Personalized Nasal Protective Devices: Importance and Perspectives
Abstract
:1. Introduction
2. The Importance of Individual Nasal Filters in Modern Air Quality Management
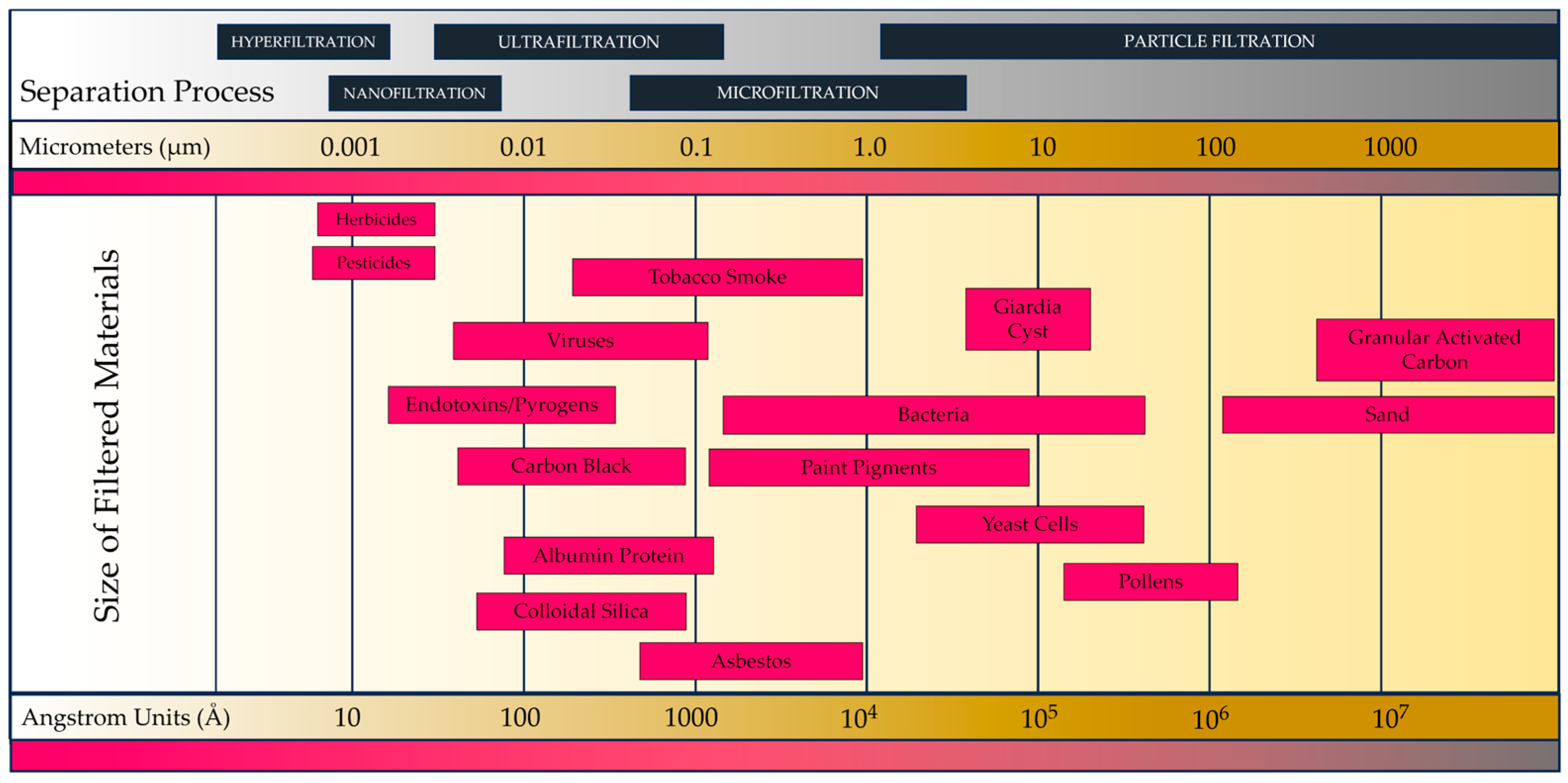
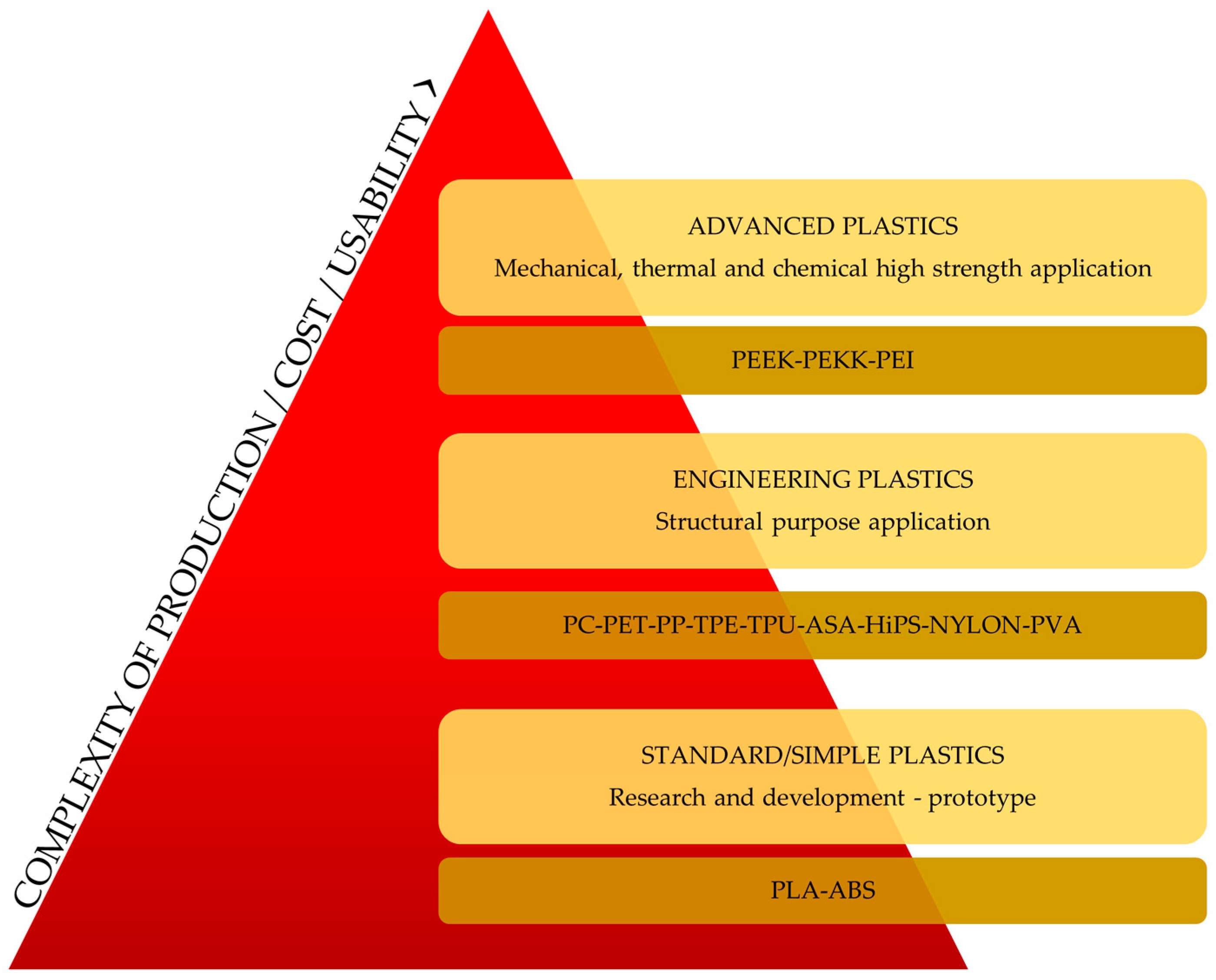
3. Nasal Filter Design and Development: Harnessing Technology for Respiratory Health
4. The Operational Principles of Healthcare Nasal Filters: Design Perspectives
5. The Sustainability Aspects of Healthcare Nasal Filters: Cost and Reusability
6. Ensuring Safety in Healthcare Nasal Filters: Manufacturers’ Testing Protocols
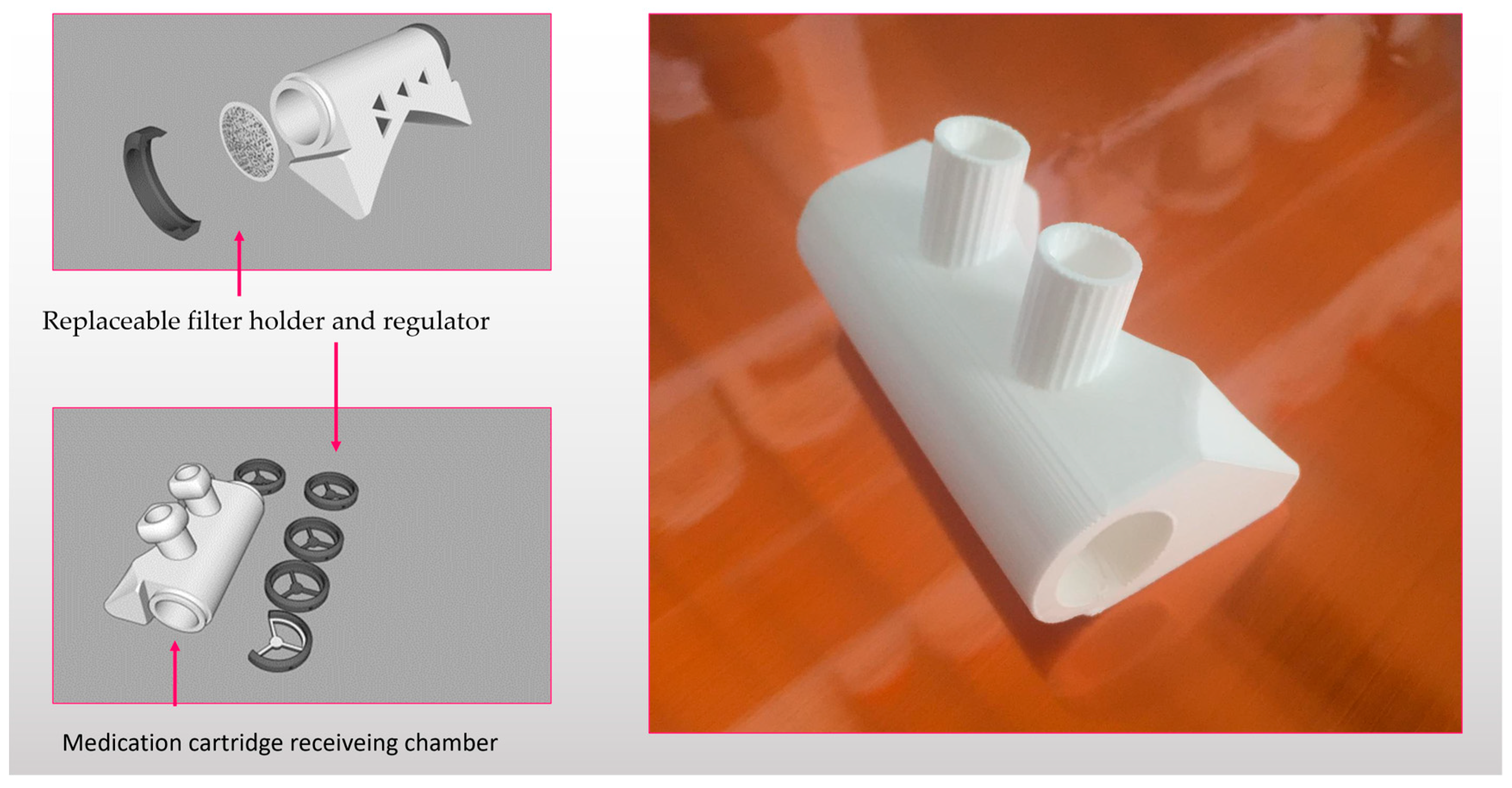
7. Authorization Process for Placing Products on the Market
8. Combination of Nasal Filters with Drug Delivery Devices
9. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferreyro, B.L.; Angriman, F.; Munshi, L.; Del Sorbo, L.; Ferguson, N.D.; Rochwerg, B.; Ryu, M.J.; Saskin, R.; Wunsch, H.; da Costa, B.R.; et al. Association of Noninvasive Oxygenation Strategies with All-Cause Mortality in Adults with Acute Hypoxemic Respiratory Failure. JAMA 2020, 324, 57. [Google Scholar] [CrossRef] [PubMed]
- Freiberg, A.; Horvath, K.; Hahne, T.M.; Drössler, S.; Kämpf, D.; Spura, A.; Buhs, B.; Reibling, N.; De Bock, F.; Apfelbacher, C.; et al. Beeinflussung Der Psychosozialen Entwicklung von Kindern Und Jugendlichen Durch Das Tragen von Gesichtsmasken Im Öffentlichen Raum Zur Prävention von Infektionskrankheiten: Ein Systematischer Review. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2021, 64, 1592–1602. [Google Scholar] [CrossRef] [PubMed]
- Magalhães, P.A.F.; D’Amorim, A.C.G.; de Oliveira, E.F.A.L.; Ramos, M.E.A.; Mendes, A.P.D.d.A.; Barbosa, J.F.d.S.; Reinaux, C.M.A. Alternância de Máscara Nasal Com Pronga Nasal Reduz a Incidência de Lesão Nasal Moderada a Grave Em Prematuros Em Uso de Ventilação Não Invasiva. Rev. Bras. Ter. Intensiv. 2022, 34, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Olin, A.C.; Hellgren, J.; Karlsson, G.; Ljungkvist, G.; Nolkrantz, K.; Torén, K. Nasal Nitric Oxide and Its Relationship to Nasal Symptoms, Smoking and Nasal Nitrate. Rhinology 1998, 36, 117–121. [Google Scholar]
- Farneti, P.; Sorace, F.; Tasca, I. Personal Protective Equipment for ENT Activity during COVID-19 Pandemic. Eur. Arch. Oto-Rhino-Laryngol. 2020, 277, 2933–2935. [Google Scholar] [CrossRef]
- Kesavan, S.; Amirav, I. Is Aerosol Delivery by High-flow Nasal Cannula in Children an Effective Alternative to Face Mask Aerosol Nebulization? Pediatr. Pulmonol. 2019, 54, 1873–1874. [Google Scholar] [CrossRef]
- Hasegawa, M.; Kern, E.B. The Human Nasal Cycle. Mayo Clin. Proc. 1977, 52, 28–34. [Google Scholar] [CrossRef]
- Maniaci, A.; Ferlito, S.; Bubbico, L.; Ledda, C.; Rapisarda, V.; Iannella, G.; La Mantia, I.; Grillo, C.; Vicini, C.; Privitera, E.; et al. Comfort Rules for Face Masks among Healthcare Workers during COVID-19 Spread. Ann. Ig. 2021, 33, 615–627. [Google Scholar] [CrossRef]
- Mauritzson-Sandberg, E. Psychological Effects on Prolonged Use of Respiratory Protective Devices in Children. Ergonomics 1991, 34, 313–319. [Google Scholar] [CrossRef]
- Grigatti, A.; Gefen, A. The Biomechanical Efficacy of a Hydrogel-based Dressing in Preventing Facial Medical Device-related Pressure Ulcers. Int. Wound J. 2022, 19, 1051–1063. [Google Scholar] [CrossRef]
- Ferraz, L.C.C.; Guedes, B.L.d.S.; Lúcio, I.M.L.; Santos, R.C.S. Desenvolvimento de Protetor Nasal Anatômico Para Recém-Nascidos Em Uso de Pronga. Rev. Esc. Enferm. USP 2020, 54, e03618. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Inchingolo, F.; Rapone, B.; Festa, F.; Rexhep Tari, S.; Lorusso, F. Protective Face Masks: Effect on the Oxygenation and Heart Rate Status of Oral Surgeons during Surgery. Int. J. Environ. Res. Public Health 2021, 18, 2363. [Google Scholar] [CrossRef] [PubMed]
- Yamasaki, T.; Komasawa, N.; Kido, H.; Minami, T. Contribution of the Nasal Passage to Face Mask Ventilation: A Prospective Blinded Randomized Crossover Trial. Can. J. Anaesth. 2017, 64, 935–939. [Google Scholar] [CrossRef]
- Kayser, V.; Ramzan, I. Vaccines and Vaccination: History and Emerging Issues. Hum. Vaccines Immunother. 2021, 17, 5255–5268. [Google Scholar] [CrossRef] [PubMed]
- Peters, R.; Ee, N.; Peters, J.; Booth, A.; Mudway, I.; Anstey, K.J. Air Pollution and Dementia: A Systematic Review. J. Alzheimer’s Dis. 2019, 70, S145–S163. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.S.; Langrish, J.P.; Nair, H.; McAllister, D.A.; Hunter, A.L.; Donaldson, K.; Newby, D.E.; Mills, N.L. Global Association of Air Pollution and Heart Failure: A Systematic Review and Meta-Analysis. Lancet 2013, 382, 1039–1048. [Google Scholar] [CrossRef]
- Tran, H.M.; Chen, T.-T.; Lu, Y.-H.; Tsai, F.-J.; Chen, K.-Y.; Ho, S.-C.; Wu, C.-D.; Wu, S.-M.; Lee, Y.-L.; Chung, K.F.; et al. Climate-Mediated Air Pollution Associated with COPD Severity. Sci. Total Environ. 2022, 843, 156969. [Google Scholar] [CrossRef]
- Sousa, A.C.; Pastorinho, M.R.; Masjedi, M.R.; Urrutia-Pereira, M.; Arrais, M.; Nunes, E.; To, T.; Ferreira, A.J.; Robalo-Cordeiro, C.; Borrego, C.; et al. Issue 1—“Update on Adverse Respiratory Effects of Outdoor Air Pollution” Part 2): Outdoor Air Pollution and Respiratory Diseases: Perspectives from Angola, Brazil, Canada, Iran, Mozambique and Portugal. Pulmonology 2022, 28, 376–395. [Google Scholar] [CrossRef]
- Jia, Y.; Lin, Z.; He, Z.; Li, C.; Zhang, Y.; Wang, J.; Liu, F.; Li, J.; Huang, K.; Cao, J.; et al. Effect of Air Pollution on Heart Failure: Systematic Review and Meta-Analysis. Environ. Health Perspect. 2023, 131, 76001. [Google Scholar] [CrossRef]
- Bhadauria, S.; Dixit, A.; Singh, D. Estimation of Air Pollution Tolerance and Anticipated Performance Index of Roadside Plants along the National Highway in a Tropical Urban City. Environ. Monit. Assess. 2022, 194, 808. [Google Scholar] [CrossRef]
- Gajski, G.; Gerić, M.; Pehnec, G.; Matković, K.; Rinkovec, J.; Jakovljević, I.; Godec, R.; Žužul, S.; Bešlić, I.; Cvitković, A.; et al. Associating Air Pollution with Cytokinesis-Block Micronucleus Assay Parameters in Lymphocytes of the General Population in Zagreb (Croatia). Int. J. Mol. Sci. 2022, 23, 83. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Xia, Q.; Lai, Y.; Wu, B.; Tian, W.; Miao, W.; Feng, X.; Xin, L.; Miao, J.; Wang, N.; et al. Spatial Effects of Air Pollution on the Economic Burden of Disease: Implications of Health and Environment Crisis in a Post-COVID-19 World. Int. J. Equity Health 2022, 21, 161. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Cai, J.; Chen, R.; Sera, F.; Guo, Y.; Tong, S.; Li, S.; Lavigne, E.; Correa, P.M.; Ortega, N.V.; et al. Coarse Particulate Air Pollution and Daily Mortality: A Global Study in 205 Cities. Am. J. Respir. Crit. Care Med. 2022, 206, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Ren, X.; Huang, S.; Wang, J.; Xu, X. The Impact of Urbanization on Air Quality in Africa from Time and Spatial Perspectives. Environ. Sci. Pollut. Res. Int. 2022, 29, 74699–74714. [Google Scholar] [CrossRef]
- Landry, S.A.; Subedi, D.; Barr, J.J.; MacDonald, M.I.; Dix, S.; Kutey, D.M.; Mansfield, D.; Hamilton, G.S.; Edwards, B.A.; Joosten, S.A. Fit-Tested N95 Masks Combined With Portable High-Efficiency Particulate Air Filtration Can Protect Against High Aerosolized Viral Loads Over Prolonged Periods at Close Range. J. Infect. Dis. 2022, 226, 199–207. [Google Scholar] [CrossRef]
- Seibt, R.; Bär, M.; Rieger, M.A.; Steinhilber, B. Limitations in Evaluating COVID-19 Protective Face Masks Using Open Circuit Spirometry Systems: Respiratory Measurement Mask Introduces Bias in Breathing Pressure and Perceived Respiratory Effort. Physiol. Meas. 2023, 44, 015001. [Google Scholar] [CrossRef]
- Mahmoudi, A.; Tavakoly Sany, S.B.; Ahari Salmasi, M.; Bakhshi, A.; Bustan, A.; heydari, S.; Rezayi, M.; Gheybi, F. Application of Nanotechnology in Air Purifiers as a Viable Approach to Protect against Corona Virus. IET Nanobiotechnol. 2023, 17, 289–301. [Google Scholar] [CrossRef]
- Rogak, S.N.; Rysanek, A.; Lee, J.M.; Dhulipala, S.V.; Zimmerman, N.; Wright, M.; Weimer, M. The Effect of Air Purifiers and Curtains on Aerosol Dispersion and Removal in Multi-Patient Hospital Rooms. Indoor Air 2022, 32, e13110. [Google Scholar] [CrossRef]
- Khan, M.T.; Shah, I.A.; Hossain, M.F.; Akther, N.; Zhou, Y.; Khan, M.S.; Al-Shaeli, M.; Bacha, M.S.; Ihsanullah, I. Personal Protective Equipment (PPE) Disposal during COVID-19: An Emerging Source of Microplastic and Microfiber Pollution in the Environment. Sci. Total Environ. 2023, 860, 160322. [Google Scholar] [CrossRef]
- Hasan, M.; Islam, A.R.M.T.; Jion, M.M.M.F.; Rahman, M.N.; Peu, S.D.; Das, A.; Bari, A.B.M.M.; Islam, M.S.; Pal, S.C.; Islam, A.; et al. Personal Protective Equipment-Derived Pollution during Covid-19 Era: A Critical Review of Ecotoxicology Impacts, Intervention Strategies, and Future Challenges. Sci. Total Environ. 2023, 887, 164164. [Google Scholar] [CrossRef]
- Chen, R.; Zhang, X.; Wang, P.; Xie, K.; Jian, J.; Zhang, Y.; Zhang, J.; Yuan, Y.; Na, P.; Yi, M.; et al. Transparent thermoplastic polyurethane air filters for efficient electrostatic capture of particulate matter pollutants. Nanotechnology 2019, 30, 015703. [Google Scholar] [CrossRef] [PubMed]
- Liang, H.; Ji, Y.; Ge, W.; Wu, J.; Song, N.; Yin, Z.; Chai, C. Release kinetics of microplastics from disposable face masks into the aqueous environment. Sci. Total Environ. 2022, 816, 151650. [Google Scholar] [CrossRef] [PubMed]
- Moghadasi, H.; Mollah, M.T.; Marla, D.; Saffari, H.; Spangenberg, J. Computational Fluid Dynamics Modeling of Top-Down Digital Light Processing Additive Manufacturing. Polymers 2023, 15, 2459. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Du, C.; Hu, Y.; Yuan, H.; Wang, J.; Pan, Y.; Bao, L.; Dong, L.; Li, C.; Sun, Y.; et al. Diagnostic Performance of Computational Fluid Dynamics (CFD)-Based Fractional Flow Reserve (FFR) Derived from Coronary Computed Tomographic Angiography (CCTA) for Assessing Functional Severity of Coronary Lesions. Quant. Imaging Med. Surg. 2023, 13, 1672–1685. [Google Scholar] [CrossRef] [PubMed]
- Quodbach, J.; Bogdahn, M.; Breitkreutz, J.; Chamberlain, R.; Eggenreich, K.; Elia, A.G.; Gottschalk, N.; Gunkel-Grabole, G.; Hoffmann, L.; Kapote, D.; et al. Quality of FDM 3D Printed Medicines for Pediatrics: Considerations for Formulation Development, Filament Extrusion, Printing Process and Printer Design. Ther. Innov. Regul. Sci. 2022, 56, 910–928. [Google Scholar] [CrossRef]
- Serrano, D.R.; Kara, A.; Yuste, I.; Luciano, F.C.; Ongoren, B.; Anaya, B.J.; Molina, G.; Diez, L.; Ramirez, B.I.; Ramirez, I.O.; et al. 3D Printing Technologies in Personalized Medicine, Nanomedicines, and Biopharmaceuticals. Pharmaceutics 2023, 15, 313. [Google Scholar] [CrossRef]
- Ahmad, J.; Garg, A.; Mustafa, G.; Mohammed, A.A.; Ahmad, M.Z. 3D Printing Technology as a Promising Tool to Design Nanomedicine-Based Solid Dosage Forms: Contemporary Research and Future Scope. Pharmaceutics 2023, 15, 1448. [Google Scholar] [CrossRef]
- Abourehab, M.A.S.; Pramanik, S.; Abdelgawad, M.A.; Abualsoud, B.M.; Kadi, A.; Ansari, M.J.; Deepak, A. Recent Advances of Chitosan Formulations in Biomedical Applications. Int. J. Mol. Sci. 2022, 23, 10975. [Google Scholar] [CrossRef]
- Eljack, S.; David, S.; Faggad, A.; Chourpa, I.; Allard-Vannier, E. Nanoparticles Design Considerations to Co-Deliver Nucleic Acids and Anti-Cancer Drugs for Chemoresistance Reversal. Int. J. Pharm. X 2022, 4, 100126. [Google Scholar] [CrossRef]
- Campodoni, E.; Artusi, C.; Vazquez Iglesias, B.; Nicosia, A.; Belosi, F.; Vandini, A.; Monticelli, P.; Tampieri, A.; Sandri, M. Nature-Inspired Heat and Moisture Exchanger Filters Composed of Gelatin and Chitosan for the Design of Eco-Sustainable “Artificial Noses”. ACS Appl. Polym. Mater. 2023, 5, 3468–3479. [Google Scholar] [CrossRef]
- Kansız, S.; Elçin, Y.M. Advanced Liposome and Polymersome-Based Drug Delivery Systems: Considerations for Physicochemical Properties, Targeting Strategies and Stimuli-Sensitive Approaches. Adv. Colloid. Interface Sci. 2023, 317, 102930. [Google Scholar] [CrossRef] [PubMed]
- Durand, G.A.; Amroun, A.; Grard, G.; Badaut, C. Positive SARS-CoV-2 RT-QPCR of a Nasal Swab Spot after 30 Days of Conservation on Filter Paper at Room Temperature. J. Med. Virol. 2023, 95, e28165. [Google Scholar] [CrossRef] [PubMed]
- Penninx, B.W.J.H.; Benros, M.E.; Klein, R.S.; Vinkers, C.H. How COVID-19 Shaped Mental Health: From Infection to Pandemic Effects. Nat. Med. 2022, 28, 2027–2037. [Google Scholar] [CrossRef] [PubMed]
- Gandjour, A. Cost-Effectiveness of Future Lockdown Policies against the COVID-19 Pandemic. Health Serv. Manag. Res. 2023, 36, 51–62. [Google Scholar] [CrossRef]
- Saylor, D.M.; Young, J.A. Modeling Extraction of Medical Device Polymers for Biocompatibility Evaluation. Regul. Toxicol. Pharmacol. 2023, 141, 105405. [Google Scholar] [CrossRef]
- Lobo, P.; Vilaça, J.L.; Torres, H.; Oliveira, B.; Simões, A. Smart Scan of Medical Device Displays to Integrate with a MHealth Application. Heliyon 2023, 9, e16297. [Google Scholar] [CrossRef]
- Semeraro, S.; Gaetano, A.S.; Zupin, L.; Poloni, C.; Merlach, E.; Greco, E.; Licen, S.; Fontana, F.; Leo, S.; Miani, A.; et al. Operative Protocol for Testing the Efficacy of Nasal Filters in Preventing Airborne Transmission of SARS-CoV-2. Int. J. Environ. Res. Public Health 2022, 19, 13790. [Google Scholar] [CrossRef]
- Natu, R.; Herbertson, L.; Sena, G.; Strachan, K.; Guha, S. A Systematic Analysis of Recent Technology Trends of Microfluidic Medical Devices in the United States. Micromachines 2023, 14, 1293. [Google Scholar] [CrossRef]
- Ming, J.; He, Y.; Yang, Y.; Hu, M.; Zhao, X.; Liu, J.; Xie, Y.; Wei, Y.; Chen, Y. Health Technology Assessment of Medical Devices: Current Landscape, Challenges, and a Way Forward. Cost Eff. Resour. Alloc. 2022, 20, 54. [Google Scholar] [CrossRef]
- Freitas, L.; Vieira, A.C.L.; Oliveira, M.D.; Monteiro, H.; Bana e Costa, C.A. Which Value Aspects Are Relevant for the Evaluation of Medical Devices? Exploring Stakeholders’ Views through a Web-Delphi Process. BMC Health Serv. Res. 2023, 23, 593. [Google Scholar] [CrossRef]
- Fink, M.; Akra, B. Comparison of the International Regulations for Medical Devices—USA versus Europe. Injury 2023, 110908. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Picone, D.S.; Padwal, R.; Campbell, N.R.C.; Drawz, P.; Rakotz, M.K.; Parati, G.; Zhang, X.-H.; Sharman, J.E. Global Proliferation and Clinical Consequences of Non-Validated Automated BP Devices. J. Hum. Hypertens. 2022, 37, 115–119. [Google Scholar] [CrossRef] [PubMed]
- McPeck, M.; Moon, J.; Jayakumaran, J.; Smaldone, G.C. In Vitro Model for Analysis of High-Flow Aerosol Delivery During Continuous Nebulization. Respir. Care 2023, 68, 1213–1220. [Google Scholar] [CrossRef] [PubMed]
- Alanazi, O.; Li, J. The Impact of Various HFNC Devices on Transnasal Aerosol Delivery. Respir. Care 2023, 68, 10777. [Google Scholar] [CrossRef] [PubMed]
- To Quoc, T.; Bíró, K.; Pető, Á.; Kósa, D.; Sinka, D.; Lekli, I.; Kiss-Szikszai, A.; Budai, I.; Béres, M.; Vecsernyés, M.; et al. Development and Evaluation of an FDM Printed Nasal Device for CPZ Solid Nanoparticles. Molecules 2023, 28, 4406. [Google Scholar] [CrossRef] [PubMed]

| Key Findings | Materials Used | Types of Filters | Application Areas | Prices | Sustainability Aspects | Limiting Factors |
|---|---|---|---|---|---|---|
| Effective Allergen Filtration | Polypropylene | Mechanical Filters | Allergy Management | Moderate Range | Recyclable materials | Limited efficacy with ultrafine particles |
| Environmental Protection | Activated Carbon | Electrostatic Filters | Respiratory Health | Low Range | Low environmental impact | Short filter lifespan |
| Microorganism Blockage | Silicone | Nano-fiber Filters | Healthcare Applications | High Range | Antibacterial properties | Potential skin irritations |
| Hypoallergenic Materials | Cotton | Carbon Dioxide Filters | Pediatric Respiratory | Variable Pricing | Organic and hypoallergenic materials | Reduced filtration efficiency |
| Comfortable Fit and Wear | Polyester | Active Filters | Sports and Recreation | Various Price Ranges | Enhanced breathability | Limited protection against gases |
| Durability and Reusability | Plastic | Shrink-wrapped Filters | Workplace Environment | Affordable Options | Reusable and sustainable | Reduced filtration capacity over time |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quoc, T.T.; Bácskay, I.; Fehér, P.; Pallér, Á.; Papp, B.; Bíró, K.; Ujhelyi, Z. Personalized Nasal Protective Devices: Importance and Perspectives. Life 2023, 13, 2116. https://doi.org/10.3390/life13112116
Quoc TT, Bácskay I, Fehér P, Pallér Á, Papp B, Bíró K, Ujhelyi Z. Personalized Nasal Protective Devices: Importance and Perspectives. Life. 2023; 13(11):2116. https://doi.org/10.3390/life13112116
Chicago/Turabian StyleQuoc, Thinh To, Ildikó Bácskay, Pálma Fehér, Ádám Pallér, Boglárka Papp, Krisztina Bíró, and Zoltán Ujhelyi. 2023. "Personalized Nasal Protective Devices: Importance and Perspectives" Life 13, no. 11: 2116. https://doi.org/10.3390/life13112116
APA StyleQuoc, T. T., Bácskay, I., Fehér, P., Pallér, Á., Papp, B., Bíró, K., & Ujhelyi, Z. (2023). Personalized Nasal Protective Devices: Importance and Perspectives. Life, 13(11), 2116. https://doi.org/10.3390/life13112116









