Points in the Orofacial Region—A Systematic Review. Life. 2023; 13(2):336. https://doi.org/10.3390/life13020336
Chicago/Turabian StyleMüggenborg, Frauke, Ester Moreira de Castro Carletti, Liz Dennett, Ana Izabela Sobral de Oliveira-Souza, Norazlin Mohamad, Gunnar Licht, Harry von Piekartz, and Susan Armijo-Olivo. 2023. "Effectiveness of Manual Trigger Point Therapy in Patients with Myofascial Trigger Points in the Orofacial Region—A Systematic Review" Life 13, no. 2: 336. https://doi.org/10.3390/life13020336
APA StyleMüggenborg, F., de Castro Carletti, E. M., Dennett, L., de Oliveira-Souza, A. I. S., Mohamad, N., Licht, G., von Piekartz, H., & Armijo-Olivo, S. (2023). Effectiveness of Manual Trigger Point Therapy in Patients with Myofascial Trigger Points in the Orofacial Region—A Systematic Review. Life, 13(2), 336. https://doi.org/10.3390/life13020336







