Early Signs of Microvascular Endothelial Dysfunction in Adolescents with Newly Diagnosed Essential Hypertension
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.1.1. Anthropometric Measures
2.1.2. Diagnosis of Hypertension
2.1.3. Diagnosis of Overweight
2.2. Protocol
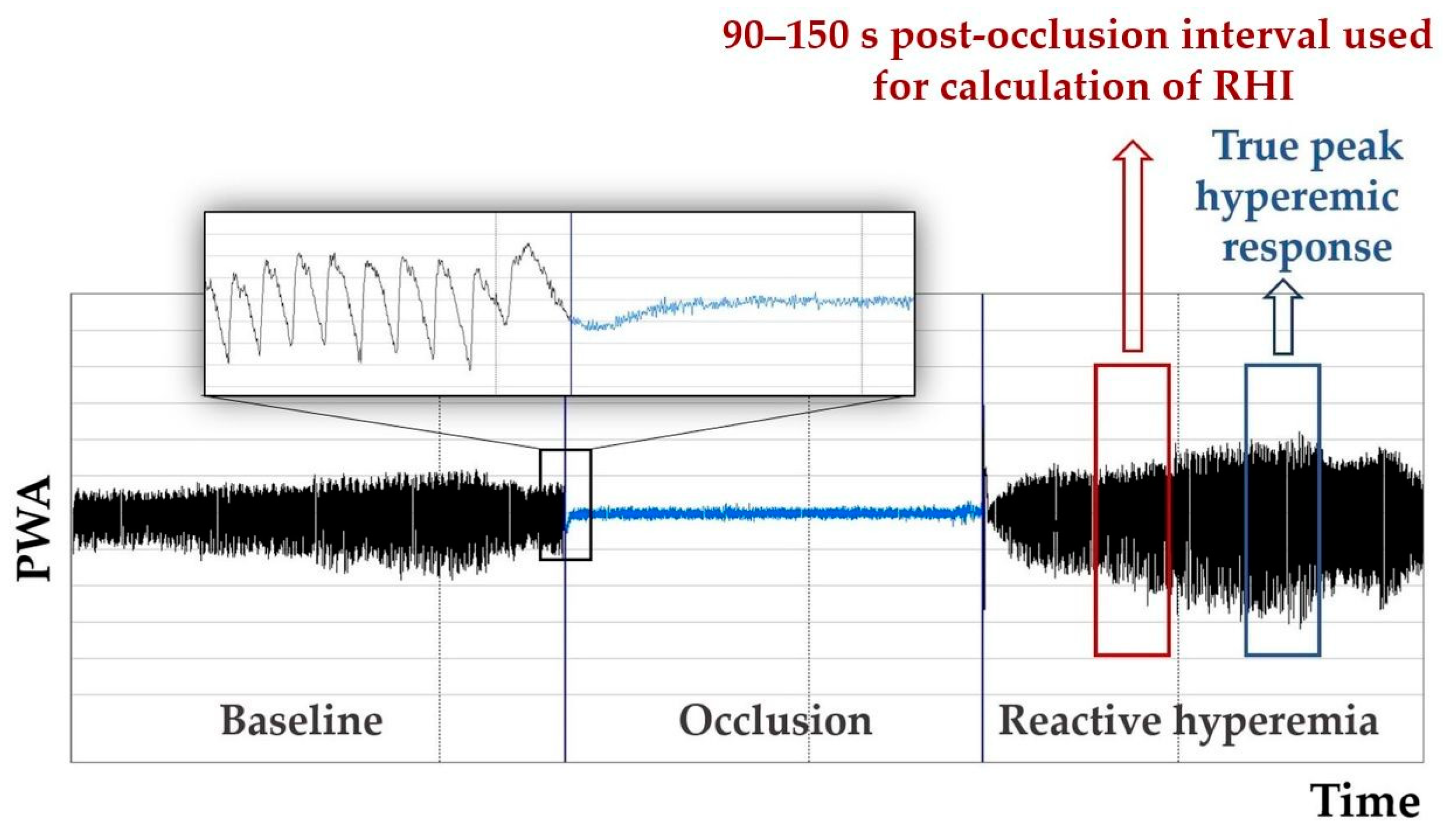
2.3. Evaluated Parameters of Endothelial Function
2.4. Statistical Analysis
3. Results
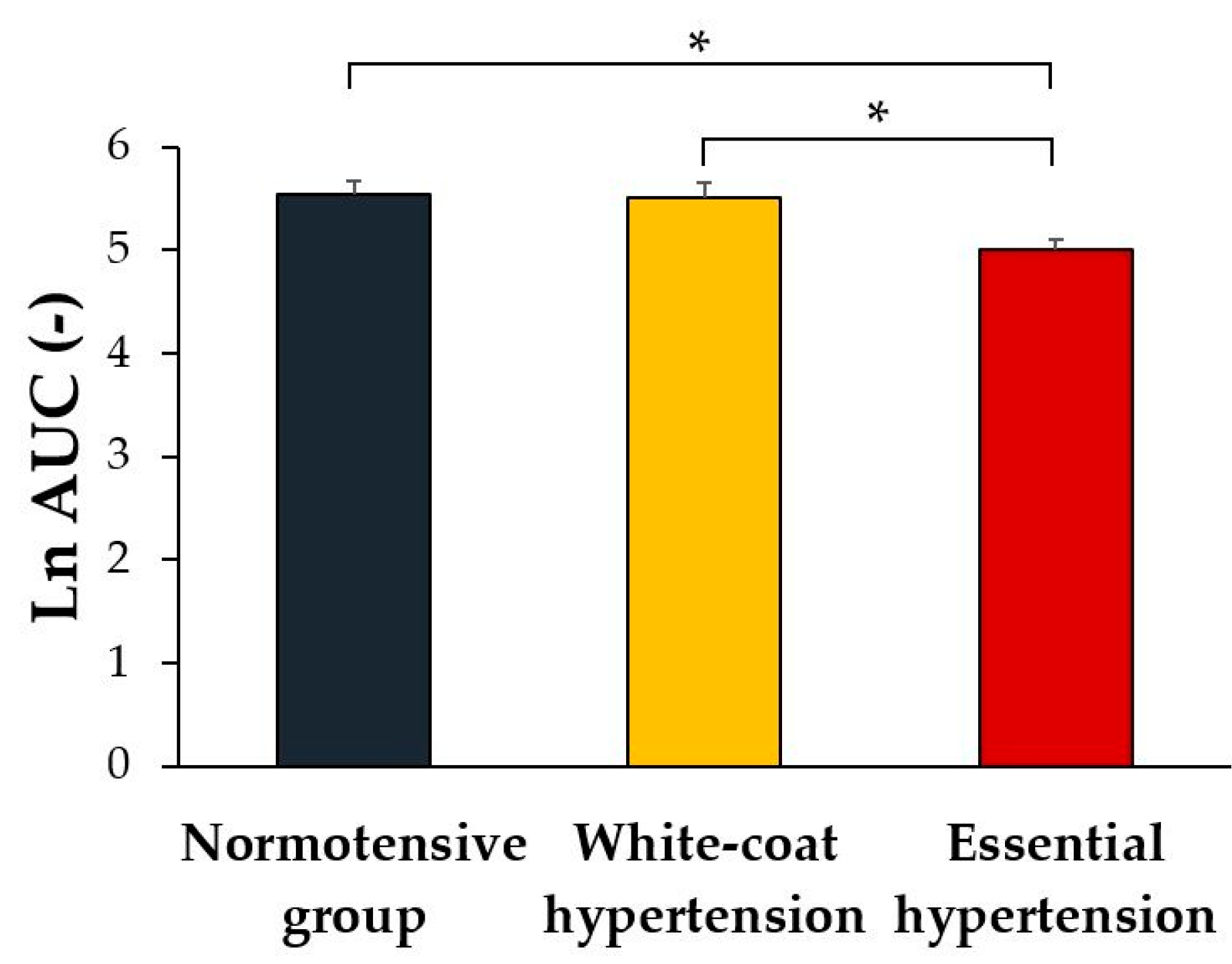
3.1. Between-Groups Comparison of the Indices of Reactive Hyperemia
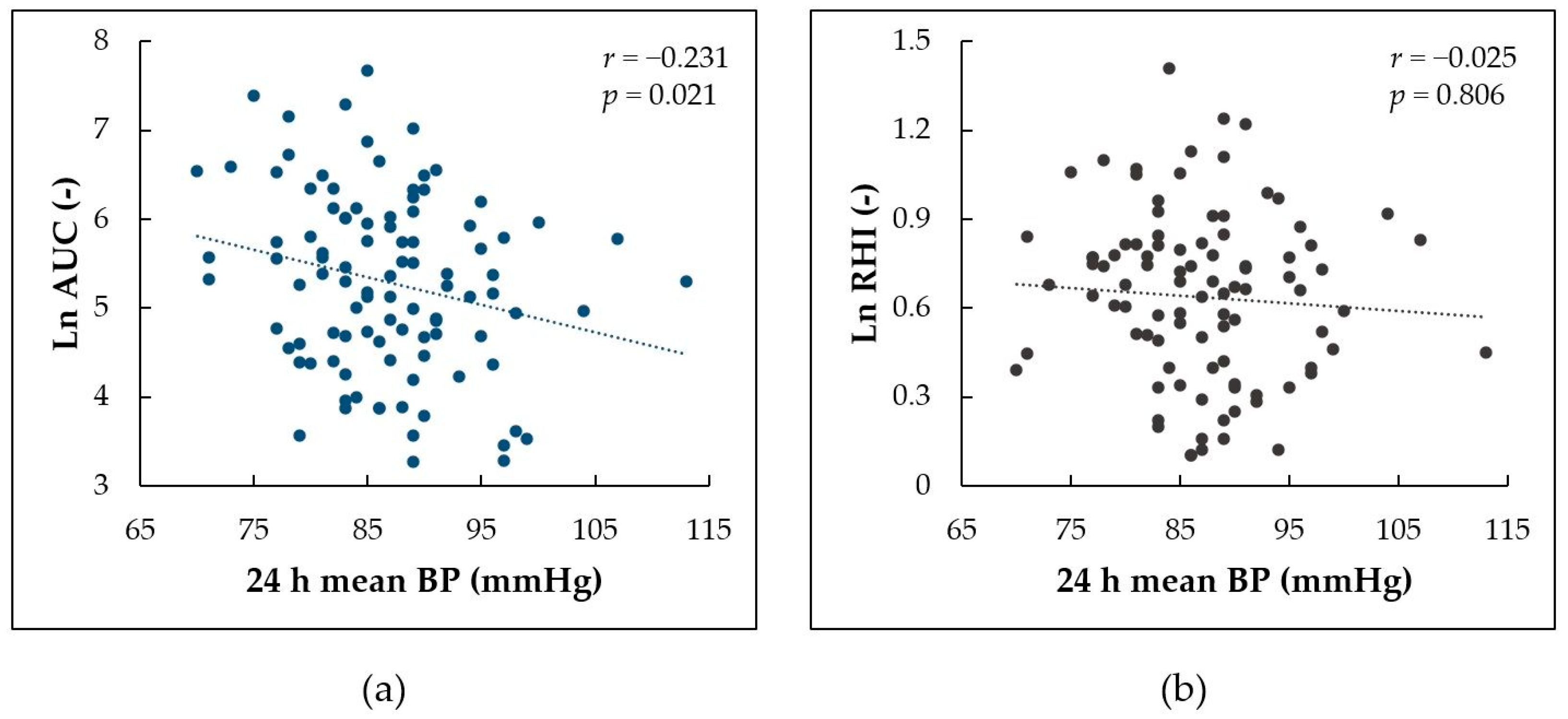
3.2. Associations of the Indices of Reactive Hyperemia with Mean BP
3.3. Regression Analysis
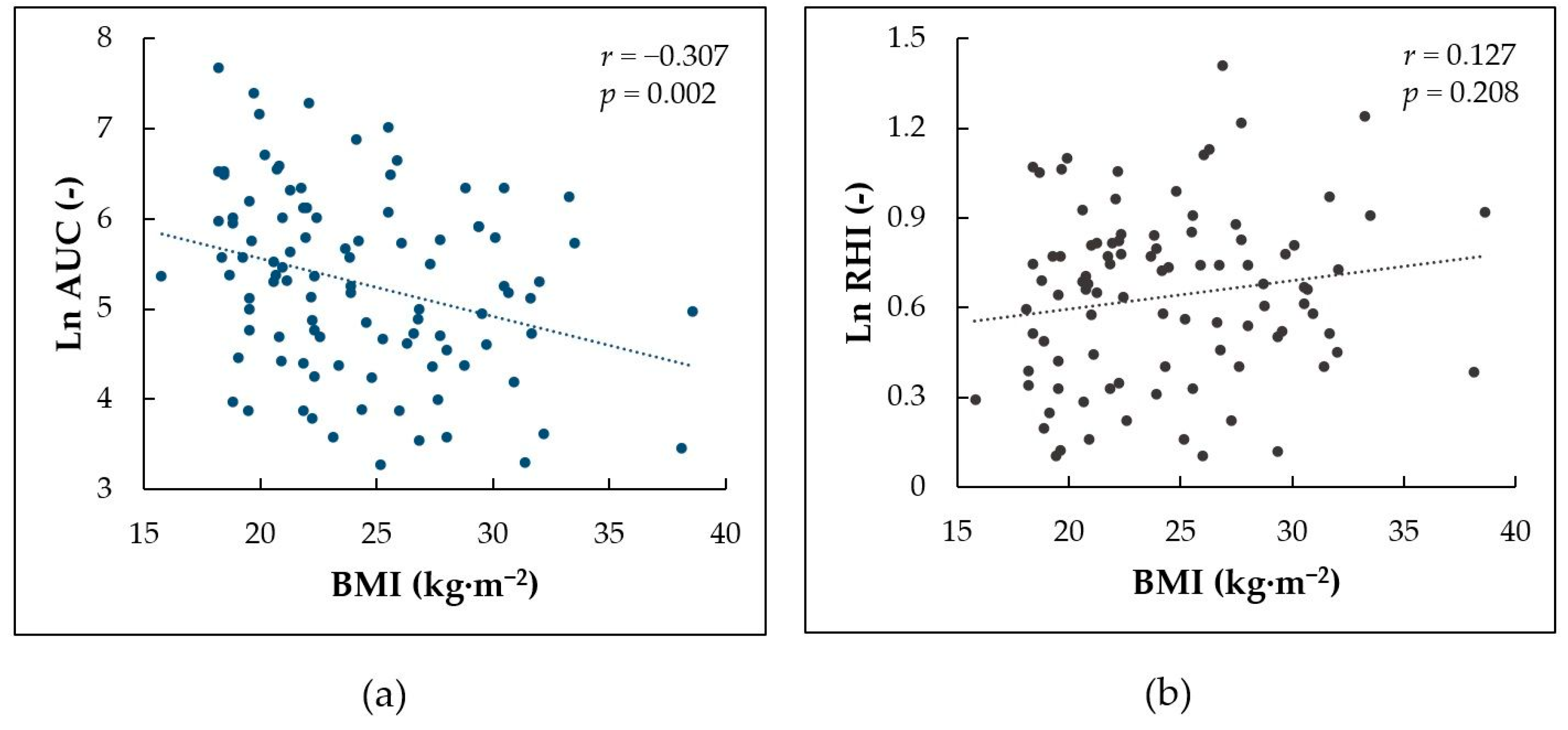
3.4. Correlation between BMI and Indices of Reactive Hyperemia
4. Discussion
4.1. Endothelial Function in Pediatric Hypertension
4.2. Measures of Microvascular Endothelial Function—RHI vs. AUC
4.3. The Effect of BMI and Aspartate Aminotransferase Levels
4.4. The Effect of Age, Pubertal Development, and Out-of-Office BP
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ambrosino, P.; Grassi, G.; Maniscalco, M. Endothelial Dysfunction: From a Pathophysiological Mechanism to a Potential Therapeutic Target. Biomedicines 2021, 10, 78. [Google Scholar] [CrossRef] [PubMed]
- Vane, J.R.; Änggård, E.E.; Botting, R.M. Regulatory Functions of the Vascular Endothelium. N. Engl. J. Med. 1990, 323, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Hamburg, N.M.; Vita, J.A. Endothelial Dysfunction in Atherosclerosis: Mechanisms of Impaired Nitric Oxide Bioactivity. In Molecular Mechanisms of Atherosclerosis; Loscalzo, J., Ed.; Taylor & Francis: London, UK, 2006. [Google Scholar]
- Juonala, M.; Viikari, J.S.A.; Laitinen, T.; Marniemi, J.; Helenius, H.; Rönnemaa, T.; Raitakari, O.T. Interrelations between Brachial Endothelial Function and Carotid Intima-Media Thickness in Young Adults: The Cardiovascular Risk in Young Finns Study. Circulation 2004, 110, 2918–2923. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H. Various Indices of Arterial Stiffness: Are They Closely Related or Distinctly Different? Pulse 2018, 5, 1–6. [Google Scholar] [CrossRef]
- Dhindsa, M.; Sommerlad, S.M.; DeVan, A.E.; Barnes, J.N.; Sugawara, J.; Ley, O.; Tanaka, H. Interrelationships among Noninvasive Measures of Postischemic Macro- and Microvascular Reactivity. J. Appl. Physiol. 2008, 105, 427–432. [Google Scholar] [CrossRef]
- Flammer, A.J.; Anderson, T.; Celermajer, D.S.; Creager, M.; Deanfield, J.; Ganz, P.; Hamburg, N.M.; Lüscher, T.F.; Shechter, M.; Taddei, S.; et al. The Assessment of Endothelial Function: From Research into Clinical Practice. Circulation 2012, 126, 753–767. [Google Scholar] [CrossRef]
- Schnall, R.P.; Sheffy, J.K.; Penzel, T. Peripheral Arterial Tonometry-PAT Technology. Sleep Med. Rev. 2022, 61, 101566. [Google Scholar] [CrossRef]
- Itamar Medical. Endo PAT2000 Device User Manual; Itamar Medical: Caesarea, Israel, 2014. [Google Scholar]
- Chen, Y.; Dangardt, F.; Osika, W.; Berggren, K.; Gronowitz, E.; Friberg, P. Age- and Sex-Related Differences in Vascular Function and Vascular Response to Mental Stress. Longitudinal and Cross-Sectional Studies in a Cohort of Healthy Children and Adolescents. Atherosclerosis 2012, 220, 269–274. [Google Scholar] [CrossRef]
- Bonetti, P.O.; Lerman, L.O.; Lerman, A. Endothelial Dysfunction: A Marker of Atherosclerotic Risk. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 168–175. [Google Scholar] [CrossRef]
- la Valle, A.; Crocco, M.; Chiarenza, D.S.; Maghnie, M.; d’Annunzio, G. Endothelial Impairment Evaluation by Peripheral Arterial Tonometry in Pediatric Endocrinopathies: A Narrative Review. World J. Diabetes 2021, 12, 810–826. [Google Scholar] [CrossRef]
- Radtke, T.; Khattab, K.; Eser, P.; Kriemler, S.; Saner, H.; Wilhelm, M. Puberty and Microvascular Function in Healthy Children and Adolescents. J. Pediatr. 2012, 161, 887–891.e1. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, C.; Cohen, H.W.; Muzumdar, R.H.; Heptulla, R.A.; Renukuntla, V.S.; Crandall, J. Obesity, Hyperglycemia and Endothelial Function in Inner City Bronx Adolescents: A Cross-Sectional Study. Int. J. Pediatr. Endocrinol. 2013, 2013, 18. [Google Scholar] [CrossRef] [PubMed]
- Bhangoo, A.; Sinha, S.; Rosenbaum, M.; Shelov, S.; Ten, S. Endothelial Function as Measured by Peripheral Arterial Tonometry Increases during Pubertal Advancement. Horm. Res. Paediatr. 2011, 76, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Kheirandish-Gozal, L.; Etzioni, T.; Bhattacharjee, R.; Tan, H.L.; Samiei, A.; Molero Ramirez, H.; Abu Eta, B.; Pillar, G. Obstructive Sleep Apnea in Children Is Associated with Severity-Dependent Deterioration in Overnight Endothelial Function. Sleep Med. 2013, 14, 526–531. [Google Scholar] [CrossRef]
- Pinto, F.F.; Laranjo, S.; Paramés, F.; Freitas, I.; Mota-Carmo, M. Long-Term Evaluation of Endothelial Function in Kawasaki Disease Patients. Cardiol. Young 2013, 23, 517–522. [Google Scholar] [CrossRef][Green Version]
- Haller, M.J.; Stein, J.; Shuster, J.; Theriaque, D.; Silverstein, J.; Schatz, D.A.; Earing, M.G.; Lerman, A.; Mahmud, F.H. Peripheral Artery Tonometry Demonstrates Altered Endothelial Function in Children with Type 1 Diabetes. Pediatr. Diabetes 2007, 8, 193–198. [Google Scholar] [CrossRef]
- Mueller, U.M.; Walther, C.; Adam, J.; Fikenzer, K.; Erbs, S.; Mende, M.; Adams, V.; Linke, A.; Schuler, G. Endothelial Function in Children and Adolescents Is Mainly Influenced by Age, Sex and Physical Activity—An Analysis of Reactive Hyperemic Peripheral Artery Tonometry. Circ. J. 2016, 81, 717–725. [Google Scholar] [CrossRef]
- Juonala, M.; Viikari, J.S.A.; Rönnemaa, T.; Helenius, H.; Taittonen, L.; Raitakari, O.T. Elevated Blood Pressure in Adolescent Boys Predicts Endothelial Dysfunction: The Cardiovascular Risk in Young Finns Study. Hypertension 2006, 48, 424–430. [Google Scholar] [CrossRef]
- Jurko, A.; Jurko, T.; Minarik, M.; Mestanik, M.; Mestanikova, A.; Micieta, V.; Visnovcova, Z.; Tonhajzerova, I. Endothelial Function in Children with White-Coat Hypertension. Heart Vessel. 2018, 33, 657–663. [Google Scholar] [CrossRef]
- Cole, T.J.; Lobstein, T. Extended International (IOTF) Body Mass Index Cut-Offs for Thinness, Overweight and Obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef]
- Lurbe, E.; Cifkova, R.; Cruickshank, J.K.; Dillon, M.J.; Ferreira, I.; Invitti, C.; Kuznetsova, T.; Laurent, S.; Mancia, G.; Morales-Olivas, F.; et al. Management of High Blood Pressure in Children and Adolescents: Recommendations of the European Society of Hypertension. J. Hypertens. 2009, 27, 1719–1742. [Google Scholar] [CrossRef] [PubMed]
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics 2004, 114, 555–576. [Google Scholar] [CrossRef]
- Shirtcliff, E.A.; Dahl, R.E.; Pollak, S.D. Pubertal Development: Correspondence Between Hormonal and Physical Development. Child Dev. 2009, 80, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Kuvin, J.T.; Patel, A.R.; Sliney, K.A.; Pandian, N.G.; Sheffy, J.; Schnall, R.P.; Karas, R.H.; Udelson, J.E. Assessment of Peripheral Vascular Endothelial Function with Finger Arterial Pulse Wave Amplitude. Am. Heart J. 2003, 146, 168–174. [Google Scholar] [CrossRef]
- Hamburg, N.M.; Keyes, M.J.; Larson, M.G.; Vasan, R.S.; Pryde, M.M.; Mitchell, G.F.; Sheffy, J.; Vita, J.A.; Emelia, J. Cross-Sectional Relations of Digital Vascular Function to Cardiovascular Risk Factors in the Framingham Heart Study. Circulation 2008, 117, 2467–2474. [Google Scholar] [CrossRef] [PubMed]
- Bruyndonckx, L.; Radtke, T.; Eser, P.; Vrints, C.J.; Ramet, J.; Wilhelm, M.; Conraads, V.M. Methodological Considerations and Practical Recommendations for the Application of Peripheral Arterial Tonometry in Children and Adolescents. Int. J. Cardiol. 2013, 168, 3183–3190. [Google Scholar] [CrossRef]
- Urbina, E.M. Abnormalities of Vascular Structure and Function in Pediatric Hypertension. Pediatr. Nephrol. 2016, 31, 1061–1070. [Google Scholar] [CrossRef]
- Jurko, A.; Minarik, M.; Jurko, T.; Tonhajzerova, I. White Coat Hypertension in Pediatrics. Ital. J. Pediatr. 2016, 42, 4. [Google Scholar] [CrossRef]
- Nohria, A.; Gerhard-Herman, M.; Creager, M.A.; Hurley, S.; Mitra, D.; Ganz, P. Role of Nitric Oxide in the Regulation of Digital Pulse Volume Amplitude in Humans. J. Appl. Physiol. 2006, 101, 545–548. [Google Scholar] [CrossRef]
- Hamburg, N.M.; Palmisano, J.; Larson, M.G.; Sullivan, L.M.; Lehman, B.T.; Vasan, R.S.; Levy, D.; Mitchell, G.F.; Vita, J.A.; Benjamin, E.J. Relation of Brachial and Digital Measures of Vascular Function in the Community: The Framingham Heart Study. Hypertension 2011, 57, 390–396. [Google Scholar] [CrossRef]
- Martinez-Majander, N.; Gordin, D.; Joutsi-Korhonen, L.; Salopuro, T.; Adeshara, K.; Sibolt, G.; Curtze, S.; Pirinen, J.; Liebkind, R.; Soinne, L.; et al. Endothelial Dysfunction Is Associated With Early-Onset Cryptogenic Ischemic Stroke in Men and With Increasing Age. J. Am. Heart Assoc. 2021, 10, e020838. [Google Scholar] [CrossRef] [PubMed]
- Toya, T.; Sara, J.D.; Ahmad, A.; Nardi, V.; Taher, R.; Lerman, L.O.; Lerman, A. Incremental Prognostic Impact of Peripheral Microvascular Endothelial Dysfunction on the Development of Ischemic Stroke. J. Am. Heart Assoc. 2020, 9, e015703. [Google Scholar] [CrossRef] [PubMed]
- Mestanik, M.; Jurko, A.; Mestanikova, A.; Jurko, T.; Tonhajzerova, I. Arterial Stiffness Evaluated by Cardio-Ankle Vascular Index (CAVI) in Adolescent Hypertension. Can. J. Physiol. Pharmacol. 2016, 94, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Radtke, T.; Eser, P.; Kriemler, S.; Saner, H.; Wilhelm, M. Adolescent Blood Pressure Hyperreactors Have a Higher Reactive Hyperemic Index at the Fingertip. Eur. J. Appl. Physiol. 2013, 113, 2991–3000. [Google Scholar] [CrossRef] [PubMed]
- Ndrepepa, G. Aspartate Aminotransferase and Cardiovascular Disease—A Narrative Review. J. Lab. Precis. Med. 2021, 6, 1–17. [Google Scholar] [CrossRef]
- Theofilis, P.; Vordoni, A.; Nakas, N.; Kalaitzidis, R.G. Endothelial Dysfunction in Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis. Life 2022, 12, 718. [Google Scholar] [CrossRef]
- Yu, E.L.; Golshan, S.; Harlow, K.E.; Angeles, J.E.; Durelle, J.; Goyal, N.P.; Newton, K.P.; Sawh, M.C.; Hooker, J.; Sy, E.Z.; et al. Prevalence of Nonalcoholic Fatty Liver Disease in Children with Obesity. J. Pediatr. 2019, 207, 64–70. [Google Scholar] [CrossRef]
- He, W.; Zhang, Y.; Li, X.; Mu, K.; Dou, Y.; Ye, Y.; Liu, F.; Yan, W. Multiple Non-Invasive Peripheral Vascular Function Parameters with Obesity and Cardiometabolic Risk Indicators in School-Aged Children. BMC Pediatr. 2022, 22, 146. [Google Scholar] [CrossRef]
- Pareyn, A.; Allegaert, K.; Verhamme, P.; Vinckx, J.; Casteels, K. Impaired Endothelial Function in Adolescents with Overweight or Obesity Measured by Peripheral Artery Tonometry. Pediatr. Diabetes 2015, 16, 98–103. [Google Scholar] [CrossRef]
- Chang, J.C.; Xiao, R.; Meyers, K.E.; Mercer-Rosa, L.; Natarajan, S.S.; Weiss, P.F.; Knight, A.M. Nocturnal Blood Pressure Dipping as a Marker of Endothelial Function and Subclinical Atherosclerosis in Pediatric-Onset Systemic Lupus Erythematosus. Arthritis Res. Ther. 2020, 22, 129. [Google Scholar] [CrossRef]
- Tryggestad, J.B.; Thompson, D.M.; Copeland, K.C.; Short, K.R. Obese Children Have Higher Arterial Elasticity without a Difference in Endothelial Function: The Role of Body Composition. Obesity 2012, 20, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Bacha, F.; Tomsa, A.; Bartz, S.K.; Barlow, S.E.; Chu, Z.D.; Krishnamurthy, R.; Krishnamurthy, R.; O’Brian Smith, E. Nonalcoholic Fatty Liver Disease in Hispanic Youth with Dysglycemia: Risk for Subclinical Atherosclerosis? J. Endocr. Soc. 2017, 1, 1029–1040. [Google Scholar] [CrossRef] [PubMed]
- Czippelova, B.; Turianikova, Z.; Krohova, J.; Wiszt, R.; Lazarova, Z.; Pozorciakova, K.; Ciljakova, M.; Javorka, M. Arterial Stiffness and Endothelial Function in Young Obese Patients—Vascular Resistance Matters. J. Atheroscler. Thromb. 2019, 26, 1015–1025. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, S.; Mylemans, E.; Ysebaert, M.; Vermeiren, E.; de Guchtenaere, A.; Heuten, H.; Bruyndoncx, L.; de Winter, B.Y.; van Hoorenbeeck, K.; Verhulst, S.L.; et al. The Impact of Obstructive Sleep Apnea on Endothelial Function during Weight Loss in an Obese Pediatric Population. Sleep Med. 2021, 86, 48–55. [Google Scholar] [CrossRef] [PubMed]
| Normotensive Group (n = 27) | White-Coat Hypertension Group (n = 28) | Essential Hypertension Group (n = 45) | |
|---|---|---|---|
| Ln RHI (-) | 0.690 (0.450–0.810) | 0.630 (0.238–0.943) | 0.680 (0.510–0.825) |
| FRHI (-) | 0.676 (0.502–0.932) | 0.711 (0.183–0.955) | 0.634 (0.367–0.818) |
| Peak response (-) | 2.280 (1.792–2.565) | 2.303 (1.453–2.780) | 2.199 (1.749–2.580) |
| Time to peak response (s) | 150.0 (90.0–240.0) | 180.0 (120.0–232.5) | 120.0 (90.0–210.0) |
| Parameter | Coefficient | Std. Error | Units | p-Value |
|---|---|---|---|---|
| Intercept | 10.786 | 1.474 | - | <0.001 |
| Age | −0.125 | 0.060 | year−1 | 0.039 |
| Male sex | −0.421 | 0.254 | - | 0.102 |
| Mean BP (24 h ABPM) | −0.033 | 0.013 | mmHg−1 | 0.011 |
| DHEAS | 0.062 | 0.028 | µmol−1·L | 0.027 |
| AST | −1.561 | 0.719 | µkat−1·L | 0.033 |
| Studied Population/Evaluated Mechanism | Findings | Reference |
|---|---|---|
| 540 children aged 7–17 years (80 with overweight, 73 with obesity), the effect of the obesity and cardiometabolic risk indicators | Increase of RHI, F-RHI, and Peak response with age Decrease of RHI, F-RHI, and Peak response with diastolic BP Decrease of RHI with TG in obese individuals | He et al., 2022 [40] |
| 27 overweight/obese and 25 normal-weight adolescents aged 12–20 years | Decrease of RHI with diastolic BP Lower RHI in overweight/obese subjects | Pareyn et al., 2015 [41] |
| 20 children aged 9–19 years with systemic lupus erythematosus, the effect of nocturnal BP dipping | Lower RHI in patients with nocturnal BP non-dipping pattern assessed using 24 h ABPM | Chang et al., 2020 [42] |
| 62 obese and 61 normal weight children aged 8–18 years | Increase of RHI with age in lean but not obese children | Tryggestad et al., 2012 [43] |
| 36 obese adolescents aged 11–19 years, the effect of the presence of NAFLD | Decrease of RHI with hepatic fat content | Bacha et al., 2017 [44] |
| 29 obese and 29 non-obese adolescents and young adults aged 12–23 years, the effect of hemodynamic parameters | Positive correlation between RHI and systemic vascular resistance, no significant difference in RHI between obese and non-obese subjects | Czippelova et al., 2019 [45] |
| 130 obese children aged 8–18 years, the effect of weight loss | Increase of RHI and decrease of Time to peak response after weight loss | Jacobs et al., 2021 [46] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jurko, T.; Mestanik, M.; Mestanikova, A.; Zeleňák, K.; Jurko, A. Early Signs of Microvascular Endothelial Dysfunction in Adolescents with Newly Diagnosed Essential Hypertension. Life 2022, 12, 1048. https://doi.org/10.3390/life12071048
Jurko T, Mestanik M, Mestanikova A, Zeleňák K, Jurko A. Early Signs of Microvascular Endothelial Dysfunction in Adolescents with Newly Diagnosed Essential Hypertension. Life. 2022; 12(7):1048. https://doi.org/10.3390/life12071048
Chicago/Turabian StyleJurko, Tomas, Michal Mestanik, Andrea Mestanikova, Kamil Zeleňák, and Alexander Jurko. 2022. "Early Signs of Microvascular Endothelial Dysfunction in Adolescents with Newly Diagnosed Essential Hypertension" Life 12, no. 7: 1048. https://doi.org/10.3390/life12071048
APA StyleJurko, T., Mestanik, M., Mestanikova, A., Zeleňák, K., & Jurko, A. (2022). Early Signs of Microvascular Endothelial Dysfunction in Adolescents with Newly Diagnosed Essential Hypertension. Life, 12(7), 1048. https://doi.org/10.3390/life12071048






