Abstract
There are various pathologies that involve the hallux, among which hallux valgus is the most common. When conservative treatment fails, it is necessary to resort to a surgical approach. The fixation elements for osteotomies in the hallux are usually composed of metallic materials; however, today, there are numerous resorbable materials that offer numerous advantages over conventional materials. In this article, the objective is to analyze the scientific evidence through the systematic analysis of the existing literature in relation to the effectiveness of resorbable versus non-resorbable osteosynthesis material in the surgical correction of hallux deformities and compare the complications as well as the patient satisfaction and quality of life between both fixation methods. A systematic review of the literature available in the PubMed, EMBASE, Web of Science and Scopus databases and 10 studies were included. The documents were chosen following the eligibility and exclusion criteria, including experimental and observational studies evaluated with the Jadad and Newcastle-Ottawa methodological quality scale, respectively. Data were extracted from valid studies for the review, and the variables functionality, pain, angular corrections, complications, satisfaction and quality of life were observed. In conclusion, there is limited scientific evidence regarding the effectiveness of resorbable versus non-resorbable osteosynthesis material in the surgical correction of hallux deformities. All observed variables are similar regardless of the surgical technique and osteosynthesis material used.
1. Introduction
There are various pathologies that involve the hallux, among which hallux valgus is the most common forefoot problem in adults [1,2,3,4]. The management of this pathology generally begins with conservative treatment, but when this fails and the deformity is painful, affecting the patient’s lifestyle, it is necessary to resort to surgical treatment [5,6,7,8].
Surgical corrections of the hallux valgus are mostly osteotomies, which must be fixed with osteosynthesis materials such as needles and screws. Stainless steel and titanium are the most commonly used materials to produce these fixation devices, showing good mechanical resistance, biocompatibility, and corrosion resistance [2,3,9]. However, in recent years, the use of resorbable implants has been gaining popularity due to some advantages over conventional metal implants; since they have an elastic modulus more similar to that of bone, it is not necessary to extract them later, and they do not interfere with the post-surgical imaging tests [10,11,12,13].
Numerous resorbable fixation materials have already been used in foot surgery, such as PLA polymers, polyglycolic acid and their copolymers. However, although successful results have been reported with these materials, complications such as granuloma formation or foreign body reaction have also been reported [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16]. Recently, resorbable magnesium screws have been introduced, which is a material that is naturally present in the human body [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20].
The development of resorbable materials is booming and, therefore, it is necessary to know what the advantages and disadvantages of these are compared to non-resorbable materials. As there is very little scientific evidence regarding this topic, this study aims to provide knowledge about resorbable and non-resorbable materials, establishing a comparison between both in order to know their differences and indications.
2. Materials and Methods
The present systematic review has been designed following the recommendations of the PRISMA Declaration (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [21,22] and, in addition, the protocol has been registered in the International Prospective Registry of Systematic Reviews (PROSPERO: CRD42023431784).
2.1. Inclusion Criteria
The literature was selected respecting the criteria detailed below: studies conducted in adult patients with hallux deformities requiring surgical treatment were considered eligible for analysis; that the surgical correction uses resorbable and non-resorbable osteosynthesis material; that variables related to the clinical and/or radiological sphere are measured; experimental or observational studies; documents written in Spanish or English; and publication date from 2013 to the present.
Documents that consist of systematic reviews or meta-analyses and studies that do not compare the experimental group with a control group are excluded, since we want the data obtained to be as homogeneous as possible to be able to analyze and compare them later. We also excluded all the studies involving animals. Outcome measures extracted from the studies were functionality, angular corrections, pain, complications, quality of life, and patient satisfaction.
2.2. Databases and Search Strategy
A systematic search of the literature was carried out in the electronic databases PubMed, EMBASE, Web of Science and Scopus during the months of April–June 2023. In order to obtain the data related to the most recent and updated treatments, we decided to select articles published between 2013 and 2023.
When establishing the design for a search strategy, the first step was to formulate a structured question. To structure it, the PICO model (patient/population/problem, intervention, comparison/control, outcome) was used: P: Adult patients who present deformities in the hallux and require surgical treatment; I: Surgical correction through open surgery or minimally invasive surgery (MIS) with resorbable osteosynthesis material; C: Surgical correction by open surgery or MIS with non-resorbable osteosynthesis material; O: Effectiveness of surgery through post-surgical outcome variables related to the clinical sphere (functionality, pain level, complications, satisfaction and quality of life) and radiological sphere (angular corrections). Thus, our research question is the following: Is surgical correction of hallux deformities with resorbable osteosynthesis material effective compared to non-resorbable osteosynthesis material?
The following search strategy was implemented in the different databases: (Wire* OR “K-wire*” OR “Kirschnerwire*” OR Screw* OR Pin* OR Implant* OR “intramedullary pin*” OR “intramedullarywire*” OR fixation) AND (Resorbable OR Bioresorbable OR Absorbable OR Bioabsorbable OR Degradable OR Biodegradable OR “Absorbablefixation” OR “Resorbablefixation” OR “Poly-L-lactideacid” OR Copolymer* OR PLLA OR PLDLA OR PLA OR PGA OR Polylactate OR “Polyglycolide” OR “Polylacticacid” OR “Polylactideacid” OR “polyglycolicacid” OR Magnesium) AND (Arthrodesis OR osteotomy OR osteotomies OR correction OR “halluxsurgery” OR “Interphalangealjoint” OR bunionectomy OR “forefootsurgery” OR “digital surgery”) AND (DIP OR PIP OR Forefoot OR Digital OR hallux OR “halluxvalgus” OR “halluxabductusvalgus” OR “halluxvarus ” OR “firstray” OR bunion OR “Interphalangealjoint” OR digit* OR “toe joint”).
Two independent reviewers (R.P.-D. and J.M.M.-S.) assisted with conducting and validating the research. Only articles written in English and Spanish were accepted.
2.3. Selection of Studies
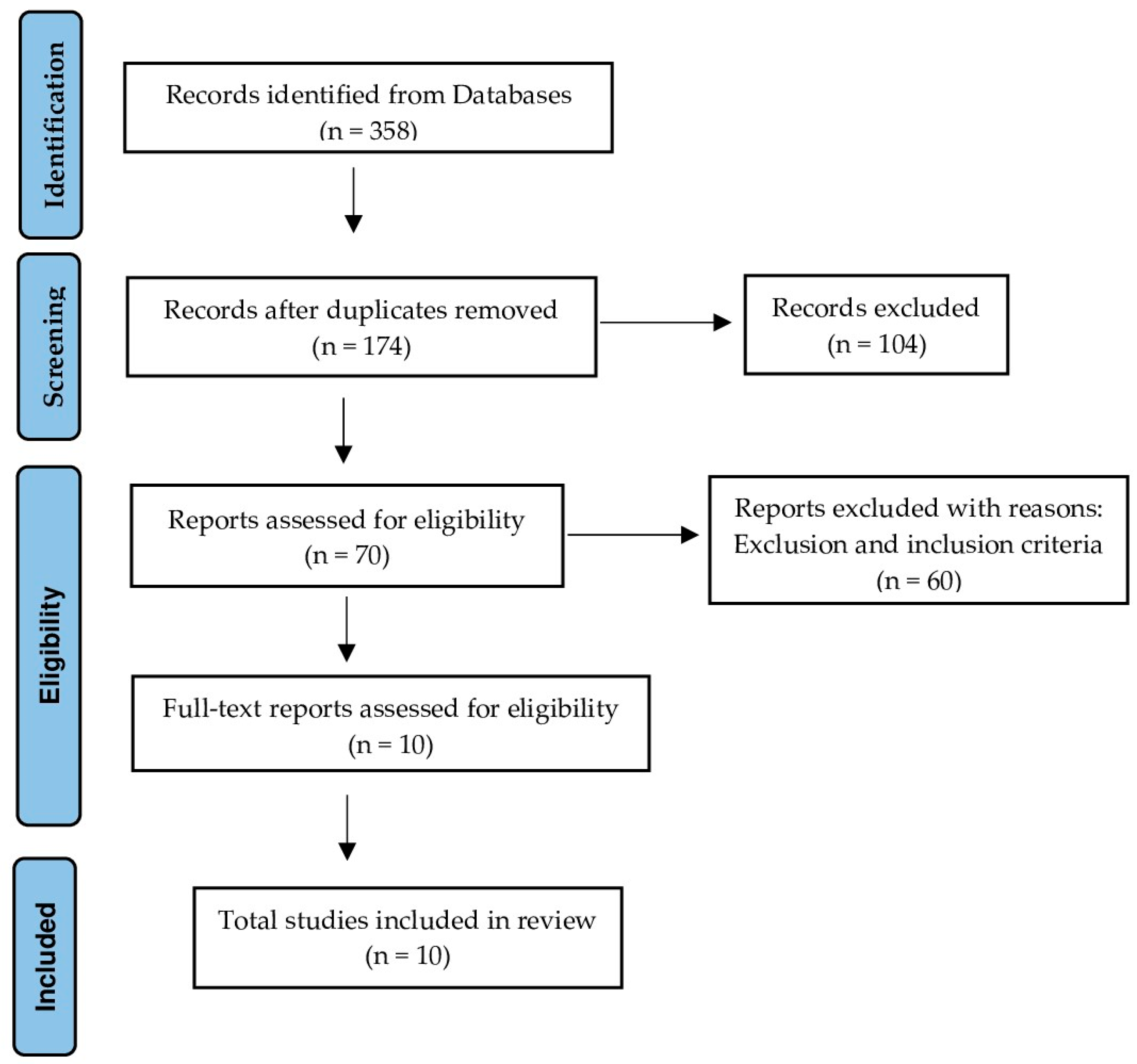
The articles that emerged from the research were independently reviewed by two independent reviewers (R.P.-D. and J.M.M.-S.). Once the total number of documents was obtained from the EMBASE, PubMed, Web of Science and Scopus databases and having applied the temporal filter from 2013 to 2023, the first step of this process consisted of locating the duplicate studies in order to discard them manually. Subsequently, the titles and abstracts of the studies were analyzed to evaluate their eligibility using the established inclusion and exclusion criteria, screening those that did not meet these criteria. Those that were not in full text and systematic reviews with or without meta-analysis were also excluded. Finally, the full text of those studies that were susceptible to selection was reviewed and included in the present systematic review. Disagreements were resolved through group discussion with arbitration by the senior author. This entire process is recorded in the flow chart (Figure 1).
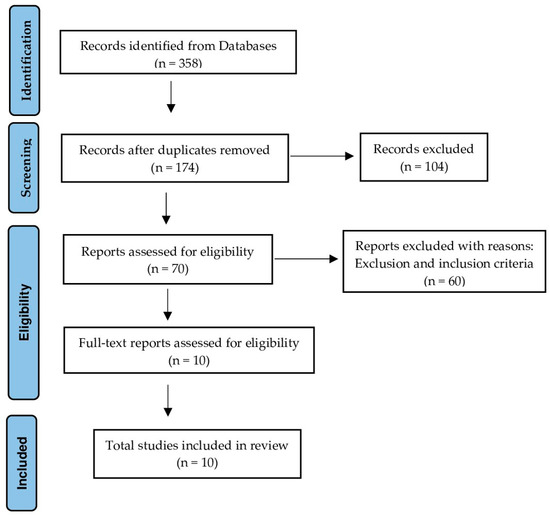
Figure 1.
Flow chart.
2.4. Data Extraction
To follow this process, a standardized table was created where the characteristics that we considered most relevant for each study were added: author and year of publication, type of study, study population, sample size, intervention performed, follow-up, variables of interest, main results, conclusions and limitations. Due to the heterogeneity of the clinical studies and the population sample analyzed in the different studies, some data were missing or cannot be extrapolated; therefore, missing data have been considered in the presentation of our results.
2.5. Quality Assessment
The quality of clinical trials was evaluated using the Jadad scale [23], and the quality of the case-control studies was assessed using the Newcastle-Ottawa scale [24,25]. The Jadad scale allows evaluating the methodological quality of clinical trials and has 5 items with the maximum score of the scale being 5 points. If the score obtained is less than 3 points, the clinical trial is considered weak [23]. The Newcastle-Ottawa scale is based on a star system through which different studies are evaluated based on 3 categories, which contain a certain number of items. Studies that have earned a score of 7 to 9 stars are classified as high quality. Those with a score of 4 to 6 stars are considered studies at high risk of bias, and those with scores of 0 to 3 stars have a very high risk of bias [24,26].
3. Results
After carrying out the search in the different databases with the aforementioned strategy and adding the temporal filter from 2013 to 2023, a total of 358 documents have been obtained. Of this total, 184 studies have been eliminated due to being duplicates, leaving 174 documents. After reading the title and abstract, 104 studies were eliminated since they were interventions other than those proposed in our objectives, leaving us with 70 documents. Of these, 60 were excluded after reading the full text according to the inclusion and exclusion criteria, finally leaving us with a total of 10 articles.
We were therefore left with a total of 10 studies for the final analysis (Figure 1).
3.1. Quality of Studies
According to the Jadad scale, clinical trials conducted by Plaass et al. [27] and Windhagen et al. [28] have obtained a score equal to 3; therefore, they are considered clinical trials with adequate methodological quality. According to the Newcastle-Ottawa scale, eight case-control studies have obtained a score greater than 7 and thus are considered to be of high quality.
3.2. Materials
Of the 10 documents included in the present review, with respect to materials, six studies compare magnesium screws with titanium screws, two studies compare polylactic acid (PLA) needles with Kirschner needles, one study compares L-lactide and trimethylcarbonate copolymer needles with titanium screws, and finally, one study compares poly L-lactic acid (PLLA) and poly D, L-lactic acid (PDLLA) copolymer needles with titanium screws.
3.3. Functionality
Of the 10 studies, nine measure functionality using various scales: seven studies use the American Foot and Ankle Society Hallux Metatarsophalangeal-Interphalangeal Score (AOFAS-MTP-IP), three studies measure the range of motion of the 1st metatarsophalangeal joint (ROM 1st AMTF) using a goniometer, two studies use the Manchester-Oxford Foot Questionnaire (MOXFQ), one study includes the Foot Function Index (FFI) and another study uses the Foot and Ankle Outcome Score (FAOS). Furthermore, one study measures functionality by assessing functional impairment using the visual analogue scale (VAS), and another study does so by assessing the patients’ ability to walk using a nominal scale.
3.4. Angular Corrections
Of the 10 studies, seven articles measure angular corrections: In seven studies, the hallux valgus angle (HVA) and the intermetatarsal angle (IMA) are measured, in two studies, the distal metatarsal joint angle (DMAA) is measured, and the authors measure the hallux interphalangeal angle (HIA) in only one study.
3.5. Pain
Of the 10 studies, eight measured the pain of patients: five articles used the VAS and one article used the Numerical Rating Scale (NRS). Furthermore, in one study, the pain of the first metatarsophalangeal joint (1st AMTF) perceived by the patient in his daily life and during the follow-up examination was evaluated using a nominal scale.
3.6. Complications
Of 10 studies, nine compile the complications that have appeared during the follow-up period.
3.7. Quality of Life and Satisfaction
Of the 10 studies, two measure the quality of life perceived by patients, and three studies measure their satisfaction after the procedure. To measure quality of life, different scales have been used: two studies use the Short-Form Health Survey (SF-36 health questionnaire), while one study uses the Foot and Ankle Ability Measure (FAAM) referring to activities of daily living (ADL) and sports (SPORT). Finally, one study uses the EuroQoL 5-Dimension 3-Level (EQ-5D-3L). To measure satisfaction, one study has used the Coughlin scale and the Likert scale.
The summarized data in our systematic review are reported in Table 1.

Table 1.
Studies included in the review and main features: results and conclusions.
4. Discussion
The main objective of this systematic review is to review the current scientific evidence through the systematic analysis of the existing literature in relation to the effectiveness of resorbable versus non-resorbable osteosynthesis material in the surgical correction of hallux deformities to improve functionality, pain and angular corrections as well as compare the associated complications and the satisfaction and quality of life perceived by patients. A total of 10 studies have been included that compare various types of resorbable osteosynthesis material such as magnesium screws and polydioxanone, polylactic acid, L-lactide-trimethylcarbonate and PLLA-PDLLA needles with non-resorbable osteosynthesis material such as Kirschner wires and titanium screws.
Based on the objectives set and the variables selected, we will proceed to discuss the findings found among the different studies analyzed.
4.1. Functionality
All studies that have assessed functionality using the AOFAS-MTP-IP scale before and after surgery have agreed that there was a significant improvement in the score at the end of follow-up in comparison with pre-surgical values both in the group where resorbable material was used and in the group where non-resorbable material was used [37,38,39]. In addition, the post-surgical AOFAS-MTP-IP scale values did not show significant differences between the study groups. However, the study by Wendelstein et al. [30] does not offer us the pre-surgical values of the scale, therefore, it cannot be known if there was an improvement in the score at the end of the follow-up. However, the final pre-surgical values that we can observe in these studies are good with no significant difference between the different groups.
Regarding the ROM 1st AMTF, in the study by Windhagen et al. [28], there was an increase in this after surgery compared to pre-surgical values in the group where magnesium screws were used and in the group where titanium screws were used. In contrast to the results obtained in previous studies, Plaass et al. [27] and Acar et al. [35] observed a significant decrease in ROM 1st AMTF in their studies regardless of whether the patient had a magnesium screw or a titanium screw. What all the studies do have in common is that no significant difference was found between the study groups regarding the final ROM 1st AMTF values.
Song et al. [29] analyzed functionality using MOXFQ in their study and observed that there was a significant improvement in scores in all domains after surgery compared to the score obtained before surgery. This result was obtained in both study groups, and they did not show significant differences in post-surgical scores. A similar result was obtained by Atkinson et al. [32] in their study, since all the parameters of the questionnaire improved significantly after surgery, with the parameters “foot pain” and “social interaction” being the ones that showed better improvement levels in both groups. In the final results, there was no significant difference between the groups except in the parameters “walking standing” and “index”, being significantly better in the group where the osteotomy was fixed with magnesium screws.
Wendelstein et al. [30] wanted to evaluate the FFI at the end of the follow-up and were able to observe that there were no significant differences in the values obtained between the three study groups; however, Kirschner needles were the ones that obtained the best FFI followed by the magnesium screws and finally the titanium screws.
Only Atkinson et al. [32] used the FAOS in their study. In it, they noticed that the score improved significantly in all patients in both groups with no significant differences between them for any of the individual scoring parameters.
Finally, in the study by Wendelstein et al. [30], the VAS was used to assess functional deterioration after surgery, and the results showed no significant differences between the three types of groups with a very low score in the VAS.
4.2. Angular Corrections
Regarding the HVA and the IMA, all the studies that measure these angles stated that thanks to the surgery, there had been a significant decrease in them at the end of the study follow-up compared to the pre-surgical results both in the group where resorbable material is used and in the group where non-resorbable material is used.
Furthermore, in most of the articles, there were no significant differences between the study groups regarding the pre-surgical and post-surgical angular values; therefore, the degrees of surgical correction were similar. However, in the study by Choo et al. [31], there were more degrees of correction of the HVA and IMA in the group where titanium screws were used than in the group where magnesium screws were used. On the contrary, the results obtained by Wendelstein et al. [30] showed significantly higher degrees of correction of the IMA in the group where magnesium screws were used compared to metallic Kirschner wires. This same result was obtained in the study by Morandi et al. [36], where the degrees of IMA correction were also significantly higher in the resorbable group, where PLLA and PDLLA needles were used, compared with titanium screws.
Only three articles have taken into account angles other than HVA and IMA. In the studies by Windhagen et al. [28] and Komur et al. [34], the DMAA was included, and the result was a significant decrease in both studies after surgery in both the group where resorbable material was used and in the group where non-resorbable material was used. Finally, Song et al. [29] decided to include the HIA in their study, and it was concluded that there was also a significant decrease in the angle after surgical correction in both the resorbable PLA needles group and the non-absorbable group of Kirschner needles.
4.3. Pain
The studies conducted by Choo et al. [31], Windhagen et al. [28], and Komur et al. [34] have used the VAS to evaluate the pain of patients, and all have concluded that there has been a significant decrease in pain at the end of follow-up compared to the level of pain before surgery both in the group where resorbable material was used and in the group where non-resorbable material was used.
These results agree with the study by Acar et al. [35]; however, in this study, a patient who underwent surgery with a titanium screw had to have the implant removed after six months due to the pain he suffered in his daily activities. In the study by Plaass et al. [27], assessed pain using the NRS and also found a significant decrease in pain three years after surgery in both groups. No patient who underwent surgery with magnesium screws had residual pain; however, in three patients with titanium screws, the pain persisted: two of them felt slight pain when running and the other patient felt pain when running, during walking and in repose.
The study by Wendelstein et al. [30] has not assessed pain before surgery; therefore, a comparison between pre-surgical and post-surgical values cannot be established. However, the post-surgical pain values on the VAS scale were quite low in both groups and in both studies.
All the studies mentioned above agree that there is no significant difference in post-surgical pain values between patients in the resorbable group and patients in the non-resorbable group.
4.4. Complications
Due to the heterogeneity of complications, the discussion of data between the different studies included in the review becomes complex.
The only study where no intraoperative or postoperative complications were observed in both groups was that of Atkinson et al. [32]. Regarding implant removal due to discomfort, no resorbable implant had to be removed in any of the studies. This did not happen with non-resorbable implants: in the studies by Plaass et al. [27], Windhagen et al. [28], Choo et al. [31], and Acar et al. [35], the titanium screw had to be removed in one patient due to the discomfort it caused.
The studies carried out by Plaass et al. [27] and Song et al. [29] showed no significant differences between post-surgical complications between the study groups. Similar results were found in the remaining studies where complications did not differ between groups. Acar et al. [35] also did not observe a significant difference between both groups in complications except for the accumulation of gas in the tissues surrounding the osteotomy, since this complication occurred in a large number of patients, all with magnesium screws. Like the previous study, Klauser [33] also found no significant differences between the groups in most complications; however, in 40% of the patients who had magnesium screws, radiological findings appeared such as osteolysis, areas lytics, radiolucency and demineralization around the screw. Both the accumulation of gas in the surrounding tissue and the radiological findings mentioned above are the result of the magnesium degradation process, being temporary and not intervening with the consolidation of the osteotomy.
4.5. Quality of Life
In the study carried out by Atkinson et al. [32], the quality of life perceived by the patients was evaluated using the EQ-5D-3L before and after surgery, resulting in a significant improvement in the quality of life of the patients after undergoing surgery—both in the group where fixation was performed with magnesium screws and in the group where titanium screws were used. Similar results were obtained by Choo et al. [31] using the SF-36 health questionnaire. In the group where magnesium screws were used, there was a significant improvement in all domains of the questionnaire except in the “emotional role” domain, which also improved, although not significantly. In the group where titanium screws were used, there was a significant improvement in all domains of the questionnaire.
Plaass et al. [27] evaluated the quality of life of the patients only after surgery using the SF-36 health questionnaire and the FAAM. A comparison of pre-surgical and post-surgical values could not be made; however, the quality of life of the patients after surgery was good, and there were no significant differences between the resorbable and non-resorbable group. This result was the same for the study by Atkinson et al. [32]; however, in the study by Choo et al. [31], the “general health” domain of the SF-36 health questionnaire was significantly better in the group where magnesium screws were used.
4.6. Satisfaction
Regarding patient satisfaction based on the procedure and result, Plaass et al. [27] were able to conclude that all patients in the study were very satisfied with the surgery, would undergo it again if necessary and would recommend it. Similar results were obtained by Windhagen et al. [28] in their study, since all patients were very satisfied with the surgery except one belonging to the resorbable group who had healing problems and was dissatisfied with the procedure.
Song et al. [29] assessed patient satisfaction using the Coughlin scale and the Likert scale, also being able to observe excellent levels of satisfaction. Although the differences were not significant between the study groups, the level of satisfaction was slightly higher in the patients who underwent surgery with PLA needles. We found the same thing in the study by Wendelstein et al. [30] where the patients were also asked if they would undergo the same intervention again, finding a significant difference since the resorbable material group had greater satisfaction.
5. Conclusions
Based on the objectives set and the results obtained in this systematic review, the following can be concluded. First, there is limited scientific evidence regarding the effectiveness of resorbable versus non-resorbable osteosynthesis material in the surgical correction of hallux deformities to improve functionality, pain and angular corrections. All existing studies show improved functionality, decreased pain and effective angular corrections after surgery regardless of the surgical technique and osteosynthesis material used. Second, regarding post-surgical complications, implant removal has only occurred in patients whose surgery used non-resorbable osteosynthesis material. The rest of the complications are quite similar regardless of the osteosynthesis material used. Finally, regarding patient satisfaction and the quality of life perceived by them after surgery, both resorbable and non-resorbable osteosynthesis material improve these variables with resorbable osteosynthesis material offering somewhat better results.
Regarding the limitations of this systematic review, it is worth highlighting the small number of studies that currently exist on the selected topic, most of them being observational case-control studies. This type of study has a lower methodological quality and scientific evidence than that provided by clinical trials; therefore, we have decided to include the few clinical trials that we have found, although this increases the heterogeneity of the studies selected for this review. However, these clinical trials are of medium-low quality. Another limitation to highlight is that there is a wide variety of resorbable hardware that differs in materials, shape, and resorption time. This represents a bias because, considering the low volume of literature, some of the hardware has been evaluated in very few studies. Due to all of the above, the conclusions obtained in this review will be limited to the articles that currently exist. Therefore, it would be advisable to carry out future lines of research where good-quality randomized clinical trials are carried out in order to increase scientific evidence on the topic of study.
Author Contributions
Conceptualization, M.C.-J., P.M.-J. and A.J.P.-B.; methodology, M.C.-J., R.P.-D., P.M.-J., A.J.P.-B., J.M.M.-S. and Á.G.-C.; software, R.P.-D., J.M.M.-S. and Á.G.-C.; validation, R.P.-D., J.M.M.-S. and Á.G.-C.; formal analysis, R.P.-D., J.M.M.-S. and P.M.-J.; research, M.C.-J., R.P.-D., J.M.M.-S. and P.M.-J.; data curation, R.P.-D., J.M.M.-S. and Á.G.-C.; writing: preparation of original draft, M.C.-J., R.P.-D., P.M.-J., A.J.P.-B., J.M.M.-S. and Á.G.-C.; writing: review and editing, M.C.-J., R.P.-D., P.M.-J., A.J.P.-B., J.M.M.-S. and Á.G.-C.; visualization, M.C.-J., A.J.P.-B., J.M.M.-S. and Á.G.-C.; supervision, M.C.-J., R.P.-D. and P.M.-J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Please contact aperez30@us.es with any data requests.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hecht, P.J.; Lin, T.J. Hallux valgus. Med. Clin. North Am. 2014, 98, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Attum, B.; Douleh, D.; Whiting, P.S.; White-Dzuro, G.A.; Dodd, A.C.; Shen, M.S.; Mir, H.R.; Obremskey, W.T.; Sethi, M.K. Outcomes of distal femur nonunions treated with a combined nail/plate construct and autogenous bone grafting. J. Orthop. Trauma 2017, 31, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Hernigou, P.; Pariat, J. History of internal fixations (Part 1): Early developments with wires and plates before World War II. Int. Orthop. 2017, 41, 1273–1283. [Google Scholar] [CrossRef] [PubMed]
- Mann, R.A.; Coughlin, M.J. Hallux valgus—Etiology, anatomy, treatment and surgical considerations. Clin. Orthop. Relat. Res. 1981, 157, 31–41. [Google Scholar] [CrossRef]
- Farraro, K.F.; Kim, K.E.; Woo, S.L.; Flowers, J.R.; McCullough, M.B. Revolutionizing orthopedic biomaterials: The potential of biodegradable and bioresorbable magnesium-based materials for functional tissue engineering. J. Biomech. 2014, 47, 1979–1986. [Google Scholar] [CrossRef] [PubMed]
- Wülker, N.; Mittag, F. The treatment of hallux valgus. Dtsch. Arztebl. Int. 2012, 109, 857–867. [Google Scholar] [CrossRef] [PubMed]
- Izturov, B.Z.; Abilmazhinov, M.T.; Tsoi, O.G. Acquired hallux varus. etiology, pathology, classification, and treatment algorithm. Literature review. Arch. Razi Inst. 2022, 77, 2037–2048. [Google Scholar] [CrossRef]
- Donley, B.G. Acquired hallux varus. Foot Ankle Int. 1997, 18, 586–592. [Google Scholar] [CrossRef]
- Geetha, M.; Singh, A.K.; Asokamani, R.; Gogia, A.K. Ti based biomaterials, the ultimate choice for orthopaedic implants—A review. Prog. Mater. Sci. 2009, 54, 397–425. [Google Scholar] [CrossRef]
- Rangdal, S.; Singh, D.; Joshi, N.; Soni, A.; Sament, R. Functional outcome of ankle fracture patients treated with biodegradable implants. Foot Ankle Surg. 2012, 18, 153–156. [Google Scholar] [CrossRef]
- An, J.; Jia, P.; Zhang, Y.; Gong, X.; Han, X.; He, Y. Application of biodegradable plates for treating pediatric mandibular fractures. J. Craniomaxillofac. Surg. 2015, 43, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Sonnow, L.; Konneker, S.; Vogt, P.M.; Wacker, F.; VonFalck, C. Biodegradable magnesium Herbert screw—Image quality and artifacts with radiography, CT and MRI. BMC Med. Imaging 2017, 17, 16. [Google Scholar] [CrossRef] [PubMed]
- Chou, D.T.; Hong, D.; Saha, P.; Ferrero, J.; Lee, B.; Tan, Z.; Dong, Z.; Kumta, P.N. In vitro and in vivo corrosion, cytocompatibility and mechanical properties of biodegradable Mg-Y-Ca-Zr alloys as implant materials. Acta Biomater. 2013, 9, 8518–8533. [Google Scholar] [CrossRef] [PubMed]
- Pelto-Vasenius, K.; Hirvensalo, E.; Vasenius, J.; Rokkanen, P. Osteolytic changes after polyglycolide pin fixation in chevronosteotomy. Foot Ankle Int. 1997, 18, 21–25. [Google Scholar] [CrossRef]
- Hussein, M.A.; Mohammed, A.S.; Al-Aqeeli, N. Wear characteristics of metallic biomaterials: A review. Materials 2015, 8, 2749–2768. [Google Scholar] [CrossRef]
- Böstman, O.M.; Pihlajamäki, H.K. Adverse tissue reactions to bioabsorbable fixation devices. Clin. Orthop. Relat. Res. 2000, 371, 216–227. [Google Scholar] [CrossRef]
- Zhou, H.; Liang, B.; Jiang, H.; Deng, Z.; Yu, K. Magnesium-based biomaterials as emerging agents for bone repair and regeneration: From mechanism to application. J. Magnesium Alloys 2021, 9, 779–804. [Google Scholar] [CrossRef]
- Seitz, J.M.; Lucas, A.; Kirschner, M. Magnesium-based compression screws: A novelty in the clinical use of implants. JOM 2016, 68, 1177–1182. [Google Scholar] [CrossRef]
- Witte, F. The history of biodegradable magnesium implants: A review. Acta Biomater. 2010, 6, 1680–1692. [Google Scholar] [CrossRef]
- Chen, Y.; Xu, Z.; Smith, C.; Sankar, J. Recent advances on the development of magnesium alloys for biodegradable implants. Acta Biomater. 2014, 10, 4561–4573. [Google Scholar] [CrossRef]
- Krüger, D.; Galli, S.; Zeller-Plumhoff, B.; Wieland, D.C.F.; Peruzzi, N.; Wiese, B.; Heuser, P.; Moosmann, J.; Wennerberg, A.; Willumeit-Romer, R. High-resolution ex vivo analysis of the degradation and osseointegration of Mg-xGd implant screws in 3D. Bioact. Materials 2022, 13, 37–52. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin. Trials. 1996, 17, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-Randomised Studies in Meta-Analyses—Ottawa Hospital Research Institute. 2009. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 16 June 2023).
- Giner, M.; Santana, L.; Costa, A.F.; Vázquez-Gámez, M.A.; Colmenero, M.; Olmo, F.J.; Chicardi, E.; Torres, Y.; Montoya-Garcia, M.J. Study of biocompatibility and osseointegration of new prosthetic materials. Rev. Osteoporos. Metab. Miner. 2020, 12, 92–97. [Google Scholar] [CrossRef]
- May, H.; Alper-Kati, Y.; Gumussuyu, G.; Yunus-Emre, T.; Unal, M.; Kose, O. Bioabsorbable magnesium screw versus conventional titanium screw fixation for medial malleolar fractures. J. Orthop. Traumatol. 2020, 21, 9. [Google Scholar] [CrossRef]
- Plaass, C.; VonFalck, C.; Ettinger, S.; Sonnow, L.; Calderone, F.; Weizbauer, A.; Reifenrath, J.; Claassen, L.; Waizy, H.; Daniilidis, K.; et al. Bioabsorbable magnesium versus standard titanium compression screws for fixation of distal metatarsalosteotomies—3 year results of a randomized clinical trial. J. Orthop. Sci. 2018, 23, 321–327. [Google Scholar] [CrossRef]
- Windhagen, H.; Radtke, K.; Weizbauer, A.; Diekmann, J.; Noll, Y.; Kreimeyer, U.; Schavanm, R.; Stukenborg-Colsman, C.; Waizy, H. Biodegradable magnesium-based screwclinically equivalent to titanium screw in hallux valgus surgery: Short term results of the first prospective, randomized, controlled clinical pilot study. BioMed. Eng. Online 2013, 12, 62. [Google Scholar] [CrossRef]
- Song, J.H.; Kang, C.; Park, W.H.; Lee, G.S.; Lee, J.K.; Kim, D.H.; Lee, S.W. Extended distal Chevron osteotomy and Akin osteotomy using bioabsorbable materials for treatment of moderate to severe hallux valgus. J. Foot Ankle Surg. 2021, 60, 1110–1116. [Google Scholar] [CrossRef]
- Wendelstein, J.; Holzbauer, M.; Neubauer, M.; Steiner, G.; Gruber, F.; Schneider, W. Matched retrospective analysis of three different fixation devices for chevron osteotomy. Foot 2021, 47, 101779. [Google Scholar] [CrossRef]
- Choo, J.T.; Lai, S.H.S.; Tang, C.Q.Y.; Thevendran, G. Magnesium-based bioabsorbable screw fixation for hallux valgus surgery: A suitable alternative to metallic implants. Foot Ankle Surg. 2019, 25, 727–732. [Google Scholar] [CrossRef]
- Atkinson, H.D.; Khan, S.; Lashgari, Y.; Ziegler, A. Hallux valgus correction using a modified short Scarf osteotomy with a biodegradable magnesium ortitanium compression screw—A comparative study of clinical outcomes. BMC Musculoskel Disord. 2019, 20, 334. [Google Scholar] [CrossRef] [PubMed]
- Klauser, H. Internal fixation of three-dimensional distal metatarsal I osteotomies in the treatment of hallux valgus deformities using biodegradable magnesium screws in comparison to titanium screws. Foot Ankle Surg. 2019, 25, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Komur, B.; Yilmaz, B.; Kaan, E.; Yucel, B.; Duymus, T.M.; Ozdemir, G.; Guler, O. Mid-term results of two different fixation methods for chevron osteotomy for correction of hallux valgus. Foot Ankle Surg. 2018, 57, 904–909. [Google Scholar] [CrossRef]
- Acar, B.; Kose, O.; Turan, A.; Unal, M.; Kati, Y.A.; Guler, F. Comparison of bioabsorbable magnesium versus titanium screw fixation for modified distal Chevron osteotomy in hallux valgus. BioMed. Res. Int. 2018, 1, 5242806. [Google Scholar] [CrossRef] [PubMed]
- Morandi, A.; Ungaro, E.; Fraccia, A.; Sansone, V. Chevron osteotomy of the first metatarsal stabilized with an absorbable pin: Our 5-year experience. Foot Ankle Int. 2013, 34, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Kamrani, S.; Fleck, C. Biodegradable magnesium alloys as temporary orthopedic implants: A review. Biometals 2019, 32, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Jastifer, J.R.; Gustafson, P.A.; Silva, L.F.; Noffsinger, S.; Coughlin, M.J. Nitinol, stainless steel, and titanium Kirschner wire durability. Foot Ankle Spec. 2021, 14, 317–323. [Google Scholar] [CrossRef]
- Amukarimi, S.; Mozafari, M. Biodegradable magnesium-based biomaterials: An overview of challenges and opportunities. Med. Comm. 2021, 2, 123–144. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).